Alveolar ridge extension in the aesthetic zone
Machine translation
Original article is written in RU language (link to read it) .
This article describes and explains a technique that effectively creates a large volume of accessible hard and soft tissue in the vertical plane without surgical intervention. The disadvantages of targeted (forced) tooth extraction are also discussed.
About methods and tools for achieving stable results of implantological and periodontal treatment in the online course Guided regeneration and navigational implantation .
Creating an esthetic restoration with an implant is a challenge for patients who have alveolar resorption and/or loss of attached gingiva, especially when they have a high smile line. Many methods have been proposed to replace alveolar ridge loss, but most have involved surgical procedures to add bone tissue or bone substitutes to compensate for the loss of alveolar bone.
This case presents an alternative to bone augmentation using orthodontic tooth movement in the esthetic zone in a 62-year-old woman. Tooth movement was facilitated by the placement of implants and by increasing the soft tissue and bony contours of the face.
Decreased alveolar ridge height
Reduction of alveolar ridge height (CAH) after tooth extraction is an important unresolved physiological process that causes physical, psychological and economic problems in millions of people worldwide. SAH is a chronic, progressive and irreversible process of multifactorial origin.
Atwood performed a clinical, cephalometric and densitometric study of residual ridge volume reduction in 76 edentulous patients. He found that the average rate of contraction (decrease/decrease) of the lower jaw was four times higher than that of the upper jaw.
Ways to compensate for alveolar ridge deficiency
One way to compensate for alveolar ridge deficiency is the use of bar bone grafts. These grafts are predominantly cortical, have a tendency to undergo little resorption, and typically adhere (assimilate) very well to the recipient bone within a relatively short period of time. They also maintain bone volume during implant placement and maintain bone density. Despite the numerous advantages of bar grafts for alveolar ridge augmentation, there are complications when using them for horizontal and vertical tissue augmentation.
Soreness can occur from both the donor and recipient. On the donor side, symphysis pain may be associated with complications such as bleeding, mental nerve injury and soft tissue damage in the cheeks, lips and tongue, as well as fracture of the transplanted structure. Pain, swelling, bruising, and sensorineural deficits that include altered sensation in the lower lip and chin may occur. Damage to the nerve branches in the cheek area can be caused by complications such as bleeding, soft tissue damage, nerve tissue damage, and fracture of the beam and mandible.
Postoperative morbidity includes spasm of the masticatory muscles, pain, swelling, bruising, and altered sensation in the lower lip/chin and lingual nerve. Spasm of the masticatory muscles, swelling, bleeding, pain, bruising, infection, bone resorption, sensorineural deficits, and graft rejection can all occur in the recipient.
Orthodontic tooth extrusion
“Orthodontic tooth extrusion” is a term used to describe the forced (purposeful) movement of teeth in a vertical plane using moderate forces. It has been suggested that single tooth extrusion may be used as an adjunctive technique in periodontal therapy aimed at eliminating or reducing angular bone defects without compromising the periodontal attachment of adjacent teeth.
The effect of orthodontic extrusion on periodontal tissues has been evaluated (proven) in both clinical studies and animal experiments. Early research by scientists including Oppenheim, Ritchey and Orban, and Reitan showed that:
- extrusion led to an increase in bone in the area of the root apex, as well as in the area of the alveolar ridge of the displaced tooth;
- the alveolar ridge of a healthy periodontium will have a normal connection (1-2 mm) with the enamel-cementum junction.
Batenhorst et al reported that tooth extrusion in a monkey not only resulted in replenishment of the ridge height but also in an increase in the width of the attached gingiva. Van Venrooy and Yukna used a dog to evaluate the effectiveness of orthodontic tooth extrusion associated with advanced periodontal disease. The authors advanced the teeth at a distance of 3 mm to 4 mm and could see that on the studied teeth, compared to those that were not advanced, inflammation of the gum tissue was less pronounced, and the periodontal pockets were less deep. They also found that extrusion resulted in an enlarged bone ridge. It has been suggested that extrusion of teeth with advanced periodontal disease:
- can move subgingival microflora to a supragingival position;
- have a therapeutic effect on periodontium.
Pontoriero et al. and Kozlowsky et al. developed a method of tooth extrusion that combined the application of orthodontic forces with resection of the periosteal attached fibers (fibretomy). The combined procedure was performed in a case series and was found to promote extrusion of individual teeth but inhibit concomitant periodontal migration towards the dental crown.
The previously prepared portion of the tooth was then left open and accessible for subsequent restorative procedures. Thus, forced (targeted) tooth movement has the right to life as a method for changing the gum margin. The most common set of clinical indications for the use of forced movement are those cases where it is undesirable to remove gingival tissue from adjacent teeth and where surgical procedures to graft tissue will not be predictable (i.e., will cover the root surface). The ideal indication for forced (targeted/forced) tooth movement would be the presence of artificial crowns when recession occurs during their placement or as a result of trauma.
Clinical case
A 62-year-old woman presented to the Department of Advanced Orthopedics at the University of Southern California. Her main complaint was increased mobility of the front teeth in the upper jaw, as well as an increase in the distance between them. Her medical history was unremarkable. An intraoral examination showed degree II and III mobility of the anterior teeth in the upper jaw, as well as their fluctuations. (photo 1)

Photo 1
The patient had no spasm of the masticatory muscles and no restrictions on mouth opening. Evaluation of her radiographs revealed significant bone loss around the maxillary anterior teeth, with up to 80% attachment loss in the lateral incisor area (Figure 2).

Photo 2
After collecting data and conducting diagnostics, a comprehensive treatment plan was developed for the patient. One of the diagnoses was loss of support. The authors believed that this is due to excessive forces that are directed towards the anterior teeth in the upper jaw. They were subject to occlusal trauma, which contributed to loss of attachment, mobility and oscillation. With the restoration of the anchorage, it was expected that there would be a decrease in mobility and possible elimination of vibration of teeth Nos. 8 and 9 and possibly an improvement in the levels of periodontal attachment.
The patient did not want to use removable dentures during treatment. The first phase of the treatment plan was removal of subgingival plaque and root planing of the maxillary anterior teeth (Photo 3 - Photo 5), followed by orthodontic extrusion of teeth Nos. 7 and 10.

Photo 3

Photo 4

Photo 5
Three months after extrusion, tooth No. 10 became sensitive and a pulpotomy was necessary. Seven months after extrusion, the available bone and soft tissue volume was examined clinically and radiographically. The volume of hard and soft tissue was considered sufficient to allow implant placement with an acceptable result (Fig. 6 and Fig. 7).

Photo 6

Photo 7
The lateral teeth on the upper jaw were removed as atraumatically as possible, and implants were immediately placed. The clinical crowns of the extracted teeth were reattached to the orthodontic appliance as temporary restorations (Figure 8). After five months, the implants were exposed and impressions were taken. Temporary restorations were also secured with screws (in implants) (Fig. 9).

Photo 8

Photo 9
At the same time, implant-supported temporary restorations were placed on the implants restoring the posterior teeth, thereby replenishing support. After removal of the orthodontic structures, the mobility of the central incisors was reduced to less than 1 degree.
After the soft tissue had healed and the provisional restorations had been contoured for 4 weeks, a custom tray was used to take impressions to duplicate the soft tissue contours on the cast model. This allowed the technician to produce submucosal contours for the final restorations identical to those created for the provisional restorations (Figure 10).

Photo 10
The final restorations were installed after 2 months. Although teeth Nos. 8 and 9 had loss of adhesion and decreased mobility, they were found to have a good prognosis with proper care. The examination shown in Photo 11 shows, both clinically and radiographically, that acceptable esthetics were obtained and the implants were well integrated. The comparison in photos 12 and 13 shows the improvements achieved by the time the treatment was completed.
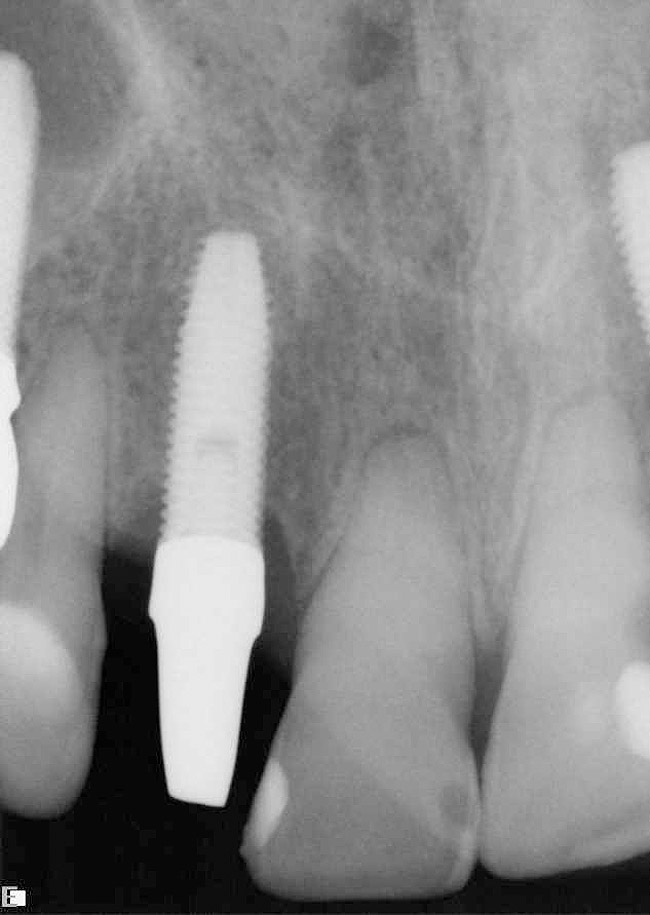
Photo 11

Photo 12

Photo 13
Treatment options for patients with periodontal disease
Osseointegrated implants allow patients who are missing teeth to replace them in the most conservative way possible, saving time on preparing adjacent teeth. They also have a well-established track record of success. However, other problems arising from the aesthetics of the soft tissue around dental implants largely depend on the volume of hard and soft tissue. These problems have necessitated the creation of new criteria when planning treatment for patients at risk of periodontal disease.
One of these criteria in the foreground should be the preparation of a site for the implant that is adequate in size and volume. It must be such that the aesthetics around the implant are acceptable. Additional treatment planning aspects to consider are whether any teeth can be saved from a periodontal prosthetic perspective and whether teeth should be extracted. It is also necessary to consider techniques that, if necessary, can increase the potential space for nerve endings.
The optimal sequence of implant placement and surgical techniques for treating the mucosa also need to be taken into account. One of the most challenging problems arises when implant placement must continue despite defect removal in patients at risk for periodontal disease. It is important to first understand how to ideally deal with residual defects that can often be associated with tooth extraction. To place implants that can provide restorative support designed to maintain functional and aesthetic harmony with adjacent natural teeth.
Tooth extraction followed by immediate placement of implants has been advocated as a more feasible approach to replacing problematic teeth with implants.
Improving the architecture of both soft and hard tissue through efficient extrusion movement of teeth has proven success. Brown and Ingber emphasize that vertical molar and forced (forced) advancement are methods for correcting osseous and gingival topography. The fibrogingival apparatus does not have elasticity, so stretching it during tooth movement relieves tension on the alveolar bone. It is widely known that this tension stimulates bone loss in the alveolar ridge region. Extrusive tooth movement also increases soft tissue volume by increasing the area of attached gingiva. This increase occurs because during this type of movement, the gingival margin migrates toward the crown while the mucogingival junction remains stable.
The alveolar bone ridge is an important basis for the gingival levels. The location of these ratios is an important way to assess what gingival levels will be after the intervention: the greater the distance from the bone crest to the free gingival margin (FCG), the higher the risk of tissue loss after an invasive procedure. Orthodontic extrusion is recommended if the distance to the bone crest is 3 mm or more. However, gingival levels must be sufficiently balanced to compensate for subsequent bone resorption and the potentially greater loss of soft tissue caused by movement of the bone crest towards the crown of the tooth.
The relationship between interproximal bone tissue has also been described and has a close relationship; the dimensions are based on the most coronally located part of the interproximal bone crest of adjacent teeth and are not related to the interproximal position of the bone crest of the tooth being removed. Therefore, if the interdental papilla is >4 mm in size (low ridge), then adjacent teeth would predictably have some interproximal soft tissue loss after extraction to a depth of 3 mm to 4 mm.
Orthodontic extrusion of a damaged tooth will not improve the position of the interproximal papilla height. This height is determined by the levels of periodontal attachment to adjacent teeth. When an advanced tooth is removed, the external bone height will be increased compared to the level before the advance began, but the interproximal bone height will remain essentially unchanged.
It should be said about the limitations (contraindications) of forced removal; The increase in bone levels and volume is largely dependent on the external condition of teeth Nos. 7 and 10. This is reflected clinically in the improved soft tissue contours of the face as a result of implant restoration of teeth Nos. 7 and 10. The forced removal of these two teeth did little to improve interproximal bone height , since it is determined by the levels of attachment to adjacent teeth. This is clearly shown by a review of the radiographs (Fig. 6 and Fig. 7). Pay attention to bone levels after forced removal and retention, and to radiographs after placement of restorations. It can be clearly seen that there was minimal or negligible improvement in soft tissue levels in the interproximal region.
conclusions
The authors analyzed the controlled tooth extrusion portion as a way in which the position of the gingival margin and bone ridge could be repositioned toward the crown before the tooth was extracted. Limitations to the application of this technique were also discussed. This approach can create a greater volume of available bone and soft tissue in the vertical plane without surgical intervention, focusing on isolated deformities in preparation for implant placement.
Read more about mini-implantation in orthodontics in the online course for orthodontists and surgeons Sergei Popov School of Orthodontics. Module 1. Mini-implantation in orthodontic practice .
http://www.aegisdentalnetwork.com/
