Fully optimized digital workflow for the rehabilitation of edentulous patients
Machine translation
Original article is written in IT language (link to read it) .
Abstract
The digital revolution is changing the world, and dentistry is no exception. Through the development of new equipment and workflows, the diagnosis and treatment of patients are becoming simpler and more efficient. However, a completely digital approach to the care of edentulous patients can be challenging and time-consuming because edentulous sites are often flat, smooth, and poorly defined. This clinical case aims to present, step by step, the completely digital workflow for the rehabilitation of a 67-year-old edentulous patient wearing a complete denture. The treatment includes Cone Beam computed tomography following a modified double scan protocol that involves: the complete digitization of the existing complete denture, the placement of the implant through guided surgery following computerized analysis, the optical impression taken with a modified model, the production of a CAD/CAM titanium bar, and a friction-retained superstructure in chrome-cobalt. The completely digital workflow has proven effective in restoring function and aesthetics in an elderly, male, edentulous patient rehabilitated with a completely implant-supported overdenture using four implants and a CAD/CAM titanium bar with a low-profile spherical attachment system.
Introduction
Guided implant placement is a key factor for successful implant therapy. Consequently, computer-assisted implant placement is increasingly being used due to higher planning and transfer accuracy from the virtual plan to the surgical site compared to freehand placement. However, the accuracy of computer-assisted implant placement depends on several factors, from data acquisition to the surgical act. Originally, guided surgical protocols were performed with a double scan protocol. Today, continuous technological advancement in both computerized development and the dental manufacturing process offers additional tools for treatment planning, surgical placement, and prosthetic rehabilitation in an interdisciplinary team approach.
A correct correspondence between the master model and the oral cavity reflects on the final accuracy of an implant-supported complete denture. Hence, an accurate impression of the implants is a fundamental prerequisite for the fabrication of an accurate master model and therefore a correct prosthesis. Several impression techniques are available to create a master model for the production of an implant-supported complete denture. In a recent randomized controlled study, the authors concluded that the clinical outcome of gypsum impressions for edentulous patients is comparable to a splinted VPS impression. Today, there is no doubt about the potential of recent intraoral optical impression systems available on the market, regarding diagnosis and treatment planning, as well as for the fabrication of fixed prostheses. Their accuracy overlaps with that of traditional impressions. Furthermore, intraoral scanners have also been successfully used in the creation of partial and complete dentures. However, scanning the edentulous area with intraoral scanners can be challenging and time-consuming because the sites are smooth and lack characterizations. Consequently, the realization of complete restorations of an edentulous arch remains a challenge, even when the data is acquired directly with an intraoral scanner. The purpose of this study is to present a completely digital protocol in a model-free approach to rehabilitate an edentulous patient in the maxilla with an implant overdenture. A new technique is described to develop an optimal intraoral optical impression for the treatment of an edentulous patient.
Clinical case
A 67-year-old partially edentulous man, wearing a removable complete denture in the upper jaw and a removable complete partial denture in the lower jaw, was referred to a private center located in Rome for possible rehabilitation with implants. The patient had been edentulous in the upper jaw for years. However, he never felt comfortable with his removable complete denture and expressed interest in a fixed implant-supported prosthesis.
First appointment
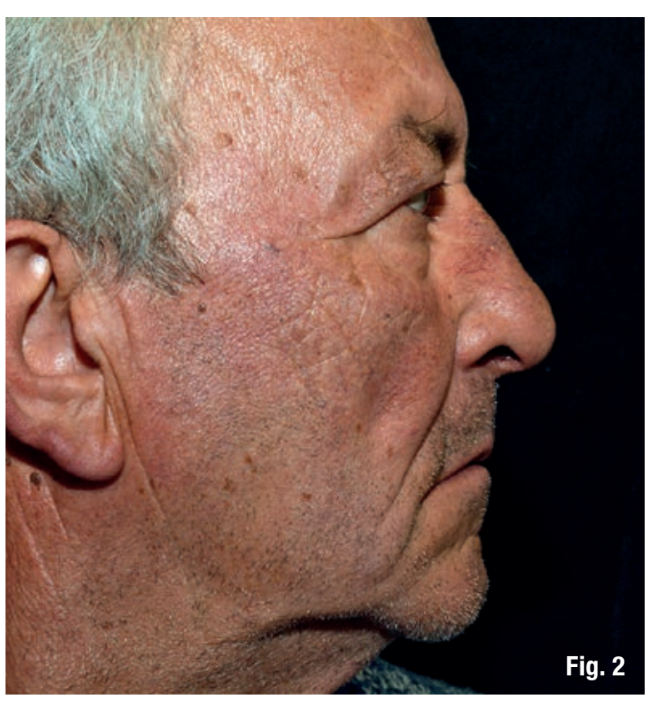
Once the patient's medical history was taken, photographs and preparatory radiographs were taken along with a periodontal screening and study models for preliminary evaluation. During the clinical examination, the existing removable complete denture was also evaluated, as well as the functional and aesthetic aspects, with particular attention to the shape of the prosthesis, the vertical dimension of occlusion, facial support, and lip position. The extraoral examination of the patient without the prosthesis revealed a wide nasolabial angle and insufficient lip support (Fig. 1, 2). All possible treatment options were discussed and evaluated with the patient; fixed implant-supported prostheses were excluded due to the need for significant lip support. The choice then fell on the implant-supported overdenture, considered the only possible therapeutic option.

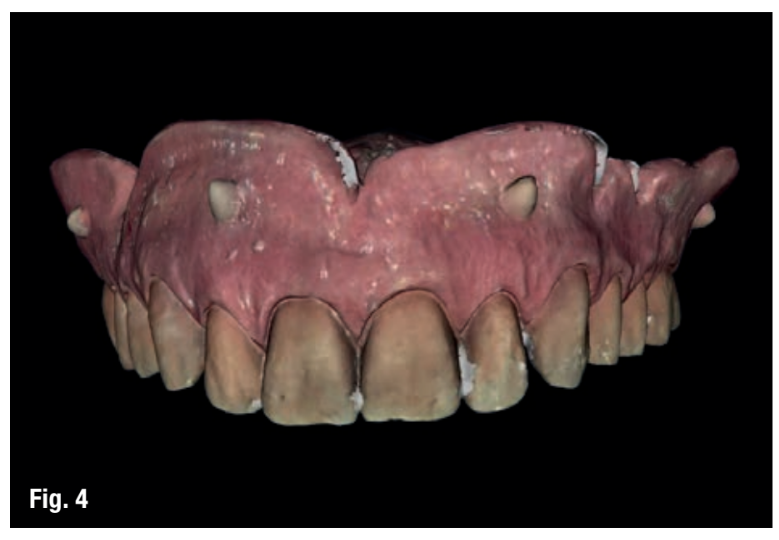
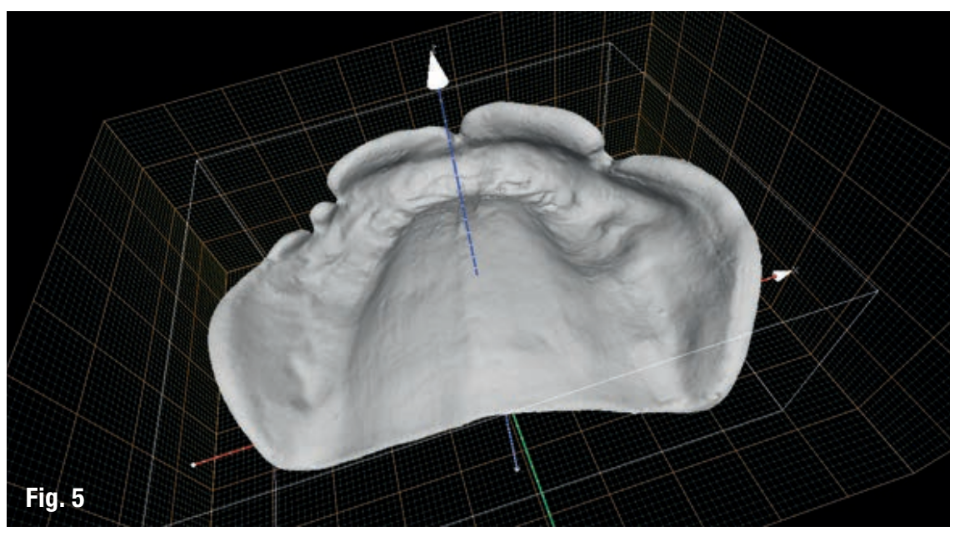
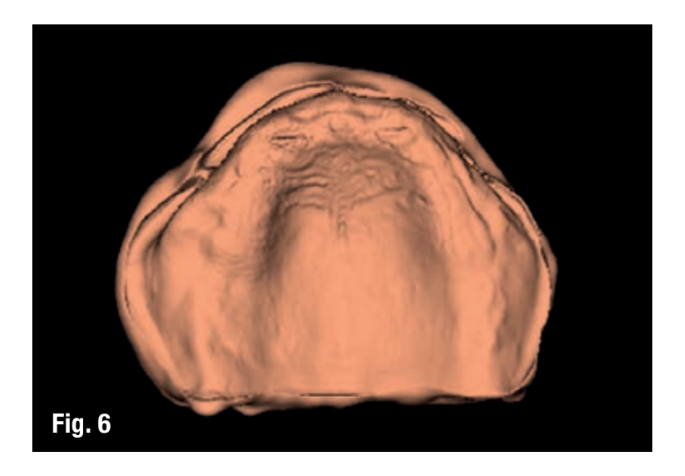
The planned workflow at the prosthetic level was initiated with a modified double scan protocol, applying 4-6 drops of flowable composite to the removable complete denture, in place of spherical gutta-percha markers (Figs. 3-6). The first scan is a cone beam computed tomography (CBCT) (Cranex 3Dx, Soredex, Tuusula, Finland) of the patient with the removable complete dental prosthesis. A wax occlusion was used to separate the dental arches (Fig. 3). The second scan involves the removable complete dental prosthesis performed using an optical intraoral scanner (Carestream Dental LLC, Atlanta, GA, USA) to allow the fusion of DICOM (Digital Imaging and Communications in Medicine) data with the STL (Stereo Lithography interface format) file (Figs. 4-5). Using reverse engineering techniques, a virtual model was created (Fig. 6).

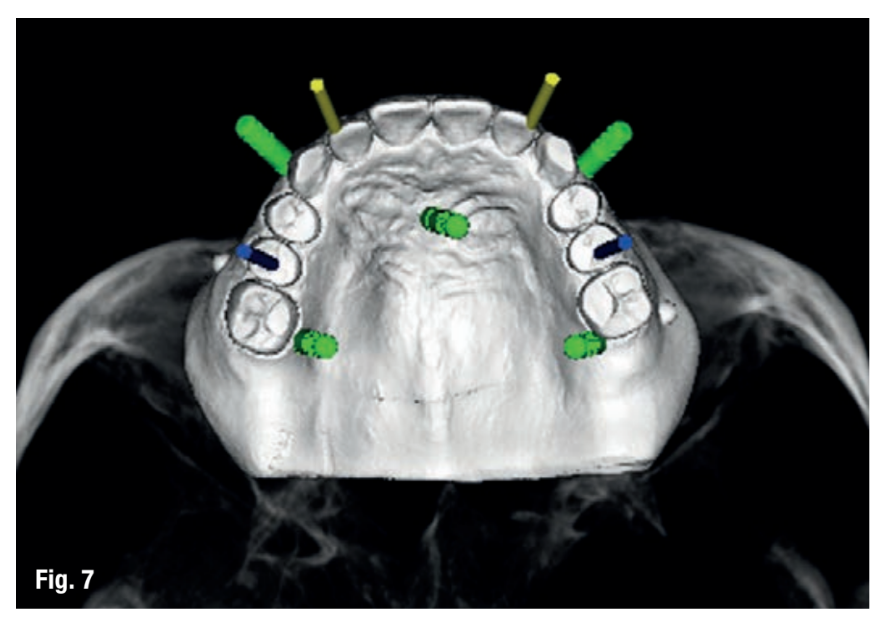
The STL and DICOM data were imported into a 3D software planning program (3Diagnosys version 4.2, 3DIEMME s.r.l., Cantù, Italy). The reconstructed surface extrapolated from the DICOM data and the surface of the prosthesis generated by the scanning process are overlaid using the repositioning tools of the software (3Diagnosys version 4.2, 3DIEMME s.r.l.). At this point, the positioning of 4 implants with a diameter of 3.5 and 4.5 mm and a length of 13 mm (Osstem TSIII, Osstem, Seoul, South Korea) was designed, taking into account the quality/quantity of bone, the thickness of the soft tissues, the anatomical reference points, as well as the type, volume, and shape of the final restoration (New Ancorvis s.r.l., Bargellino, Italy) (Fig. 7). After a careful functional and aesthetic evaluation and a final verification, the prosthetic plan was approved and a stereolithographic surgical model was manufactured using a new rapid prototyping technology (New Ancorvis s.r.l.) (Fig. 8).

Second clinical appointment
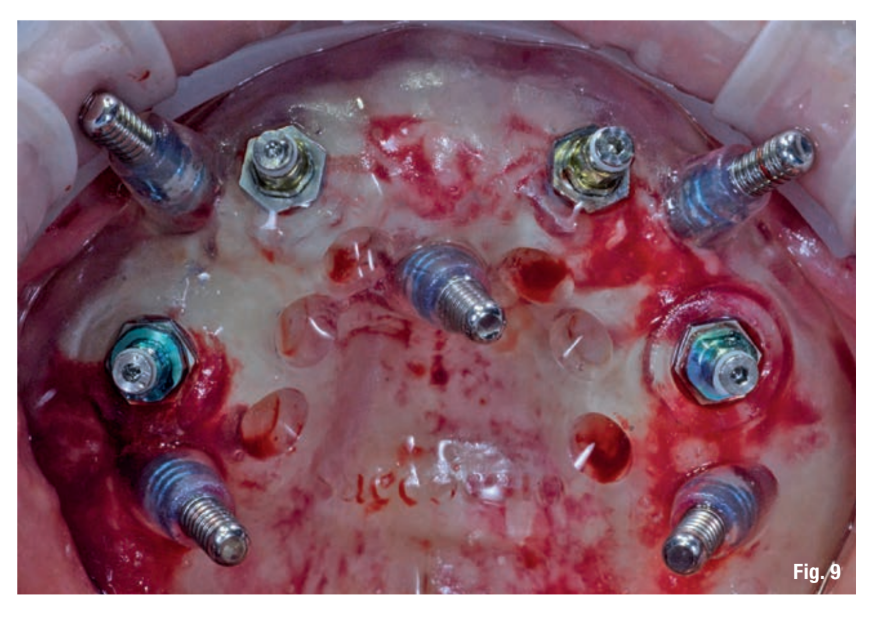
One hour before the implant surgery, the patient underwent a professional dental cleaning and a one-minute antiseptic prophylaxis with a 0.2% chlorhexidine solution (Curasept, Curaden Healthcare, Saronno, Italy) and an antibiotic (2 g of amoxicillin or 600 mg of clindamycin in case of penicillin allergy). The correct fit of the surgical templates was carefully tested directly in the patient's mouth (fit Checker, GC - Tokyo, Japan). The patient was treated under local anesthesia using articaine with adrenaline 1:100000 administered 20 minutes before the surgical procedure. The surgical guide was stabilized using a silicone surgical index, derived from the virtual plan and five pre-installed anchoring pins (New Ancorvis s.r.l.). The planned implants (Osstem TSIII, Osstem) were placed with flapless surgery using dedicated drills (OsstemGuide Kit, Osstem) (Fig. 9). All implants were inserted with a minimum insertion torque of 35 Ncm according to previously published protocols. The multi-unit abutments were immediately screwed onto the implants (New Ancorvis s.r.l.) right after the implant placement and were never removed again. A digital impression (CS 3600 intraoral scanner, Carestream Dental LLC) of the abutments was taken, using dedicated scan abutments (type AQ, New Ancorvis s.r.l.) (Figg. 10a, b).
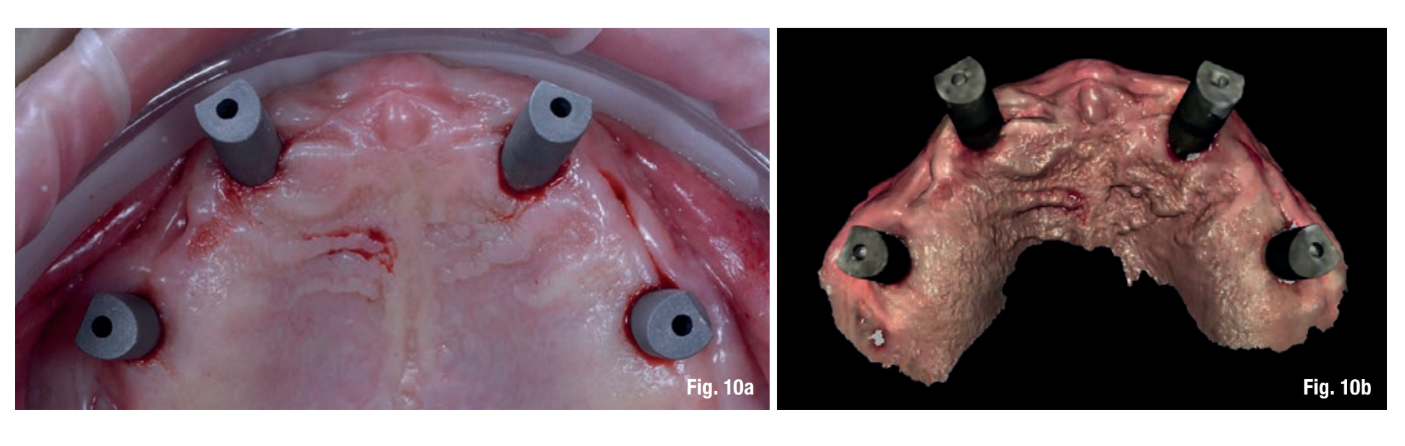
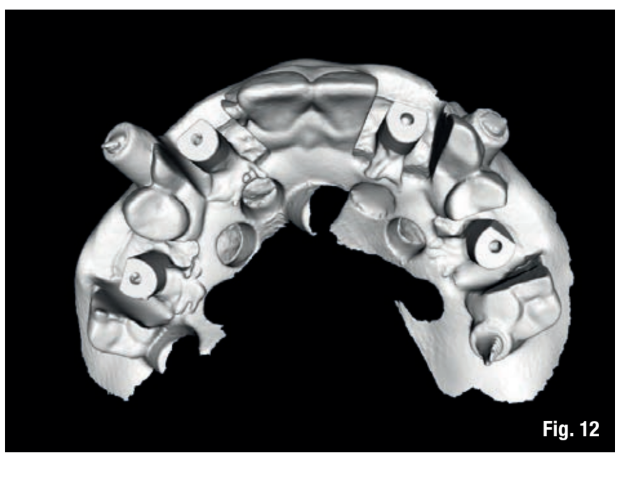
To improve the accuracy of the digital impression in a completely edentulous patient, a second digital impression was taken using an opaque dedicated model, created from virtual planning, stabilized in the patient's mouth using the same pins from guided surgery. This model was manufactured while maintaining the design of the teeth, but allowing the attachment of scanning supports (type AQ, New Ancorvis s.r.l.) (Fig. 11). In this way, it was possible to overlay the new STL file onto the previous planning (Fig. 12). Finally, the multi-unit abutments were covered with healing abutments, and the existing removable prosthesis was relined in the office with self-curing resin (Hydro-Cast, Sultan Healthcare, York, PA, USA), so as not to stress the healing abutments. After the implant placement, the patient was instructed, also with a paper copy, about the use of medications, oral hygiene, and diet.

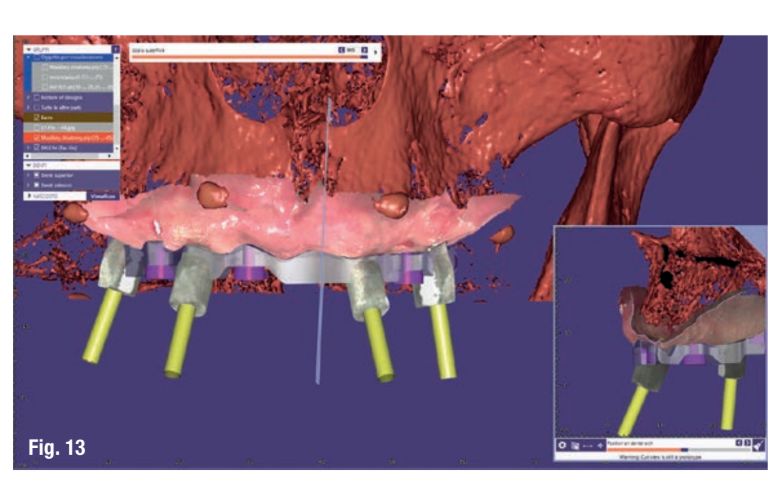
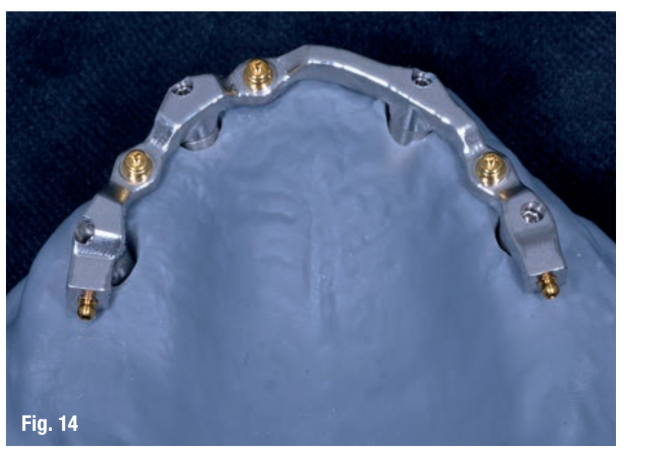
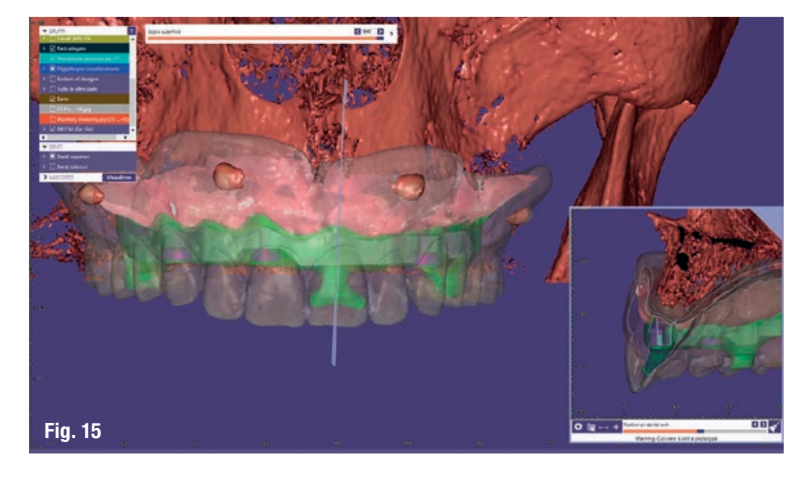
A CAD/CAM (Computer-Aided Design/Computer-Assisted Manufacturing) anatomical titanium bar was designed by an expert dental technician and a CAD designer (M. A.) based on the position of the implant, as well as the shape and volume of the existing prosthesis (Exocad DentalCAD Engine Build 6136, Exocad GmbH, Darmstadt, Germany) (Fig. 13). Three low-profile threaded attachments (OT Equator, Rhein 83, Bologna, Italy) and two micro threaded spheres (Rhein 83, Bologna, Italy) were placed on the bar (Fig. 14). Subsequently, a cobalt-chromium alloy framework was directly designed (Fig. 15) in accordance with the mounting of teeth (exocad Partial Framework CAD V0.x, Exocad GmbH). The obtained files were transmitted to the production center (New Ancorvis s.r.l.), where a titanium bar was milled from a solid and homogeneous block of medical titanium alloy (Ti6Al4V), while the counter-bar was fused using laser melting technique (Fig. 16).

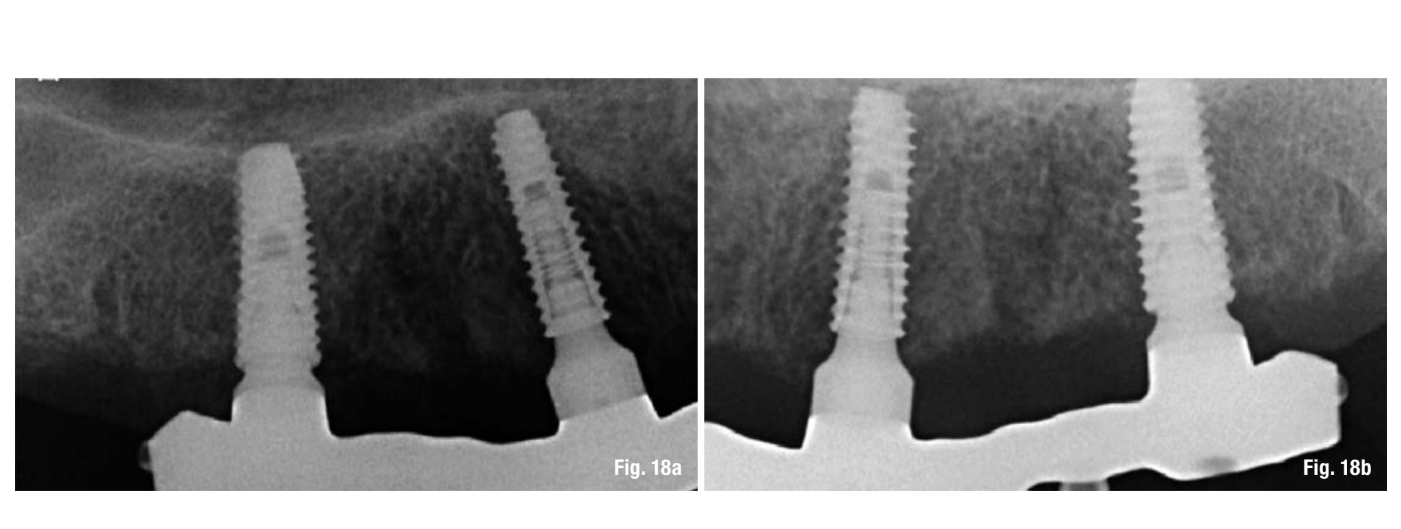
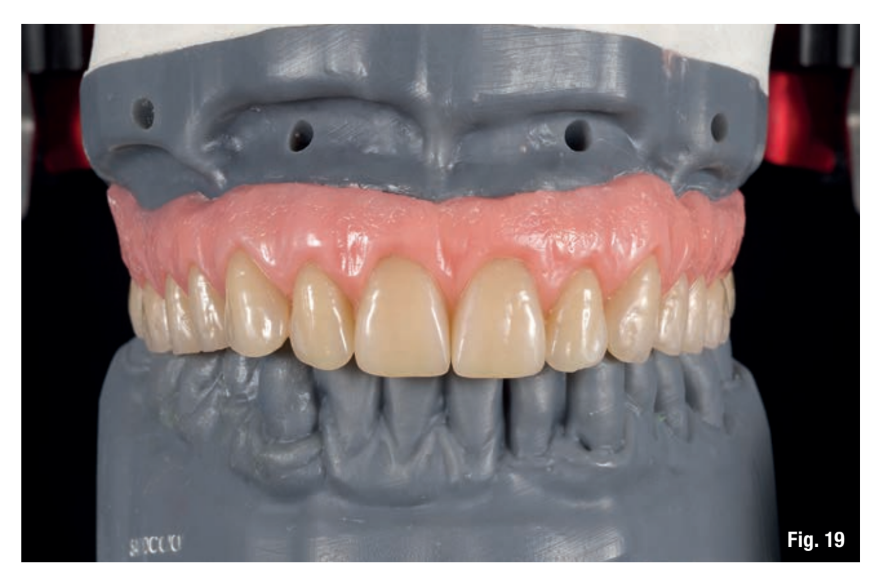
Third clinical appointment
The coupling of the bar on the implants and subsequently the coupling of the superstructure on the bar has been clinically and radiographically tested in the patient's mouth according to established criteria (Figs. 17-18b). Subsequently, the centric relation of the mandible was recorded, and the master models, manufactured using rapid prototyping techniques, with specially designed implant analogs, were mounted in a fully adjustable articulator (KaVo Protar evo 7, KaVo Dental, Biberach, Germany) (Fig. 19). The digital analysis of condylar movement was performed using the Digma ARCUS device (KaVo Dental) to ascertain and document all the settings necessary for programming the articulator (e.g., condylar inclination, Bennett angle, immediate side shift, shift angle). Finally, the overdenture was completed using a silicone template derived from the newly designed dental prosthesis with the positioning of prefabricated teeth and sealing all contours well to minimize the infiltration of food, saliva, and air leaks.

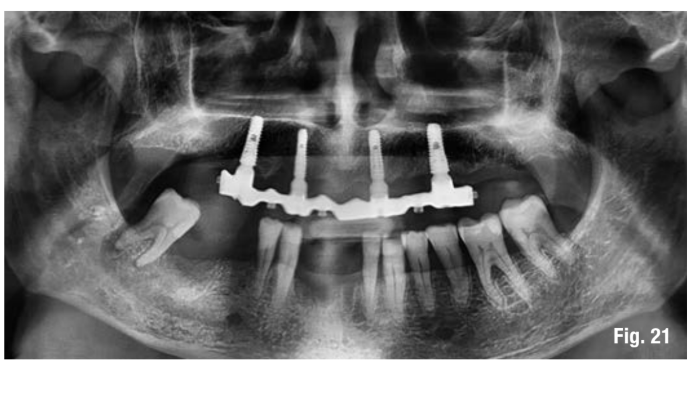
Fourth clinical appointment
The titanium bar was screwed onto the abutments according to the manufacturer's instructions, and the overdenture was delivered 6 weeks after the first visit (Figs. 20, 21). The patient was included in a follow-up program in which proper oral hygiene maintenance was checked, and radiographs were taken following the delivery of the prosthesis. The occlusion was also checked at each appointment.

Discussion
This clinical case describes a new technique for the fabrication of a complete dental prosthesis supported by implants, using an intraoral digital scanner to record the positions of the implant and the morphology of the soft tissues.
Existing technologies such as CBCT, in combination with virtual three-dimensional reconstruction of the implant positioning and the fabrication of surgical models with stereolithography, are used both in treatment planning and in the surgical positioning of the implant. However, errors of 1.5 mm and 1 mm have been reported in the horizontal and vertical planes for the CBCT technique. Additionally, CBCT images are also subject to significant contamination from scatter signals that create large image artifacts, limiting the applications of CBCT. To overcome such inconveniences and for better accuracy, the removable dental prosthesis was digitized using an intraoral scanner.
Intraoral scanners are rapidly spreading within dental clinics for the acquisition of digital impressions of teeth and implants, also improving workflow with other already existing digital technologies. Optical impressions are more comfortable for the patient, optimizing time and improving precision and operational ease for the dentist. A recent systematic review of the literature and a meta-analysis conducted by Chochlidakis et al. concludes that the intraoral scanner can be safely used to take impressions of single and multiple abutments in patients with dentition. However, there is still a lack of evidence regarding the possibility of using intraoral scanners to take impressions for extensive restorations or in the case of completely edentulous patients. In a recent in vitro study by Imburgia et al., the CS 3600® performed best in terms of matching and precision in partially and completely edentulous models with six implants. Mangano et al., in another in vitro study, found no differences in terms of matching and precision between partially and completely edentulous models. However, this result may be due to the fact that the three-dimensional surface models of the partially edentulous patient were not sectioned and cut, and the related calculations were therefore performed on the entire arch.
In this study, in addition to the acquisition of digital data on the morphology of soft tissues and implant positioning, a second optical impression was taken with a specially designed opaque model in combination with the same scan abutments (New Ancorvis s.r.l.) to acquire accurate digital data of the implant in completely edentulous patients, as if it were a partially edentulous patient. This procedure can avoid a necessary appointment to verify and then confirm the positions of the implant analogs.
The technique presented uses CAD/CAM (Computer-Aided Design/Computer-Aided Manufacturing) technology with a subtractive manufacturing process for the creation of a milled bar (primary structure) and an additive process for the creation of a friction-supported superstructure (secondary structure). This digital restoration pathway can reduce patient discomfort and decrease the work associated with the fabrication of implant-supported removable prostheses. The overdenture fully supported by four implants and a CAD/CAM titanium bar with a low-profile attachment system can be considered an effective and predictable option for patients with atrophic mandibles classified as Class VI according to Cawood and Howell. Over time, minimal marginal remodeling and limited complications can be expected along with good periodontal health and patient satisfaction.
Conclusions
This clinical case confirms the high precision of implant placement with computer-planned guided surgery and supports the use of intraoral scanners to obtain an optimal oral impression even in edentulous patients. Further studies with larger sample sizes are necessary to confirm the results emerging from this work.
Authors: Marco Tallarico, Danilo Schiappa, Franco Schipani, Fabio Cocchi, Marco Annucci, Erta Xhanari
References
- Tallarico M, Meloni SM, Canullo L, Xhanari E, Polizzi G. Guided surgery for single-implant placement: a critical review. J Oral Science Rehabilitation. 2016 Dec; 2(4):8–14.
- Polizzi G, Cantoni T, Pasini E, Tallarico M. Immediate loading of variable-thread expanding tapered-body implants placed into maxillary post-extraction or healed sites using a guided surgery approach: An up-to-five year retrospective analysis. J Oral Science Rehabilitation. 2016 Sep; 2(3):50–60.
- Tallarico M, Meloni SM, Canullo L, Caneva M, Polizzi G. Five-Year Results of a Randomized Controlled Trial Comparing Patients Rehabilitated with Immediately Loaded Maxillary Cross-Arch Fixed Dental Prosthesis Supported by Four or Six Implants Placed Using Guided Surgery. Clin Implant Dent Relat Res. 2016 Oct;18(5):965-972.
- Pozzi A, Tallarico M, Marchetti M, Scarfo B, Esposito M. Computer-guided versus free-hand placement of immediately loaded dental implants: 1-year post-loading results of a multicentre randomised controlled trial. Eur J Oral Implantol. 2014 Autumn; 7(3):229-42.
- Vermeulen J. The Accuracy of Implant Placement by Experienced Surgeons: Guided vs Freehand Approach in a Simulated Plastic Model. Int J Oral Maxillofac Implants. 2017 Mar/Apr;32(3):617–624.
- Van Steenberghe D., Glauser R., Blomback U., Andersson M., Schutyser F., Pettersson A., Wendelhag I. Computed tomographic scan-derived customized surgical template and fixed prosthesis for flapless surgery and immediate loading of implants in fully edentulous maxillae: a prospective multicentre study. Clin Implant Dent Relat Res. 2005; 7 Suppl 1:S111-20.
- Jemt T. & Hjalmarsson L. (2012) In vitro measurements of precision of fit of implant-supported frameworks: a comparison between “virtual” and “physical” assessments of fit using two different techniques of measurements. Clin Implant Dent Relat Res. 2012 May; 14 Suppl 1:e175-82.
- Pozzi A., Tallarico M., Mangani F., Barlattani A. Different implant impression techniques for edentulous patients treated with CAD/CAM complete-arch prostheses: a randomised controlled trial reporting data at 3 year postloading. Eur J Oral Implantol. 2013 Winter; 6(4):325-40.
- Papaspyridakos, P., Chen C.J., Gallucci G.O., Doukoudakis A., WeberH.P. & Chronopoulos V. (2014) Accuracy of implant impressions for partially and completely edentulous patients: a systematic review. Int J Oral Maxillofac Implants. 2014 Jul-Aug; 29(4):836-45.
- Amin S., Weber H.-P., Finkelman M., Rafie El K., Kudara Y., Papaspyridakos P. Digital vs. conventional full-arch implant impressions: a comparative study. Clin Oral Implants Res. 2016 Dec 31.
- Kattadiyil M.T., Mursic Z., AlRumaih H., Goodacre C.J. Intraoral scanning of hard and soft tissues for partial removable dental prosthesis fabrication. J Prosthet Dent. 2014 Sep; 112(3):444-8.
- Wu J., Li Y., Zhang Y. Use of intraoral scanning and 3-dimensional printing in the fabrication of a removable partial denture for a patient with limited mouth opening. J Am Dent Assoc. 2017 May; 148 (5):338-341.
- Fang J.-H., An X., Jeong S.-M., Choi B.-H. Development of complete dentures based on digital intraoral impressions-Case report. J Prosthodont Res. 2017 Jun 15. pii: S1883-1958(17)30049-X.
- Tallarico M., Meloni S.M. Open-cohort prospective study on early implant failure and physiological marginal remodeling expected using sandblasted and acid-etched bone level implants featuring an 11° Morse taper connection within one year after loading. J Oral Science Rehabilitation. 2017 Mar; 3(1):68–79.
- Tallarico M., Xhanari E., Kadiu B., Scrascia R. Implant rehabilitation of extremely atrophic mandibles (Cawood and Howell Class VI) with a fixed-removable solution supported by four implants: one-year results from a preliminary prospective case series study. J Oral Science Rehabilitation. 2017 Jun; 3(1):32–40.
- Abduo J., Bennani V., Waddell N., Lyons K., Swain M. Assessing the fit of implant fixed prostheses: a critical review. Int J Oral Maxillofac Implants. 2010 May-Jun; 25(3):506-15.
- Eisenmann E., Mokabberi A., Walter M.H., Freesmeyer W.B. Improving the fit of implant-supported superstructures using the spark erosion technique. Int J Oral Maxillofac Implants. 2004 Nov-Dec; 19(6):810-8.
- Jabero M., Sarment D.P. Advanced surgical guidance technology: a review. Implant Dent. 2006 Jun; 15(2):135-42.
- Loubele M., Bogaerts R., Van Dijck E., Pauwels R., Vanheusden S., Suetens P., et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol. 2009 Sep; 71(3):461-8.
- Niu T., Zhu L. Overview of X-ray scatter in Cone-beam computed tomography and its correction methods. Current Medical Imaging Reviews. 2010; 6 (2):82–89.
- Mario Imburgia, Silvia Logozzo, Uli Hauschild, Giovanni Veronesi, Carlo Mangano, and Francesco Guido Mangano. Accuracy of four intraoral scanners in oral implantology: a comparative in vitro study. BMC Oral Health. 2017 Jun; 17: 92.
- Mangano F.G., Veronesi G., Hauschild U., Mijiritsky E., Mangano C. Trueness and Precision of Four Intraoral Scanners in Oral Implantology: A Comparative in Vitro Study. PLoS One. 2016 Sep 29; 11 (9):e0163107.
- Chochlidakis K.M., Papaspyridakos P., Geminiani A., Chen C.J., Feng I.J., Ercoli C. Digital versus conventional impressions for fixed prosthodontics: A systematic review and meta-analysis. J Prosthet Dent. 2016 Aug; 116(2):184-190.e12.
- Wismeijer D., Mans R., van Genuchten M., Reijers H.A. Patients’ preferences when comparing analogue implant impressions using a polyether impression material versus digital impressions (Intraoral Scan) of dental implants. Clin Oral Implants Res. 2014 Oct; 25 (10):1113-8.
- Joda T., Lenherr P., Dedem P., Kovaltschuk I., Bragger U., Zitzmann N.U. Time efficiency, difficulty, and operator’s preference comparing digital and conventional implant impressions: a randomized controlled trial. Clin Oral Implants Res. 2016 Sep 5. doi:10.1111/clr.1298.
- Tsirogiannis P., Reissmann D.R., Heydecke G. Evaluation of the marginal fit of single-unit, complete-coverage ceramic restorations fabricated after digital and conventional impressions: A systematic review and meta-analysis. J Prosthet Dent. 2016 Sep; 116 (3):328-335.e2.
- Almeidae Silva J.S., Erdelt K., Edelhoff D., Araújo E., Stimmelmayr M., Vieira L.C., Güth J.F. Marginal and internal fit of four-unit zirconia fixed dental prostheses based on digital and conventional impression techniques. Clin Oral Investig. 2014; 18 (2):515-23.
- Ender A., Zimmermann M., Attin T., Mehl A. In vivo precision of conventional and digital methods for obtaining quadrant dental impressions. Clin Oral Investig. 2016 Sep; 20 (7):1495-504.
- Lin W.S., Chou J.C., Metz M.J., Harris B.T., Morton D. Use of intraoral digital scanning for a CAD/CAM-fabricated milled bar and superstructure framework for an implant-supported, removable complete dental prosthesis. J Prosthet Dent. 2015 Jun; 113 (6):509-15.
