Computer-guided vs freehand placement of immediately loaded dental implants: 5-year post-loading results of a randomised controlled trial
Purpose: To compare planning and patient rehabilitation using 3D implant planning software and dedicated surgical templates with conventional freehand implant placement for the rehabilitation of partially or fully edentulous patients using flapless or mini-flap procedures and immediate loading.
Materials and methods: Patients requiring at least two implants to be restored with a single prosthesis, having at least 7 mm of bone height and 4 mm in bone width were consecutively enrolled. Patients were randomised according to a parallel group study design into two groups: computer-guided group or conventional freehand group. Implants were loaded immediately with a provisional prosthesis, replaced by a definitive prosthesis 4 months later. Outcome measures assessed by a blinded independent assessor were: implant and prosthesis failures, any complications, marginal bone levels, number of treatment sessions, duration of treatment, post-surgical pain and swelling, consumption of pain killers, surgical and prosthetic time, time required to solve complications, and patient satisfaction. Patients were followed up to 5 years after loading.
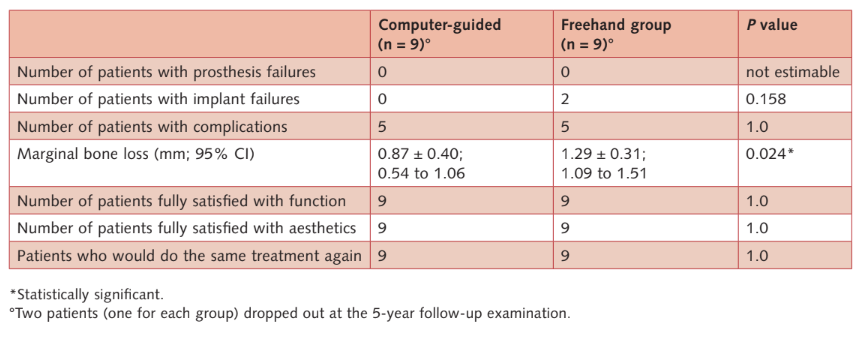
Results: Ten patients (32 implants) were randomised to the computer-guided group and 10 patients (30 implants) were randomised to the freehand group. At the 5-year follow-up examination one patient of the computer-guided group and one of the freehand group dropped-out (both moved to another country). No prostheses failed during the entire follow-up. Two implants failed in the conventional group (6.6%) vs none in the computer-guided group (P = 0.158). Ten patients (five in each group) experienced 11 complications (six in the computer-guided group and five in the freehand group), that were successfully solved. Differences between groups for implant failures and complications were not statistically significant. Five years after loading, the mean marginal bone loss was 0.87 mm ± 0.40 (95% CI: 0.54 to 1.06 mm) in the computer-guided group and 1.29 mm ± 0.31 (95% CI: 1.09 to 1.51 mm) in the freehand group. The difference was statistically significant (difference 0.42 mm ± 0.54; 95% CI: 0.05 to 0.75; P = 0.024). Patient self-reported post-surgical pain (P = 0.037) and swelling (P = 0.007) were found to be statistically significant higher in patients in the freehand group. Number of sessions from patient’s recruitment to delivery of the definitive prosthesis, number of days from the initial CBCT scan to implant placement, consumption of painkillers, averaged surgical, prosthetic, and complication times, were not statistically significant different between the groups. At the 5-year follow-up, all the patients were fully satisfied with the function and aesthetics of their definitive prostheses.
Conclusions: Both approaches achieved successful results over the 5-year follow-up period. Statistically higher post-operative pain and swelling were experienced at sites treated freehand with flap elevation. Less marginal bone loss (0.4 mm) was observed in the computer-guided group, at 5 years follow-up.
Introduction
The growing interest in prosthetically-driven treatment planning, together with the possibility of placing a temporary restoration immediately after implant placement, have led to the development of software capable of virtual planning and manufacturing a surgical guide and a metal-reinforced temporary restoration before surgery.
Guided implant placement was initially supported by enthusiastic preliminary reports, but then received criticism from some uncontrolled prospective studies. These studies supposed that deviations in 3D directions between virtual planning and the actual final position of the implant may compromise the final results. However, favourable long-term survival and success rates and a low incidence of template-related complications were reported by studies. Furthermore, when treatment planning was made on a 3D cone beam computer tomography (CBTC) scan using dedicated software, more postoperative pain and swelling were reported at sites treated freehand. In addition, guided surgery provides significantly higher predictability and accuracy than half-guided surgery in transferring the virtual implant position to the patient’s mouth. Despite these benefits, the use of guided surgery has remained rare due to a supposedly higher time-consuming workflow, the need to purchase dedicated surgical kit, software and guide. Nevertheless, a recent randomised controlled trial comparing computer-guided vs freehand placement of immediately loaded dental implants failed to find a statistically increased number of days from CBCT scan to provisional prostheses, as well as sessions to definitive prostheses. The same study reported slightly higher costs for the dedicate instrumentation compared with the conventional, freehand group, but a higher cost for the computer-aided design/computer-aided manufacture (CAD/CAM) surgical template for guided implant placement. Furthermore, the availability of high-quality 3D desktop printers allows for the cost-effective production of accurate surgical template by dental laboratories.
The aim of this 5-year randomised controlled trial was to update the preliminary 1-year data from partially or fully edentulous patients planned and rehabilitated using 3D implant planning software and customised surgical templates vs freehand implant placement, using flapless or mini-flap procedures and immediate loading8. This study tested the null hypothesis that there were no differences between the two procedures against the alternative hypothesis of a difference. This article is reported according the CONSORT statement for improving the quality of reports of parallel-group randomised trials.
Materials and methods
Study design
This study was originally designed according to a multicentre randomised controlled trial of parallel group design with two arms and independent outcome assessment, when possible. At the start, five centres agreed to participate, but two centres never recruited any patients, so only three centres provided data for the 1-year after loading publication8. However, two out of the three remaining centres never supplied the 5-year data, therefore the present publication presents the data of all the patients of the only centre that followed the patients to 5 years after loading, according to the original study protocol. Patients were recruited and treated from February 2011 until May 2012 in a private practice in Rome and were treated by a single operator (Dr Marco Tallarico).
Patient selection
Any fully or partially edentulous patient, aged 18 years or older, able to sign an informed consent, needing at least two implants under the same prosthesis, with at least 7 mm of bone height and 4 mm in bone width measured on computer tomography (CT) or CBCT scans was eligible for this study. In the case of patients requiring multiple prostheses, only the prosthesis more complex to be delivered was included in this study. The delivered prostheses had to be removable to be able to assess individual implant stability. Immediate post-extractive implants could be placed if the residual socket presented a coronal diameter not wider than 8 mm, there was at least 3 mm of bone below the tooth apex, a planned gap bone-to implant up to 2 mm, and presence of the buccal wall up to 2 mm lower than the most coronal bony peak. Otherwise, if the operator decided to wait for healing of the post-extractive socket, the implant sites had to heal for at least 3 months. Adjacent implants had to be placed with an implant-to-implant distance of at least 3 mm and a distance from implant to tooth of at least 1.5 mm.
Patients were divided into two groups depending on the amount of available bone:
- Simple case: if all implant sites have bone height > 9 mm and bone width > 5 mm.
- Complex case: if at least one implant site has bone height between 7 mm and 9 mm and/or bone width between 4 mm and 5 mm.
Patients were not admitted in the study if any of the following exclusion criteria were present:
- General contraindications to implant surgery;
- Subjected to irradiation in the head and neck area less than 1 year before implantation;
- Untreated periodontitis;
- Poor oral hygiene and motivation;
- Uncontrolled diabetes;
- Pregnant or nursing;
- Substance abuse;
- Psychiatric problems or unrealistic expectations;
- Severe bruxism or clenching;
- Immunosuppressed or immunocompromised;
- Treated or under treatment with intravenous amino-bisphosphonates;
- Lack of opposite occluding dentition/prosthesis in the area intended for implant placement;
- Active infection or severe inflammation in the area intended for implant placement;
- Need of bone augmentation procedures at implant placement;
- Unable to open mouth sufficiently to accommodate the surgical tooling;
- Any ‘complex case’ if implants had to be placed in the aesthetic zone defined as second to second maxillary premolars;
- Patients participating in other studies, if the present protocol could not be properly followed;
- Referred only for implant placement or unable to attend a 5-year follow-up;
- Requiring only single implant-supported crowns.
Patients were categorised into three groups according to what they declared: non-smoker; moderate smoker (up to 10 cigarettes per day); and heavy smoker (more than 10 cigarettes per day).
Prior to being enrolled, all patients received detailed explanations and signed a written informed consent form. Two separate CBCT or CT scans were made according to the double-scan protocol.
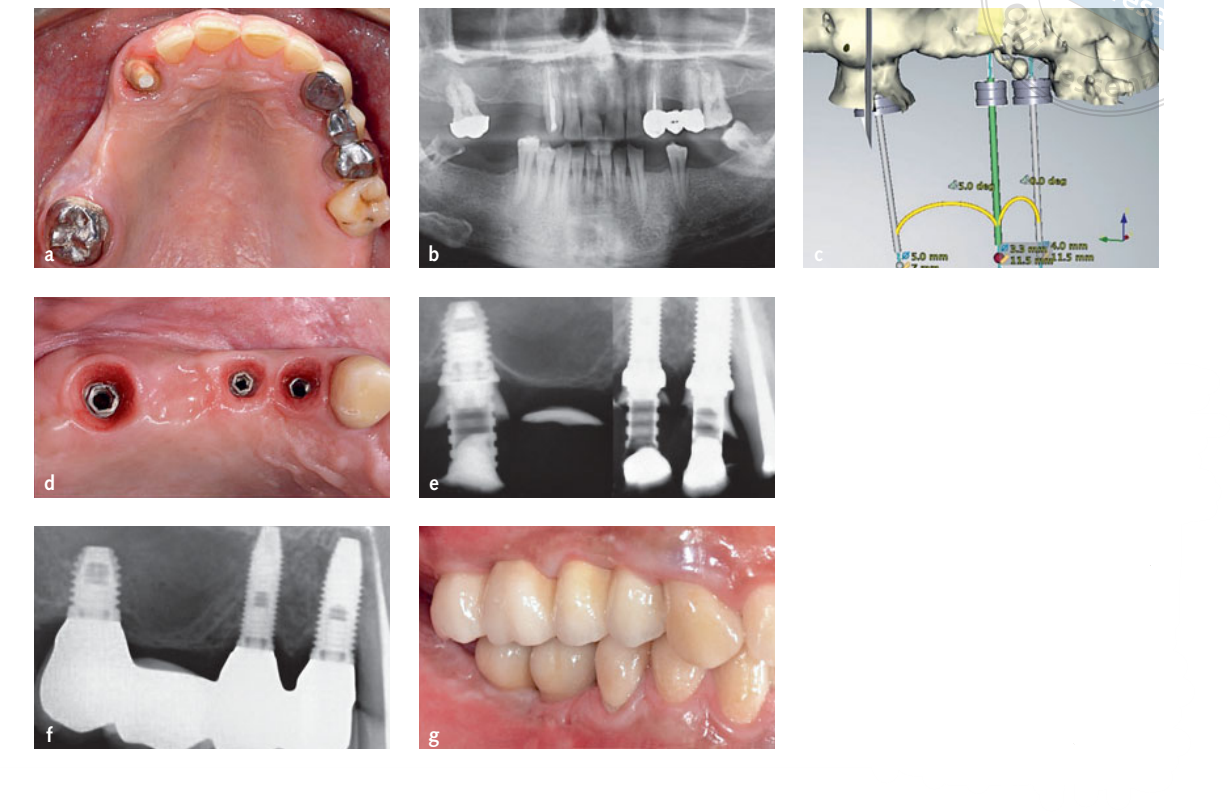
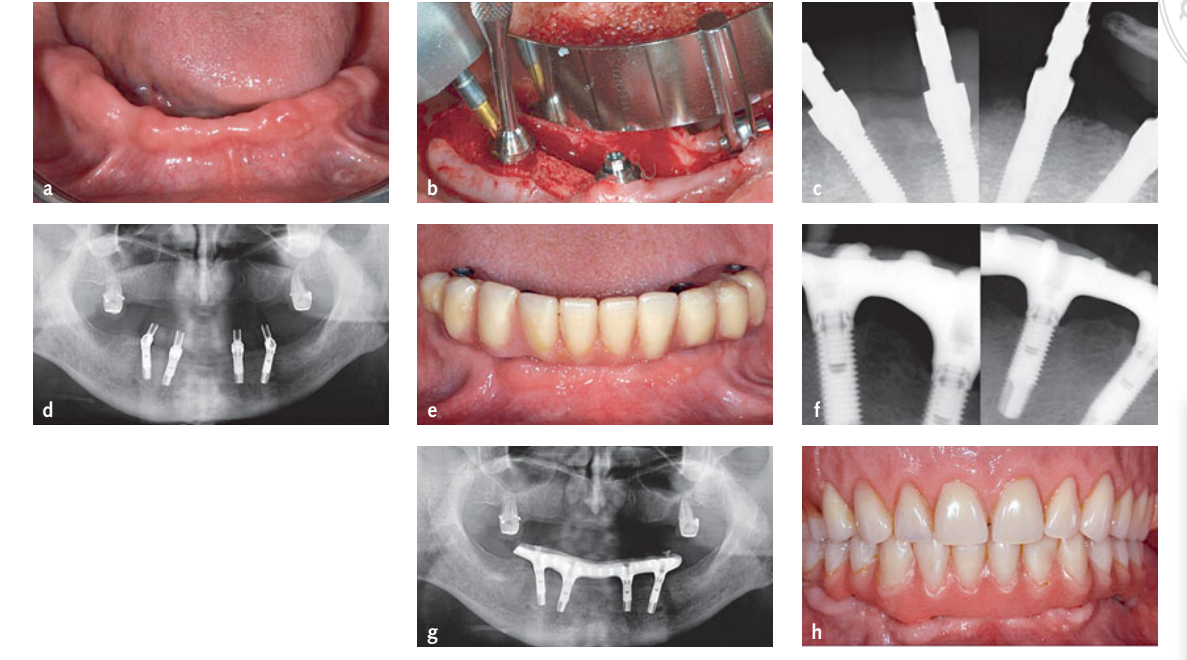
Planning procedures
The Digital Imaging and Communication in Medicine (DICOM) data of the two sets of scans were transferred to a 3D implant planning software (NobelGuide, Nobel Biocare, Kloten, Switzerland) and matched to each other. After prosthetically driven virtual planning was approved, patients were randomly allocated either to the computer-guided group (Figs 1a to g) or to the freehand group (Figs 2a to h), according to a parallel group design, following the indications contained in a sequentially numbered envelope. Planning data of the patients allocated to the computer-guided group were sent to a milling centre located in Sweden (NobelProcera, Nobel Biocare), where stereolithographic surgical templates were fabricated. In all patients, a metal-reinforced, screw-retained, provisional acrylic resin restoration, without any cantilever, was prefabricated for immediate implant loading. In the computer-guided group, the stereolithographic surgical template was used to pour the preoperative master casts with the implant replicas in place, while in the freehand group, the master cast used to produce the radiographic template was used. No stents were made for patients allocated to the freehand group.
Surgical procedures
All patients received 2 g of amoxicillin (or 600 mg clindamycin, if allergic to penicillin) 1 h before implant placement and rinsed with chlorhexidine mouthwash 0.2% for 1 min prior to the intervention. All patients were treated under local anaesthesia using articaine with adrenaline 1:100000. In the computer-guided group, the fit of the surgical templates was checked before surgery. Then, the surgical templates were stabilised using the silicone surgical index derived from the mounted casts, and fixed with two to three pre-planned anchor pins.
In both groups, parallel-walled implants with external connection and an oxidised surface (Nobel Speedy Groovy, Nobel Biocare) were placed flapless or with a minimally invasive flap. Implant sites were prepared according to the manufacturer’s guidelines using the Brånemark System surgery kit (Nobel Biocare, freehand group), or the Brånemark System Guided Surgery Kit, in combination with a customised surgical template (Nobel Biocare, computer-guided group). Implants were to be inserted with an insertion torque of more than 35 Ncm (torque wrench, Nobel Biocare). In the computer guided-group, the insertion torque was measured after the surgical template was removed. After implant placement, non-engaging, titanium temporary abutments (Nobel Biocare) were screwed directly to the implants or to the intermediate straight or angulated multi-unit abutments (MUA, Nobel Biocare). If needed, flaps were sutured around the abutments using expanded polytetra-fluoroethylene dental sutures (American Dental System, Vaterstetten, Germany). The prefabricated provisional restorations were relined on to the temporary abutments using an auto-polymerising polyurethane resin (Voco, Cuxhaven, Germany), then refined and polished. Occlusion was carefully assessed avoiding any lateral contact. Patients were instructed to use 0.2% chlorhexidine mouthwash for 1 min twice a day for 2 weeks, to follow a soft diet for 1 month, and to avoid brushing and trauma on the surgical sites. Patients were also provided with 12, 600 mg tablets of ibuprofen, or for patients allergic to NSAIDs, 12 tablets of 1 g paracetamol two to four times a day in case of pain. Patients were recalled after 3 days to check occlusion and to evaluate their reported pain, swelling and consumption of analgesics, and were recalled again 7 days after implant placement to recheck occlusion, suture removal (if required), and to deliver oral hygiene instructions.
Prosthetic procedures
Four months after initial loading, definitive impressions were taken using an open, customised, impression tray (Elite LC tray, Zhermack SpA, Badia Polesine, Rovigo, Italy). Definitive ceramic (partial restorations) or composite (full-arch restorations), titanium prostheses were screw-retained at implant or abutment level. One month after delivery of definitive prostheses, patients were recalled, occlusion and oral hygiene was checked and the blind outcome assessor evaluated patient satisfaction. Patients were then enrolled on an oral hygiene programme and occlusion checks with recall visits every 6 months. Blinded outcome assessors conducted follow-ups up to 5 years after initial loading.
Outcome measures
Primary outcome measures were:
- Prosthesis failure: planned prosthesis which could not be placed due to implant failure(s), loss of the prosthesis secondary to implant failure(s), and any prosthesis which had to be replaced during the entire follow-up period.
- Implant failure: implants which had to be removed at implant insertion due to lack of stability, implant mobility, removal of stable implants dictated by progressive marginal bone loss or infection, and any mechanical complications (e.g. implant fracture) rendering the implant unusable. The stability of individual implants was assessed with the prostheses removed at delivery of definitive prostheses (4 months post-loading), at 1 and 5 years after initial loading, by tightening the abutment screw with a torque of 20 Ncm.
Any biological or prosthetic complications experienced during the entire follow-up.
Secondary outcome measures were:
- Marginal bone levels were evaluated on periapical digital radiographs taken with the paralleling technique using a film-holder (Rinn XCP, Dentsply, Elgin, IL, USA) at implant placement and at 1 and 5 years after initial loading. In cases where the marginal bone levels around the study implants were hidden or difficult to read, a second radiograph was taken. At baseline and at the 1-year follow-up, marginal bone levels were measured using the Kodak Digital Imaging Software 6.11.7.0 (Kodak, Eastman Kodak Company, Rochester, NY, USA); at the 5-year follow-up, the DfW 2.8 image analysis program (Soredex, Tuusula, Finland) was used. The software was calibrated for every single image using the known implant diameter. Measurements of the mesial and distal bone crest level adjacent to each implant were made to the nearest 0.01 mm and averaged at patient level and group level. Reference points for the linear measurements were the most coronal margin of the implant collar and the most coronal bone-to-implant contact. The marginal bone loss was calculated as the difference between marginal bone levels.
- Number of sessions with the patient from recruitment to delivery of the definitive prosthesis.
- Days from the initial CBCT scan to implant placement.
- Patient self-reported post-surgical pain: on an ordinal scale: 0 = no pain; 1 = mild pain; 2 = moderate pain; 3 = severe pain, assessed 3 days after surgery at the postoperative check-up visit by the blinded assessors.
- Patient self-reported post-surgical swelling, on an ordinal scale: 0 = no swelling; 1 = mild swell- ing; 2 = moderate swelling; 3 = severe swelling, assessed 3 days after surgery at postoperative
- Check up visit by the blinded assessors.
- Consumption of painkillers: how many tablets out of the 12 provided painkiller tablets (400 mg ibuprofen, or 1 g paracetamol for those allergic to NSAIDs) were used, recorded 3 days after surgery at the postoperative check-up visit by the blinded assessor.
- Treatment time (in min) divided into:
- Surgical time: from the delivery of local anaesthesia to the placement of last abutment or suture.
- Prosthetic time: total time employed to deliver and adapt the provisional fixed prosthesis, including occlusal, phonetic, and aesthetic adjustments.
- Complication time: total time required to solve any complications at the office and in laboratory after delivery of the provisional prosthesis.
- Patient satisfaction was evaluated with a questionnaire 1 month after delivery of the final prosthesis and 5 years after loading provided by independent blinded outcome assessor. The assessor asked the following questions:
- Are you satisfied with the function of your implant-supported prosthesis? Possible answers: yes absolutely; “yes partly”; “not sure”; “not really”; “absolutely not”.
- Are you satisfied with the aesthetic outcome of your implant supported prosthesis? Possible answers: yes absolutely; “yes partly”; “not sure”; “not really”; “absolutely not”.
- Would you undergo the same therapy again? Possible answers: “yes” or “no”.
- Patients’ comments were also recorded.
Statistical analysis
All data analyses were carried out according to a pre-established analysis plan. A bio-statistician with expertise in dentistry analysed the data using SPSS for Windows release 18.0 (SPSS, Chicago, IL, USA), without knowing the group codes. The patient was the statistical unit of the analyses. Differences in the proportion of patients with prosthesis failures, implant failures and complications (dichotomous outcomes) were compared between the groups using the Fisher’s exact probability test. Differences of means at patient level for continuous outcomes (bone levels, number of treatment sessions and time needed to complete the procedures) between groups were compared by independent sample t tests. Comparisons between each time point and the baseline measurements were made by paired tests, to detect any changes in marginal bone levels. The Mann-Whitney U test was used to compare the medians of the two groups for postoperative pain, swelling and patient satisfaction. All statistical comparisons were conducted at a 0.05 level of significance.
Results
Originally, 20 patients were to be recruited at each of five different Italian private practices. Only three centres actually participated in the study, but only one centre (Dr Marco Tallarico) followed the patients 5 years after loading, according to the original study protocol. A total of 22 patients were screened and 20 patients were consecutively enrolled for the trial. Two patients were not included because they refused to have CBCT scans taken. At the end, 10 patients (32 implants) were randomised to the computer-guided group and 10 patients (30 implants) were randomised to the freehand group.
At the 5-year follow-up examination one patient of the computer-guided group and one of the free-hand group dropped-out (both moved in another country). The following deviations from the original research protocol occurred: one patient of the free-hand group who lost one out of two implants did not want to have it replaced and had to be rehabilitated with a prosthesis connecting the residual implant with natural tooth; in another patient of the freehand group three out of six of the maxillary implants placed did not achieve an insertion torque of at least 35 Ncm and therefore they were conventionally loaded after 6 months; finally one patient of the computer-guided group had one of the two implants placed with less than 35 Ncm, however it was immediately loaded anyway.
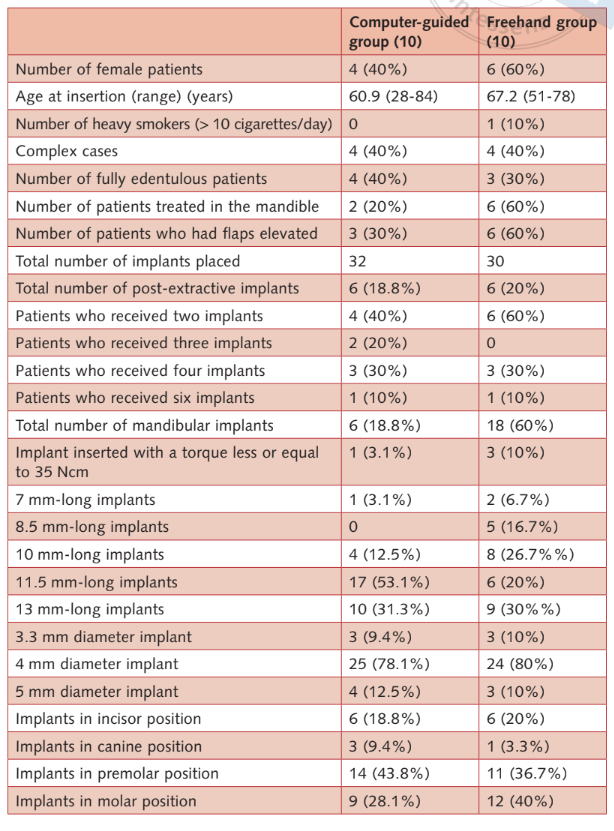
There were no apparent baseline imbalances between the two groups apart for the presence of more mandibular implants, 8.5 mm long implants and less 11.5 mm long implants in the freehand group. Patients’ and interventions’ characteristics are summarised in Table 1. Groups appeared balaced with the exception of implant lenght, since implants in the computer-guided group appeared on average to longer than those in the free-hand group.
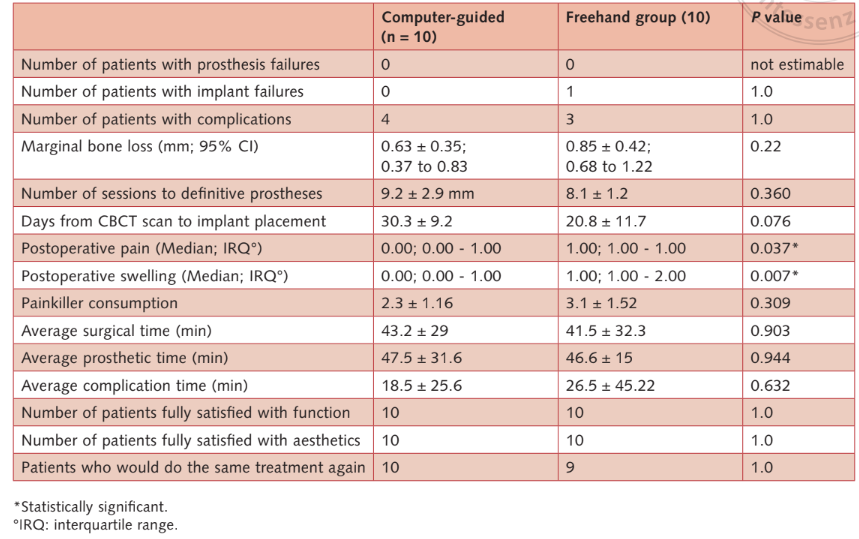
- Prosthesis failures: no prosthesis failed during the entire follow-up.
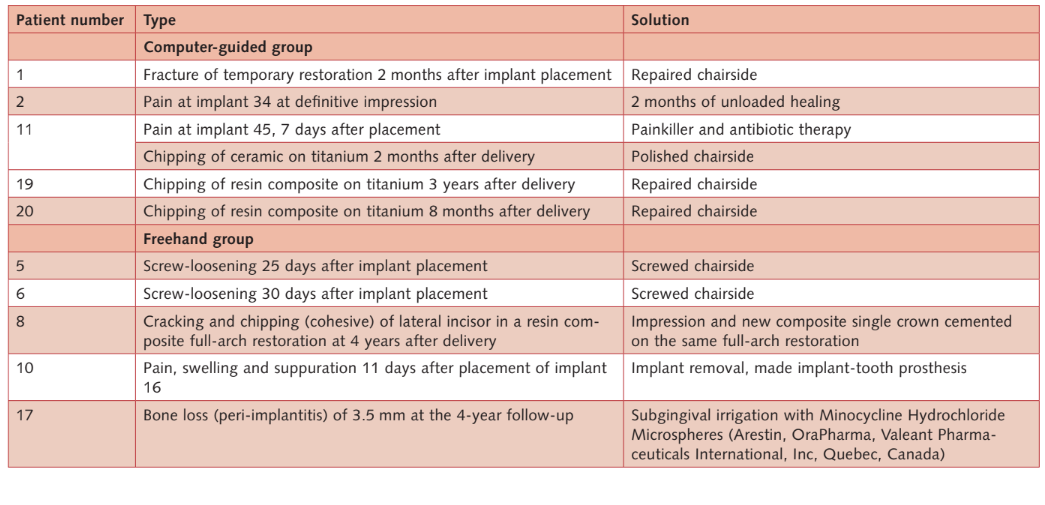
- Implant failures: Two implants failed in the free-hand group vs none in the computer-guided group. One maxillary implant failed in a female heavy smoker 11 days after implantation, due to an infection with suppuration. The implant was removed and the infection treated. The temporary prosthesis was modified chair side connecting the residual implant in position 17 and tooth 15. Patients refused to replace it in favour of a hybrid implant-tooth supported restoration. The second implant (mandibular anterior implant) failed at the 5-year follow-up examination in a female patient rehabilitated with a screw-retained fixed dental prosthetic on four implants. The prosthesis was modified on the remaining three implants. At the 5-year follow-up examination, two implants failed in the conventional group (6.6%) vs none in the computer-guided group. The difference was not statistically significant (P = 0.158; odds ratio = 0.007 to 3.811) (Tables 2a and b).
- Complications: 10 patients (five in each groups) experienced 11 complications (six in the computer-guided group and five in the freehand group; Table 2b) that were successfully solved (Table 3).The difference was not statistically significant (P = 1.0; odds ratio = 1.0; 0.213 to 4.693).
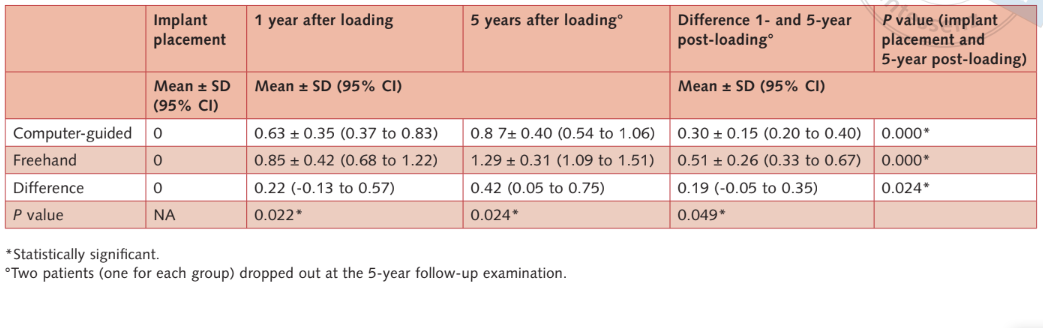
- Marginal bone levels: all the implants were placed with the most coronal margin of the implant collar at bone level or slightly below. One year after loading, the mean marginal bone level/loss was 0.63 mm ± 0.35 (95% CI: 0.37 to 0.83 mm) in the computer-guided group and 0.85 mm ± 0.42 (95% CI: 0.68 to 1.22 mm) in the freehand group (difference 0.22 mm ± 0.55; 95% CI: -0.13 to 0.57; P = 0.22). At the 5 years after loading follow-up, the mean marginal bone level/loss was 0.87 ± 0.40 (95% CI: 0.54 to 1.06 mm) in the computer-guided group and 1.29 mm ± 0.31 mm (95% CI: 1.09 to 1.51 mm) in the freehand group. The difference was statistically significant (difference 0.42 mm; 95% CI: 0.05 to 0.75; P = 0.024) (Tables 2a and b). Bone levels/loss are detailed in table (Table 2c).
- Number of sessions from a patient’s recruitment to delivery of the definitive prosthesis, and the number of days from the initial CBCT scan to implant placement were not statistically significant different between groups (Table 2a).
- Patients’ self-reported post-surgical pain and swelling were found to be statistically significant higher for the patients of the freehand group (Table 2a).
- Consumption of painkillers: no statistically significant differences were observed between the two groups (Table 2a).
- Averaged surgical, prosthetic, and complication times: no statistically significant differences were observed between the two groups (Table 2a).
- Patient satisfaction: All patients were fully satisfied with the function and aesthetics of their definitive prostheses, at both 1 month after delivery of the final prosthesis and 5 years after loading. Only one patient from the freehand group declared, 1 month after delivery of the final prosthesis, that he would not undergo the same treatment again. No statistically significant difference was observed between the two groups (Table 2a).
Discussion
This randomised controlled trial was conducted with the aim of understanding which procedure was preferable – after having planned the intervention with a dedicated software on a 3D CBCT scan – between computer-guided surgery using a surgical template and freehand implant placement.
The main limitation of the present study is the limited number of participants that may have hidden some differences between treatments. Unfortunately, only one of the three centres originally involved in the study followed the patients for the 5-year follow-up.
Despite the evident advantages related to less post-operative pain and swelling, there is still the need to clinically evaluate the long-term aesthetic and functional advantages of the computer-guided template-assisted surgery. To the best of our knowledge this is the only RCT comparing freehand surgery and guided surgery at a 5-year follow- up. Nevertheless, the results of both groups are in accordance to other studies where the same implants were used.
In the present study, both techniques achieved successful results, and no statistically significant differences were observed between groups, with the exception of less postoperative self-reported pain and swelling for patients having implants placed using computer-guided surgery. Moreover, patients in the computer-guided group experienced statistically lower marginal bone loss compared with patients in the freehand group, at both 1 and 5-year follow-ups. However, the clinical relevance might be controversial since the difference of 0.4 mm may not be considered as clinical relevant. In fact, high statistically relevance was found at the 1-year examination (P = 0.022), compared with the difference between the 1- and 5-year follow-ups (P = 0.049). A possible explanation of these differences could be that twice patients in the freehand group had a flap elevated. Nevertheless, there is no evidence of significant effects of flapless technique on the marginal bone loss15,16. More likely, the lower sample size and the dropouts may have underpowered the results. Low powered studies reduce the chance of detecting a true effect, as well as, low they reduce the likelihood that a statistically significant result reflects a true effect. In fact, in the 1-year preliminary report of the present study, reporting data from three centres (51 patients), the marginal bone loss was not statistically significant different between groups.
Treatment planning involving implants has changed to a patient-centred, prosthetically driven approach, allowing for preoperative implant planning and proper communication with the patient, surgeon and the prosthodontist. The main purpose of the diagnostic set-up scan is to pre-visualise the approved prosthetic design of the tooth/teeth to be replaced, and to relate it/them with the patient’s available soft and hard tissues. Therefore, implant position can be optimised according to the aesthetic and functional needs, and an interim prosthesis can be manufactured prior to the surgical procedure, allowing for an immediate function.
In the present study both techniques were tested in real clinical situations, therefore the results of the present trial could be generalised to larger populations with similar characteristics. The authors recommend the use of dental planning software to make a diagnosis and a prosthetically driven approach to the treatment plan. However, the clinician’s experience, training, respect of the protocols, and reasoning skills (learning curve) are all needed to perform every surgical and prosthetic step as best as possible.
Conclusions
Results of the present study seem to validate both approaches over the 5-year follow-up period. Higher post-operative pain and swelling were experienced at sites treated freehand. Less marginal bone loss (0.4 mm) was observed at implants placed with guided surgery, at the 5-year follow-up. These preliminary findings should be validated by further studies with larger samples.
Marco Tallarico, Marco Esposito, Erta Xhanari, Marco Caneva, Silvio Mario Meloni
References
- van Steenberghe D, Glauser R, Blomback U, AnderssonM, Schutyser F, Pettersson A, Wendelhag I. A computed tomographic scan-derived customized surgical template and fixed prosthesis for flapless surgery and immediate loading of implants in fully edentulous maxillae: a prospective multicenter study. Clin Implant Dent Relat Res 2005;7(Suppl 1):S111–120.
- Sanna AM, Molly L, van Steenberghe D. Immediately loaded CAD-CAM manufactured fixed complete dentures using flapless implant placement procedures: A cohort study of consecutive patients. J Prosthet Dent 2007;97:331–339.
- Komiyama A, Klinge B, Hultin M. Treatment outcome of immediately loaded implants installed in edentulous jaws following computer-assisted virtual treatment planning and flapless surgery. Clin Oral Implants Res 2008;19:677–685.
- Johansson B, Friberg B, Nilson H. Digitally planned, immediately loaded dental implants with prefabricated prostheses in the reconstruction of edentulous maxillae: a 1-year prospective, multi- center study. Clin Implant Dent Relat Res 2009;11:194–200.
- Pettersson A, Komiyama A, Hultin M, Näsström K, Klinge B. Accuracy of virtually planned and template guided implant surgery on edentate patients. Clin Implant Dent Relat Res 2012;14:527–537.
- Tallarico M, Meloni SM. Retrospective analysis on survival rate, template-related complications, and prevalence of peri-implantitis of 694 anodized implants placed using computer-guided surgery: results between 1 and 10 years of follow-up. Accepted for publication. Int J Oral Maxillofac Implants 2017 (https://www.manuscriptmanager.com/v6/forthcoming_list.php).
- Pozzi A, Holst S, Fabbri G, Tallarico M. Clinical reliability of CAD/CAM cross-arch zirconia bridges on immediately loaded implants placed with computer-assisted/template-guided surgery; a retrospective study with follow-up between 3 and 5 years. Clin Implant Dent Relat Res 2015;17(Suppl 1):e86-96.
- Pozzi A, Tallarico M, Marchetti M, Scarfo B, Esposito M. Computer-guided versus free-hand placement of immediately loaded dental implants: 1-year post-loading results of a multicentre randomised controlled trial. Eur J Oral Implantol 2014;7:229–242.
- Bover-Ramos F, Vina-Almunia J, Cervera-Ballester J, Peñarrocha-Diago M, García-Mira B. Accuracy of Implant Placement with Computer-Guided Surgery: A Systematic Review and Meta-Analysis Comparing Cadaver, Clinical, and In Vitro Studies. Int J Oral Maxillofac Implants 2017.
- Neumeister A, Schulz L, Glodecki C. Investigations on the accuracy of 3D-printed drill guides for dental implantology. Int J Comput Dent 2017;2035-2051.
- Tallarico M, Canullo L, Pisano M, Penarrocha-Oltra D, Peñarrocha-Diago M, Meloni SM. An up to 7-Year Retrospective Analysis of Biologic and Technical Complication With the All-on-4 Concept. Journal of Oral Implantology 2016;42:265–271.
- Tallarico M, Meloni SM, Canullo L, Caneva M, Polizzi G. Five-Year Results of a Randomized Con- trolled Trial Comparing Patients Rehabilitated with Immediately Loaded Maxillary Cross-Arch Fixed Dental Prosthesis Supported by Four or Six Implants Placed Using Guided Surgery. Clin Implant Dent Relat Res 2016;18:965–972.
- Meloni SM, Tallarico M, Pisano M, Xhanari E, Canullo L. Immediate Loading of Fixed Complete Denture Prosthesis Supported by 4-8 Implants Placed Using Guided Surgery: A 5-Year Prospective Study on 66 Patients with 356 Implants. Clin Implant Dent Relat Res 2017;19:195–206.
- Pozzi A, Tallarico M, Moy PK. Three-year post-loading results of a randomised, controlled, split-mouth trial comparing implants with different prosthetic interfaces and design in partially posterior edentulous mandibles. Eur J Oral Implantol 2014;7:47–61.
- Pisoni L, Ordesi P, Siervo P, Bianchi AE, Persia M, Siervo S. Flapless Versus Traditional Dental Implant Surgery: Long-Term Evaluation of Crestal Bone Resorption. J Oral Maxillofac Surg 2016;74: 1354–1359.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Flapless versus conventional flapped dental implant surgery: a meta-analysis. PLoS One 2014;9:e100624.

