Accuracy of newly developed sleeve-designed templates for insertion of dental implants: A prospective multicenters clinical trial
Abstract
Background: The insertion of dental implants by means of computer-assisted template-based surgery is an established method.
Purpose: To investigate the accuracy of a newly developed sleeve-designed template and to evaluate differences between maxillary and mandibular implants as well as anterior versus posterior area. Materials and Methods: Any partially edentulous patients requiring at least one implant to be planned on three-dimensional cone beam computed tomography scan, according to a computer-assisted template-based protocol, were consecutively enrolled at two centers. Any potential implant position was considered eligible for the present trial. Outcome measures were: implant failure, complications, and accuracy.
Results: A total of 39 patients with 119 implants were evaluated. No patients dropped out during the study period (mean follow-up 12.4 ± 7.1 months). Three implants failed at centre two, whereas, one complication was experienced at centre one (limited access in posterior area). Differences were not statistically significant (P > .05). The mean deviations were 0.53 ± 0.46 mm (range 0.05-3.38 mm; 95% CI 0.32-0.48 mm) in the horizontal plan (mesiodistal); 0.42 ± 0.37 mm (range 0.0-1.53 mm; 95% CI 0.26-0.40 mm) in the vertical plan (apico-coronal); and 1.43 ± 1.98° (range 0.03-11.8°; 95% CI 0.31-1.01°) in angle. Differences between centers were compared using the nonparametric Mann-Whitney U test (P > .05). More accurate results were found for anterior implants in both horizontal plan and angle.
Conclusion: This study showed good precision in all the parameters measured. The results were thus in a range equal to or better than the mean precision found in numerous clinical trials described in the literature. Posterior implants were less accurate because of the use of open sleeves template.
Introduction
The insertion of dental implants by means of computer-assisted template-based surgery is an established method. One of the most important stages for the development of guided implant placement has been the diffusion of 3-dimensional imaging technique and modern implant planning softwares. The increased demand for dental implants to replace teeth has encouraged advancement in digital technology to improve patients' acceptance and clinical outcomes. Recently, the evaluation of digital data from intraoral optical scanner (IOS) has been shown to be a viable option for the rehabilitation of partial edentulous patients when computer-guided template-assisted implant placement is used. Among the advantages of digital technologies, intraoral digital impression may reduce the number of appointments, resulting in shorter treatment time.
Glossary of prosthodontic terms defines surgical template (or surgical guide) as “a guide used to assist in proper surgical placement and angulation of dental implants”. Implant survival rate has been showed similar for conventional and computer-guided template-assisted implant placement procedures. Furthermore, the reduction of postoperative pain and surgical time, as well as lower marginal bone loss after 5 years of function were founded placing implants with a template-based approach.
The main purpose of the surgical template is to guide the implant drilling system and provide accurate placement of the implant according to the virtual treatment plan. At now, guided surgery is based on metal sleeves integrated into the surgical guides, through which dedicate drill are used. Hence, surgical template represents the union of guiding cylinders (sleeves) and contact surface. The contact surface fits either on hard and soft tissues giving stability. Cylinders works as a drill guides orienting the drill in the exact location and direction.
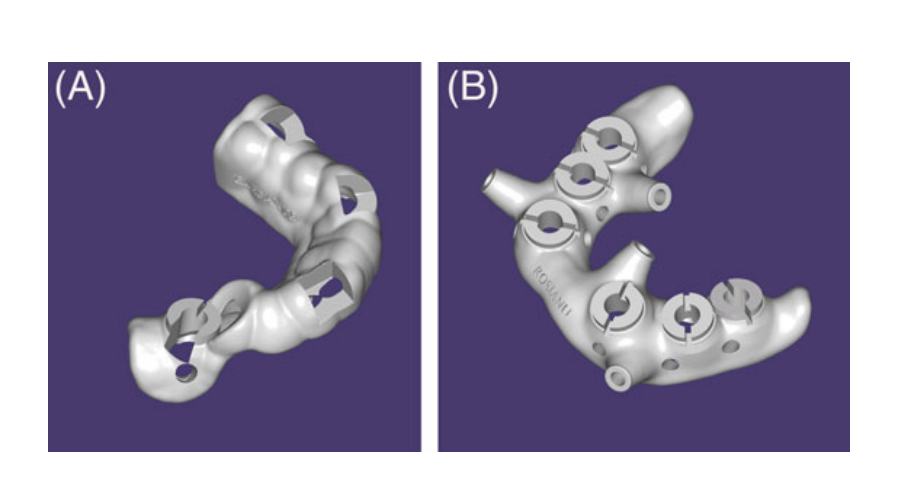
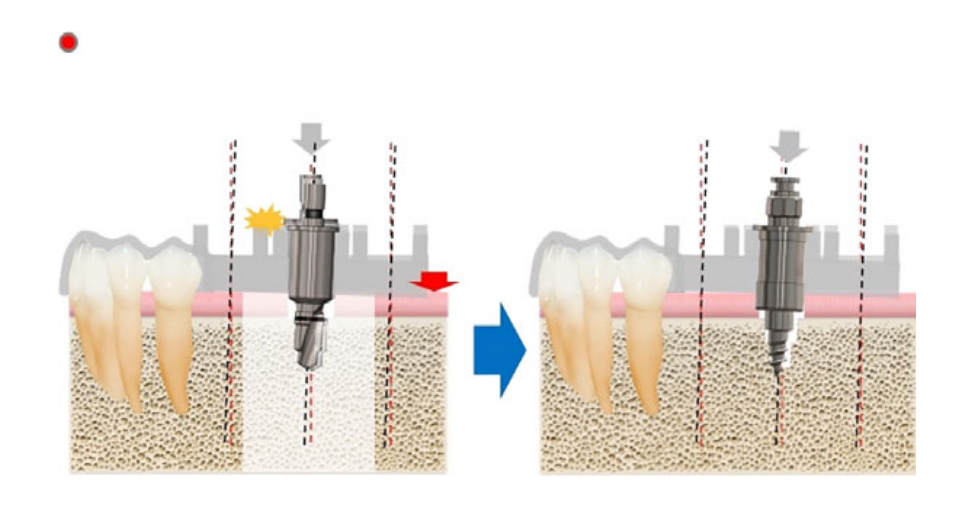
Additive manufacturing, including stereolithography, is becoming predominant for the fabrication of surgical templates, because of the upcoming technological developments. Conventionally, the polymeric prototype contains holes for metallic (stainless steel or titanium) drill-guiding sleeves, which accommodate a vast majority of guided surgical kits. Recently, new in-built sleeve-designed templates have been introduced with the aim to make guided surgery work-flow faster and easier. One of the advantages of this templates is the less mesio-distal space required for its fabrication because of the lack of steel or titanium drill-guiding sleeves. Moreover, sleeve-designed templates can be produced with a vestibular or buccal slot (open site) that allows the horizontal insertion of the drills, reducing the need of inter-arches space and also reducing the bone heating because of a direct saline irrigation on the drill. Furthermore, sleeve-designed templates should be easier to produce and probably less expensive because of the absence of stainless steel or titanium drill-guiding tubes. For these reasons too, cost-effective high quality desktop 3-dimensional printers, recently introduced to the dental market, make in-house surgical templates production affordable. Nevertheless, there is still lack of data in their accuracy.
The aim of the present study is to compare early implant failure, template-related complications, and virtual planning accuracy of computer-assisted template-based implant placement using computer-aided design (CAD)/computer-aided manufacturing (CAM) stereolithographic surgical templates with or without metallic sleeves. Furthermore, to compare open versus closed holes in case of sleeve-designed templates. The null hypothesis was that there would be no differences between these interventions. This trial is reported in accordance with the STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) statement (https://www.strobe-statement.org/) for improving the quality of reporting of observational studies.
Materials and methods
This investigation was designed as multicenter single cohort prospective study conducted according to the principles embodied in the Helsinki Declaration of 2008. Surgical and prosthetic procedures were performed at two centers by two expert clinicians (MT and J-YK) between July 2016 and May 2018.
The study was performed before approval was received from the institutional review board of the Aldent University, Tirana, Albania (2/2017). All participants were enrolled and treated in the study in consecutive order after being informed about the nature of the study and providing their written consent.
Any partially edentulous patient with at least five remaining teeth in two quadrants, aged 18 years or older, able to sign an informed consent, and in need of an implant-supported fixed restoration was considered eligible for this study and consecutively enrolled. Any potential implant position, based on individual patient requirements was considered eligible for the present trial. Patients were not admitted to the study if any of the following exclusion criteria was present: general medical contraindication to oral surgery (American Society of Anesthesiologist, ASA, class III or IV); irradiation in the head and neck area less than 1 year before implantation; psychiatric problems; alcohol or drug abuse; pregnant or nursing; untreated periodontitis; need to bone reconstruction; severe bruxism or clenching; uncontrolled diabetes; poor oral hygiene and motivation; and inability to complete the follow-up.
All patients received preoperative photographs, periapical radiographs or panoramic x-rays for initial screening and evaluation. Enrolled patients receive a cone beam computed tomography (CBCT) scan, by using a wax bite to separate dental arches and a complete digital impression (3M True Definition Scanner, 3M Italia, Pioltello, Milano), according to a previously published manuscript. Afterwards, a virtual wax-up was performed, according to the functional and esthetic requirements. Then, the DICOM (Digital Imaging and COmmunications in Medicine) data derived from the CBCT scan and the STL (STereo Lithography interface format, STL) data derived from the impression and the virtual wax-up, were imported in a 3-dimensional software planning program (3Diagnosys ver. 4.2, 3DIEMME srl, Cantù, Italy at centre one and Implant studio, 3Shape A/S, Copenhagen, Denmark at centre two). At this point, prosthetic-driven implants/abutments size and location were planned taking into account the bone quality and quantity, soft tissue thickness, anatomical landmarks, as well as, type, volume and shape of the final restoration. After careful functional and esthetic evaluation and final verification, the prosthetic-driven plan was approved. Finally, a stereolithographic surgical template was designed and then fabricated by an independent certified center not previously involved in the study (New Ancorvis srl, Bargellino, Italy). All the surgical templates were designed with a minimum of three inspection windows of 4-5 mm of diameter. The thickness of the surgical templates was 2.5 ± 0.5 mm. Dental LT Clear (Formlabs Inc, Somerville, Massachusetts) was print resolutions of 100 μm. After printing, all the surgical templates were cleaned with isopropyl alcohol and then dried. Finally, postcuring was performed for 8 minutes. At centre one, the surgical templates were sleeve-designed with closed hole in case of implants to be place between premolars, while, open holes were designed for molars replacement. While, at centre two, all the surgical templates were sleeve-designed with closed holes (Figure 1,B).
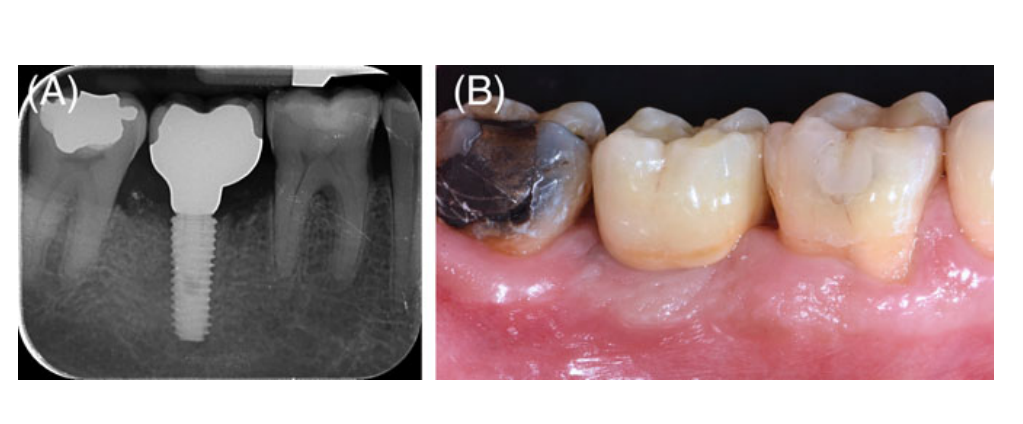
One hour before implant placement, all patients underwent professional oral hygiene, prophylactic antiseptic with 0.2% chlorhexidine for 1 minute, and prophylactic antibiotic therapy (2 g of amoxicillin or clindamycin 600 mg if allergic to penicillin). The fit of the surgical templates were tried directly in the patient mouth to achieve a stable fit (Fit Checker, GC – Tokyo, Japan). All patients were treated under local anesthesia using articaine with adrenaline 1:100.000 administered 20 minutes before surgery. The surgical templates were stabilized in relation to the opposing arch using a rigid surgical index derived from the virtual plan, and with two to four preplanned anchor pins. Planned implants (Osstem TSIII, Osstem, Seoul, South Korea) were placed flapless or with a minimally invasive flap using dedicated drills (OsstemGuide Kit[Taper], Osstem). The implant site was prepared based on the bone density evaluated by the surgeon at the first drill. The flaps (if present) were then sutured with Vicryl 4.0 sutures (Vicryl, Ethicon J&J International, Sint-Stevens-Woluwe, Belgium). Immediately after implant placement, patients of both groups received a digital impression taken at implant level using dedicated abutments, to check the position of the placed implants. Hopeless teeth were extracted at the end of the intervention in order to improve the stability of the surgical template and to provide more reference point in the postoperative STL files, for measurements of the implant accuracy. Following implant placement, preplanned provisional restorations were immediately delivered to the patients, according to an immediate loading protocol. Finally, all patients received oral and written recommendations about medication, oral hygiene maintenance and diet. Suture (if present) were removed 10-14 days later, after local cleaning by using 0.2% chlorhexidine.
Three to four months after implant placement, definitive impressions were taken using a customized open tray. Definitive restorations were delivery 1 month later. Investigators were free to deliver cemented or screw-retained prostheses, which could be either stock or fabricated with CAD/CAM technology, including angle screw channel solution. Occlusion was adjusted avoiding any premature contact. Patients were followed every three to 6 months for hygiene maintenance and occlusion controls (Figures 2–6).



Outcome measurements
Implant failure: an implant was considered to be a failure if it had to be removed because of lack of stability, implant mobility, progressive marginal bone loss or infection, and any mechanical complications (eg, implant fracture) rendering the implant unusable. The stability of individual implants was assessed during the delivery of definitive crowns by tightening the abutment screw with a torque of 20 Ncm, and then 1 year after implant placement by the percussion test.
Early surgical and template-related complications (limited access in posterior areas, buccal bony dehiscence because of a mismatching of the surgical template, insertion of different implant than planned, and fracture of surgical template) were recorded. All the complications were recorded during follow-up by the same expert clinicians that perform the implant surgery (MT and J-YK).
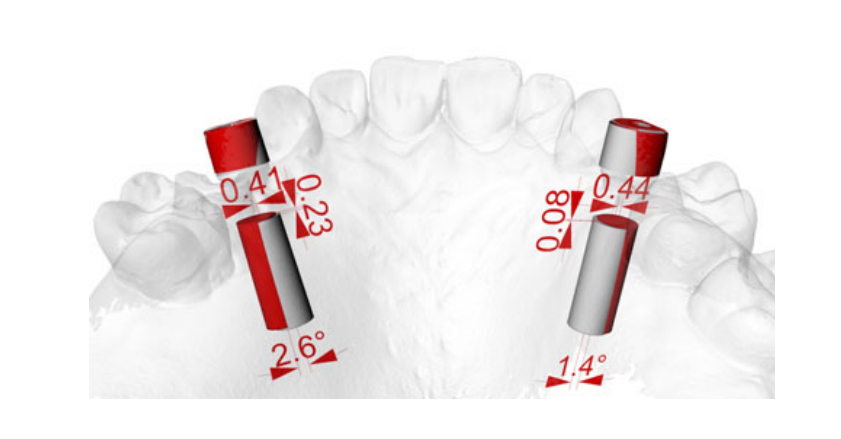
Measurements of accuracy. Three deviation parameters (horizontal, vertical, and angular) were defined and calculated between the planned and placed implant positions. The postoperative STL file, derived from the intra-oral scan, was geometrically aligned with the files exported from the planning, by automated image registration using maximization of mutual information (Dental SCAN, ver.6, Open Technologies srl, Brescia, Italy). The horizontal (lateral), vertical (depth), and angular deviation between virtual and placed implants were calculated along the long axis of each implants. An expert blinded mechanical engineer performed all the measurements (Figure 7).
Statistical analysis
Patient data was collected in a numbers spreadsheet (Version 3.6.1 for Mac OS X 10.11.4). A bio-statistician with expertise in dentistry analyzed the data using SPSS software for Mac OS X (version 22.0; SPSS Inc, Chicago, Illinois) for statistical analysis. Descriptive analysis was performed for numeric parameters using mean SD and median with confidence interval (95% CI). Complications between the two groups were compared using Fisher's exact probability test. The mean differences of the overall deviation in the clinical outcomes compared to the virtual plan, were compared between groups using the non- parametric Mann-Whitney U test. All statistical comparisons were conducted at the .05 level of significance.
Results
A total of 39 patients with 119 implants were evaluated. Sixteen patients with 48 implants were treated in the centre one and 23 patients with 71 implants in the centre two. No patients dropped out during the study period (mean follow-up 12.4 ± 7.1 months after implant placement [range 3-24 months]). Three implants failed at centre two. Implants were replaced after 3 months of healing period. One complication was experienced at centre one resulting in limited access in posterior areas during the placement of an implant in the right lower second molar position. In this case, a shorten drill (7 mm instead of 10 mm) was used to sign the entry point, then the implant was placed free-end. All the implants were inserted according to the manufacturer's instructions, with an insertion torque ranged between 35 and 45 Ncm. There were baseline imbalances between the two groups for the presence of more treated female at the centre one (68.8% vs 30.4%); more implants placed in the anterior region at the centre two (60.6% vs 16.7%); more implants placed in the maxilla at centre one (66.7% vs 46.5%); more implants placed thought open holes at centre one (31.3% vs none); and longer follow-up at centre two (17.3 vs 5.3 months). Patients and implant characteristics between groups were reported in Table 1.
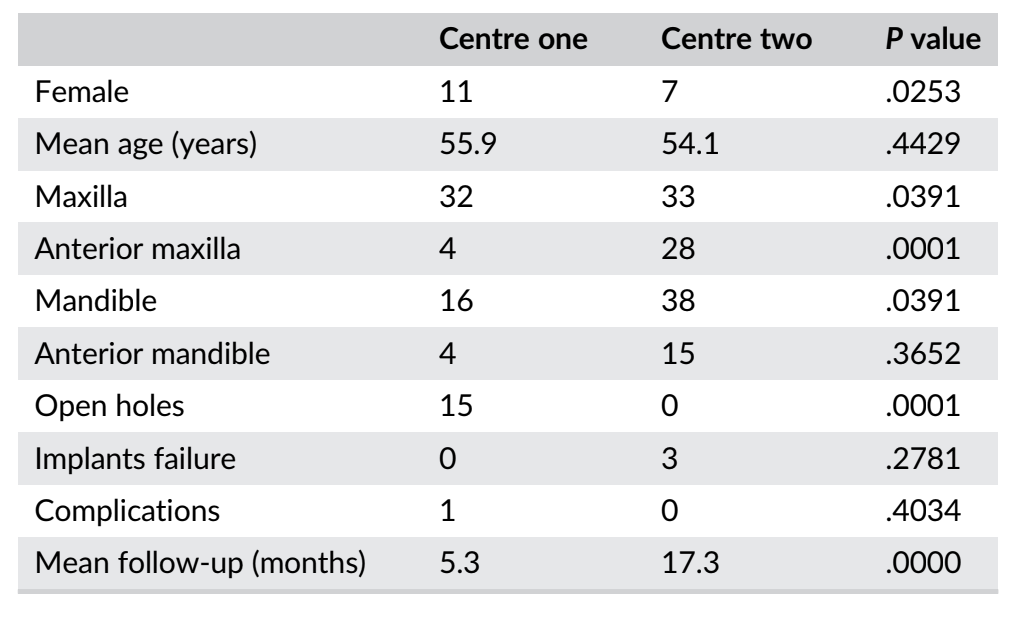
Overall, the analysis of the final accuracy revealed a total mean error of 0.53 ± 0.46 mm (range 0.05-3.38 mm; 95% CI 0.32-0.48 mm) in the horizontal plan (mesio-distal); 0.42 ± 0.37 mm (range 0.0-1.53 mm; 95% CI 0.26-0.40 mm) in the vertical plan (apico-coronal); and 1.43 ± 1.98° (range 0.03-11.8°; 95% CI 0.31-1.01°) in angle.
In the horizontal plan (mesio-distal), the mean error was 0.61 ± 0.49 mm (95% CI 0.36-0.64 mm) at centre one and 0.48 ± 0.44 mm (95% CI 0.27-0.47 mm) at centre two (P = 0.1508); in the vertical plan (apico-coronal), the mean error was 0.37 ± 0.28 mm (95% CI 0.23-0.39 mm) at centre one and 0.45 ± 0.42 mm (95% CI 0.23-0.43 mm) at centre two (P = .2108). The mean error in angle was 1.98 ± 2.38° (95% CI 0.13-1.47°) at centre one and 1.06 ± 1.56° (95% CI 0.13-1.856°) at centre two (P = .0221) (Table 2).
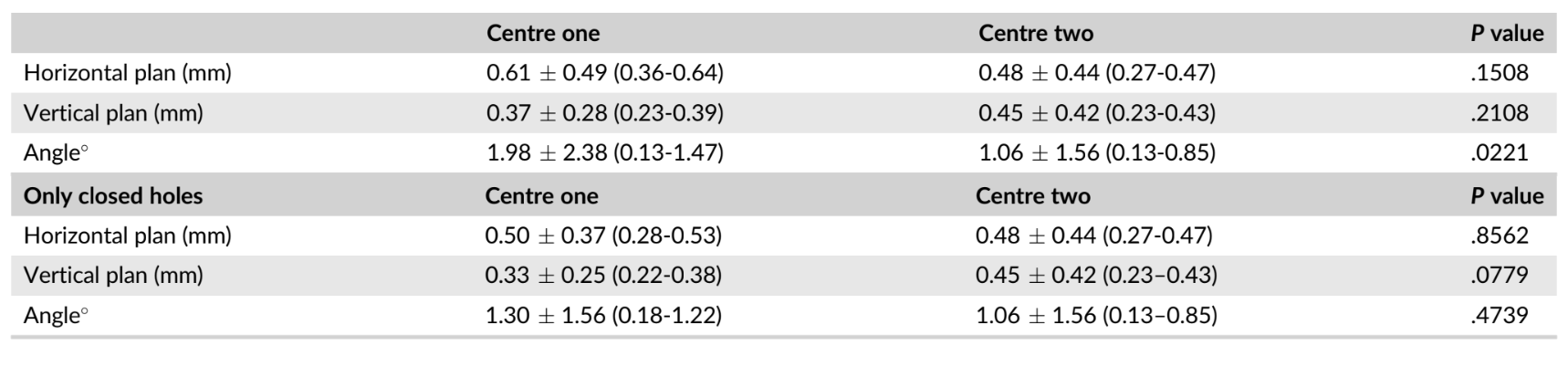
Excluding open holes, at centre one, the analysis of the final accuracy revealed a total mean error of 0.50 ± 0.37 mm (95% CI 0.28-0.53 mm) in the horizontal plan (mesio-distal); 0.33 ± 0.25 mm (95% CI 0.22-0.38 mm) in the vertical plan (apico-coronal); and 1.30 ± 1.56° (95% CI 0.18-1.22°) in angle. The differences between centers were not statistically significant (P > .05; Table 2).
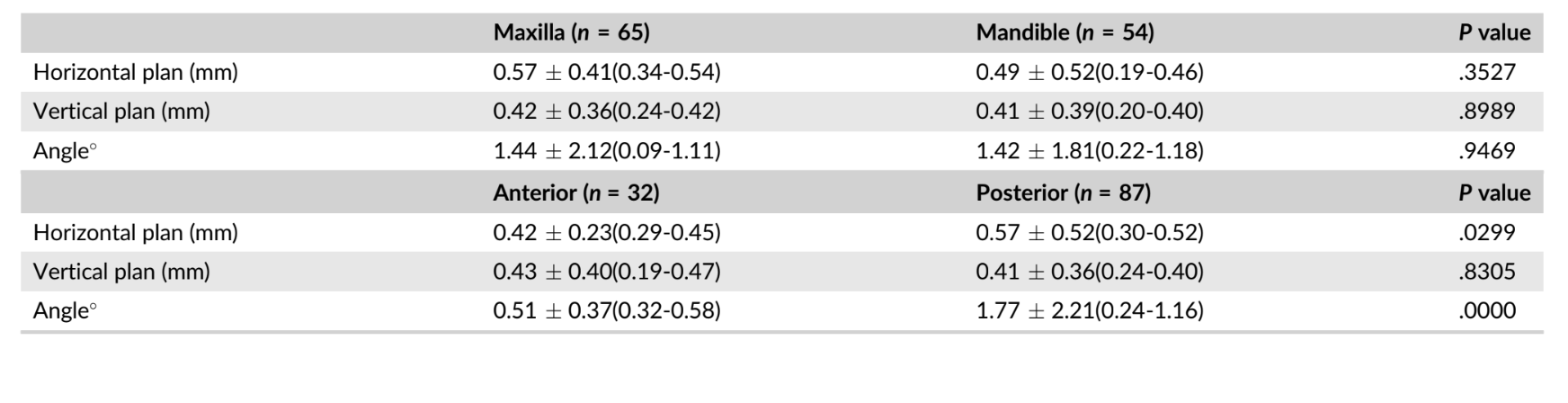
Subgroup comparison of implants' accuracy between maxilla and mandible relived no statistically significant differences between groups (Table 3). Otherwise, subgroup comparison of implants' accuracy between anterior and posterior implants relived statistically significant differences between groups with more accurate results for anterior implants in both horizontal plan and angle. Viceversa, no statistically significant differences between groups were reported for vertical plan accuracy. Data were reported in Table 3.
Discussion
This multicenters prospective study was conducted with the aim to evaluated the implant accuracy using a newly developed sleeve-designed template to place dental implants according to a computer-assisted template-based protocol.
To the best of our knowledge, at the time of writing this manuscript, there were no published randomized controlled trials evaluating the accuracy of the newly developed sleeve-designed templates. Looking at the gray literature, the same authors suggested that sleeve-designed templates with open sleeves may be used with caution in molar region only when the inter-arches space is reduced, because of less accuracy compared with closed sleeves.
Schnutenhaus et al., in a prospective study on the accuracy of sleeveless 3-dimensional drill guides, experienced a mean deviation of 0.52 mm (95% CI 0.37-0.67 mm) at the crestal position of the implant; 0.82 mm (95% CI 0.56-1.08 mm) at the apical tip of the implant; 0.35 mm (95% CI: 0.01-0.68 mm) in the vertical plan; and a mean angular deviation of 2.85° (95% CI 2.18-3.51°). Comparing this results with the data from the present research, similar values were found in
the horizontal and vertical plan. Nevertheless, half the value were reported for the angle accuracy.
In the present study, no statistically significant difference on implant accuracy was found between implants placed in the maxilla and in the mandible. On the contrary, statistically higher accuracy was experienced for anterior implants rather than posterior, on both horizontal plan and angle. A possible explanation for this results could be that in the posterior area, at centre one, sleeve-designed templates with open holes were used14. In fact, when considering only closed sleeve-designs template with closed holes, data on accuracy improved (Table 2).
Our results are in line with Naziri et al. who verified that the location of the implant, whether in the upper or lower jaw, did not significantly affect deviations and also implantation in a free-end dental arch has a statistically significant negative influence on the precision of implant insertion compared to implantation in an interdental gap.
In the present study, the maximum angle deviation (11.8°) was found in a free-hand saddles maxilla. In this cases, the implant mount driver can create a pressure touching the template that could produce a distortion, reducing the final implant accuracy. The most likely explanation for this is that the surgical guide is only partially tooth-supported in free-end dental arch implantation. According to Tallarico et al., the maximum acceptable value for angle discrepancy should range between 5.9 and 16.7° depending of the implant length and diameter. Nevertheless, the clinicians can choose between open or closed holes, limiting the use of the open holes only in case with limited access in the posterior areas.
In the present study, nine maxillary lateral incisors and 15 lower incisors were treated. Another benefit of the sleeve-designed template was the lower mesio-distal space required. In fact, metallic tubes presented a thickness of 0.5 mm that reduce its use in case of limited mesio-distal space, such as lower incisor and maxillary lateral incisors.
Both centers were able to achieve successful results. Despite the evident benefits related to higher accuracy with the sleeve-designed templates, there is still the need to clinically evaluate the long-term esthetic and functional advantages. High accuracy with sleeve-designed templates could be explained with a larger template/drill contact during the implant site development, reducing the wobbling of the drills. In fact, the sleeve-designed templates presented 5 mm high guidance, compared to 3.5 mm in the metallic sleeve. Furthermore, the implant mount drivers of the sleeve-designed templates (NoMount Driver and Fixture Driver, OneGuide Kit, Osstem) are designed without any stop. In case of an angle discrepancy, the inbuild stop of the implant mount driver (OsstemGuide Kit, Osstem) should touch the metallic sleeve on a side, not allowing for an accurate flat-to-flat matching.
The main limitation of the present study was that a priori sample size calculation was not performed, thus, the limited power of the analysis, because of a limited number of participants, could have hidden some differences between groups. This can only be solved by conducting more similar trials with larger sample sizes, calculated based on this preliminary result. Another limitation could be the base-line imbalances between the two groups that reflect the different population between Korea and Italy. Nevertheless, implant failure, complications and accuracy were similar between the two centers expect for better accuracy on angle at centre two. This difference could be explained with the use of open sleeve at centre one rather than to different population. Hence, taking into account both cohort of patients, the overall results can be generalized to different populations, even worldwide.
Conclusion
With the limitations of the present study, high accuracy was found in all the parameters measured. The results were thus in a range equal to or better than the mean precision found in numerous clinical trials described in the literature. Posterior implants were less accurate because of the use of sleeve-designed templates with open holes. Further randomized controlled trials are needed to confirm this result.
Marco Tallarico, Yong-Jin Kim, Fabio Cocchi, Matteo Martinolli, Silvio Mario Meloni
References
- Tallarico M, Esposito M, Xhanari E, Caneva M, Meloni SM. Computer-guided vs freehand placement of immediately loaded dental implants: 5-year post loading results of a randomised controlled trial. Eur J Oral Implantol. 2018;11:203-213.
- Tallarico M, Meloni SM. Retrospective analysis on survival rate, template-related complications, and prevalence of Peri-implantitis of 694 anodized implants placed using computer-guided surgery: results between 1 and 10 years of follow-up. Int J Oral Maxillofac Implants. 2017;32:1162-1171.
- Meloni SM, Tallarico M, Pisano M, Xhanari E, Canullo L. Immediate loading of fixed complete denture prosthesis supported by 4-8 implants placed using guided surgery: a 5-year prospective study on 66 patients with 356 implants. Clin Implant Dent Relat Res. 2017;19: 195-206.
- Tallarico M, Meloni SM, Canullo L, Caneva M, Polizzi G. Five-year results of a randomized controlled trial comparing patients rehabilitated with immediately loaded maxillary cross-arch fixed dental prosthesis supported by four or six implants placed using guided surgery. Clin Implant Dent Relat Res. 2016;18:965-972.
- Meloni SM, De Riu G, Pisano M, Tullio A. Full arch restoration with computer-assisted implant surgery and immediate loading in edentulous ridges with dental fresh extraction sockets. One year results of 10 consecutively treated patients: guided implant surgery and extraction sockets. J Maxillofac Oral Surg. 2013;12:321-325.
- Meloni SM, De Riu G, Pisano M, et al. Implant restoration of edentulous jaws with 3D software planning, guided surgery, immediate loading, and CAD-CAM full arch frameworks. Int J Dent. 2013;2013: 683423.
- Meloni SM, De Riu G, Pisano M, Cattina G, Tullio A. Implant treatment software planning and guided flapless surgery with immediate provisional prosthesis delivery in the fully edentulous maxilla. A retrospective analysis of 15 consecutively treated patients. Eur J Oral Implantol. 2010;3:245-251.
- Meloni SM, Tallarico M, De Riu G, et al. Guided implant surgery after free-flap reconstruction: four-year results from a prospective clinical trial. J Craniomaxillofac Surg. 2015;43:1348-1355.
- Mangano F, Gandolfi A, Luongo G, Logozzo S. Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health. 2017; 17:149.
- Tallarico M, Xhanari E, Cocchi F, Canullo L, Schipani F, Meloni SM. Accuracy of computer-assisted template- based implant placement using a conventional impression and scan model or digital impression: a preliminary report from a randomized controlled trial. J Oral Science Rehabilitation. 2017;3(3):08-16.
- The glossary of Prosthodontic terms: ninth edition. J Prosthet Dent. 2017;117(5S):e1-e105.
- Pozzi A, Tallarico M, Marchetti M, Scarfo B, Esposito M. Computer- guided versus free-hand placement of immediately loaded dental implants: 1-year post-loading results of a multicentre randomised con- trolled trial. Eur J Oral Implantol. 2014;7(3):229-242.
- Sommacal B, Savic M, Filippi A, Kühl S, Thieringer FM. Evaluation of two 3D printers for guided implant surgery. Int J Oral Maxillofac Implants. 2018;33(4):743-746.
- Tallarico M, Martinolli M, Abadzhiev M, Cocchi F, Kim YJ. A safe and predictable treatment option for experts and beginners. EDI Journal. 2018;14(3):52-57
- Schnutenhaus S, von Koenigsmarck V, Blender S, Ambrosius L, Luthardt RG, Rudolph H. Precision of sleeveless 3D drill guides for insertion of one-piece ceramic implants: a prospective clinical trial. Int J Comput Dent. 2018;21(2):97-105.
- Naziri E, Schramm A, Wilde F. Accuracy of computer-assisted implant placement with insertion templates. GMS Interdiscip Plast Reconstr Surg DGPW. 2016;5:Doc15.
