Platform switching versus regular platform single implants: 5-year post-loading results from a randomised controlled trial
Abstract
Purpose: To compare the clinical and radiographic outcomes of platform switching (PS) and regular platform (RP) implants.
Materials and methods: This study was designed as a randomised controlled split-mouth trial. Eighteen patients, with bilaterally missing single premolars or molars to be restored with implant-supported single crowns, were consecutively enrolled. Implant sites were randomly assigned to be treated according to the PS concept (PS group), or with matching implant–abutment diameters (RP group). A total of 36 implants were placed in healed bone, with an insertion torque between 35 and 45 Ncm, according to a one-stage protocol. All the implants were loaded with a screw-retained provisional crown 3 months after implant insertion. Definitive screw-retained single crowns were delivered 2 months later. Outcome measures were implant and prosthetic survival rates, biological and prosthetic complications, marginal bone level (MBL) changes, pocket probing depth (PPD) and bleeding on probing (BOP). Clinical data were collected at implant placement (baseline), implant loading (3 months later) and at 9, 36 and 60 months after loading.
Results: One patient dropped out after 4 years of follow-up. No implant failed and no prosthetic complications were recorded during the study period. One patient experienced mucosal inflammation with positive BOP (RP group) after 3 months and three patients had bilateral peri-implant mucosal inflammation with positive BOP at 6, 24 and 36 months, respectively. No other biological complications were recorded up to 60 months of follow-up. There were no statistically significant differences between groups for complications (3/18 versus 4/18; P = 1.0). Nine months after loading the mean MBL was 0.93 ± 0.26 mm (95% CI 0.81 to 1.05) for RP implants and 0.84 ± 0.2 mm (95% CI 0.73 to 0.95) for PS implants. No statistically significant difference was observed between the groups (P = 0.18). Thirty-six months after loading, the mean MBL was 1.09 ± 0.3 mm (95% CI 0.95 to 1.24) in the RP group and 1.06 0.24 mm (95% CI 0.94 to 1.17) in the PS group, with no statistically significant difference between groups (P = 0.70). Sixty months after loading the mean MBL was 1.24 ± 0.39 mm (95% CI 1.05 to 1.43) in the RP group and 1.20 ± 0.21 mm (95% CI 1.01 to 1.39) in the PS group, with no statistically significant difference between the groups (P = 0.85). The mean PPD was 2.58 0.58 mm (95% CI 2.32 to 2.84) in the RP group and 2.40 ± 0.72 mm (95% CI 2.21 to 2.59) in the PS group at 60 months follow-up, with no statistically significant difference between the groups (P = 0.49). The mean BOP was 0.90 ± 0.88 (95% CI 0.58 to 1.22) in the RP group and 0.93 ± 0.97 (95% CI 0.51 to 1.35) in the PS group at 60 months of follow-up, with no statistically significant difference between the groups (P = 0.85)
Conclusions: Implants restored according to the PS concept and matching implant–abutment diameters showed comparable clinical and radiographic results up to 5 years after loading.
Introduction
Peri-implant marginal bone loss is unavoidable and is suggested to be related to the establishment of a pathogenic microflora that causes mucosal inflammation and progressive bone resorption. A large number of studies investigating matched-abutment implants reported an initial bone remodelling up to 2 mm during the first year of loading Several factors seem to contribute to this physiological event, including not limited to the implant design, implant–abutment connection and biological width establishment. In addition, bio mechanical stress, position of the implant plat form6 and framework misfit could be negatively involved in this process and eventually affect the physiological peri-implant bone remodelling.
Some clinical trials have shown that implants with platform switching (PS) had significantly less bone resorption compared with diameter-matched traditional implant–abutment connection. The rationale for this approach is to locate the micro-gap of the implant–abutment connection away from the bone-to-implant contact area, suggesting that a switched platform may prevent or reduce the marginal bone loss. Despite initial questionable evidence of a positive effect of the PS concept on marginal bone stability, other studies reported similar outcomes in comparison with the conventional procedure.
An interim 9 months post-loading report from a previous trial conducted by the authors showed that PS and regular platform (RP) implants have similar clinical and radiographic outcomes in single-tooth replacements These data were confirmed by the results from 3 years after loading.
In the present study, the null hypothesis that there are no differences in clinical and radiographic outcomes between PS and RP implants, in single-tooth replacement, has been tested against the alternative hypothesis of differences, up to 5 years after loading. This trial is reported according to the CONSORT statement (http://www.consort-state ment.org) for improving the quality of reporting of parallel-group randomised trials.
Materials and methods
Study design and patient selection
This study was designed as a prospective randomised, controlled, split-mouth trial. Patients were recruited in three different centres between November 2011 and February 2013. The study was conducted in accordance with Helsinki Declaration guidelines and all participants provided writ ten informed consent prior to enrolment. Patients were treated by the same dentist (SM). Data were analysed at the Dentistry Unit of the University Hospital of Sassari, Italy.
Patients were selected according to the following inclusion and exclusion criteria.
Inclusion criteria:
- age ≥ 18 years
- need for a single bilateral implant-supported crown in the posterior area
- stable interocclusal relationship
- residual bone height ≥ 10
- esidual bone wide ≥ 6 mm with at least 5 of keratinised gingiva crestally
- provided written informed consent.
Exclusion criteria:
- general contraindications for implant surgery
- lack of occluding dentition in the area intended for implant placement
- periodontitis
- severe bruxism
- immunosuppression
- previous history of irradiation of the head and neck area
- uncontrolled diabetes
- heavy smoker (> 10 cigarettes/day)
- probing pocket depth (PPD) and/or bleeding on probing (BOP) 25%
- current or past treatment with bisphosphonates
- substance abuse
- psychiatric disorder
- inability to complete a follow-up to 5 years post-loading
- lactation
- implant insertion torque less than 35 Ncm at implant placement.
Clinical procedures
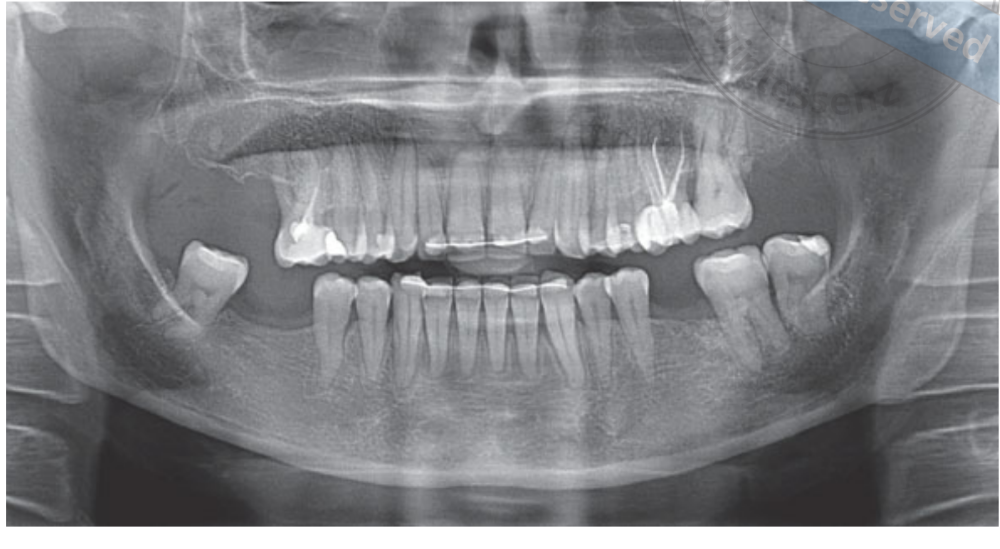
All patients were evaluated clinically and their medical history was recorded. Preliminary screening and radiographs (Fig 1) were performed to evaluate potential patients’ eligibility. Patients who met the selection criteria received oral hygiene treatment and a cone beam computed tomography (CBCT, Imaging Sciences International, Hatfield, PA, USA) scan.
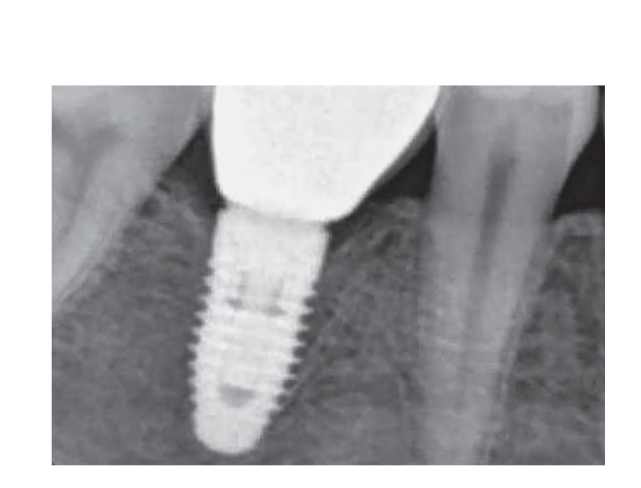
875/125 mg of amoxicillin/clavulanic acid (Augmentin, GlaxoSmithKline, Verona, Italy) were administered twice daily from 1 hour before implant placement to 6 days postsurgery. Prior to implant placement, patients rinsed for 1 minute with 0.2% chlorhexidine (Curasept, Curaden Healthcare, Saronno, Varese, Italy) mouthwash. Local anaesthesia was induced using articaine with adrenaline (1:100,000; Pierrel, Milan, Italy) immediately before surgery. A minimally invasive flap was designed with an intrasulcular and crestal incision, without releasing incisions. Implant drills were used to prepare the implant site according to bone density and the manufacturer’s instructions. Once the implant site was prepared to receive a 4.3- or 5.0-mm diameter implant, the envelope containing a randomisation code to assign the PS and the RP implant site was opened by a blinded independent physician. Implants (NobelReplace Tapered Groovy, Nobel Biocare, Gothenburg, Swe den) with anodised surface were placed with an insertion torque of between > 35 and < 45 Ncm. One site received 8- or 10-mm-long NobelReplace Platform Shift implants, 4.3-mm body diameter with a 3.5-mm (narrow platform [NP], fuchsia) implant–abutment interface, or 5.0-mm body diameter with a 4.3-mm (RP, yellow) implant–abutment interface. The contralateral site received identical implants (RP group) with matching implant–abutment diameters (4.3 mm, yellow; or 5.0 mm, blue; Fig 2). Healing abutments were connected to implants at the time of surgery. Flaps were sutured with Vicryl 4.0 sutures (Vicryl, Ethicon J&J International, Sint-Stevens-Woluwe, Belgium).

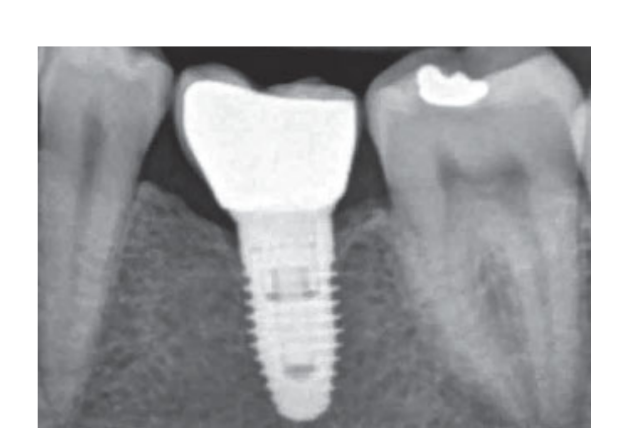
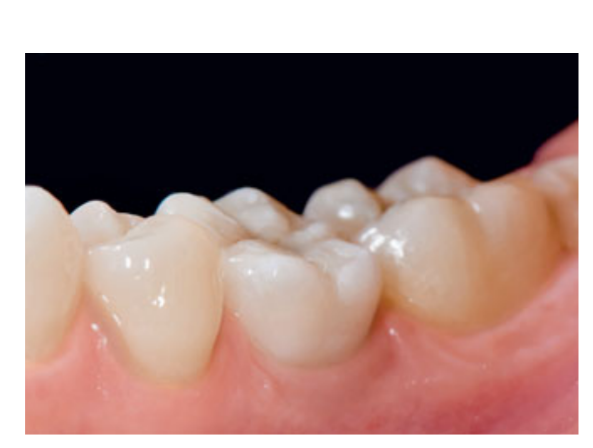
80 mg of ketoprofen (Oki, Dompe, Milan, Italy) was prescribed two or three times daily for as long as required. Patients were instructed to rinse with 0.2% chlorhexidine (Curasept) for 2 weeks and to stay on a soft diet regimen for 10 days. Sutures were removed after 2 weeks. Three months after placement, implant stability was checked manually, and definitive impressions were taken. After 1 week, screw-retained provisional resin crowns rebased on temporary titanium abutments were delivered. Six months after implant placement, definitive metal- or zirconia-ceramic screw-retained crowns were delivered (Figs 3 to 5). Clinical follow-up and intraoral radiographs were scheduled at implant placement (baseline), implant loading (3 months later) and at 9, 36 and 60 months after loading (Figs 6 to 11). Patients were then enrolled in an oral hygiene programme with recall appointments every 3 months for the first year and then twice per year.





The following outcome measures were recorded.
- Implant/prosthesis failure: Removal of implants dictated by implant mobility, progressive marginal bone loss, infection or implant fracture. The stability of individual implants was measured by the prosthodontist (PM) at the time of provisional and definitive crown delivery (3 and 6 months after implant placement) by applying 35 Ncm of removal torque. One year after implant placement, implant stability was tested manually by the same prosthodontist with two dental mirror handles
- Complications: Fractures or chipping of the provisional or definitive ceramic crown, abutment mobility and biological complications, such as wound or implant infection, mucositis, abscesses or peri-implantitis, were recorded during all the follow-up period.
- Marginal bone levels (MBLs): Peri-implant MBLs were evaluated on intraoral digital radiographs taken with the parallel technique at the time of implant placement, and at 3, 9, 36 and 60 months after loading. Radiographs were accepted or rejected for evaluation based on the clarity of the implant threads. A radiologist, not previously involved in the study, evaluated all the radiographs. The distances from the mesial and distal interproximal bone to the horizontal interface between the implant and abutment (reference point) were measured with a software measurement tool (Digora for Windows 2.8, Soredex, Tuusula, Finland) that was calibrated for every single image against the space between two threads to the nearest 0.1 mm. The mesial and distal measurements were recorded with reference to the implant axis and averaged.
- Periodontal parameters: PPD and BOP were measured by a blinded operator not previously involved in the study, with a periodontal probe (PCP-UNC 15, Hu-Friedy Manu facturing, Chicago, IL, USA) at 3, 9, 36 and 60 months after loading. Three vestibular and three lingual values were collected for each implant.
Sample size and randomisation
Since this study was intended, at the beginning, to be preliminary to a larger clinical trial, an a priori sample size calculation was not performed. In each patient, the right or left molar or premolar were randomly allocated to receive either PS or RP implants. The randomisation code was created using computer software (Excel, Microsoft, Redmond, WA, USA) by combining a sequence of randomised non-consecutive numbers matching the two different procedures (PS versus RP implants) with the right or left tooth, and was assigned by an independent operator not otherwise involved in the trial, and numbers were placed in opaque envelopes. The left site was allocated as indicated in the envelope, and the contralateral site was treated during the same session, according to the other intervention. Data were collected in spread-sheets (Microsoft Office Excel) by an independent physician at the Dentistry Unit, University of Sassari, Italy.
Statistical analysis
Statistical analyses were conducted using QI Macros SPC software (ver. 2010, KnowWare Inter national, Denver, CO, USA) for Microsoft Office Excel. All values were presented as mean and mean difference, with standard deviation (SD) and 95% confidence intervals (CIs). Differences in the proportion of patients with prosthesis failures, implant failures and complications (dichotomous outcomes) were compared between groups using the McNemar test. Odds ratio (OR) was used to evaluate possible association between interventions and complications. Mean differences of continuous outcomes (MBL, PPD and BOP) between groups were compared by using matched paired t tests conducted at the 95% level of significance. Multiple testing was corrected according to the Bonferroni method.
Results
In total, 25 patients were screened for eligibility, but seven patients did not meet the selection criteria for the following reasons: three declined to adhere to a strict clinical and radiological follow-up, three had insufficient bone height, and one had insufficient bone width. Eighteen patients (8 men, 10 women), with a mean age of 48 years (range 28 to 70), were considered eligible and consecutively treated. In total, 36 implants were placed in healed sites with an insertion torque ranging between 35 and 45 Ncm. One patient dropped out of the study after 4 years. No deviation from the original protocol occurred. Data were collected at baseline (implant placement) and after 3 (implant loading), 9, 36 and 60 months.
No implant mobility, infection or fracture occurred. All implants were stable at the end of the study. No prosthetic complications were observed. No major biological complications were recorded in either treatment group. One patient experienced mucosal inflammation with positive BOP (RP group) after 3 months. One patient had bilateral peri-implant mucosal inflammation with positive BOP after 6 months. Another two patients experienced bilateral mucosal inflammation 24 and 30 months after loading, with positive BOP. All of these patients mantained good oral hygiene using oral health promotion programmes. After that, the peri-implant inflammation resolved, and no other complications were recorded up to 60 months of follow-up. Overall, there was no statistically significant difference between the groups (3/18 versus 4/18; P = 1.0; OR 1.333; 95% CI 0.3467 to 5.1272).
The mean MBL 3 months after loading was 0.6 ± 0.17 mm (95% CI 0.55 to 0.71 mm) for RP implants and 0.58 ± 0.17 mm (95% CI 0.50 to 0.66 mm) for PS implants. No statistically significant difference was observed between the groups (P = 0.14). Nine months after loading the mean MBL was 0.9 ± 0.26 mm (95% CI 0.81 to 1.05 mm) for RP implants and 0.84 ± 0.2 (95% CI 0.73 to 0.95 mm) for PS implants. No statistically significant difference was observed between the groups (P = 0.18). Thirty-six months after loading, the mean MBL was 1.09 ± 0.3 (95% CI 0.95 to 1.24 mm) in the RP group and 1.06 ± 0.24 mm (95% CI 0.94 to 1.17 mm) in the PS group, with no statistically significant difference between groups (P = 0.70). Sixty months after loading the mean MBL was 1.24 ± 0.39 mm (95% CI 1.05 to 1.43 mm) in the RP group and 1.20 ± 0.2 mm (95% CI 1.01 to 1.39 mm) in the PS group, with no statistically significant difference between the groups (P = 0.85). The results are summarised in Table 1.
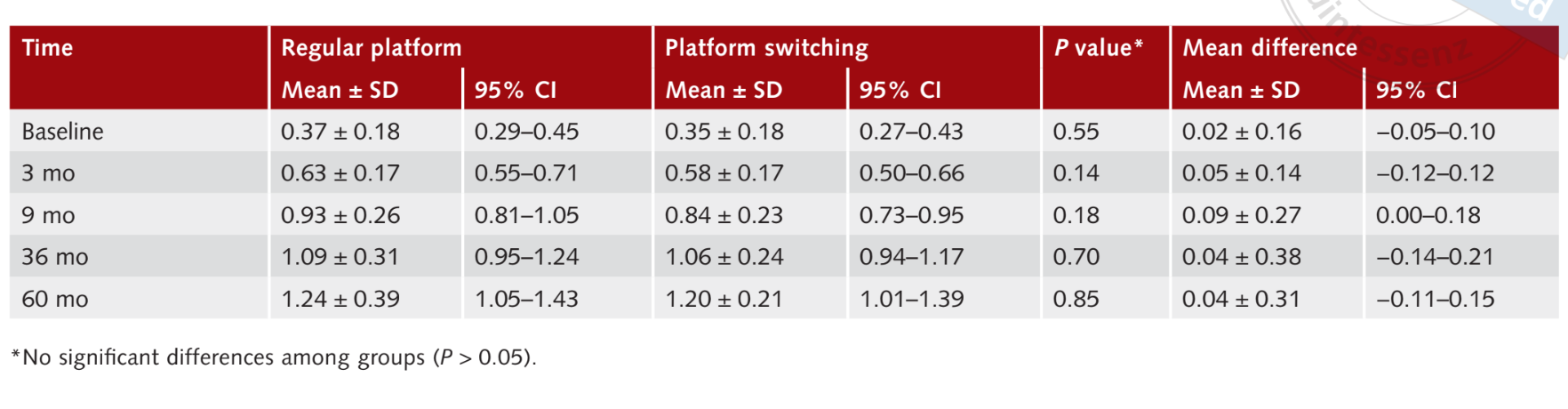
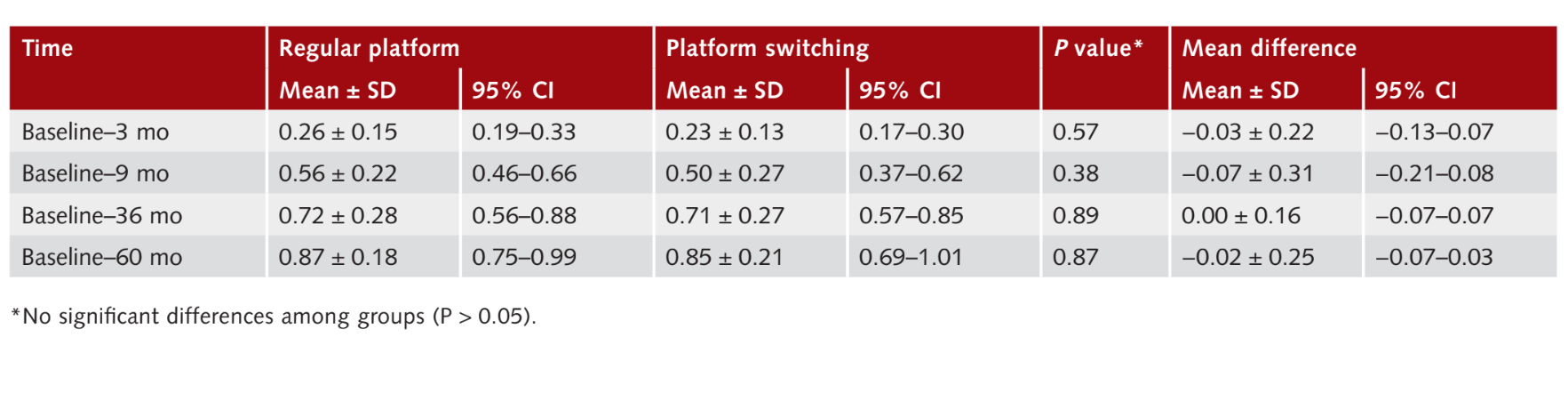
The average change in interproximal MBL was analysed for each implant. Three months after loading, the change in MBL was 0.26 ± 0.15 mm (95% CI 0.19 to 0.33 mm) for RP implants and 0.2 ± 0.1 mm (95% CI 0.17 to 0.30 mm) for PS implants. No statistically significant difference was observed between the groups (P = 0.57). Nine months after loading, the change in MBL from baseline was 0.56 ± 0.22 mm (95% CI 0.46 to 0.66 mm) for RP implants and 0.50 ± 0.27 mm (95% CI 0.37 to 0.62 mm) for PS implants. No statistically significant difference was observed between the groups (P = 0.38). The MBL change between 36 months after loading and baseline was 0.72 ± 0.28 mm (95% CI 0.56 to 0.88) in the RP group and 0.71 0.27 mm (95% CI 0.57 to 0.85), with no statistically significant difference between the groups (P 0.89). Sixty months after loading, the MBL change was 0.87 0.18 mm (95% CI 0.75 to 0.99 mm) for RP implants and 0.85 ± 0.21 mm (95% CI 0.69 to 1.01 mm) for PS implants. No statistically significant difference was observed between the groups (P = 0.87). The results are summarised in Table 2.
Probing pocket depths
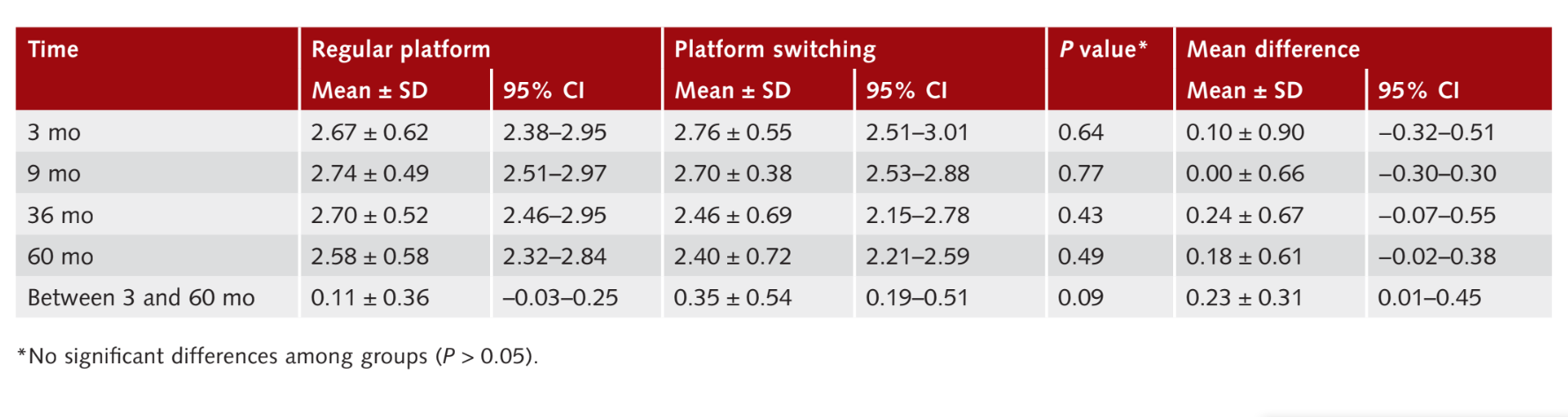
Nine months after loading (1 year after im plant placement) the mean PPD values were 2.74 ± 0.49 mm (95% CI 2.51 to 2.97 mm) for RP implants and 2.70 ± 0.38 mm (95% CI 2.53 to 2.88 mm) for PS implants, with no statistically significant difference between the groups (P = 0.77). Thirty-six months after loading mean PPD values were 2.70 ± 0.52 mm (95% CI 2.46 to 2.95 mm) for the RP group and 2.46 0.69 mm (95% CI 2.15 to 2.78 mm) for the PS group, with no statistical difference between the groups (P = 0.43). Sixty months after loading mean PPD values were 2.58 ± 0.58 mm (95% CI 2.32 to 2.84 mm) for the RP group, and 2.40 0.72 mm (95% CI 2.21 to 2.59 mm) for the PS group, with no statistical difference between the groups (P 0.49). During the entire follow-up examination, changes in PPD values were 0.1 0.36 mm (95% CI −0.03 to 0.25 mm) in the RP group and 0.35 ± 0.54 (95% CI 0.19 to 0.51 mm) in the PS group (P = 0.09). The results are summarised in Table 3.
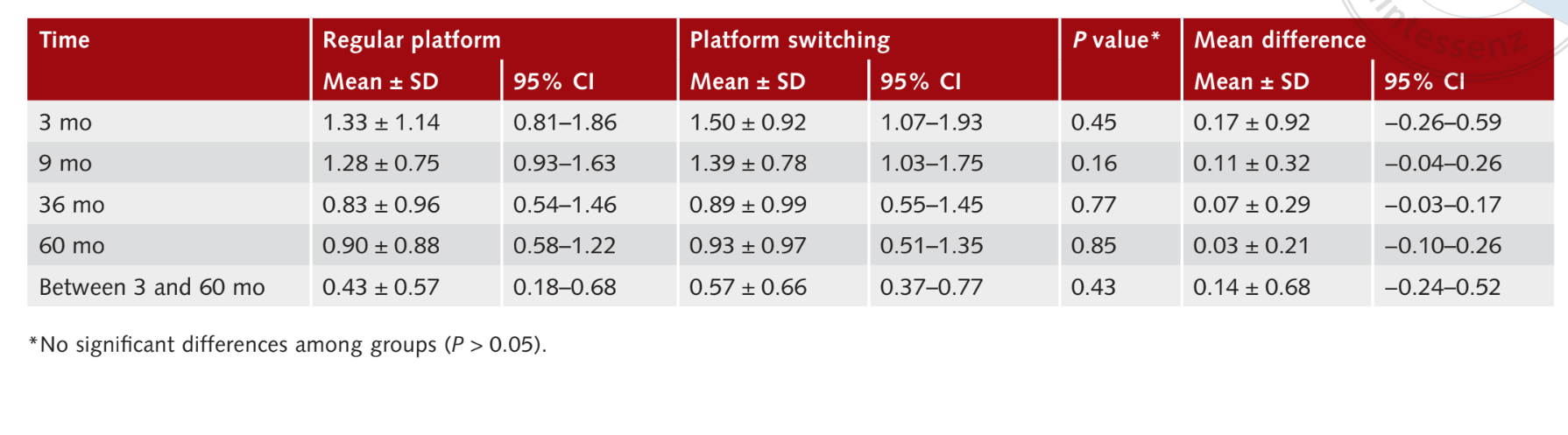
Bleeding on probing
The mean BOP values measured 9 months after implant loading were 1.28 0.75 (95% CI 0.93 to 1.63) for RP implants and 1.39 ± 0.78 (95% CI 1.03 to 1.75) for PS implants, with no statistically significant difference between the groups (P = 0.16). Sixty months after loading, mean BOP values were 0.90 ± 0.88 (95% CI 0.58 to 1.22) in the RP group and 0.93 ± 0.97 (95% CI 0.51 to 1.35) in the PS group, with no statistical difference (P = 0.85). During the entire follow-up examination, changes in BOP values were 0.4 ± 0.57 (95% CI 0.18 to 0.68) in the RP group and 0.570.66 (95% CI 0.37 to 0.77) in the PS group (P = 0.43). The results are summarised in Table 4.
Discussion
The aim of this study was to compare clinical and radiographic outcomes of PS and RP implants. The null hypothesis that there are no differences in clinical and radiographic outcomes between PS and RP implants in single-tooth replacement was tested against the alternative hypothesis of differences. Overall, the 60-months after loading results confirmed the two preliminary reports at 9 and 36 months post-loading14,15, demonstrating that implants restored according to the PS concept showed similar outcomes to implants with matching implant–abutment diameters (RP) when compared in the same patients.
The main limitation of this study was a lack of allocation concealment. The envelope containing the randomisation code was opened before implant placement, when it should have been opened at healing abutment connection. However, this study was designed as a split-mouth randomised controlled trial, avoiding possible influence of the patient biotype, bone density and/or lifestyle, and a medium follow-up (5 years) was achieved by almost all patients involved (one patient dropped out). Other limitations were that an a priori sample size calculation was not performed, thus a small sample size might have hidden some differences between groups.
Marginal bone loss around different types of implant occurs regardless of any efforts made to prevent it. Several theories raised during the last decade that support the idea that peri-implant bone resorption is mediated by the bone inflammatory response, but this topic it is still controversial. Recently, Esposito et al, in a 5-year post-loading randomised clinical trial comparing implants with internal connection and platform switched, and external connections and not platform switched, did not find any statistically significant differences between the two different connection and neck design types. Bateli et al suggested that a multi factorial approach is needed to preserve marginal bone around dental implants. Other results from clinical studies and systematic reviews suggest that the bone resorption around implants can be reduced by moving the implant–abutment junction medially from the bone crest. Atieh et al, in a systematic review, concluded that platform-switched implants presented lower bone resorption compared with RP implants, and that the degree of marginal bone resorption is inversely correlated to the implant–abutment mismatch. Some recent sys tematic reviews showed less enthusiastic results, suggesting cautious interpretation of these results due to the heterogeneity of the included stud es. Accordingly, the results from the present randomised controlled trial confirmed the first 9-month and 36-month post-loading results that implants with PS seem not to preserve crestal bone better in comparison with implants with traditional implant–abutment connection.
It should be noted that most comparative studies tested wide-diameter implants versus regular-diameter implants, both restored with the same abutment. In contrast, in the present research, implants with identical diameters were used in a split-mouth design.
It was assumed in the first preliminary report that implants with the same diameter inserted in each patient would have similar outcomes; this was confirmed in the medium-term report and is supported by more evidence in the present report, 60 months after loading. However, owing to limitations of the study as well as favourable inclusion criteria, some results could not be obtained, such as those for bone width of < 6m and a minimum amount of keratinised gingiva of 5 mm. Another reason for comparable results between the approaches could be related to the regular maintenance procedures, resulting in healthy peri-implant tissues. Finally, the investigation was focused only on single teeth, and the neighbouring teeth may have contributed to the preservation of the peri-implant tissues. Hence, the effect of the PS concept remains controversial.
Conclusions
The clinical and radiographic outcomes of implants restored according to the PS concept versus implants restored with matching implant–abutment diameters are comparable, up to 5 years after loading.
References
- Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants 1986;1:11–12.
- Pozzi A, Agliardi EL, Tallarico M, Barlattani A. Clinical and radiological outcomes of two implants with different pros thetic interfaces and neck configurations: randomized, controlled, split-mouth clinical trial. Clin Implant Dent Relat Res 2014;16:96–106.
- Lindhe J, Meyle J; Group D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology J Clin Periodontol 2008;35(8 Suppl):282–285.
- Lang NP, Berglundh T, on Behalf of Working Group 4 of the Seventh European Workshop on Periodontology. Periimplant diseases: where are we now? Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol 2011;38(Suppl 11):178–181.
- Rungsiyakull C, Rungsiyakull P, Li Q, Li W, Swain M. Effects of occlusal inclination and loading on mandibular bone remodeling: a finite element study. Int J Oral Maxillofac Implants 2011;26:527–537.
- Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodon tics Restorative Dent 2005;25:113–119.
- Assunção WG, Gomes EA, Rocha EP, Delben JA. Three-dimensional finite element analysis of vertical and angular misfit in implant-supported fixed prostheses. Int J Oral Maxillofac Implants 2011;26:788–896.
- Canullo L, Fedele GR, Iannello G, Jepsen S. Platform switching and marginal bone-level alterations: the results of a randomized-controlled trial. Clin Oral Implants Res 2010;21:115–121.
- Strietzel FP, Neumann K, Hertel M. Impact of platform switching on marginal peri-implant bone-level changes. A systematic review and meta-analysis. Clin Oral Implants Res 2015;26:342–358.
- Lazzara RJ, Porter SS. Platform switching: a new con cept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent 2006;26:9–17.
- Gardner DM. Platform switching as a means to achieving implant esthetics. N Y State Dent J 2005;71:34–37.
- Broggini N, McManus LM, Hermann JS, et al. Peri-implant inflammation defined by the implant-abutment interface. J Dent Res 2006;85:473–478.
- Al-Nsour MM, Chan H-L, Wang H-L. Effect of the plat form-switching technique on preservation of peri-implant marginal bone: a systematic review. Int J Oral Maxillofac Implants 2012;27:138–145.
- Meloni SM, Jovanovic SA, Lolli FM, et al. Platform switching vs regular platform implants: nine-month post-loading results from a randomised controlled trial. Eur J Oral Implantol 2014;7:257–265.
- Meloni SM, Jovanovic SA, Pisano M, Tallarico M. Platform switching versus regular platform implants: 3-year post-loading results from a randomised controlled trial. Eur J Oral Implantol 2016;9:381–390.
- Bragger U. Use of radiographs in evaluating success, stability and failure in implant dentistry. Periodontolol 2000 1998;17:77–88.
- Pozzi A, Tallarico M, Moy PK. Three-year post-loading results of a randomised, controlled, split-mouth trial com- paring implants with different prosthetic interfaces and design in partially posterior edentulous mandibles. Eur J Oral Implantol 2000;7:47–61.
- Albrektsson T, Dahlin C, Jemt T, Sennerby L, Turri A, Wennerberg A. Is marginal bone loss around oral implants the result of a provoked foreign body reaction? Clin Implant Dent Relat Res 2014;16:155–165.
- Esposito M, Maghaireh H, Pistilli R, et al. Dental implants with internal versus external connections: 5-year post-loading results from a pragmatic multicenter randomised controlled trial. Eur J Oral Implantol 2016; 9: 129–141.
- Bateli M, Att W, Strub JR. Implant neck configurations for preservation of marginal bone level: a systematic review. Int J Oral Maxillofac Implants 2011;26:290–303.
- Enkling N, Jöhren P, Klimberg V, Bayer S, Mericske-Stern R, Jepsen S. Effect of platform switching on peri-implant bone levels: a randomized clinical trial. Clin Oral Implants Res 2011;22:1185–1192.
- Atieh MA, Ibrahim HM, Atieh AH. Platform switching for marginal bone preservation around dental implants: a systematic review and meta-analysis. J Periodontol 2010;81:1350–1366.
