Acute periostitis. Etiology, clinic, treatment
Machine translation
Original article is written in RU language (link to read it) .
Remembering the structure of bone, including the jaws, it must be said that the bone is covered with periosteum (another synonymous name is periosteum). Any inflammation of the periosteum, whether serous or purulent, will be called periostitis. If this is inflammation, then it can be acute, chronic, or it can be an exacerbation of a chronic process - a relapse.
Learn more about the treatment of periostitis at the webinar Protocols for the treatment of periodontitis and periostitis .
Summarizing the above, it should be said that periostitis is an inflammation of the periosteum of the alveolar process of the upper jaw, the alveolar process of the lower jaw or the body of the jaw. In this article we will look at the etiology, clinical picture and treatment of acute periostitis.

What is the cause of acute periostitis?
Etiology of acute periostitis
The most common causes of acute periostitis of the jaws are:
- exacerbation of chronic periodontitis;
- suppuration of odontogenic cysts;

- alveolitis;
- difficult eruption of 3 molars;

- suppurating odontomas;
- impacted, semi-impacted teeth;
- complex tooth extraction;
- as a result of poor quality endodontic treatment;
- jaw injury.
It has been established that in a quarter of patients with periostitis of the jaw, the source of infection is aerobes - in most cases these are gram-positive streptococci and staphylococci, in the rest - non-clostridial anaerobes.
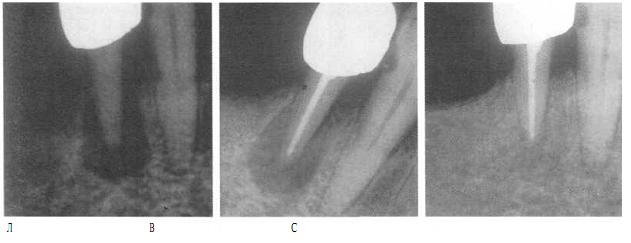
Mechanism of development of acute periostitis
The mechanism of development of acute periostitis can be explained as follows. Let's say we have a focus of inflammation around the tops of the roots of the tooth or in the canals of the tooth. The exudate that forms is serous at first, but after a while it will become purulent and will seek a way out. The exit can be either through a gum pocket or through open canals in the teeth. But if there is no outlet for the outflow of exudate, then the exudate will spread towards the periosteum, filling small holes in the alveolar plate and osteon canals. This is the first way exudate enters the periosteum, as a result of which periostitis occurs.
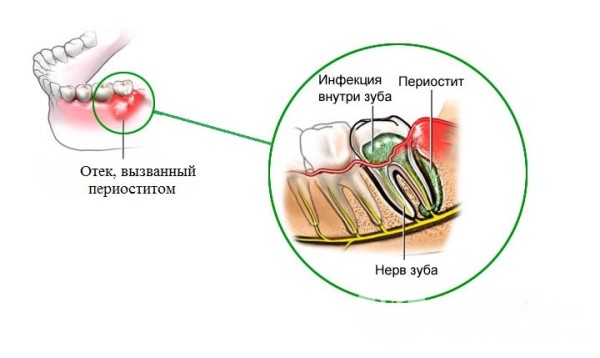
The second mechanism for the development of acute periostitis is the lymphogenous or hematogenous route. The infection will enter the periosteum through blood vessels or lymphatic vessels. This type of periostitis is not odontogenic. The cause of acute periostitis of the jaws will not be related to the teeth. More often, the causes of this type of acute periostitis will be:
- otitis,
- sinusitis,
- measles and scarlet fever,
- complication of acute respiratory viral infection.
Lymphogenous and hematogenous acute periostitis is more common in childhood.
Classification of acute periostitis
In the classification of acute periostitis, the following points should be highlighted. Due to the occurrence of acute periostitis:
- odontogenic periostitis;
- lymphatic periostitis;
- hematogenous periostitis;
- traumatic periostitis.
According to the course of acute periostitis:
- serous periostitis of the jaws;
- purulent periostitis of the jaws.
By process distribution:
- limited periostitis of the jaws;
- diffuse periostitis of the jaws.
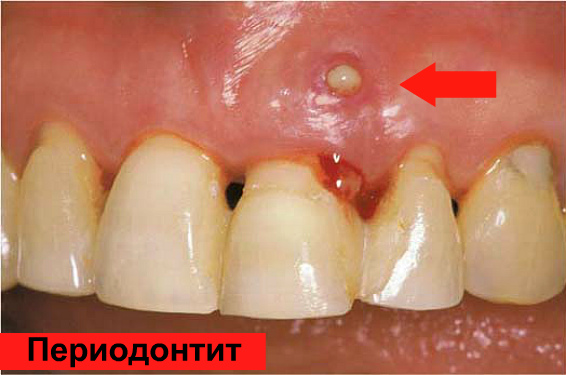
Clinical picture of acute periostitis
The clinical picture, or rather its severity, depends on the following factors:
- state of local and general immunity;
- presence of concomitant diseases;
- microflora, its virulence (the ability of a microorganism to infect);
- age of the patient (periostitis occurs more often in old age);
- type of inflammatory reaction;
- localization of the source of inflammation.
Patients with developed periostitis of the jaw the day before had either hypothermia/overheating, stress, tension, or prolonged intense exercise.
Periostitis can occur in both the upper and lower jaws. In the upper jaw, the most common cause of acute periostitis is a focus of inflammation, which is localized near the first molars (1.6 and 2.6 teeth); in the lower jaw, the most common causative teeth are (by reducing the incidence of acute periostitis):
- 3.6 and 4.6 teeth;
- 3.8 and 4.8 teeth;
- 3.7 and 4.7 teeth.
In approximately 30% of cases, the cause of acute periostitis of the mandible is the first permanent molars of the mandible.
Complaints in acute serous periostitis
Acute serous periostitis is observed in the first 2-3 days of the disease. Patients note:
- intense pain that is felt constantly;
- swelling of the cheeks, lips.
Clinically
- a damaged tooth (either not treated or a filling of poor quality);
- periodontal pocket;
- smoothness of the transition fold;
- pain when percussing the “causal tooth”;
- when cutting the mucosa and periosteum, we can say that the periosteum is infiltrated and hyperemic;
- If left untreated, serous periostitis turns into purulent periostitis.
Complaints with purulent periostitis, which is limited (that is, the processes of the jaws are affected)
- intense pain;
- soft tissue swelling;
- violation of general condition (weakness, fatigue, elevated body temperature);
- pain when touched;
- pain when percussing the “causal tooth”.
Complaints with purulent diffuse periostitis (that is, the body of the jaw is affected):
- intense pain;
- soft tissue swelling;
- violation of general condition (weakness, fatigue, malaise, chills, high body temperature);
- pain when touching tongue:
- pain when percussing the “causal tooth”;
- irradiation of pain along the branches of the trigeminal nerve;
- dense, painful lymph nodes.
The doctor will notice a hyperemic, smoothed transitional fold, destroyed/half-destroyed teeth, and periodontal pockets.
Causal teeth play an important role in the clinic of acute periostitis. Depending on their location, the clinical manifestations of edema vary. With periostitis from teeth 1.3 and 2.3, swelling spreads to the infraorbital region; if the cause of acute periostitis is an odonotogenic infection from the incisors, then the upper lip and wings of the nose will be more swollen.

When the purulent process moves to the periosteum from the large molars of the upper jaw, swelling can affect not only the buccal and zygomatic areas, but also the parotid area.

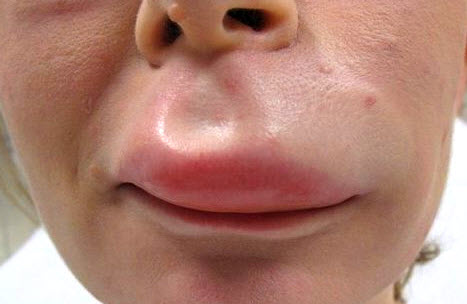
We will also look at the spread of swelling from the teeth in the lower jaw:
- from the incisors and canines on the lower jaw, swelling spreads to the chin area and lower lip;
- from large molars - to the cheek, chin and parotid areas.


The amount of edema depends on the type of structure of the vascular (venous) system; if it is finely looped, then the edema will be insignificant. With a large venous system, in the area of the tubercle and body of the jaw, the swelling will be greater.
It should be emphasized that in acute periostitis, the purulent focus can be localized on both the vestibular and oral surfaces.
If purulent periostitis is localized on the lingual side, patients experience pain when eating, talking, or opening the mouth. Clinically noted:
- swollen tongue covered with plaque;
- the tongue is often raised and turned in the healthy direction;
- it is painful for the patient to move it;
- the hyoid ridge is enlarged, protruding above the tongue and alveolar process;
- if the lesion has spread from the lower wisdom teeth to the pterygomaxillary fold or the anterior palatal arches, then pain when swallowing is determined.
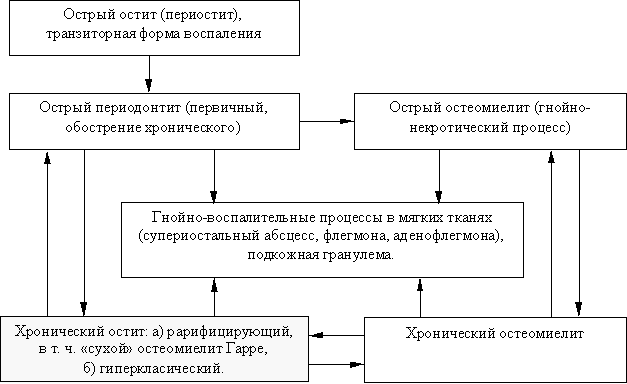
Differential diagnosis of acute periostitis
Differential diagnosis of acute periostitis should be carried out with:
- aggravated chronic periodontitis;
- inflammation of the sublingual and submandibular glands;
- acute odontogenic osteomyelitis;
- acute nonodontogenic lymphadenitis.
The difference between acute periostitis and aggravated chronic periodontitis is that in acute periostitis, the source of inflammation most often affects a group of teeth, and aggravated periodontitis occurs in only one tooth.
With aggravated periodontitis, there are no symptoms that characterize acute periostitis:
- Facial asymmetry.
- Swelling of soft tissues.
- Pain on palpation.
Differential diagnosis
- In acute periostitis, the salivary glands are not involved in the pathological process. If a cloudy or purulent exudate is released from the mouths of the salivary glands, this indicates a pathological process in the salivary glands themselves.
- You can differentiate between acute periostitis and acute osteomyelitis by Vincent’s symptom, which is characteristic only of acute osteomyelitis (pain in the lower lip or chin, or a combination of these signs);
- In acute nonodontogenic lymphadenitis, there are no reactions from the dental system. That is, there will be no clinical signs in the oral cavity.
Treatment of acute periostitis
Treatment of acute serous periostitis
To treat acute serous periostitis, the causative tooth should be removed, the symptoms will disappear on their own. The patient may be prescribed physical therapy. Recommended for acute serous periostitis:
- UHF;
- warming compresses;
- fluctuarization;
- helium – neon laser.
Treatment of acute purulent periostitis
Treatment of acute purulent periostitis involves removing the tooth and opening the abscess. An incision is made three teeth long, the mucosa and periosteum are cut along the transitional fold to the bone. The wound is drained. Drainage is installed for 1-2 days.

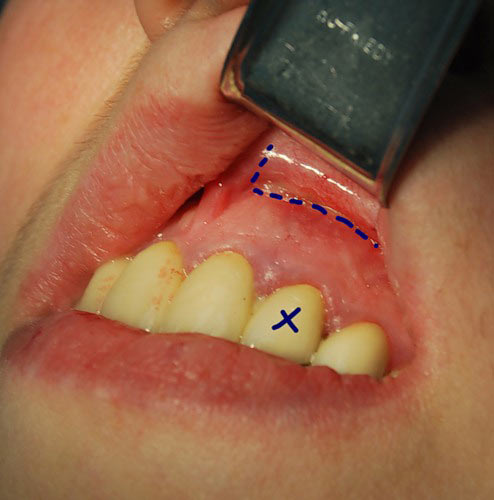
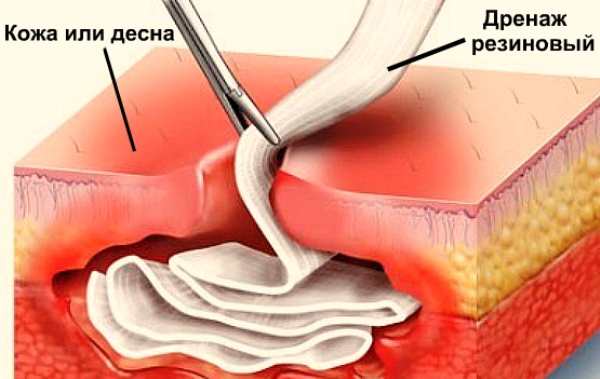
If the incision was made on the hard palate, then it is advisable to excise some triangular-shaped soft tissue. When purulent exudate is localized on the side of the tongue, a linear incision is made just above the transitional fold.
The patient is prescribed antibiotic therapy, restorative therapy, and physical therapy (UHF, helium-neon laser, fluctuarization).
To remove pus as quickly as possible, patients are advised to rinse the mouth with solutions of chamomile, sage, calendula, and potassium permanganate. Solutions must be warm.
To prevent sinusitis, if the periostitis was from large molars in the upper jaw, the patient can be prescribed vasoconstrictor drops/sprays into the nose for 5-6 days.
Treatment for regional lymphadenitis should be prescribed to prevent complications. This can be fluctuarization, UHF, electrophoresis with potassium iodide, magnetic applicators.
Detailed information on this topic in the online course Treatment of inflammatory diseases of the maxillofacial region: new approaches .

