Radiologic comparative analysis between saline and platelet-rich fibrin filling after hydraulic transcrestal sinus lifting without adjunctive bone graft: A randomized controlled trial
Abstract
Objectives: To evaluate implant survival rate, any complications, and changes in residual alveolar bone height (RABH) using saline or platelet-rich fibrin (PRF) filling after hydraulic transcrestal sinus lifting.
Methods: Dental implants were placed after hydraulic transcrestal sinus lifting and the filling of saline (20 patients) or PRF (20 patients). Outcome measurements were implant survival, any complications, and RABH changes. Cone-beam computed tomography (CBCT) scans were taken and compared preoperatively (T0), immediately postoperatively (T1), at 3 months (T2), 6 months (T3), and 12 months postoperatively (T4), respectively.
Results: In a total of 40 patients, 45 implants with a mean length of 10.4 ± 0.8 mm were placed in posterior maxilla of a mean RABH of 6.8 ± 1.1 mm. The increase in RABH peaked at T1, and continuous drooping of the sinus membrane was observed but stabilized at T3. Meanwhile, the gradual increase in the radiopacities was found below the lifted sinus membrane. The PRF filling induced the radiographic intrasinus bone gain of 2.6 ± 1.1 mm, which was significantly more than 1.7 ± 1.0 mm of saline filling at T4 (p < .05). All the implants were in function with no significant complications over the one-year follow-up period.
Conclusions: In this randomized case–control study, the feasibility of hydraulic transcrestal sinus lifting without bone graft was confirmed and PRF might be a better filler to support the elevated sinus membrane. However, adjunctive bone grafting should still be indicated for cases requiring more than 2–3 mm of intrasinus bone gain.
Introduction
The placement of dental implants in the edentulous posterior maxilla is frequently limited due to the resorption of the alveolar process beneath the maxillary sinus after tooth loss. To overcome these drawbacks, various techniques and instruments have been developed for sinus lifting surgery. The transalveolar (or transcrestal) approach was introduced by Tatum, and the instrument known as a "socket former" was used to infracture the sinus floor and to move it in a more apical direction (Tatum, 1986). No graft material was utilized to increase and maintain the volume of the elevated area. Various materials, including autogenous, allogeneic, or xenogeneic bone grafts, have been added into the space created below the elevated sinus membrane (Wallace et al., 2012). However, there is no conclusive study reporting on the advantages of bone grafting inserted at the apical portion of the implant (Andreasi Bassi, Lopez, Confalone, & Carinci, 2015). In addition, there may be a risk of membrane perforation due to the sharp edges of the graft granules (Kher et al., 2014).
Recently, it has been demonstrated that consistent bone gain within the maxillary sinus could be achieved without the addition of any bone graft material (Lundgren, Andersson, Gualini, & Sennerby, 2004; Nedir, Bischof, Vazquez, Szmukler-Moncler, & Bernard, 2006; Nedir, Nurdin, Vazquez, Abi Najm, & Bischof, 2016; Palma et al., 2006; Sohn, Lee, Ahn, & Shin, 2008). There seems to be increasing evidence indicating that the implant fixture itself functions as a "tent-pole" to prevent the elevated sinus membrane from collapsing. Moreover, the sinus membrane could be elevated more and longer during the new bone formation phase if there were materials filling the space between the sinus floor and the elevated sinus membrane; saline, patient's own venous blood, and collagen sponges soaked with these fluids have been commonly used for this purpose (Lundgren et al., 2004; Palma et al., 2006; Sohn et al., 2008).
Platelet-rich fibrin (PRF) is an autologous platelet concentrate that contains platelet-derived growth factor (PDGF), insulin-like growth factor (IGF), vascular endothelial growth factor (VEGF), transforming growth factor beta (TGF-β), and platelet-derived angiogenic factors (Peterson et al., 2010). PRF has been used as a graft material in maxillary sinus augmentation procedures alone or in combination with grafting materials to promote bone regeneration and increase the amount of newly formed bone by increasing the number of osteoprogenitor cells (Mazor et al., 2009; Nizam et al., 2018).
The purpose of this randomized controlled trial was to evaluate whether inserting saline or PRF can influence the implant survival rate, as well as to determine any changes in the residual alveolar bone height (RABH) after hydraulically elevating the sinus membrane using a transcrestal approach. The null hypothesis was that there is no difference in increase in the RABH between the groups.
Materials and methods
This study was designed as a randomized controlled trial and conducted at two centers (Division of Oral and Maxillofacial Surgery/Department of Dentistry, Hanyang University Hospital, and Apsun Dental Hospital) between September 2016 and August 2017. The study was approved by the Institutional Review Board of Hanyang University Hospital (IRB No. 2016–05–039) and registered at the WHO international clinical trials registry platform (KCT0005252). It was conducted in accordance with the Declarations of Helsinki and internationally accepted guidelines for RCTs, including the CONSORT statement (www.consort-statement.org). All the surgical and prosthetic procedures were performed by two expert clinicians (YSC and CJP).
Periapical and panoramic radiographs were used for initial screening. Any healthy patient, aged 18 years or older, presenting with edentulism in the posterior maxilla and a reduced RABH, making the placement of implants with a length longer than 8.5 mm impossible, was included in this study after providing informed consent. The exclusion criteria were RABH less than 5 mm, measured on cone-beam computed tomography (CBCT) scan, and systemic or local contraindications for the implant placement, including history of uncontrolled metabolic disorders, smoking habit, bruxism, or uncontrolled periodontal disease. Enrolled patients were informed about the surgical procedures, materials to be used, benefits, and the potential risks, and complications of this clinical study.
After local anesthesia, a full-thickness flap was elevated to expose the alveolar ridge. Cortical bone marking was performed, and a 2.2-mm twist drill was used to drill to a depth of 1 mm below the sinus floor. A special drilling system (OneCAS Kit; Osstem) was used to enlarge the osteotomy site and gain access to the sinus membrane (Gatti et al., 2018). Injection and retrieval of saline were repeated in an incremental manner to separate and lift the membrane hydraulically from the sinus floor. Any damage of the membrane was ruled out by the negative pressure resulting from the aspiration of the injected saline. After randomization prior to the surgery, patients were assigned into two groups, saline or PRF. In the saline group, 5 ml of saline was injected to support the elevated sinus membrane, while in the PRF group, the same amount of the leukocyte and platelet-rich fibrin (L-PRF) was produced using a protocol of approximately 480 g for 12 min by (relative centrifugal force (RCF) clot = 408 g) by a centrifugal device (33° rotor angulation, 50 mm radius at the clot, 80 mm at the maximum, Intra-Lock, Boca Raton, FL) in 9-ml glass-coated plastic tubes (Miron, Pinto, Quirynen, & Ghanaati, 2019) and inserted en masse beneath the lifted sinus membrane through the implant drilling hole.
No bone graft materials were added in either group. The length of the implants was determined by selecting the nearest fixture, which was double that of the RABH, without exceeding 11.5 mm. All the implants (TS III SOI, Osstem) were installed with a seating torque over 25 Ncm. Implants had a sandblasted and acid-etched surface coated with a pH-buffering agent to introduce hydrophilic properties, promote osseointegration during the early healing period, and accelerate new bone formation. Following the connection of the healing abutment, the flaps were sutured without any tension. Patients received pain killers and antibiotics for 10 days, and a 0.2% chlorhexidine mouthwash was also prescribed thrice daily. Postoperative complications were recorded, and sutures were removed 10 days after surgery.
The outcome measures were implant survival rates, biological or mechanical complications, and changes in the RABH. The survival rates of the implants were evaluated by an independent assessor (KGH), and an implant was considered as a failure if it presented mobility, progressive marginal bone loss, infection, or any complications rendering the implant unusable. Any biological (pain, swelling, suppuration, etc.) and/or mechanical (such as fracture) complications that occurred during the one-year follow-up period were recorded and treated by the same experts.
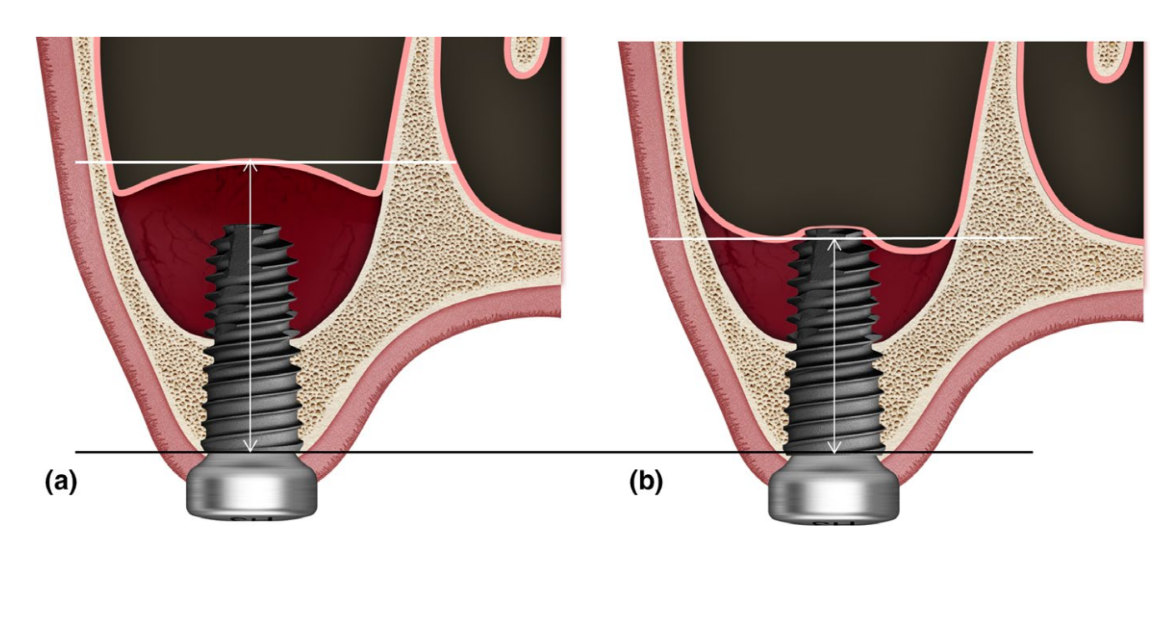
Changes in the RABH were evaluated on the CBCT images taken preoperatively (T0), immediately postoperatively (T1), and 3 (T2), 6 (T3), and 12 months (T4) postoperatively by an independent blinded examiner (SHJ). Exposure parameters for CBCT scan (field of vision 35 × 50 mm; voxel size 0.2 mm; time 10.8 s; kV 75; mA 10; dose area product 240 mGy·cm2) were set as low as reasonably achievable (ALARA). The RABH was measured as the farthest distance from the alveolar crest to the upper intrasinus radiopaque margin, which was presumed to be an elevated sinus membrane, parallel to the long axis of each implant on the reconstructed coronal CBCT image (Figure 1). Particularly, when this radiopaque margin sank down below the implant apex, the penetrated implant apex was not set as the upper radiopaque margin, and in cases with multiple implants, the distances measured on each implant were summed and averaged. The overlay and analysis of the CBCT images were performed with OnDemand3D software (Cybermed Inc).
Statistical analysis
With the equal variance assumption, the sample size was determined with an alpha level of 0.05 to satisfy the power of 90% by the means of RABH ranged from 1.5 to 6.0 mm with standard deviation of 0.9 mm from the previous study using PRF (Mazor et al., 2009). Based on these results, the minimum sample size was estimated to be 21 subjects in each group considering a possible attrition rate of 10% during the study period. Repeated analysis of variance (ANOVA) was used to analyze the effects of the group and the time on RABH and ad hoc test based on the Bonferroni correction to compare the effect of the group on RABH at specific time period, respectively. All statistical analysis was performed using SPSS, version 20 (SPSS Inc). Statistical significance was set as p < .05.
Results
A total of 42 patients were consecutively enrolled, and two patients dropped out (one in each group) due to losses to follow-up. Finally, data from 40 patients (21 men and 19 women) with a mean age of 45.6 years (range from 27 to 70 years) were collected and evaluated in this trial (Table 1). Overall, the mean RABH was 6.8 ± 1.1 mm (range from 5.3 to 8.1 mm), and a total of 45 implants with a mean length of 10.4 ± 0.8 mm were placed in the posterior maxilla. The saline group had 22 implants and the PRF group had 23 implants, respectively.
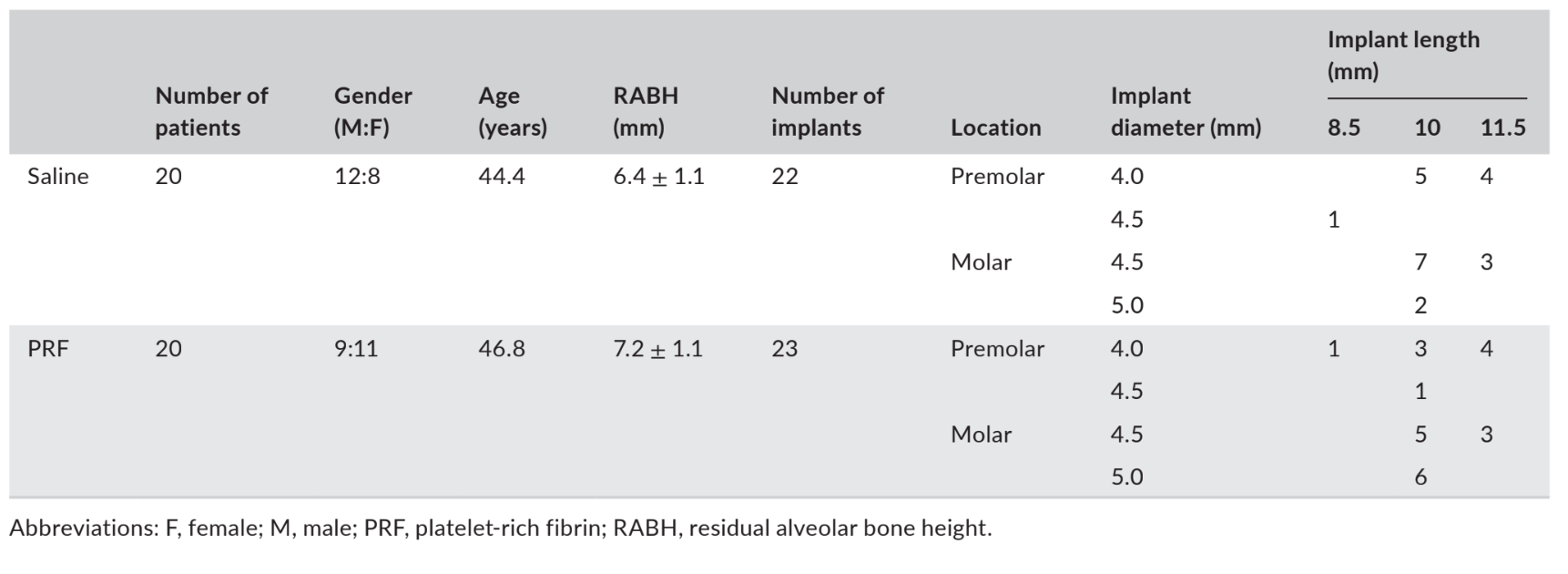
No implants failed, and no significant complications, with the exception of physiologic swelling after surgery, were observed in either group during the follow-up period. The upper intrasinus radiopaque margin, which was clearly demarcated at T1, was almost indistinguishable from the remaining alveolar bone at T4 in the panoramic and CBCT images (Figure 2). Though no bone graft material was used, there was an increase in the RABH measured around the implants, which peaked at T1 and continued to decrease up to T4. The increase in RABH was shown with mean, standard deviation, and 95% confidence interval (Figure 3), and the power of this test was estimated as 98.44%. Regarding the effect of the group on the increase in RABH, the significant difference was found only at T4 (p < .05).
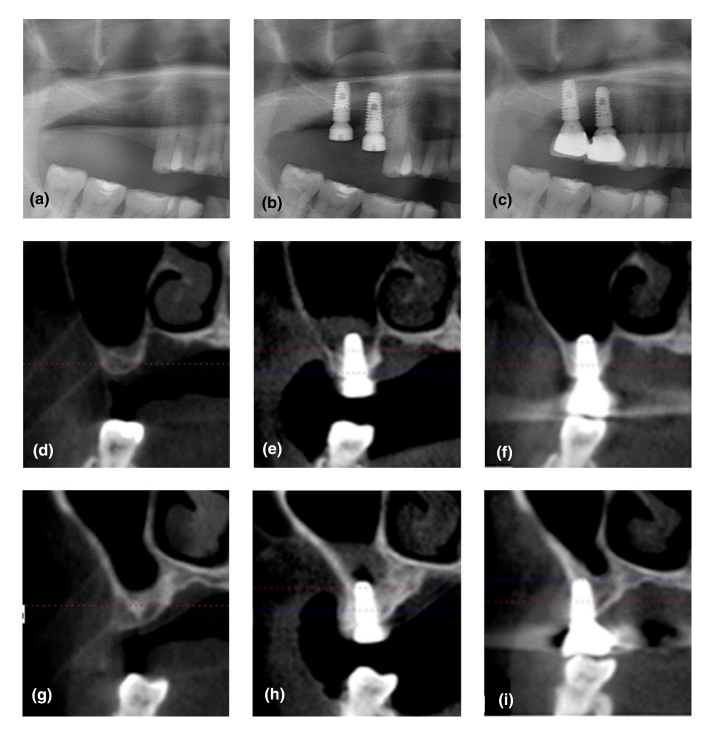
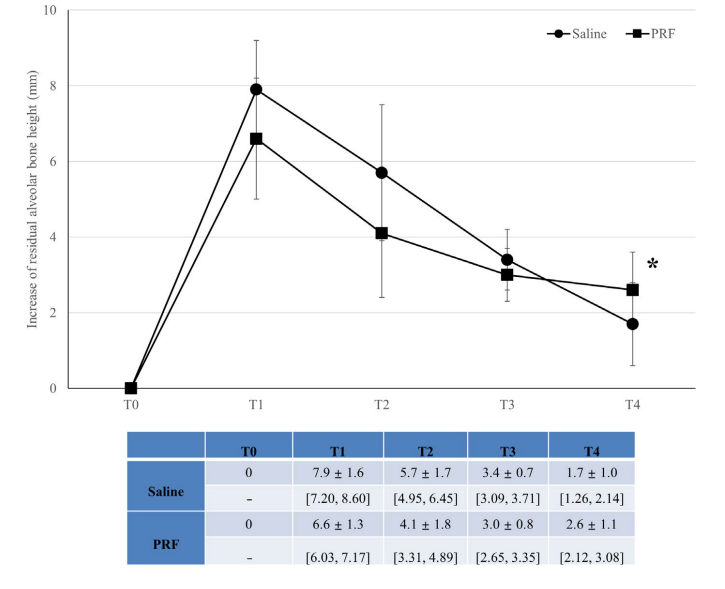
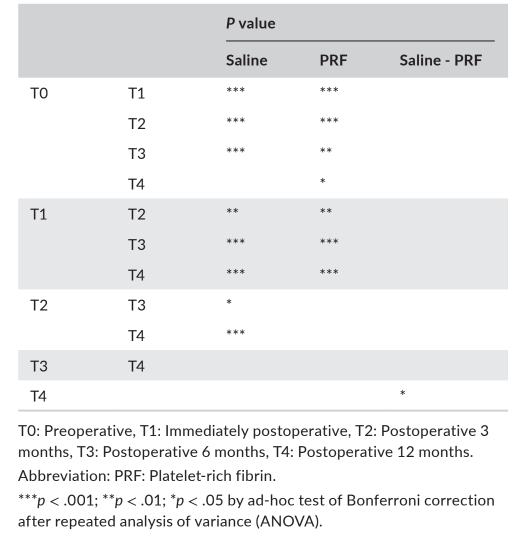
Table 2 presented the statistical significances of the difference in measurements between times and groups. In the saline group, there was a statistically significant difference among RABHs at all time periods (p < .001), and the Bonferroni multiple comparison tests showed statistically significant differences at T0-T1, T0-T2, T0-T3, T1-T3, T1-T4, T2-T4 (p < .001), T1-T2 (p < .01), and T2-T3 (p < .05). In the PRF group, there was also a statistically significant difference among RABHs at all time periods (p < .001), and the Bonferroni multiple comparison tests showed statistically significant differences at T0-T1, T0- T2, T1-T3, T1-T4 (p < .001), T0-T3 (p < .01), and T0-T4 (p < .05).
Discussion
This randomized controlled trial was designed to evaluate the implant survival rate, complications, and changes in RABH using saline or PRF after hydraulic transcrestal sinus lifting without insertion of adjunctive bone graft. Several clinical publications have demonstrated that the "tent-pole" effects of implants that were simultaneously placed prevented the elevated sinus membrane from collapsing (Lundgren, Cricchio, Palma, Salata, & Sennerby, 2008; Sohn et al., 2008). When an absorbable gelatin sponge was loosely inserted under the elevated sinus membrane as an alternative to bone filler, it was also found to act as space maintainer for new bone formation in the maxillary sinus (Sohn et al., 2008). Our results confirmed the findings of previous studies, including the drooping of the elevated sinus membrane or re-pneumatization of the maxillary sinus (Lundgren et al., 2004, 2008; Nedir et al., 2016; Sohn et al., 2008). This process was found to be stabilized at 6 months postoperatively, however, continued up to 12 months in both groups.
In this study, a radiographic bone gain of 1.7 ± 1.0 mm and 2.3 ± 1.9 mm was found in the sinus cavity at a one-year follow-up after hydraulic sinus elevation with no bone grafts with the addition of saline and PRF, respectively. It has been previously reported that implants installed into the sinuses of 40 patients using an osteotome technique without bone graft materials had a mean gain of RABH in scanned panoramic radiographs of 2.9 ± 1.2 mm at 6 months (Leblebicioglu, Ersanli, Karabuda, Tosun, & Gokdeniz, 2005); furthermore, as in the present study, the implant survival rate was 100%. New bone formation of 2.5 ± 1.2 mm from the sinus floor to the implant apex on periapical radiographs 1 year after the osteotome sinus floor elevation technique without grafting (Nedir et al., 2006), and the bone gain of 1.7 ± 2.0 mm on periapical radiographs 3 years after implant placement (Pjetursson & Lang, 2014) were demonstrated. Unlike these previous studies, our study used CBCT images to measure the changes in the elevated sinus membrane more accurately. Despite the fact that major clinically relevant changes were clearly detected by comparing T1 and T4 and serial CBCTs had increased risk of radiation exposure, CBCTs were taken at T2 and T3 solely for research purposes. More specifically, T2 was included to clarify the substantial settling of the elevated sinus membrane, which was mostly observed 3 months postoperatively (Lundgren et al., 2008), and T3 was presumed to be important in terms of intrasinus bone regeneration since occlusal loading is generally applied to implants 6 months postoperatively.
Some clinicians could raise a doubt about using the term of RABH because the soft and hard tissues are mixed during the whole study period. Since the comprehensive measurement of intrasinus soft and hard tissues was thought to be important to understand the intrasinus change up to bone formation, we adopted the term of RABH and measured the farthest distance to the upper intrasinus radiopaque margin. Occasionally, it was technically hard to separate both of them clearly.
The radiopacities of the compartment that was filled with either saline or PRF below the lifted sinus membrane were observed to be gradually increased, and further studies will be necessary to confirm new bone formation in this compartment. Interestingly, previous histologic studies mostly reported new bone formation after sinus membrane elevation without a bone graft (Lundgren et al., 2008; Palma et al., 2006); how- ever, one study showed no noticeable new bone formation (Ahn, Cho, Byrne, Kim, & Shin, 2011).
Many clinical studies have reported successful results of sinus lifting surgery using osteotomes (Giannini et al., 2015; Komarnyckyj & London, 1998). However, the complication resulting from repeated blunt trauma to the inner ear from tapping by malletting, such as benign paroxysmal positional vertigo, is possible and its prevalence could be increased in cases of hard cortical sinus floor or sinus floor with septum (Ahn, Park, & Kim, 2012; Hatano, Sennerby, & Lundgren, 2007). To overcome the limitations of the conventional osteotome technique, many innovative instruments have been introduced to the implant market, and the hydraulic lifter in the CAS Kit is also designed for hydraulic lifting of the sinus membrane in lieu of saline. Another advantage of the hydraulic lifter is that the sinus membrane can be elevated much wider and higher (Supplemental data).
In our study, saline or PRF was filled in the new compartment under the elevated sinus membrane as a spacer to support the sinus membrane and all implant were successful. Though there were some voids at T1, radiopacities beneath the elevated sinus membrane were increased with disappearance of the voids in both groups over time. Our results also suggest that PRF could occupy the space created under the elevated sinus membrane more efficiently than saline and induce more intrasinus bone formation with no adjunctive bone grafting in hydraulic transcrestal sinus lifting. A preliminary study has shown that PRF gradually releases autologous growth factors and elicits a strong and durable effect on the proliferation and differentiation of osteoblasts (He, Lin, Hu, Zhang, & Wu, 2009). In addition, the use of PRF as the sole filling material during a simultaneous sinus lift and implantation has been reported to stabilize a high volume of natural regenerated bone in the subsinus cavity up to the tip of the implants (Mazor et al., 2009). Since PRF is a simple and inexpensive biomaterial, its use seems a more relevant option than any other filling material during sinus lifting surgery with no bone grafts. However, the overall bone gain limited to 2–3 mm and the small difference between the saline and PRF groups should be considered prior to the routine application of PRF as the sole filling material. Moreover, as shown in Figure 2f, the "tent-pole" effect of the implant failed to last till 12 months postoperatively and drooping of the thin and pliable sinus membrane was inevitable in almost all cases. Strict inclusion criteria for this procedure are mandatory and the use of bone graft materials should be indicated for cases requiring a greater intrasinus bone formation, particularly over the implant apex.
The main limitation of our randomized controlled trial was that neither negative control without saline and PRF nor positive control with grafting has been set. Considering the blindness nature of the transcrestal sinus lifting, particularly hydraulic lifting, it is practically very hard to confirm the complete removal of the saline, which was used to separate and lift the sinus membrane. Therefore, the group without saline was almost impossible to set as negative control and we strictly controlled the total volume of the saline used during the surgery instead. Saline group was also chosen as negative control to make two procedures, saline and PRF filling, as similar as possible. Recent studies have reported the capacity of new bone formation with only sinus membrane elevation and no bone graft (Lundgren et al., 2004, 2008; Nedir et al., 2006, 2016; Palma et al., 2006; Sohn et al., 2008; Sohn, Moon, Moon, Cho, & Kang, 2010; Winter, Pollack, & Odrich, 2003). Based on these encouraging results, the group with bone grafting was not set as positive control because this study aimed to find out whether PRF may offer some additional benefits over no bone grafting. It was also taken into account that there had been a variety of results about intrasinus bone formation, which cannot be formulated according to bone graft materials.
Conclusions
Within the limitations of this study, it can be concluded that:
- After hydraulic transcretal sinus lifting, the use of saline or PRF as the sole filling material could induce an increase in RABH, which resulted from the intrasinus bone gain, at T4. All implants survived, and no significant complications were observed during the follow-up period.
- In spite of the "tent-pole" effect of implants, drooping of sinus membrane was found to be stabilized at T3, however, continued up to T4.
- PRF filling led to a significantly greater increase in RABH than saline at T4. However, adjunctive bone grafting should still be indicated for cases requiring larger intrasinus bone gain, considering the overall intrasinus bone gain limited to 2–3 mm.
Yong-Seok Cho, Kyung-Gyun Hwang, Sang Ho Jun, Marco Tallarico, Amy M. Kwon, Chang-Joo Park
References
- Ahn, J. J., Cho, S. A., Byrne, G., Kim, J. H., & Shin, H. I. (2011). New bone formation following sinus membrane elevation without bone grafting: Histologic findings in humans. International Journal of Oral Maxillofacial Implants, 26(1), 83–90.
- Ahn, S. H., Park, E. J., & Kim, E. S. (2012). Reamer-mediated transalveolar sinus floor elevation without osteotome and simultaneous implant placement in the maxillary molar area: Clinical outcomes of 391 implants in 380 patients. Clinical Oral Implants Research, 23(7), 866–872. https://doi.org/10.1111/j.1600-0501.2011.02216.x
- Andreasi Bassi, M., Lopez, M. A., Confalone, L., & Carinci, F. (2015). Hydraulic sinus lift technique in future site development: Clinical and histomorphometric analysis of human biopsies. Implant Dentistry, 24(1), 117–124. https://doi.org/10.1097/ID.0000000000000200
- Gatti, F., Gatti, C., Tallarico, M., Tommasato, G., Meloni, S. M., & Chiapasco, M. (2018). Maxillary sinus membrane elevation using a special drilling system and hydraulic pressure: A 2-year prospective cohort study. International Journal of Periodontics & Restorative Dentistry, 38(4), 593–599. https://doi.org/10.11607/prd.3403
- Giannini, S., Signorini, L., Bonanome, L., Severino, M., Corpaci, F., & Cielo, A. (2015). Benign paroxysmal positional vertigo (BPPV): It may occur after dental implantology. A mini topical review. European Review for Medical and Pharmacological Sciences, 19(19), 3543–3547.
- Hatano, N., Sennerby, L., & Lundgren, S. (2007). Maxillary sinus augmentation using sinus membrane elevation and peripheral venous blood for implant-supported rehabilitation of the atrophic posterior maxilla: Case series. Clinical Implant Dentistry and Related Research, 9(3), 150–155. https://doi.org/10.1111/j.1708-8208.2007.00043.x
- He, L., Lin, Y., Hu, X., Zhang, Y., & Wu, H. (2009). A comparative study of platelet-rich fibrin (PRF) and platelet-rich plasma (PRP) on the effect of proliferation and differentiation of rat osteoblasts in vitro. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 108(5), 707–713. https://doi.org/10.1016/j.tripleo.2009.06.044
- Kher, U., Ioannou, A. L., Kumar, T., Siormpas, K., Mitsias, M. E., Mazor, Z., & Kotsakis, G. A. (2014). A clinical and radiographic case series of implants placed with the simplified minimally invasive antral membrane elevation technique in the posterior maxilla. Journal of Cranio-Maxillofacial Surgery, 42(8), 1942–1947. https://doi.org/10.1016/j.jcms.2014.08.005
- Komarnyckyj, O. G., & London, R. M. (1998). Osteotome single-stage dental implant placement with and without sinus elevation: A clinical report. International Journal of Oral Maxillofacial Implants, 13(6), 799–804. Leblebicioglu, B., Ersanli, S., Karabuda, C., Tosun, T., & Gokdeniz, H. (2005). Radiographic evaluation of dental implants placed using an osteotome technique. Journal of Periodontology, 76(3), 385–390.https://doi.org/10.1902/jop.2005.76.3.385
- Lundgren, S., Andersson, S., Gualini, F., & Sennerby, L. (2004). Bone reformation with sinus membrane elevation: A new surgical technique for maxillary sinus floor augmentation. Clinical Implant Dentistry and Related Research, 6(3), 165–173. https://doi.org/10.1111/j.1708-8208.2004.tb00224.x
- Lundgren, S., Cricchio, G., Palma, V. C., Salata, L. A., & Sennerby, L. (2008). Sinus membrane elevation and simultaneous insertion of dental implants: A new surgical technique in maxillary sinus floor augmentation. Periodontology, 2000(47), 193–205. https://doi.org/10.1111/j.1600-0757.2008.00264.x
- Mazor, Z., Horowitz, R. A., Del Corso, M., Prasad, H. S., Rohrer, M. D., & Dohan Ehrenfest, D. M. (2009). Sinus floor augmentation with simultaneous implant placement using Choukroun's platelet-rich fibrin as the sole grafting material: A radiologic and histologic study at 6 months. Journal of Periodontology, 80(12), 2056–2064. https://doi.org/10.1902/jop.2009.090252
- Miron, R. J., Pinto, N. R., Quirynen, M., & Ghanaati, S. (2019). Standardization of relative centrifugal forces in studies related to platelet-rich fibrin. Journal of Periodontology, 90(8), 817–820. https://doi.org/10.1002/JPER.18-0553
- Nedir, R., Bischof, M., Vazquez, L., Szmukler-Moncler, S.,& Bernard, J. P.(2006). Osteotome sinus floor elevation without grafting material: A 1-year prospective pilot study with ITI implants. Clinical Oral Implants Research, 17(6), 679–686. https://doi.org/10.1111/j.1600-0501.2006.01264.x
- Nedir, R., Nurdin, N., Vazquez, L., Abi Najm, S., & Bischof, M. (2016). Osteotome sinus floor elevation without grafting: A 10-year prospective study. Clinical Implant Dentistry and Related Research, 18(3), 609–617. https://doi.org/10.1111/cid.12331
- Nizam, N., Eren, G., Akcalı, A., & Donos, N. (2018). Maxillary sinus augmentation with leukocyte and platelet-rich fibrin and deproteinized bovine bone mineral: A split-mouth histological and histomorphometric study. Clinical Oral Implants Research, 29(1), 67–75. https://doi.org/10.1111/clr.13044
- Palma, V. C., Magro-Filho, O., de Oliveria, J. A., Lundgren, S., Salata, L. A., & Sennerby, L. (2006). Bone reformation and implant integration following maxillary sinus membrane elevation: An experimental study in primates. Clinical Implant Dentistry and Related Research, 8(1), 11–24. https://doi.org/10.2310/j.6480.2005.00026.x
- Peterson, J. E., Zurakowski, D., Italiano, J. E. Jr, Michel, L. V., Fox, L., Klement, G. L., & Folkman, J. (2010). Normal ranges of angiogenesis regulatory proteins in human platelets. American Journal of Hematology, 85(7), 487–493. https://doi.org/10.1002/ajh.21732
- Pjetursson, B. E., & Lang, N. P. (2014). Sinus floor elevation utilizing the transalveolar approach. Periodontology 2000, 66(1), 59–71. https://doi.org/10.1111/prd.12043
- Sohn, D. S., Lee, J. S., Ahn, M. R., & Shin, H. I. (2008). New bone formation in the maxillary sinus without bone grafts. Implant Dentistry, 17(3), 321–331. https://doi.org/10.1097/ID.0b013e318182f01b
- Sohn, D. S., Moon, J. W., Moon, K. N., Cho, S. C., & Kang, P. S. (2010). New bone formation in the maxillary sinus using only absorbable gelatin sponge. Journal of Oral Maxillofacial Surgery, 68(6), 1327–1333. https://doi.org/10.1016/j.joms.2010.02.014
- Tatum, H. Jr (1986). Maxillary and sinus implant reconstructions. Dental Clinics of North America, 30(2), 207–229.
- Wallace, S. S., Tarnow, D. P., Froum, S. J., Cho, C. S., Zadeh, H. H., Stoupel, J., … Testori, T. (2012). Maxillary sinus elevation by lateral window approach: Evolution of technology and technique. Journal of Evidence Based Dental Practice, 12(3), 161–171. https://doi.org/10.1016/S1532-3382(12)70030-1
- Winter, A. A., Pollack, A. S., & Odrich, R. B. (2003). Sinus/alveolar crest tenting (SACT): A new technique for implant placement in atrophic maxillary ridges without bone grafts or membranes. International Journal of Periodontics Restorative Dentistry, 23(6), 557–565.
