Clinical Considerations on Strategies That Avoid Multiple Connections and Disconnections of Implant Abutments
Typically, healing or temporary abutments are connected and disconnected several times between implant placement and definitive restoration delivery, and soft tissue disruption occurs each time the abutment is disconnected and reconnected. This histologic event is supposed to cause bone resorption around the implant after second-stage surgery. To minimize this clinical scenario, immediately placing and never removing a definitive abutment the day of implant insertion (one-stage protocol) or at second-stage surgery in cases of submerged implants (two-stage protocol) was suggested. This paper details the prosthetic protocol and presents strategies and rationales for placing a definitive abutment the day of implant insertion or at second-stage surgery with cement- and screw-retained restorations.
This protocol seems to be an efficient strategy to preserve peri-implant hard and soft tissues. However, positive outcomes in peri-implant bone and soft level changes should be viewed with caution, as their clinical significance is still uncertain.
Absence of bone level changes around two-piece dental implants should represent, in the short and long term, the final aim of any therapy where implants are employed. However, longitudinal studies have demonstrated that this might represent a clinical illusion.
The implant-abutment interface in two-piece implants is typically placed at the alveolar crest or slightly below. Similar to natural teeth, a biologic width is established around implants. Furthermore, a wide array of factors may potentially contribute to the extent of early bone remodeling. Among them, implant-abutment connection, implant position, collar macro-design, and implant placement protocol seem to be influential on the initial bone remodeling at the time of implant insertion. Depending on the protocol used, the healing or prosthetic abutments may have to be disconnected several times during the prosthetic phases. The microgap between these two components, as well as the disruption of the soft tissue that occurs each time the abutment is disconnected and reconnected, are supposed to cause bone resorption around the implant after second-stage surgery. To minimize the number of abutment disconnections, immediately placing and never removing a definitive abutment the day of implant insertion (one-stage protocol) or at second-stage surgery in cases of submerged implants (two-stage protocol) (sometimes called the “one-abutment/one-time” approach) was suggested.
One-year postloading data from a recent systematic review and meta-regression analysis of the included RCTs showed that repeated disconnection and reconnection statistically significantly increased peri-implant bone loss and buccal recession by 0.279 mm and 0.198 mm, respectively. This result is also in agreement with a recent open-cohort prospective study on sandblasted and acid-etched bone-level implants featuring an 11-degree Morse taper connection. Sublevel analysis showed that placing a definitive abutment the day of implant insertion and never removing it statistically reduced the marginal bone remodeling in the first year after loading. On the other hand, many of that study’s authors pointed out that no clinical difference (ie, soft tissue recession) was noted in the time frame of the study.
Moreover, placement of a customized definitive or stock abutment at the time of implant placement should be carefully considered in cases in which more apically positioned restorative margins are needed, due to the difficulty in removing the deeply positioned residual excess cement. Finally, there might be some clinical situations where it is not possible to predict the amount of soft tissue shrinkage.
Hence, the present paper aims to detail the clinical and technical steps for placing a definitive abutment, which does not need to be removed afterwards, on the day of implant insertion.
Strategies and Rationales for Implant Restorations
For Cement-Retained Restorations
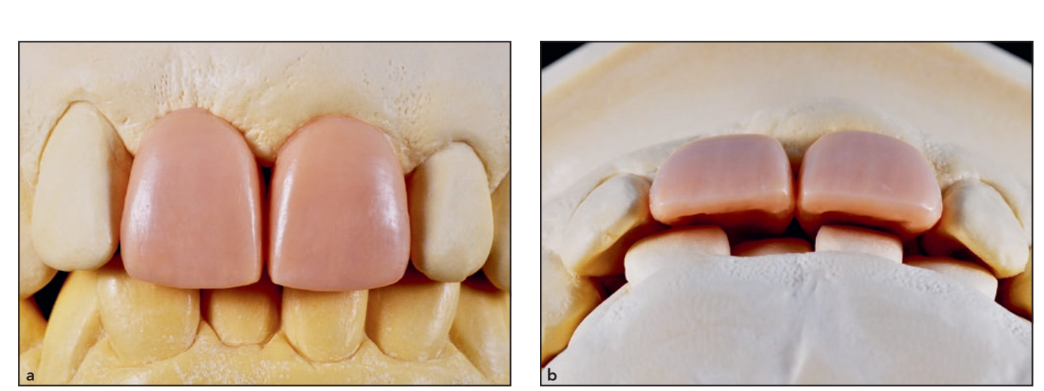
Procedures for cemented implant reconstructions clinically and technically resemble procedures used for tooth-borne reconstructions. The use of a customized shoulderless abutment is key during this protocol since there is doubtlessly a difficulty in previewing the final soft tissue contour and therefore the right position for a traditional horizontal finish line. Using this concept, the soft tissue contouring of the provisional restoration is essential to sculpt the soft tissue margin.
For Screw-Retained Restorations
The convenience and advantages of fabricating screw-retained restorations employing prefabricated titanium abutments have been well documented. The major benefit of screw-retained reconstructions is their retrievability; however, more technical problems were documented. Typically, either straight or angulated abutments have been used to bring the crown-abutment interface to an accessible level and to correct a prosthetically unfavorable implant axis. The main issue of utilizing the screw-retained restoration protocol in the “one- abutment/one-time” approach is that these components do not have an anti-rotation feature and thus were designed for multiple splinted restorations. Recently, multiple manufacturers have introduced a similar component for single units.
Clinical Procedures and Description of Techniques
- Once the clinical case is analyzed (Fig 1), a careful design of the final crown (with defined soft tissue architecture and prosthetic emergence profile) is obtained by the dental technician from diagnostically waxed casts, allowing for the fabrication of a radiologic/surgical stent for optimal positioning and angulation of the planned implant (Fig 2).
- At the time of surgery, a single dose of antibiotics (2 g of amoxicillin or 600 mg of clindamycin if allergic to penicillin) is administered; the patient then rinses with 0.2% chlorhexidine for 1 minute.
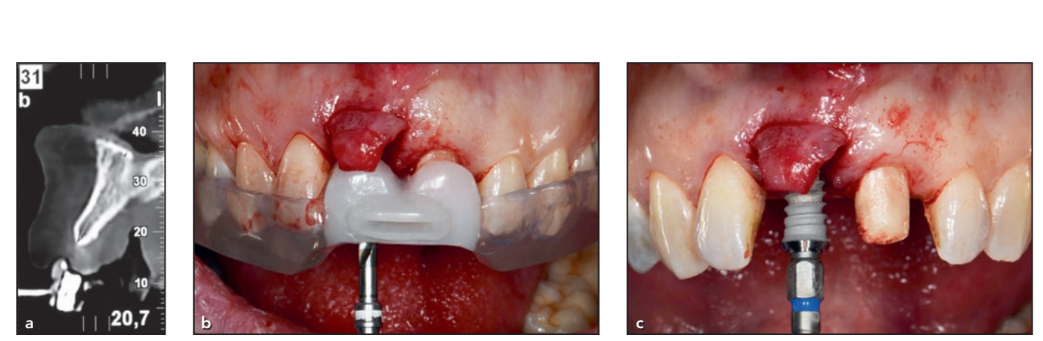
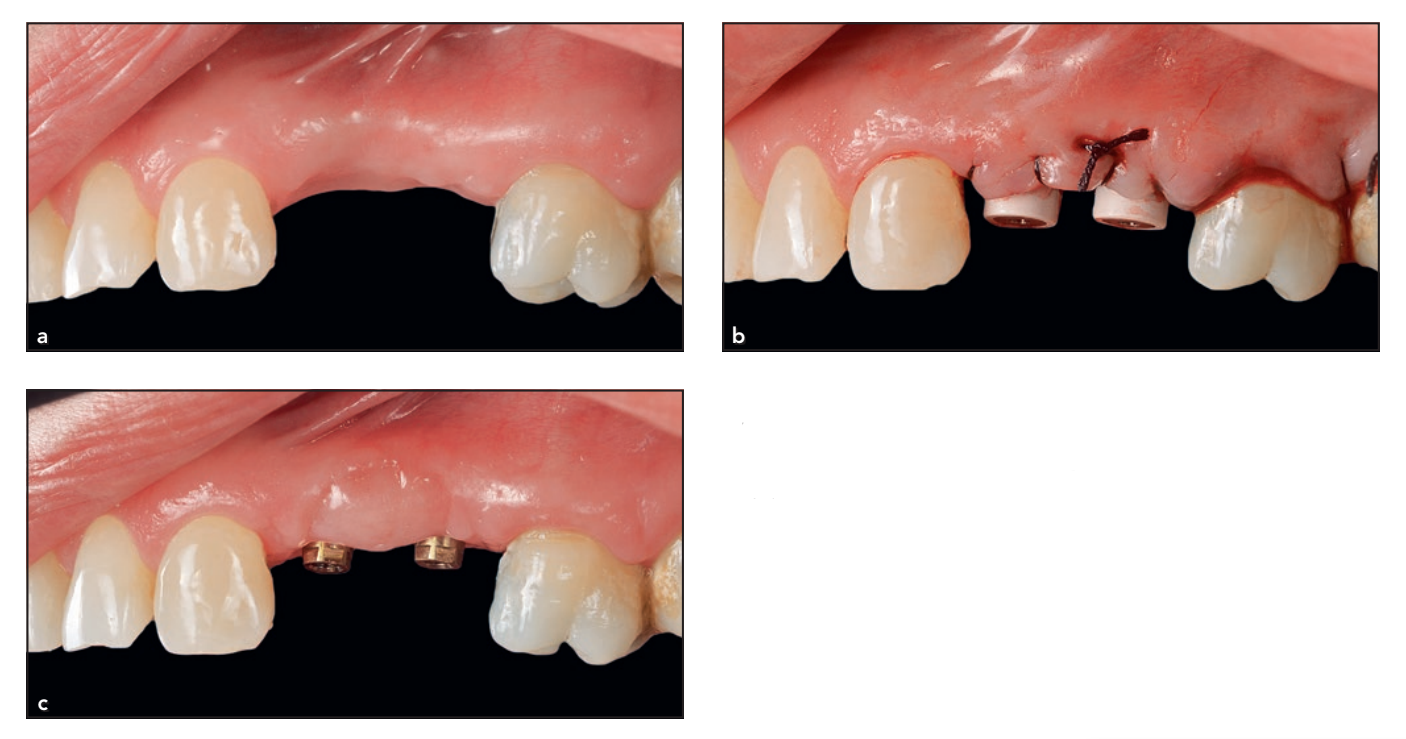
- The implant is placed flapless (after using soft tissue punches) or with a minimally invasive flap (with papilla preservation). The flap can be extended for regenerative procedures, if needed. Once the bone crest has been exposed, implant placement is performed using either computer-guided templates or conventional surgery (Fig 3).

For Cement-Retained Implant Restorations
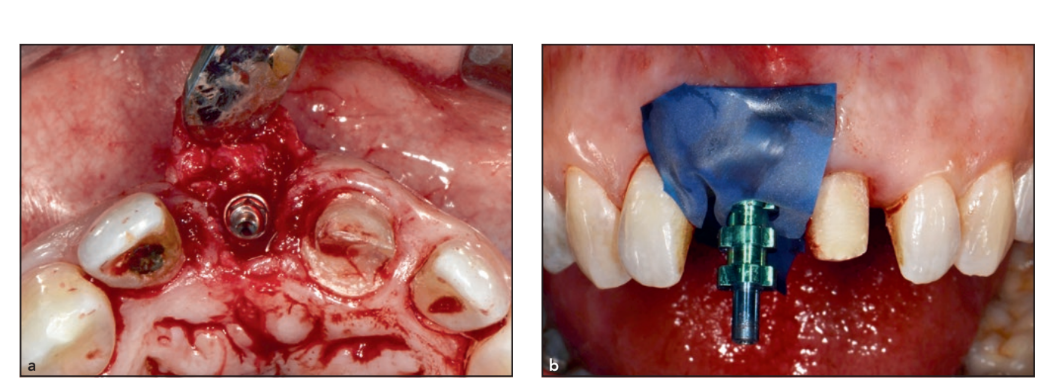
- For a two-stage protocol, a conventional or digital impression is taken immediately after implant placement, allowing the dental technician to fabricate the definitive abutment and the temporary restoration during osseointegration (Fig 4). Finally, the flap is closed. For immediate loading or at second-stage surgery, a titanium or zirconia definitive abutment is screwed directly on the implant, with pros- thetic screws tightened to 30 Ncm, on the day of surgery.
- The abutment can be stock or computer-aided design/ computer-assisted manufactured. A prosthetic stent could be advantageous for abutment positioning. Cleaning, decontamination, and sterilization of the abutment are performed before insertion. A prefabricated, non-occlusal, cemented temporary acrylic restoration is delivered. Then, the flap is closed around the abutment. Finally, occlusion and oral hygiene are carefully checked (Fig 5).
- Afterwards, patients receive oral and written recommendations for medications, oral hygiene maintenance protocols, and diet.
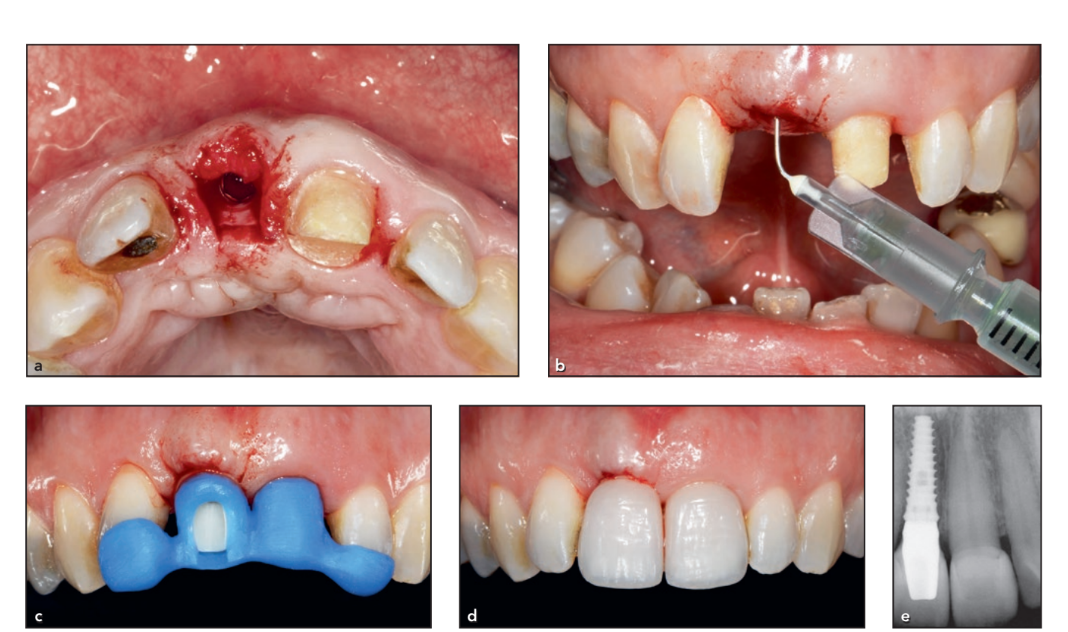
- Once the soft tissues mature, a pre-fabricated plastic transfer coping is inserted with firm finger pressure over the abutment (snap-on technique; Fig 6). A polyvinyl siloxane impression is taken using a conventional closed tray. A 00- or 000-size retraction cord (Ultrapack, Ultradent Products) impregnated with 0.9% sodium-chloride solution is used for mucosal displacement. A previously duplicated polyurethane abutment is repositioned in the plastic transfer coping. Afterwards, a definitive crown can be fabricated.
- Before cementation, a thin layer of petroleum jelly (Vaseline, Unilever) is applied over the external marginal contour of the restoration and to the adjacent teeth to reduce cement adhesion over the external surface and to facilitate removal of excess cement. The final restoration is cemented using a glass-ionomer cement (Ketac Cem, 3M ESPE).
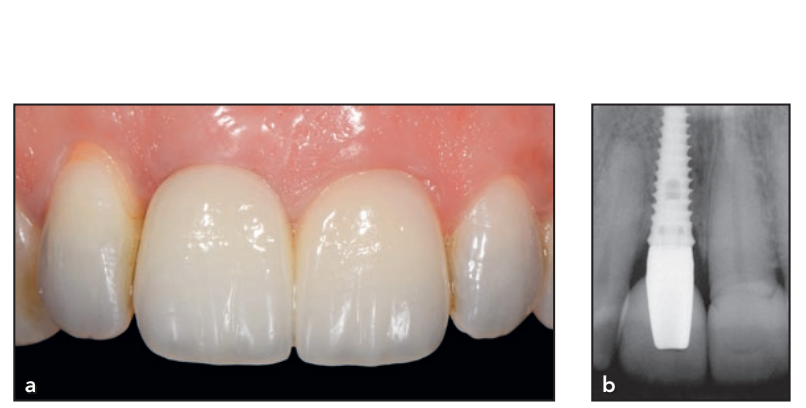
- After 7 minutes of setting, the excess cement is removed and the patient is clinically and radiographically inspected (Fig 7).
- All patients are then enrolled in a standard implant recall program. Oral hygiene maintenance is checked and radiographs are taken early after final prosthesis delivery. Occlusion has to be checked at every appointment (Fig 8).


For Screw-Retained Implant Restorations
- For an immediate/early loading protocol or at second-stage surgery, transmucosal stock abutments of correct gingival cuff height and angulation are screwed directly on the implant with prosthetic screws, tightened at the torque setting recommended by the manufacturer (Fig 9). After an impression (Fig 10), a prefabricated, non-occlusal, screw-retained temporary acrylic restoration is delivered. Finally, occlusion and oral hygiene are carefully checked.
- Afterwards, patients receive oral and written recommendations for medications, oral hygiene maintenance protocols, and diet.
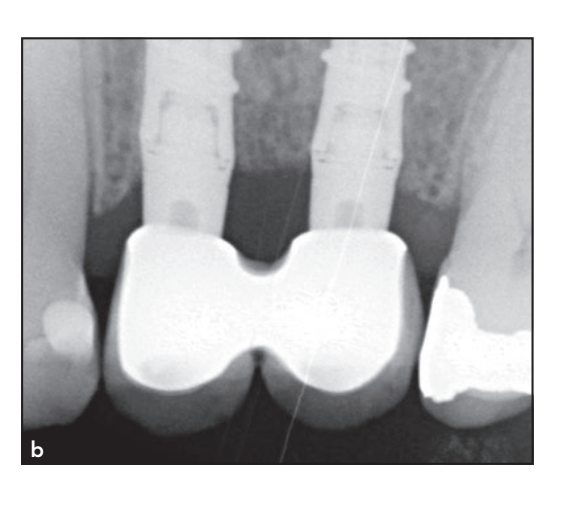
- Once the soft tissues mature, the definitive transmucosal abutments are re-screwed at the torque setting recommended by the manufacturer; then, a plaster14 or digital impression15 is taken at the abutment level using a customized open tray.
- After the definitive restoration is delivered, the screw access holes are filled with Teflon tape and sealed with composite resin. The patient is inspected clinically and radiographically.
- All patients are then enrolled in a standard implant recall program. Oral hygiene maintenance is checked and radiographs are taken early after final prosthesis delivery. Occlusion has to be checked at every appointment (Fig 11).


Discussion
The use of definitive abutments never removed after placement at implant insertion has been suggested as an effective strategy to preserve peri-implant hard and soft tissues. A recent systematic review analyzing only short-term studies concluded that multiple abutment disconnections/reconnections have a modest effect (0.19 mm) on marginal bone level changes. Another systematic review highlighted even better bone level maintenance when longer follow-ups were considered.
To explain this clinically significant evidence, several etiologic factors were advocated: microdamages of the connective tissue, microdeformation of the implant connection, and microbiologic contamination.8 The first and probably the most evident reason seems to be related to biologic aspects. Abutment insertion should be considered part of the soft tissue integration of an implant-supported restoration. Every effort to minimize disturbance of the healing phases may prevent connective tissue microdamages and, therefore, apical migration of the epithelium, even when the biologic width is formed.
By this reasoning, disconnections and reconnections of the abutment can disturb the stability of the healing both in the early stage (hemostasis, inflammatory phase, and proliferation phases) and also in the long term (remodeling phase). Indeed, minimizing the number of abutment disconnections by never removing an abutment after its immediate placement was proven to provide peri-implant alveolar bone level stability and avoid continuous soft tissue shrinkage.
Although the biologic explanation of this protocol appears the most relevant, additional biomechanical reasons could be advocated to explain its positive outcomes. In fact, several studies demonstrated that, due to the differences in mechanical strength of different titanium alloys used for the implant and the abutment, continuous disconnections and reconnections might damage the connection.
The main clinical limitation of this technique may be considered the difficulty in previewing the final soft tissue contour—and therefore the margin line—for a traditional abutment. Although the original shapes of the abutment walls and shoulders could be modified chairside to improve parallelism and to place the prosthetic finish line just below the gingival margin, previewing the final soft tissue position is often a taught task. In fact, a customized shoulderless abutment may be a valid option. Using this alternative abutment shape, the soft tissue contouring of the provisional restoration is essential to sculpt the soft tissue margin. The use of this alternative abutment design allows soft tissue adaptation to follow provisional restoration modifications.
An additional clinical option for this approach, particularly for restorations with multiple implants, is the fabrication of a screw-retained restoration that employs prefabricated abutments (ie, the so called multi-unit abutment). This approach requires the early determination of a collar height that remains hidden in the mucosal tunnel but is not too far below the margin, which would result in tissue impingement every time the prosthesis is tried in. Recently, some manufacturers have started to provide ready-made solutions for the fabrication of single crowns screw-retained to a transmucosal abutment, as these had not previously been as readily available.
Given the importance of the connective tissue compartment and the implant-abutment junction position, an additional aspect to be taken into consideration is the abutment surface cleaning.
Finally, it must be highlighted that, although this prosthetic approach was demonstrated to significantly reduce peri-implant bone loss and recession of the gingival margin, these differences could not be considered clinically relevant. Nevertheless, optimization of clinical outcomes is made through small improvements, such as minimally invasive techniques, platform-switching restorations, connection stability, connection decontamination, and abutment cleaning.
Conclusions
Traditionally, the “one-abutment/ one-time” prosthetic approach is based on the use of a definitive abutment placed at implant insertion and never removed. Usually, this is a cement-retained restoration. An intermediate abutment is an alternative clinical option, mostly used for multiple implant restorations, that is screwed in at the time of implant insertion and then finally restored with a screw-retained restoration.
The present prosthetic approach has been suggested as a critical strategy to preserve peri-implant hard and soft tissues. Nevertheless, the favorable outcomes in peri-implant bone level changes should be viewed with caution as their clinical significance is still uncertain.
Luigi Canullo, Marco Tallarico, Stefano Gracis, Xavier Vela, Xavier Rodriguez, Ugo Covani
References
- Doornewaard R, Christiaens V, De Bruyn H, et al. Long-term effect of surface roughness and patients’ factors on crestal bone loss at dental implants. A systematic review and meta-analysis. Clin Implant Dent Relat Res 2017;19: 372–399.
- Cochran DL, Nevins M. Biologic width: A physiologically and politically resilient structure. Int J Periodontics Restorative Dent 2012;32:371–373.
- Bishti S, Strub JR, Att W. Effect of the implant-abutment interface on peri-implant tissues: A systematic review. Acta Odontol Scand 2014;72:13–25.
- Gracis S. Prosthetic and biomechanical factors affecting bone remodeling around implants. Eur J Esthet Dent 2013;8:314–333.
- Albrektsson T, Isidor F. Consensus report of session IV. In: Lang NP, Karring T (eds). Proceedings of the 1st European Workshop on Periodontology. London, England: Quintessence, 1993:365–369.
- Albrektsson T, Canullo L, Cochran D, De Bruyn H. “Peri-Implantitis”: A complication of a foreign body or a man-made “disease.” Facts and Fiction. Clin Implant Dent Relat Res 2016;18:840–849.
- Abrahamsson I, Berglundh T, Lindhe J. The mucosal barrier following abutment dis/reconnection. An experimental study in dogs. J Clin Periodontol 1997; 24:568–572.
- Tallarico M, Caneva M, Meloni SM, Xhanari E, Covani U, Canullo L. Definitive abutments placed at implant insertion and never removed: Is it an effective approach? A systematic review and meta-analysis of randomized controlled trials. J Oral Maxillofac Surg 2018; 76:316–324.
- Tallarico M, Meloni SM. Open-cohort prospective study on early implant failure and physiological marginal remodeling expected using sandblasted and acid-etched bone level implants featuring an 11º Morse taper connection within one year after loading. J Oral Science Rehabilitation 2017;3:68–79.
- Wittneben JG, Joda T, Weber HP, Brägger U. Screw retained vs. cement retained implant-supported fixed dental prosthesis. Periodontol 2000 2017; 73:141–151.
- Sailer I, Mühlemann S, Zwahlen M, Hämmerle CHF, Schneider D. Cemented and screw-retained implant reconstructions: A systematic review of the survival and complication rates. Clin Oral Implants Res 2012;23(suppl 6):s163–s201.
- Tallarico M, Ceruso FM, Xhanari E, Gargari M, Canullo L, Meloni SM. Immediately loaded tilted implants combined with angulated screw channel zirconia abutments in atrophic maxillary patients: A three-year after loading prospective case series study. Oral Implantol 2018;11:106–114.
- Pozzi A, Sannino G, Barlattani A. Minimally invasive treatment of the atrophic posterior maxilla: A proof-of-concept prospective study with a follow-up of between 36 and 54 months. J Prosthet Dent 2012;108:286–297.
- Pozzi A, Tallarico M, Mangani F, Barlattani A. Different implant impression techniques for edentulous patients treated with CAD/CAM complete-arch prostheses: A randomised controlled trial reporting data at 3 year post-loading. Eur J Oral Implantol 2013;6: 325–340.
- Tallarico, Xhanari E, Cocchi F, Canullo L, Schipani F, Meloni SM. Accuracy of computer-assisted template-based implant placement using a conventional impression and scan model or digital impression: A preliminary report from a randomized controlled trial. J Oral Science Rehabilitation 2017;3:8–16.
- Koutouzis T, Gholami F, Reynolds J, Lundgren T, Kotsakis GA. Abutment disconnection/reconnection affects peri-implant marginal bone levels: A Meta-Analysis. Int J Oral Maxillofac Implants 2017;32:575–581.
- Canullo L, Bignozzi I, Cocchetto R, Cristalli MP, Iannello G. Immediate positioning of a definitive abutment versus repeated abutment replacements in post-extractive implants: 3-year follow- up of a randomised multicentre clinical trial. Eur J Oral Implantol 2010;3: 285–296.
- Nevins M, Camelo M, Koo S, Lazzara RJ, Kim DM. Human histologic assessment of a platform-switched osseointegrated dental implant. Int J Periodontics Restorative Dent 2014;34(suppl 3):s71–s73.
- Semper W, Heberer S, Mehrhof J, Schink T, Nelson T. Effect of repeated manual disassembly and reassembly on the positional stability of various implant abutment complexes: An experimental study. Int J Oral Maxillofac Implants 2010;25:86–94.
- Micarelli C, Canullo L, Iannello G. Implant/abutment connection deformation after prosthetic procedures: An in vitro study. Int J Prosthodont 2015;28:282–286.
- Loi I, Di Felice A. Biologically oriented preparation technique (BOPT): A new approach for prosthetic restoration of periodontically healthy teeth. Eur J Esthet Dent 2013;8:10–23.
- Canullo L, Tallarico M, Pradies G, Marinotti F, Loi I, Cocchetto R. Soft and hard tissue response to an implant with a convergent collar in the esthetic area: Preliminary report at 18 months. Int J Esthet Dent 2017;12:306–323.
- Cocchetto R, Canullo L. The “hybrid abutment”: A new design for implant cemented restorations in the esthetic zones. Int J Esthet Dent 2015;10: 186–208.
- Canullo L, Tallarico M, Chu S, Peñarrocha D, Özcan M, Pesce P. Cleaning, disinfection, and sterilization protocols employed for customized implant abutments: An international survey of 100 universities worldwide. Int J Oral Maxillofac Implants 2017;32:774–778.
- Atieh MA, Tawse-Smith A, Alsabeeha NHM, Ma S, Duncan WJ. The “one abutment - one time” protocol: A systematic review and meta-analysis. J Periodontol 2017;32:575–581.

/public-service/media/default/456/3eXLd_671a1f18319d2.jpg)
/public-service/media/default/446/xUzvr_671a187c9aa46.png)
/public-service/media/default/455/zGYoq_671a1ed13fef9.jpg)
/public-service/media/default/454/7jN0r_671a1b5b648ff.jpg)