Fully Digital Workflow For Immediate Loading Of Screw-Retained Titanium-Resin Prostheses On Morse Cone Tissue-Level Connectors: 1-Year Post-Loading Results Of A Case Series
Purpose: To evaluate the clinical performance of a fully digital workflow for full-arch prostheses screwed on Morse cone tissue-level connectors at implant installation and not removed.
Materials and methods: In this case series, edentulous patients were rehabilitated with immediately loaded full-arch implant prostheses on Morse cone tissue-level connectors. All procedures were performed using a fully digital protocol. The primary outcome measures were implant and prosthesis survival rates and complications. The secondary outcome measure was peri-implant marginal bone loss.
Results: Nine patients received 52 implants supporting 10 cross-arch titanium-resin prostheses, seven in the lower jaw and three in the upper jaw. One year after prosthesis fitting, no patient dropped out, no implants or prostheses failed, and no biological complication occurred. Only two minor resin chips occurred in two different patients. However, the first two prostheses prefabricated via a fullly digital workflow (to be fitted in two consecutive patients) did not fit on the Morse cone tissue level connectors. The misfit was solved via intra-oral resin relining after abutment removal from the prosthesis, which was screwed directly onto the tissue-level connectors. After these two consecutive misfits, the protocol was changed: a physical intra-oral impression was taken and the other eight cross-arch prostheses were fitted 24 hours after surgery. One year after loading, the mean marginal bone loss at patient level was 0.07±0.02 mm (95% CI: 0.05-0.08).
Conclusions: Fully digital protocols still present various limitations when used in complex rehabilitations.
Introduction
Edentulism remains a serious oral disease with millions of people being impacted by a lack of dentition and consequent functional and aesthetics issues. However, fixed implant-supported prostheses are considered an efficient solution to restore the aesthetics and function of totally edentulous jaws, and significantly improve patients’ quality of life.
Nowadays, there is a growing interest in minimally invasive surgery combined with a fully digital workflow.
A computer-guided surgical-prosthetics protocol offers several clinical benefits, helping clinicians to virtually plan the ideal implant position and direction taking into account the patient’s anatomical structures and the prosthetic parameters.
Likewise, the development of digital dental equipment, such as cone-beam computed tomography, intraoral scanners, and specialized software that allows for virtual implant planning, have improved guided implant placement, making it safer, simpler and more accurate. The fully digital workflow has been developed with the aim of making these procedures more predictable and less invasive, and to require shorter chair-side time and appointments.
To be successful over time, an implant-supported prosthesis needs to respect some requirements, in particular passive fit of the framework, because prosthesis misfit may lead to mechanical and biological complications. As with every method, the fully digital workflow presents some drawbacks, such as a learning curve and costs, but other problems are related to the accuracy of implant placement using a fully digital protocol versus virtual planning and impression taking.
Several authors, including Tahmaseb and Vercruyssen, have revealed a discrepancy between the virtual planning of implant placement and the actual final position in the oral cavity, and the effectiveness of digital impressions for full arches is still unclear. In fact, Zhang, in a review, claimed that the digital full-arch implant impressions using intraoral scanners are not sufficiently accurate for clinical application. Other authors, such as Andriessen or Schmidt, have concluded the same.
In this context, aim of this case series was to evaluate the performance of full-arch prostheses screwed on Morse cone abutments connected at implant installation and not removed, with the entire protocol relying on digital workflow. This study is reported according to the STROBE guidelines (https://www.strobe-statement.org/checklists/).
Materials and methods
Patients were treated at a private centre in Sardinia (Italy) from March 2021 to December 2022. Two experienced clinicians (S.M.M, B.F.) performed all surgical procedures. Two other clinicians (M.P, B.F.) performed all prosthetic treatments. All patients gave their informed written consent to the treatment. Any patient aged 18 years or older, affected by total edentulism or with non-viable dentition, and able to understand and sign informed consent was treated. Patients were not treated if any of the following exclusion criteria applied: American Society of Anesthesiologist (ASA) class III or IV; pregnancy or nursing; alcohol or drug abuse; heavy smoking (>10 cigarettes/day); radiation therapy to head or neck region within 5 years; and/or untreated periodontitis.
Surgical and prosthetic procedures
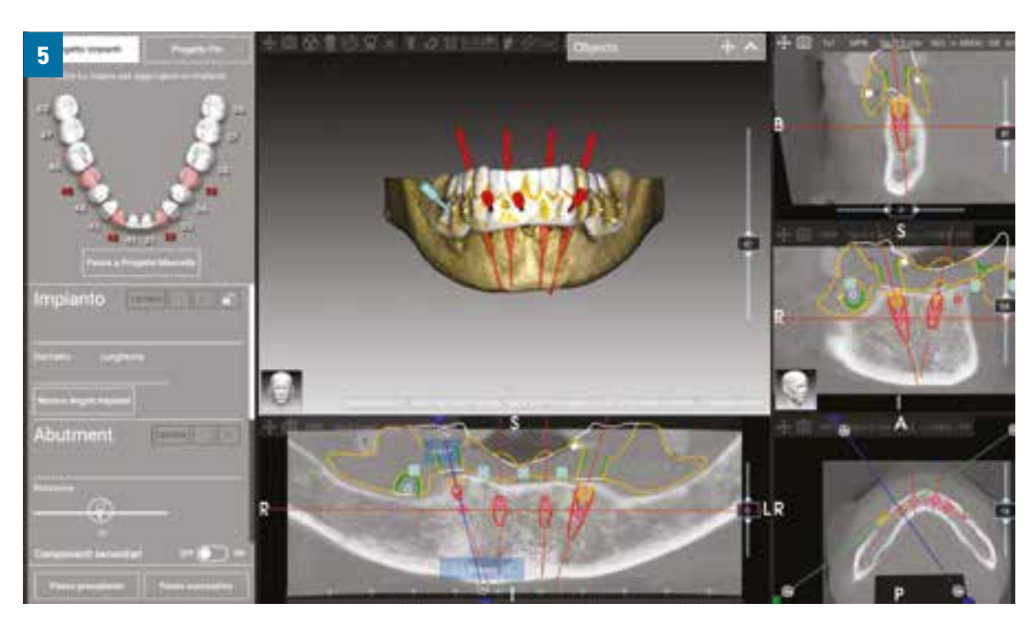
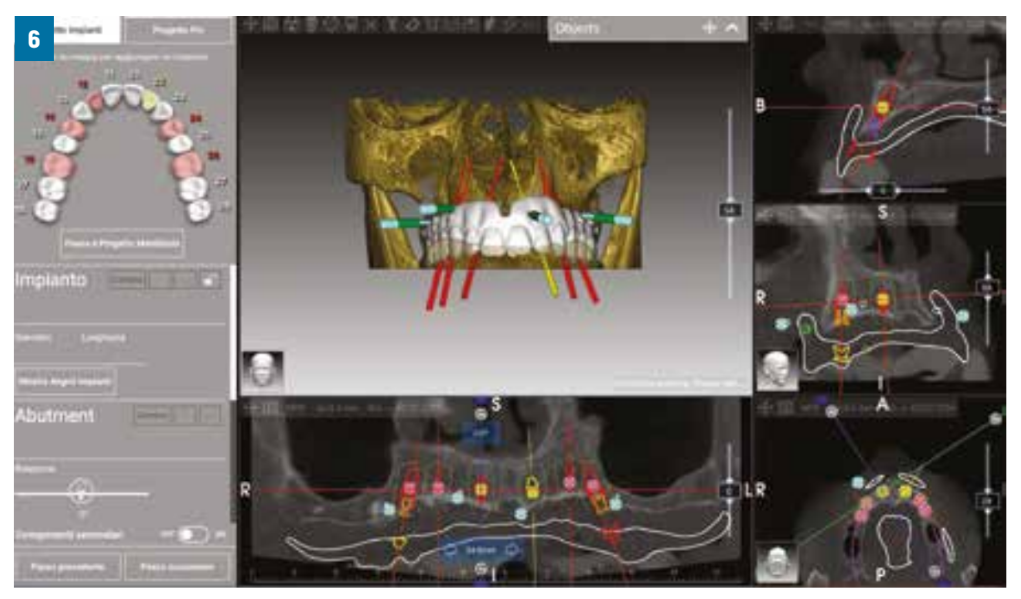
All patients received periapical or panoramic radiographs for initial screening and assessment. The implant-prosthetics workflow began by taking a CBCT scan (Rayscan, Sulzbach, Germany) to plan the correct implant position. After that, a digital model was generated using a CS 3600 intraoral scanner (Carestream Dental, Atlanta, GA, USA). In fully edentulous subjects, a double-scan protocol was ultimately implemented. Specifically, prostheses were made from physical impressions; after that a CBCT scan of the patient was performed with the prosthesis in situ, followed by a single scan of the prosthesis with gutta-percha (Dentsply Sirona Italia, Rome, Italy) reference points to obtain a match between the two datasets (Figs. 1-4). Standard Tesselation Language interface format digital data (STL data) was imported into 3D design software (Exocad DentalCAD, Exocad, Darmstadt, Germany) to generate a virtual wax-up according to the functional and aesthetic requirements and planning. STL and Digital Imaging and Communications in Medicine (DICOM) data were imported into 3D planning software (3Diagnosys, 3P Guide, Version 4.2, 3DIEMME, Cantù, Italy) (Figs. 5, 6).



Patients received 2 g amoxicillin + clavulanic acid (Augmentin, GlaxoSmithKline, London, UK) one hour before surgery and 1 g twice daily for one week thereafter. In the event of penicillin allergy, clindamycin was administered for premedication (600 mg one hour before surgery) and after surgery (300 mg four times a day for one week). Patients were instructed to rinse with 0.2% chlorhexidine solution (Curasept, Curaden Healthcare, Saronno, Italy) for one minute before surgery, and a sterile surgical drape was applied to minimise potential contamination from extra-oral sources. Oral sedation with triazolam 0.50 mg (Triazolam Ratiopharm, Milan, Italy) was given prior to surgery. Local anaesthesia (Septanest with adrenaline, 1/100000, Septodont, Mataró, Spain) was used.
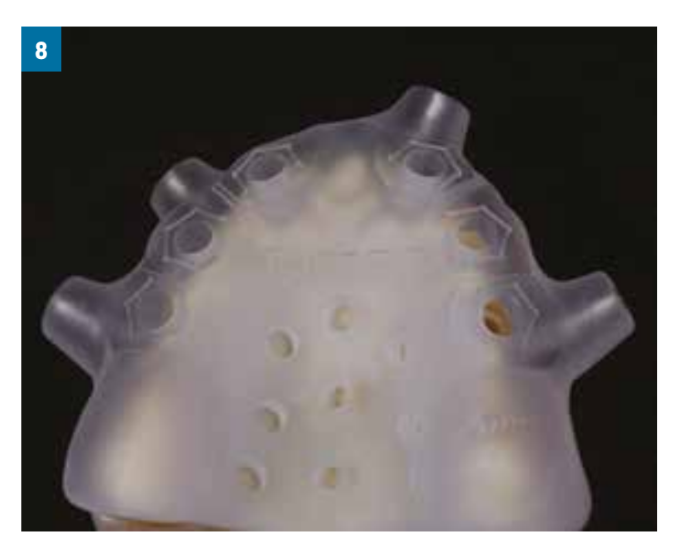
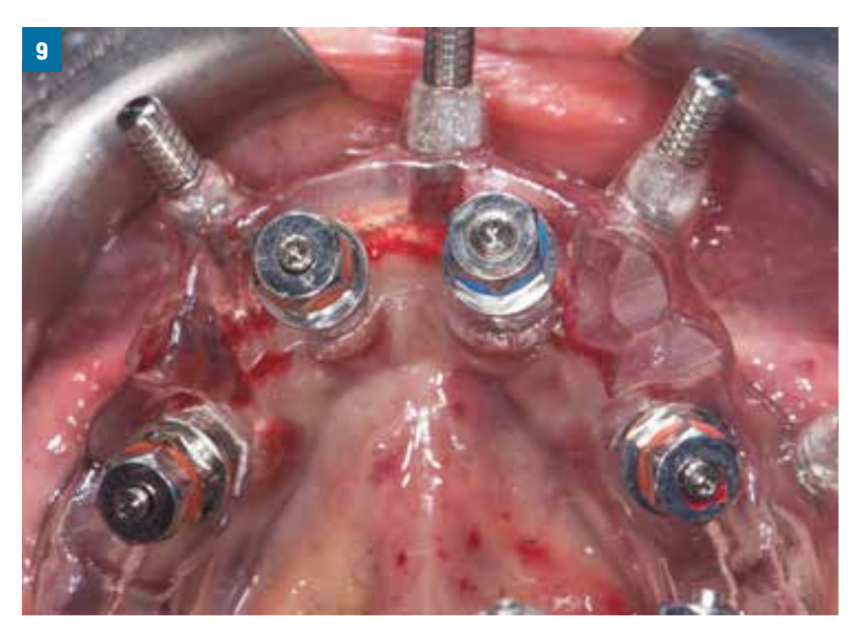
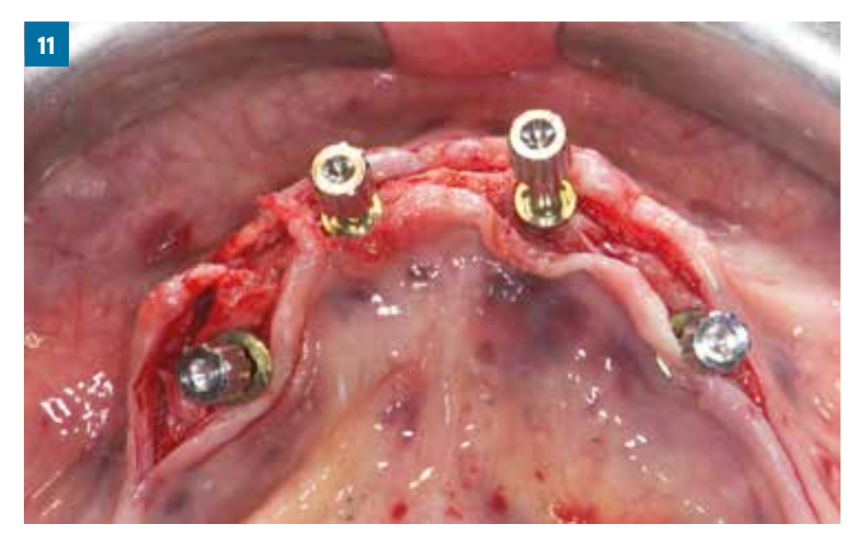
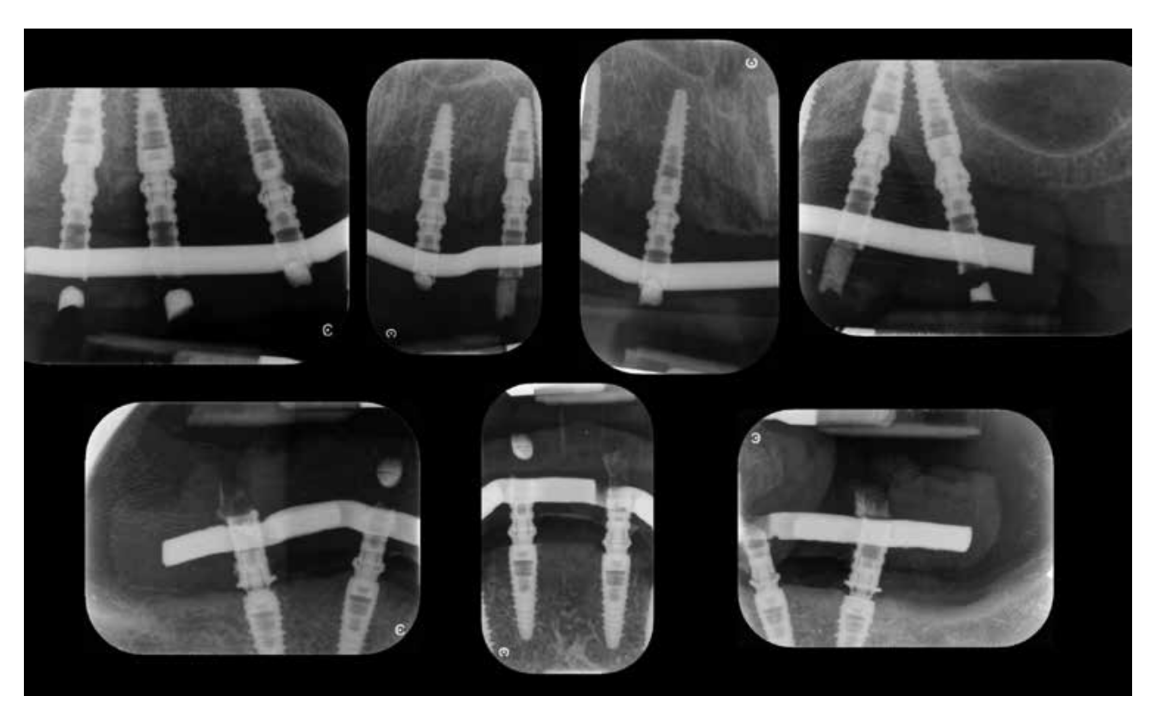
Following the extraction of non-viable teeth, a mid-crestal incision was made into the keratinized tissue using a n. 15 surgical blade, and a full-thickness mini-flap was raised. In three subjects, a flapless protocol was performed. All implants (cono in 3P Implafavourite, Scalegne, Torino, Italy) were installed following a fully guided protocol (Figs. 7, 8). In cases of poor bone density, the implant site was underprepared. All of the implants were inserted with a minimum insertion torque of 35 Ncm 0.0 mm to 1 mm below bone level (Figs. 9, 10). Morse cone tissue level connectors abutment were inserted (TLC base 3P Implafavourite) (Figs. 11, 12). In post-extraction cases, the gap between the implant and the vestibular bone plate was filled with bovine bone (Re-bone, Ubgen, Vigonza, Italy). Flaps were sutured with Vicryl 4-0 sutures (Ethicon J&J International, Sint-Stevens Woluwe, Belgium). Immediate loading was to be performed with a prefabricated titanium resin prosthesis (Figs. 13, 14). Afterwards, all patients received oral and written recommendations about medication, oral hygiene maintenance with an antiseptic agent (0.2% chlorhexidine, CURASEPT, Curaden) and diet. Patients were recalled every three months until one year after loading.




connectors

Outcome measures
Implant and prosthesis survival rates and complications were the primary outcome measures.
- Implant failure: any removal of implants dictated by implant mobility, progressive marginal bone loss, infection or implant fracture.
- Prosthesis failure: any prosthesis redone for any reason.
Surgical complications, such as infection or intraoperative or postoperative issues, prosthetic complications (e.g., fractures, chipping, abutment mobility, prefabricated prosthesis not fitting) and biological complications (wound or implant infection, mucositis, abscesses or peri-implantitis) were recorded. Complications were assessed and treated by the same clinicians who originally treated the patients.
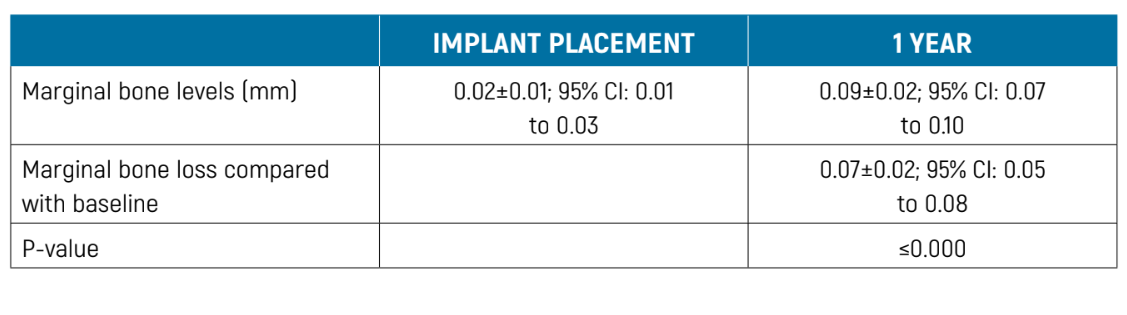
The secondary outcome measure was peri-implant marginal bone loss. This was calculated on digital periapical radiographs taken with the paralleling technique using a film-holder (Rinn XCP, Dentsply, Elgin, Illinois, USA) at both implant placement/loading (baseline) and one year after loading. The radiographs were accepted or rejected for evaluation based on the clarity of the implant threads. The distance from the most coronal margin of the implant collar to the most coronal point of bone-to-implant contact was calculated. All readable radiographs were displayed using image analysis software (DFW2.8 for windows, Soredex, Tuusula, Finland) on a 24-inch LCD screen (iMac, Apple, Cupertino, CA, USA) and evaluated under standardised conditions (SO 12646: 2004). The software was calibrated for each single image using the known distance between two adjacent implant threads. Measurements of the mesial and distal bone crest level adjacent to each implant were made to the nearest 0.01 mm and averaged at patient level.
Statistical analysis
All analyses were carried out using SPSS software for Mac OS X (version 22.0; SPSS, Chicago, Illinois, USA). Two dentists (M.T., M.D.) analysed the data. Descriptive analysis was performed for numeric parameters using mean ±SD and 95% confidence interval (CI). The differences in mean marginal bone levels over time were compared using paired t-tests.
Results
Nine patients (three male and six female) with a mean age of 55±3.2 years received 10 titanium-resin full-arch restorations, seven in the lower jaw and three in the upper. All procedures were performed fully guided, and three procedures were carried out flapless. Overall, 52 implants of diameter 4.5, 3.8 or 3.2 mm and length 10 or 13 mm were inserted, and Morse cone tissue-level connectors (TLC bases, 3P Implafavourite) 3.8 mm in diameter and 1.5 or 2.5 mm long were connected.
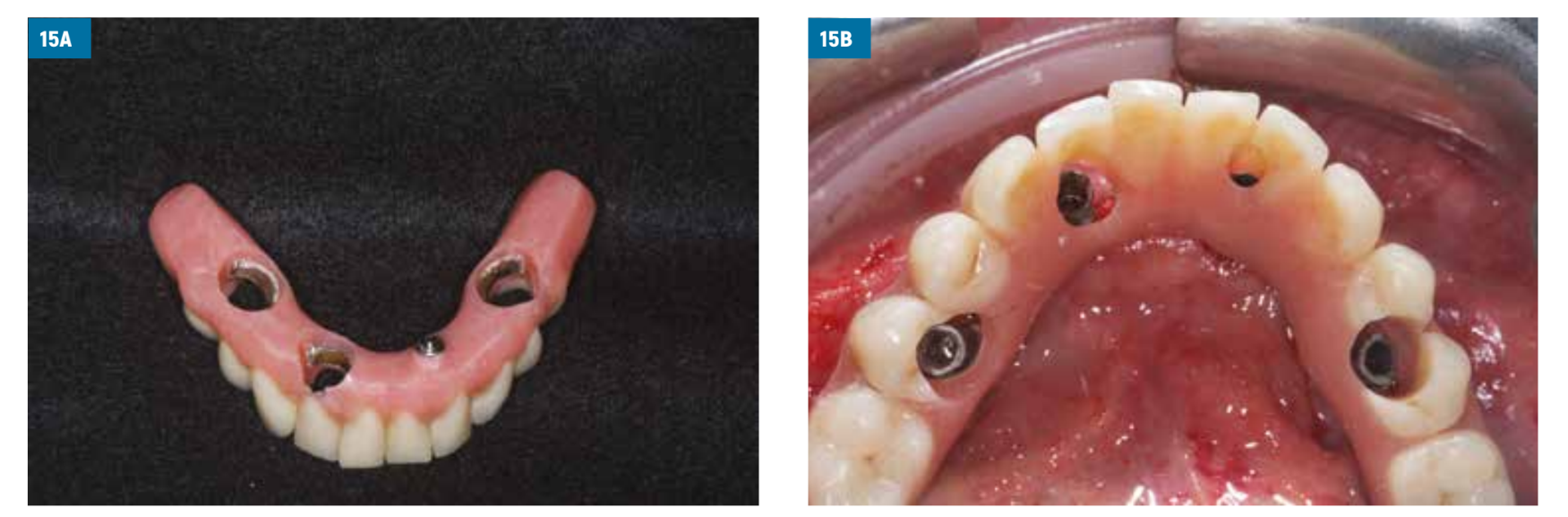
One year after prosthesis delivery no patient had dropped out, no implant or prosthesis had failed, and no surgical or biological complications had arisen. However, the first two prefabricated prosthesis obtained from a fully digital workflow, to be fitted in two consecutive patients, did not fit on the Morse cone tissue-level connectors; the misfit was corrected via intra-oral resin relining after abutment removal from the prosthesis, and screwing the latter directly onto the tissue-level connectors (Figs. 15A, B, 16, 17). After these two consecutive misfits, the protocol was changed: a physical intra-oral impression was taken and the other eight cross-arch prosthesis were fitted 24 hours after surgery (Figs. 18, 19). Only two other biomechanical complications were recorded, both minor, namely two resin chipping events in two different patients; in both cases it was sufficient to rubber polish the resin intraorally.




One year after loading, the mean marginal bone loss at patient level was 0.07±0.02 (95% CI: 0.05-0.08; Table 1) (Fig. 20).
Discussion
The results of this study support the use of computer-guided surgery and minimal bone remodelling around implants with Morse cone connection, but do not support the fitting of prosthesis obtained via a fully digital workflow before surgery. The main concerns emerging from this study are related to the fit of the prefabricated prosthesis. In the first two cases treated, the prosthesis did not fit correctly, and it was necessary to refit the prosthesis intraorally; subsequently the protocol was changed, and loading was performed after 24 hours.
In implant dentistry, the use of digital workflow is quickly developing, with accurate work and a lower number of manual stages in clinical practice. The various stages of treatment may seem easy, but digital workflow has a demanding learning curve and includes possible drawbacks such as inaccurate intraoral scanning, variations in implant position and prostheses misfit. Indeed, in order to obtain an accurate result, it is essential to have knowledge of different software programmes for proper planning. Furthermore, the software programmes used for virtual planning in implantology require several steps that are not always easy to perform, like segmentation, elimination of artefacts, image overlay (DICOM/STL) and virtual implant positioning. Due to this, the presence of numerous complex points during the planning stages could lead to errors and their accumulation, which may result in failure.
One of the first problems observed in a fully digital protocol regards impression taking. Zhang, in a review, showed that full-arch digital implant impressions are not sufficiently accurate for clinical application. Similarly, Andriessen, in a pilot study comparing the effectiveness of digital intraoral scans and preformed cast models showed that the implant distance and angulation errors in the scans were too great to allow fabrication of well-fitting implant structures for edentulous jaws; the main cause of unreliable scans appeared to be the lack of anatomical reference points for scanning.
Regarding surgical technique, however, guided implant surgery is typically quicker than traditional freehand surgery, and results in higher comfort for the patient in the post-operative period. The efficacy of fully guided surgery compared to freehand surgery for implant placement is documented in the literature, and several authors such as Gargallo-Albiol, Varga or Vercruyssen have shown statistically significant differences between different protocols, with fully guided surgery displaying greater accuracy. However, there is an issue regarding the discrepancy between virtual implant position and the real position in the oral cavity. A systematic review conducted by Tahmaseb et al. showed that a discrepancy can exist between the virtual and real positions of the implant amounting to a total mean error of 1.2 mm (1.04 mm to 1.44 mm) at the entry point and 1.4 mm (1.28 mm to 1.58 mm) at the apical point, as well as a deviation of 3.5°(3.0° to 3.96°); nevertheless, they concluded that computerised static implant surgery is accurate, albeit with some errors, and that a safety margin of at least 2 mm must be respected.
In line with these findings, there were errors related to prosthesis fit in our case series when the fully digital protocol associated with computerized static implant surgery was applied; hence, after two consecutive cases of evident prosthesis misfit, the loading protocol was changed to involve an analogue workflow.
We wish to underline that this kind of titanium-reinforced resin screw-retained prosthesis is to be considered a medium-term, temporary prosthesis, especially if intra-orally relined. Often in our clinical practice, we replace these prostheses with polymethylmethacrylate (PMMA) or acrylic resin prostheses on computer-aided design/computer aided manufacturing (CAD/CAM) titanium bar or zirconia-ceramic on CAD/CAM titanium prosthesis after two to three years.
The main limitations of the present study are the fact that it was a case series, without suitable controls, the low number of patients treated, the lack of independent assessment, and the short follow-up. Despite these limitations, the fully guided computer-assisted implant installation proved to be easily applied, and the Morse cone tissue-level connector simplified the fitting of screw-retained prosthesis on implants with Morse cone connection.
It is our opinion that procedures described in this article can be easily managed by dentists with medium-level skills in implant therapy. To rehabilitate edentulous patients, we suggest using a digital workflow and computer assistance for implant placement; however, a fully digital workflow for immediate loading is to be avoided, preferring instead a manual procedure for prosthesis design and loading after 24 hours.
Conclusions
Fully digital protocols still present various limitations when used in complex rehabilitations.
Milena Pisano, Dario Melodia, Marco Tallarico, Aurea Maria Immacolata Lumbau, Edoardo Baldoni, Giovanni Spano
References
- Emami E, De Souza RF, Kabawat M, Feine JS. The impact of edentulism on oral and general health. Int J Dent 2013;498305.
- Meloni SM, Melodia D, Tallarico M, Lumbau AMI, Baldoni E et al. Horizontal and vertical computer guided bone regeneration with slow-resorbing bovine pericardium membrane: case series results one year after loading. Clinical Trials in Dentistry 2022;4(4):12-22.
- Meloni SM, Tallarico M, Pisano M. Computer-guided vertical and horizontal bone regeneration with resorbable customized bone laminas filled with 100% particulate autologous bone: a case report. Clinical Trials in Dentistry 2022;4(3):22-32.
- Tahmaseb A, Wismeijer D, Coucke W, Derksen W. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants 2014;29:25-42.
- Mangano F, Gandolfi A, Luongo G, Logozzo S. Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health 2017;17:149.
- Meloni SM, De Riu G, Pisano M, Cattina G, Tullio A, Implant treatment software planning and guided flapless surgery with immediate provisional prosthesis delivery in the fully edentulous maxilla. A retrospective analysis of 15 consecutively treated patients. Eur J Oral Implantol 2010;3(3):245-51.
- Arisan V, Karabuda CZ, Ozdemir T. Implant surgery using bone- and mucosa-supported stereolithographic guides in totally edentulous jaws: surgical and post-operative outcomes of computer-aided vs. standard techniques. Clin Oral Implants Res 2010;21(9):980-8.
- Hultin M, Svensson KG, Trulsson M. Clinical advantages of computer-guided implant placement: a systematic review. Clin Oral Implants Res 2012;23(6):124-35.
- Cicciù M, Tallarico M. Dental implant materials: current state and future perspectives. Materials 2021;14:371.
- Meloni SM, Duvina M, Baldoni E, Tallarico M. Computer guided implant installation and immediate loading of cross-arch fixed dental prosthesis - a 5-year prospective clinical study. Clin Oral Impl Res 2018;29:97-97.
- Putra RH, Yoda N, Astuti ER, Sasaki K. The accuracy of implant placement with computer-guided surgery in partially edentulous patients and possible influencing factors: a systematic review and meta-analysis. J Prosthodont Res 2022;66(1):29-39.
- D’haese J, Van De Velde T, Komiyama A, Hultin M, De Bruyn H. Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: a review of the literature. Clin Implant Dent Relat Res 2012;14:321-35.
- Eckert SE, Meraw SJ, Cal E, Ow RK. Analysis of incidence and associated factors with fractured implants: a retrospective study. Int J Oral Maxillofac Implants 2000;15(5):662-7.
- Vinci R, Manacorda M, Abundo R, Lucchina AG, Scarano A et al. Accuracy of edentulous computer-aided implant surgery as compared to virtual planning: a retrospective multicenter study. J Clin Med 2020;9:774.
- Shaikh M, Lakha T, Kheur S, Qamri B, Kheur M. Do digital impressions have a greater accuracy for full-arch implant-supported reconstructions compared to conventional impressions? An in vitro study. J Indian Prosthodont Soc 2022;22(4):398-404.
- Tahmaseb A, Wu V, Wismeijer D, Coucke W, Evans C. The accuracy of static computer-aided implant surgery: a systematic review and meta-analysis. Clin Oral Implants Res 2018;29(16):416-35.
- Vercruyssen M, Cox C, Naert I, Jacobs R, Teughels W, Quirynen M. Accuracy and patient-centered outcome variables in guided implant surgery: a RCT comparing immediate with delayed loading. Clin Oral Impl Res 2016;27:427-32.
- Zhang YJ, Shi JY, Qian SJ, Qiao SC, Lai HC. Accuracy of full-arch digital implant impressions taken using intraoral scanners and related variables: a systematic review. Int J Oral Implantol (Berl) 2021;14(2):157-79.
- Andriessen FS, Rijkens DR, Van der Meer WJ, Wismeijer DW. Applicability and accuracy of an intraoral scanner for scanning multiple implants in edentulous mandibles: a pilot study. J Prosthet Dent 2014;111(3):186-94.
- Schmidt A, Klussmann L, Wöstmann B, Schlenz MA. Accuracy of digital and conventional full-arch impressions in patients: an update. J Clin Med 2020 4;9(3):688.
- Monaco C, Scheda L, Ciocca L, Zucchelli G. The prototype concept in a full digital implant workflow. J Am Dental Assoc 2018;149(10):918-23.
- Tatakis DN, Chien HH, Parashis AO. Guided implant surgery risks and their prevention. Periodontol 2000 2019;81(1):194-208.
- Kihara H, Hatakeyama W, Komine F, Takafuji K, Takahashi T et al. Accuracy and practicality of intraoral scanner in dentistry: a literature review. J Prosthodont Res 2020;64(2):109-13.
- Sommacal B, Savic M, Filippi A, Kühl S, Thieringer FM. Evaluation of two 3D printers for guided implant surgery. Int J Oral Maxillofac Impl 2018;33(4):743-6.
- Hämmerle CH, Stone P, Jung RE, Kapos T, Brodala N. Consensus statements and recommended clinical procedures regarding computer-assisted implant dentistry. Int J Oral Maxillofac Impl 2009;24:126-31.
- Jaemsuwan S, Arunjaroensuk S, Kaboosaya B, Subbalekha K, Mattheos N, Pimkhaokham A. Comparison of the accuracy of implant position among freehand implant placement, static and dynamic computer-assisted implant surgery in fully edentulous patients: a non-randomized prospective study. Int J Oral Maxillofac Surg 2023;52(2):264-71.
- Gargallo-Albiol J, Barootchi S, Marqués-Guasch J, Wang HL. Fully guided versus half-guided and freehand implant placement: systematic review and meta-analysis. Int J Oral Maxillofac Implants 2020;35(6):1159-69.
- Varga E Jr, Antal M, Major L, Kiscsatári R, Braunitzer G, Piffkó J. Guidance means accuracy: a randomized clinical trial on freehand versus guided dental implantation. Clin Oral Implants Res 2020;31(5):417-30.
- Vercruyssen M, Cox C, Coucke W, Naert I, Jacobs R, Quirynen M. A randomized clinical trial comparing guided implant surgery (bone- or mucosa-supported) with mental navigation or the use of a pilot-drill template. J Clin Periodontol 2014;41(7):717-23.
