A Rare Case of Front Mandible Orthokeratinized Odontogenic Cyst – Surgical Management with Preventive Rigid Osteosynthesis
Purpose: Cysts and other intrabony lesions can grow asymptomatic until being diagnosed by occasionally done radiologic examination. Missing tooth and malposition of adjacent teeth should induce clinicians to perform X-Ray diagnostic.
Methods: A 37-year-old, male patient was admitted with a hopeless tooth 36, to be extracted and replaced with an implant. Clinical examination revealed also missing one of lower incisors and malposition of remaining lower incisors. Cone-beam computed tomography revealed horizontally impacted lower incisor surrounded by bone defect −15 × 20 × 8 mm with the bone thickness remaining only 3.5 mm in the narrowest area. The basis on strong masticatory muscles and low thickness of bone after surgical removal of tooth and lesion, prophylactic osteo- synthesis was planned. To explain the surgery to the patient model of the mandible was 3D printed.
Results: Two treatment plans were presented to the patient: 1. custom plate production according to the bone defect and the shape of remaining bone and 2. choosing a standard plate and adjusting it on the 3D printed model. Costs of the material were 10 times higher in a custom solution. Plan 2 was then accepted. 1.2 mm straight plate was prebend on the model and sterilized. Lesion and impacted tooth were removed in local anesthesia. Prepared plates were fixed.
Conclusions: In the presented case custom 3D printed osteosynthesis plate was about 10 times more expensive compared to the standard osteosynthesis plate used. 3D printing of bone model may be helpful for prebending chosen standard plate and planning the surgery.
Cysts and other intrabony lesions can grow asymptomatic until being diagnosed by occasionally done radiologic examination. Missing tooth and malposition of adjacent teeth should induce clinicians to perform X-Ray diagnostic. The Orthokeratinized Odontogenic Cyst (OOC) was first described as an orthokeratinzed variant of the Odontogenic Keratocyst by Wright in 1981 owing to its different histopathology and low risk to recur. OOC occurs predominantly in the mandible and males. These cysts are often asymptomatic and discovered as an incidental finding especially in the orthodontics’ radiographs. The OOC is mostly localized in lateral segments of the mandible and extremely rare in the front part of that bone. To the best knowledge of authors, this is the first case in the literature describing OOC in front mandible. Fractures caused by the underlying pathologic lesion in the mandible, are rare and don’t reach 2% of all fractures of the mandible. Pathological fractures usually result from regions of osteomyelitis, osteoradionecrosis, bisphosphonate-related osteonecrosis of the jaw, and idiopathic reasons, or are facilitated by cystic lesions, benign, malignant, and metastatic tumors. Pathological fractures of the mandible associated with benign cystic lesions are relatively rare, particularly the pathological fractures arising from radicular cysts. Nevertheless fracture may happen during tooth extraction. Especially impacted tooth combined with pathologic lesion may lead to iatrogenic fracture of the mandible. Most published cases are connected with fractures during or after impacted third molar extractions. In this case, the risk of the front segment of the mandible during impacted tooth extraction or as a delayed fracture was calculated as high. So that preventive rigid osteosynthesis was performed.
Clinical report
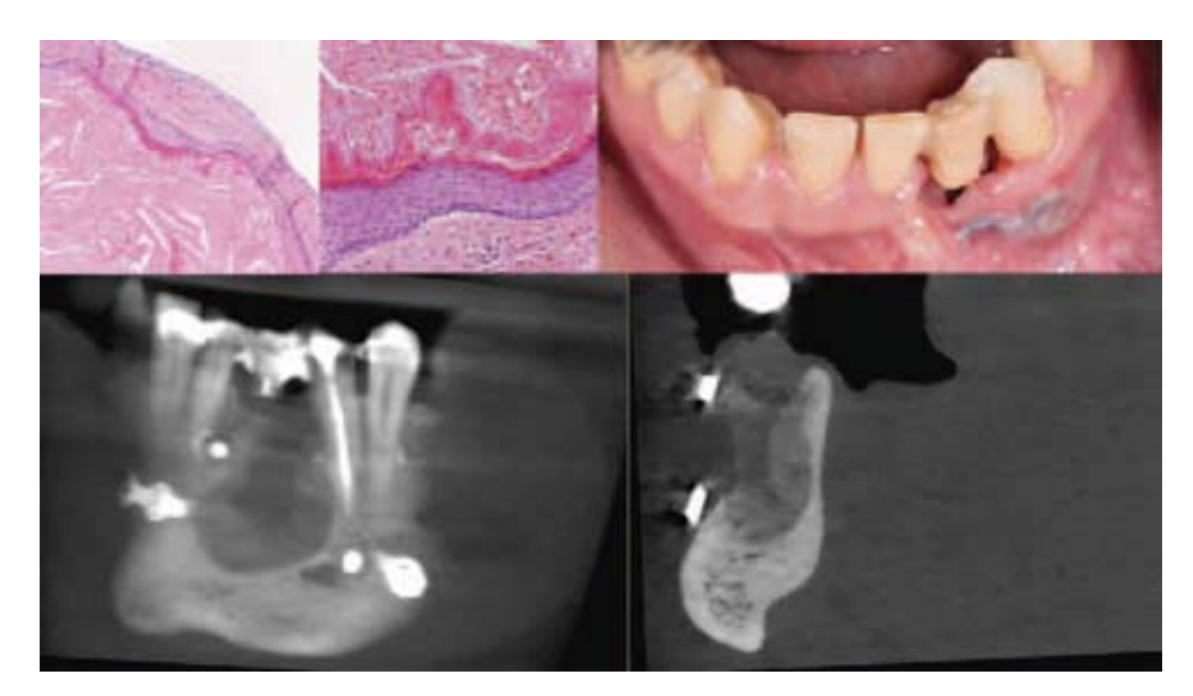
A 37-year-old, male patient was admitted to the clinic with hopeless tooth 36, to be extracted and replaced with an implant. Clinical examination revealed also missing one of lower incisors and malposition of remaining lower incisors (Fig. 1). Cone-beam computed tomography (CBCT) revealed horizontally impacted lower incisor surrounded by bone defect − 15 × 20 × 8 mm with the bone thickness remains only 3.5 mm in the narrowest area (Fig. 1). Basis on strong masticatory muscles, patient weight − 120 kg, and low thickness of remaining bone after surgical removal of tooth and lesion, preventive rigid osteosynthesis was planned. Osteosynthesis has been planned to prevent also possible iatrogenic fracture of the mandibula during removal of impacted incisor. To explain surgery to the patient, Digital Imaging and Comunication in Medicine visualization was exported as Stereolitography file and model of mandible (Fig. 1) was 3D manufactured with Digital Light Processing 3D printer. At the same time, the planning and designing of custom osteosynthesis plate (Fig. 1) was done by means of Customy 3D Planner (Smart Labs Sp. z o.o., Chorzów, Poland) an online platform for surgery planning. Two treatment plans were presented to the patient: 1. custom plate production accordingly to the bone defect and the shape of remaining bone and 2. choosing a standard plate and adjusting it on the 3D printed model. Costs of the material were 9 times higher in custom solution. Second plan was then accepted mainly because of financial reasons. 1.5 mm thickness straight plate was prebend on the prepared model (Fig. 1) and sterilized. Two hours before surgery patient took 2 g Amoxicillin and 100 mm mg Nimesulid. 30 ml of venous blood was collected and centrifugated to obtain Platelet rich factors (PRF) plugs and membranes. The surgery was done under local anesthesia with 4% Articaine þ Noradrenaline (1/100,000). The tooth 31 was extracted after sulcular incision done by 15C blade. Trapezoid fullthickness flap was cut with blade no 15C from mesial section of tooth 42 to distal section of tooth 33. Flap was elevated and facial aspect of frontal mandible was exposed reaching also exposure of the left mental nerve. With the Luer forceps bone border of the lesion was removed and the lesion was partially removed. Prebend osteosynthesis plate was checked for fitting, and fixed with two 2.0 mm screws on each side. Prepared plate was fixed with 2.0 system screws, as it was planned on the model. After plate fixation impacted tooth was extracted with sectioning into 3 pieces. The rest of the lesion was removed with the tooth. Collected material was stored with 3% Formalin solution and sent for histopathologic examination. Additional buccal bone plate had to be removed to create an access to extract the tooth. That led to lack of the buccal bone plate at the level of the lesion in whole vertical dimension. To create better support for soft tissue during healing period another osteosynthesis plate was adjusted during surgery and fixed coronally to the main plate with two 2.0 mm screws, one each side. PRF clots ware placed into the bone defect and PRF membranes were placed over the fixed plates. Flap was sutured with 4.0 and 6.0 nylon sutures. Crown of extracted tooth 31 was cut, pulp was removed, and chamber was filled with flowable material from. Fiberglass and flowable composite material were used to fixed crown of 31 to adjacent teeth as a temporary restoration. Postoperative CBCT was done (Fig. 1). Antibiotic therapy was continued for 5 days after the surgery: 1 g per 8 hours. Healing was uneventful. Sutures were removed in 2 sessions, part after 1 and the rest after 2 weeks of healing. Soft diet was suggested for 4 months after the surgery. After 5 months, patient presented partial exposure of the upper plate through the soft tissue. Another CBCT was done to evaluate the bone healing pattern and decision of removal of upper plate was done. In local Anastesia with 4% Articain þ Noradrenaline (1/100,000) small incision of mucosa was done over the plate, screws were removed and plate was removed. Site was rinsed with the 0.9% NaCl solution and the mucosa was sutured with 6.0 nylon sutures more apically than the incision line to achieve better conditions of the vestibulum. Sutures were removed after 7 days.

Results
Postoperative CBCT revealed proper adaptation of both osteo- synthesis plates to the bone surface. Histopathologic examination of the lesion revealed OOC (Fig. 2). After 5 months of observation, no complication happens in terms of bone fracture and temporary tooth reconstruction (Fig. 2). Control CBCT done 5 months postoperative revealed sights of bone healing in postoperative site (Fig. 2). Nevertheless for implant treatment in this site additional bone reconstruction surgery will be required.
Discussion
Men with complete dentition are able to generate high biting forces that are transmitted to the mandible during mastication, and consequently, the risk of fracture is higher than in women. Nevertheless, most mandibular fracture cases described in the literature was found in men in the fifth decade of life, presented patient was in third but was muscular and very strong. Completely impacted teeth especially horizontal with associated lesions have a greater incidence of mandibular fracture because the volume of the bone surrounding the tooth and lesion is already low or needs to be removed during the operation which weakens the mandible. Bodner et al analyzed 189 cases and found 86% cases of mandibular fractures develop post- operatively and usually occurred between the first and third week after the operation. Possible reasons for that may be excessive biting force or minor trauma to a weakened bone. However, other authors claimed that mastication does not affect late mandibular fracture soft diet should be recommended up to 4 weeks postoperatively. If the fracture happens rigid fixation is today a method of choice in treatment. Prophylactic rigid fixation of the mandible should be also considered in cases when there is an increased risk of iatrogenic fracture to prevent additional surgery and increased morbidity. Finite Element Analysis research by Murakami et al illustrated the theoretical efficacy of plate application for the decrease of stress on the mandible after surgical removal of a cyst including a third molar based on a computer simulation. In the presented patient decision was done to perform rigid fixation as a preventive procedure during tooth and lesion removal in the frontal part of the mandible. Initially, a custom 3D printed osteosynthesis plate was considered to be used. Such a plate will strengthen the remaining bone as well as support the soft tissue over the defect. Unfortunately, the custom solution was 9 times more expensive comparing to the standard osteosynthesis plate. Using 3D printing of bone model was though an affordable and helpful aid to choose and prebend the standard plate and for the planning of the surgery. In this case, single fixation plate was planned for bone fixation. Nevertheless, an additional plate was used to support soft tissue. Using additional osteosynthesis plates such as in the fence technique described by Merli et al in 2015 helped to support soft tissue for up to 5 months during the initial healing period. Unfortunately without additional grafting materials, in this case, the supporting plate had to be removed due to dehiscence of the soft tissue. Within the most critical period after surgery, no fracture occurred in the presented case. Within 5 months of follow-up, no signs of OOC recurrence were detected.
Conclusions
Within the limitation of this clinical report following conclusion can be drawn. The Educational message to the clinicians and surgeons can be summarized as follows:
Accurate clinical examination should be performed during each dental appointment and additional diagnostics should be referred if signs of teeth malposition have been detected. Digital technologies, such as CBCT and surgery planning software, can help to carefully plan the surgery but as for now the custom CAD/CAM osteosynthesis plates are significantly much more expensive than the standard available materials. The 3D printed bone model is cheap, affordable, and helpful in surgery analyzing and adjustment of the standard osteosynthesis plates. To evaluate if preventive rigid osteosynthesis is effective in prevalence of postextractive bone fractures more studies on bigger groups are needed.
Łukasz Zadrozny, Pawel Rogus, Michał Pyzlak, Marco Tallarico and Marco Cicciu
References
- Bilodeau EA, Collins BM. Odontogenic cysts and neoplasms. Surg Pathol Clin 2016;10:177–222
- Wright JM. The odontogenic keratocyst: orthokeratinized variant. Oral Surg Oral Med Oral Pathol 1981;51:609–618
- Wright BA, Fanibunda K. Odontogenic keratocyst dentigerous cyst type? J Can Dent Assoc 1981;47:313–314
- Mahdavi N, Taghavi N. Orthokeratinized odontogenic cyst of the maxilla: report of a case and review of the literature. Turk Patoloji Derg 2017;33:81–85
- Macdonald-Jankowski DS. Orthokeratinized odontogenic cyst: a systematic review. Dentomaxillofac Radiol 2010;39:455–467
- Sarvaiya B, Vadera H, Sharma V, et al. Orthokeratinized odontogenic cyst of the mandible: a rare case report with a systematic review. J Int Soc Prev Community Dent 2014;4:71–76
- de Souza AS, Colombo LT, Hadad H, et al. Bone regeneration around implants with modified surface by acid conditioning with the fluoride ions deposition. J Osseointegration 2020;12:222–228
- Xiao X, Dai JW, Li Z, et al. Pathological fracture of the mandible caused by radicular cyst: a case report and literature review. Medicine (Baltimore) 2018;97:13529
- Bodner L, Brennan PA, McLeod NM. Characteristics of iatrogenic mandibular fractures associated with tooth removal: review and analysis of 189 cases. Br J Oral Maxillofac Surg 2011;49:567–572
- Miyaura K, Matsuka Y, Morita M, et al. Comparison of biting forces in different age and sex groups: a study of biting efficiency with mobile and non-mobile teeth. J Oral Rehabil 1999;26:223–227
- Al-Belasy FA, Tozoglu S, Ertas U. Mastication and late mandibular fracture after surgery of impacted third molars associated with no gross pathology. J Oral Maxillofac Surg 2009;67:856–861
- Van Sickels JE, Richardson DA. Stability of orthognathic surgery: a review of rigid fixation. Br J Oral Maxillofac Surg 1996;34:279–285
- Hartman MJ, Sibley DM. Prophylactic internal fixation to avoid mandible fracture with third molar removal: use of computer- assisted surgery to improve clinical outcomes. J Oral Maxillofac Surg 2020;78:2147–2152
- Baron J, Hazubski S, Otte A. 3D multi-material printing of an anthropomorphic, personalized replacement hand for use in neuroprosthetics using 3D scanning and computer-aided design: first proof-of-technical-concept study. Prosthesis 2020;2:362–370
- Murakami K, Yamamoto K, Tsuyuki M, et al. Theoretical efficacy of preventive measures for pathologic fracture after surgical removal of mandibular lesions based on a three-dimensional finite element analysis. J Oral Maxillofac Surg 2014;72:833e1–833e18
- Krakowczyk Ł, Piotrowska-Seweryn A, Szymczyk C, et al. Virtual surgical planning and cone beam computed tomography in reconstruction of head and neck tumors - pilot study. Otolaryngol Pol 2020;75:28–33
- Farré-Guasch E, Wolff J, Helder MN, et al. Application of additive manufacturing in oral and maxillofacial surgery. J Oral Maxillofac Surg 2015;73:2408–2418
- Barazanchi A, Li KC, Al-Amleh B, et al. Mechanical properties of laser- sintered 3D-printed cobalt chromium and soft-milled cobalt chromium. Prosthesis 2020;2:313–320
- Lavorgna L, Cervino G, Fiorillo L, et al. Reliability of a virtual prosthodontic project realized through a 2D and 3D photographic acquisition: an experimental study on the accuracy of different digital systems. Int J Environ Res Public Health 2019;16
- Merli M, Mariotti G, Moscatelli M, et al. Fence technique for localized three-dimensional bone augmentation: a technical description and case reports. Int J Periodontics Restorative Dent 2015;35:57–64
- Merli M, Nieri M, Mariotti G, et al. The fence technique: autogenous bone graft versus 50% deproteinized bovine bone matrix /50% autogenous bone graft-a clinical double-blind randomized controlled trial. Clin Oral Implants Res 2020;31:1223–1231
