An in-vitro study on accuracy of modular templates used to fully guide implants in combination with bone reduction for complete arch restorations: Experts versus students
Objectives: This in-vitro study evaluates the accuracy of modular surgical templates used to fully guide implants in combination with bone reduction, performed by expert and students, for complete arch restorations.
Methods: All the procedures were performed by dental students of the final year and an expert clinician, on twelve edentulous mandible models. A virtual implant planning, simulating a complete arch restoration on six implants were performed. Three different surgical guides were designed and printed to allow conventional fully guided implant placement (group 1); fully guided implant placement with modular guides (group 2); and fully guided implant placement after bone reduction, with similar, modular guides (group 3). After implant placement, optical scans of the study models were taken. Surface deviation and accuracy were evaluated and compared between groups and subgroups.
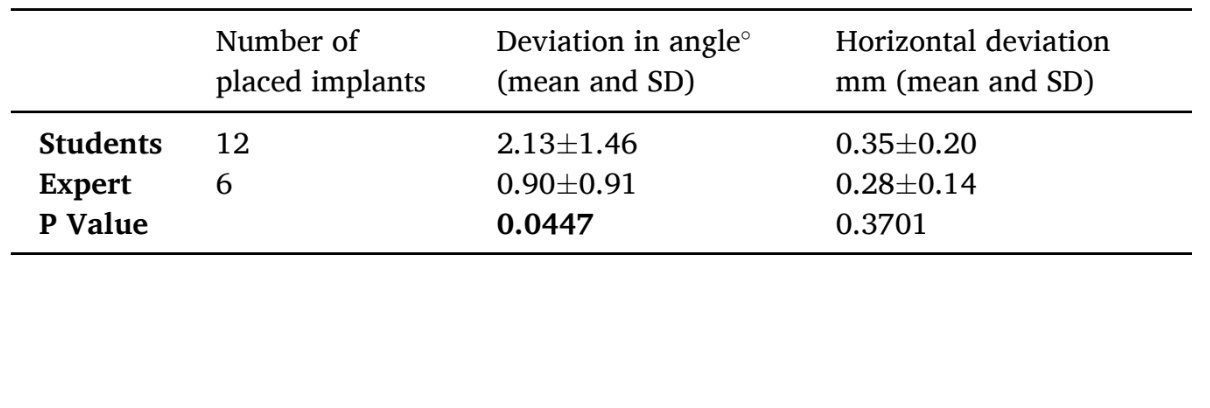
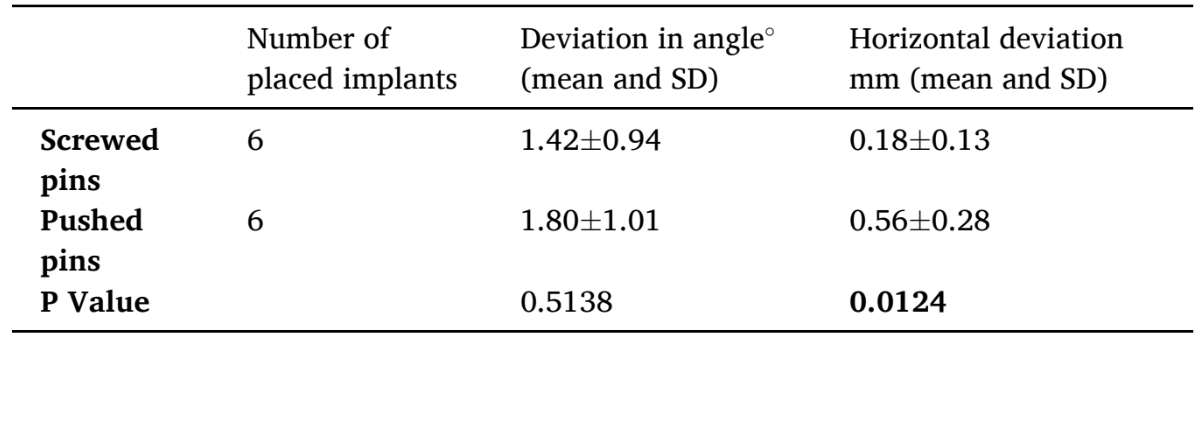
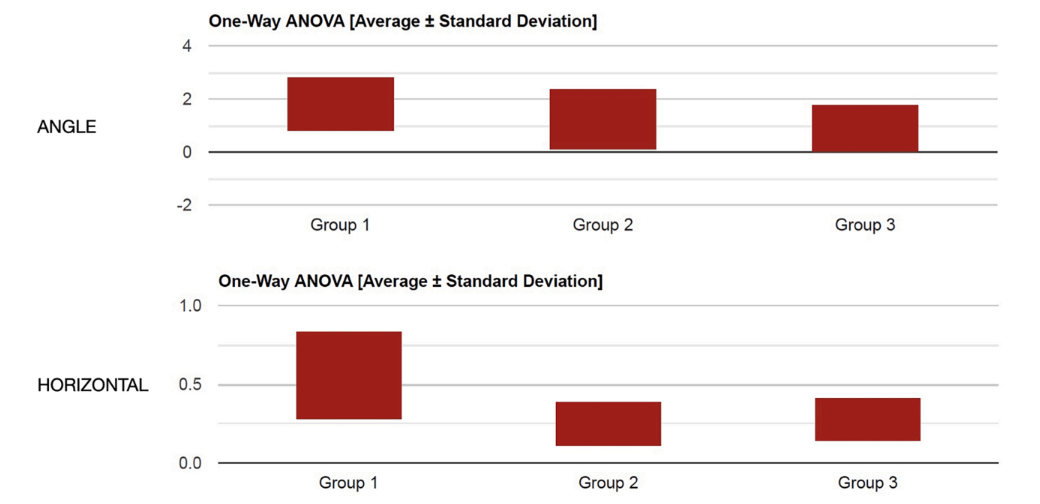
Results: A total of 12 surgical templates were used. Of these, Two templates in each group were used by two different students, while, the other six templates were used by an expert clinician as follows: one template with screwed anchor pins and one with pushed anchor pins in each group. A total of 72 implants were placed. Statistically significant difference was found between different template designs, when the implants were placed by an expert clinician. No statistically significant difference was found between expert and students, except the deviation in an angle value (students 2.13±1.46° versus expert 0.90±0.9°; P Value=0.0447) in the group 3. A statistically significant difference was found in favor of screwed anchor pins, in the group 1, in horizontal deviation (screwed pins 0.18±0.13 mm versus pushed pins 0.56±0.28 mm; P Value=0.0124; Table 5). No statistically significant difference was found between different template designs when the fully guided implants were placed by students, in both angle and horizontally (P=0.2787 and P=0.6601, respectively). A statistically significant difference was found between groups when the implants were placed by an expert clinician, with better value using screwed anchor pins, in the horizontal plane (P= 0.0293) but not in angle (P= 0.3380).
Conclusions: Modular templates provide a similar level of accuracy to conventional, one-piece guides. Screwed pins should be used to fix the base portion of the modular guides. Further clinical studies are needed to confirm these preliminary results.
Clinical Significance: Modular surgical guides provide comparable accuracy to conventional, single-piece guides, however they offer more possibilities, helping in bone reduction and immediate loading procedures. Screwed anchor pins used to fix the base portion of the modular guides provide better final results than pushed pins.
Introduction
Digital planned prosthetically driven implant placement become a predictable method for implant placement and immediate loading. Following an accurate work-flow, the accuracy of fully guided implants is expected to be closely matched to the proposed virtual plan. This allows for a high surgical accuracy and minimize surgical time, as well as, chairside adjustments of an interim prosthesis. The accuracy of a surgical template is evaluated measuring the three dimensional (3D) deviation of the placed implants compared to the virtual planned positions. The final accuracy of the entire process can be influenced by several factors, including, but not limited to clinical conditions, used software, type and precision of the template fabrication, also related to the guide design, and 3D printing technologies/materials.
In the last years, particularly in the complete arch restorations, the trend of placing implants has shifted from delayed implants in healed bone, to immediately, post-extractive implantations. Bone reduction and implant placement can be accomplished in the same surgical procedure, minimizing trauma and the need for two separate interventions. However, in patients with high smile line in the maxilla, or in case of irregular or thin bone crest, bone reduction is recommended in order to reduce biological and technical related complications of the implant-supported prostheses.
For more than 10 years, several manuscripts have been published proposing fully digital workflows for the treatment of failing dentition, using double or different types of multi-piece surgical templates. The so called multi-piece (or stackable, or modular guide), showed promising clinical results when used by expert clinicians. Modular surgical templates may improve the confidence in case of bone reduction, post-extractive implants, and immediate loading. However, the level of evidence is low and inconsistent, and there is still lack of generalizable data on which is the best design of such multi-piece surgical templates. Then, there is also inconsistency in the nomenclature used in the available literature. The term "modular" is used along this paper and refers to template which consists in a few parts providing different features (modules).
The aim of this in-vitro, comparative study, is to evaluate the accuracy of modular surgical templates used to fully guide implants in combination with bone reduction, performed by expert clinician and students. The present research was written according to the CRIS (Checklist for Reporting In-vitro Studies) guidelines.
Materials and methods
This study was designed as comparative, in-vitro research. Two dental students of the final year (FP and ADM) and one expert clinician with over 15 years of experience in guided surgery (MT) performed all the procedures. Twelve identically, complete edentulous mandible models with gingiva, dedicated for implantology exercises, with a dense and thick porous cortical bone and internal trabecular bone representing a D2 consistency (Dentalstore & Edizioni Lucisano SRL, Milan, Italy), were used for all the experiments. A cone beam computer tomography scan (Cranex 3Dx, Soredex, Tuusula, Finland) was taken (90 KV, 5.0 mA, FOV 6 × 8, resolution 0.2 mm) and the DICOM files were matched with the STL files derived from the optical scan of the same model (i700, Medit Corp., Yeongdeungpo-gu, Seoul, South Korea).
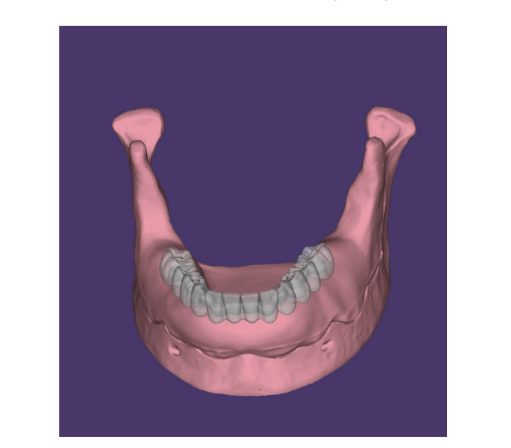
A virtual wax-up was performed to prosthetically plan the virtual implants (Exoplan 3.1 Rijeka prototype, Exocad GmbH, Darmstadt, Germany, Fig. 1). After that, six Osstem TSIII implants (Osstem Implants, Seoul, South Korea), of 4 mm diameter and 10 mm of length were virtually planned using a medical certified software (RealGUIDE 5.1 3DIEMME, Cantù, Italy) (Figs. 1 and 2). Implants were planned in lateral incisors, first premolars, and first molars position, about four millimeters below the bone crest in order to allow a bone crest reduction. Implants were placed fairly perpendicular to the occlusal plane, with a discrepancy of 6° (lateral incisors), 4.5° (premolars), and 0° (molars). In addition, three anchor pins were planned in the buccal position to fix and stabilize the surgical guide.
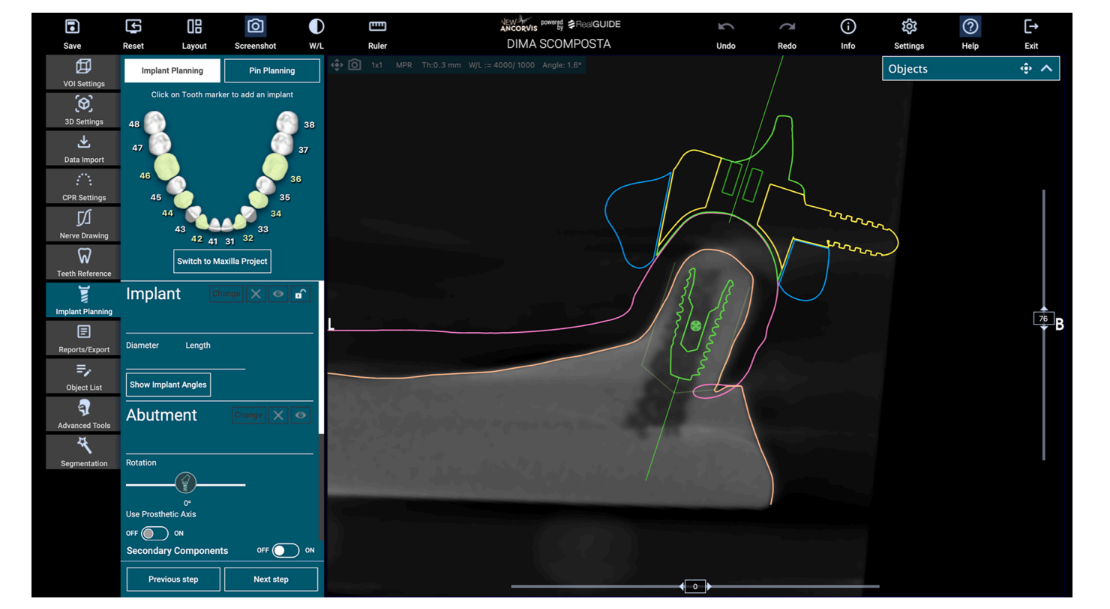
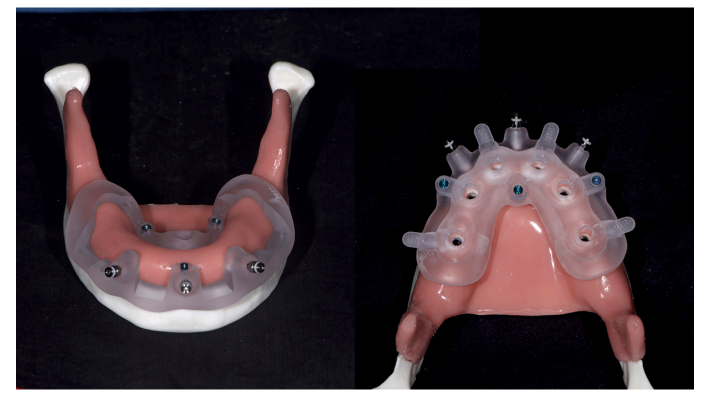
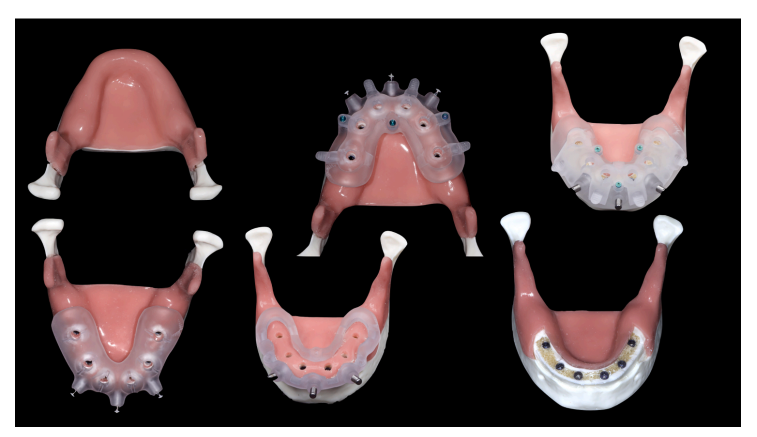
After virtual implant planning was completed and finally approved by a second expert clinician (LZ), the surgical guides were prepared accordingly to the protocol of the present research with three different designs as follows (groups 1 to 3). Single piece template was used in the group 1 and multi-piece surgical templates in groups 2 and 3 (modular guides). Particularly, in the group 1 (or control group), a conventional one-piece surgical template. In the group 2 (or modular guides group without bone reduction), a modular surgical template was. Lastly, a similar but not identical modular guide was designed to be used in the group 3, in combination with pre-planned, 4-mm vertical bone reduction (modular guides and bone reduction group). The base portion of all the modular guides includes the sleeves for the anchor pins and the slots for other modules: the implant module that includes the sleeves (printed) for the implant sites preparation and to fully guide the implants; and the index module, used to fix and stabilize the base portion in the proper position, before anchor pins fixation. However, the index part was not used for this in-vitro test due to the absence of teeth and the antagonist arch. Base and implant module were connected using three metallic mini-screws (New Ancorvis SRL, Bologna, Italy) (Fig. 3).
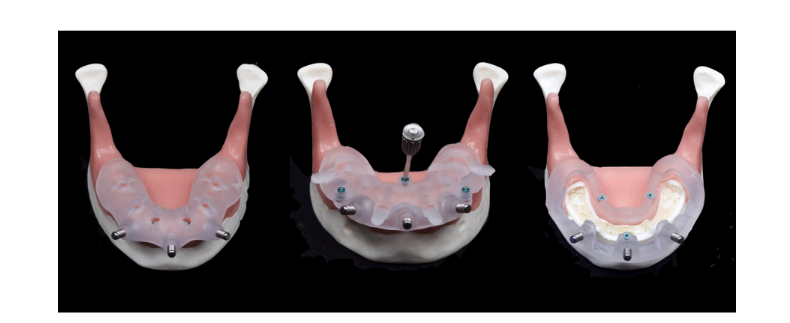
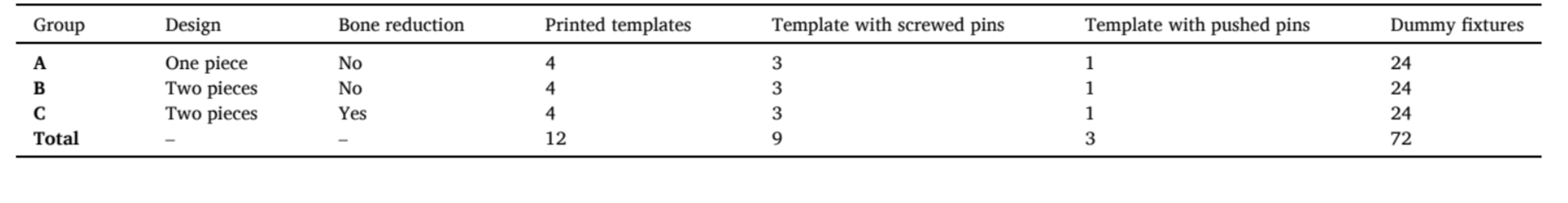
In each group, four identical templates were used. Two templates were used by two different students (one each), while, the other two templates were used by an expert clinician: one template with screwed anchor pins and one with pushed anchor pins. All the surgical templates were designed to fully guide six implants and being stabilized with three anchor pins. According to the used surgical kit (OneGuide Kit, Osstem Implants, Seoul, South Korea) no metallic sleeves were used and templates were fully 3D printed. All the surgical templates were printed in a professional milling center (New Ancorvis SRL, Bologna, Italy) using a DMP Dental 100 printer and a certified resin material (VisiJet M2R-CL 3D Systems Inc., Rock Hill, South Carolina, USA). In each group, three out of four templates were designed to allow the placement of screwed anchor pins, while, the last template was designed to allow the placement of pushed anchor pins. A total of 72 dummy implants were fully guided and placed, 24 dummies per group. A summary of the used templates is presented in Table 1. All the implants were placed according to the manufacturers’ instructions. The drilling protocol was the same for all the specimens, except for additional use of a mucotome in the groups 1 and 2. Before starting the research, the students were trained by participating in a 3-days theoretical/practical course (on models) on guided surgery.
- In the group 1, the conventional, one-piece surgical template was fixed using three screwed anchor pins. Then, fully guided, flapless implants placement, was performed according to the manufacturer-suggested drilling protocol, with an insertion torque ranging from 30 to 40 Ncm.
- In the group 2 (Fig. 4), the base portion of the surgical template was fixed using three screwed anchor pins. After that, the implant module was connected using three metallic mini screws (New Ancorvis SRL, Bologna, Italy). Finally, six implants were placed flapless and fully guided, as previously described.
- In the group 3 (Fig. 5), a flap was designed before template stabilization. The gingiva was partially removed from the model. After that, the base of the modular surgical template was fixed using three screwed anchor pins. Bone reduction was performed chairside, using a dedicated bone surgery ultrasonic tip with 9 mm cutting depth (BS1 s, for Piezotome Solo Ultrasonic Bone Surgery, ACTEON Germany GmbH, Düsseldorf, Germany), under saline irrigation. The base portion of the modular surgical template was designed to guide the ultrasonic tip during the initial bone reduction. After that, bone reduction was finished free-hand. Finally, the implant module was connected using three metallic mini screws and the implants were fully guided as previously described.

After implants placement (Fig. 6), in all the groups, digital scan abutments (Osstem Implant, Seoul, South Korea) were connected to the implants and an intraoral optical scans were taken (Medit i700, Medit corp., Seoul, South Korea, Fig. 7). The scanner was calibrated according to the manufacturer guidelines before each procedure.

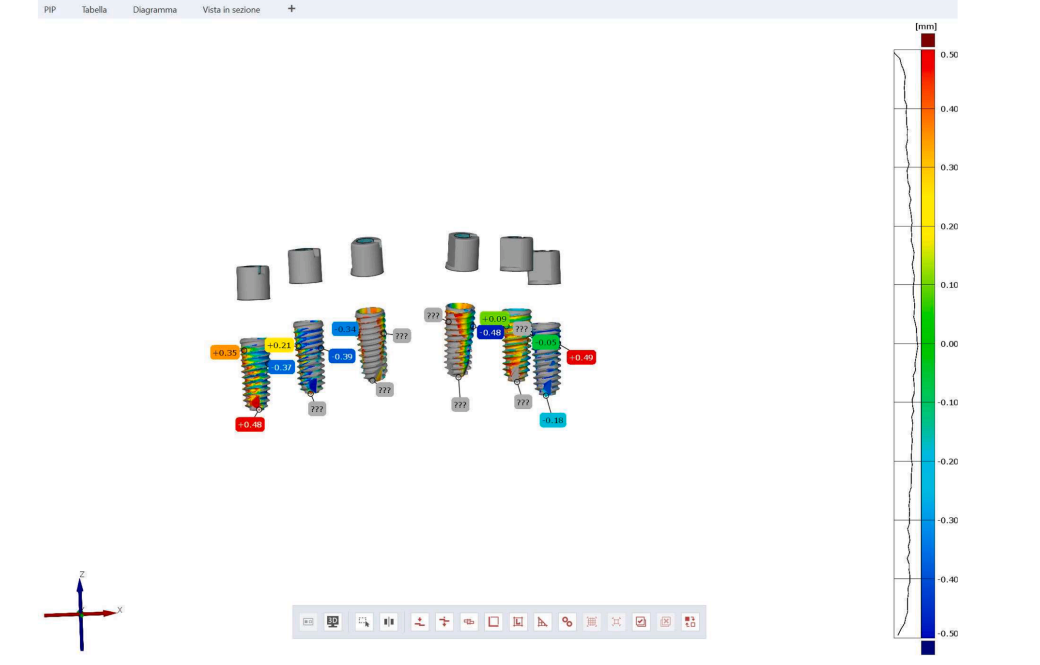
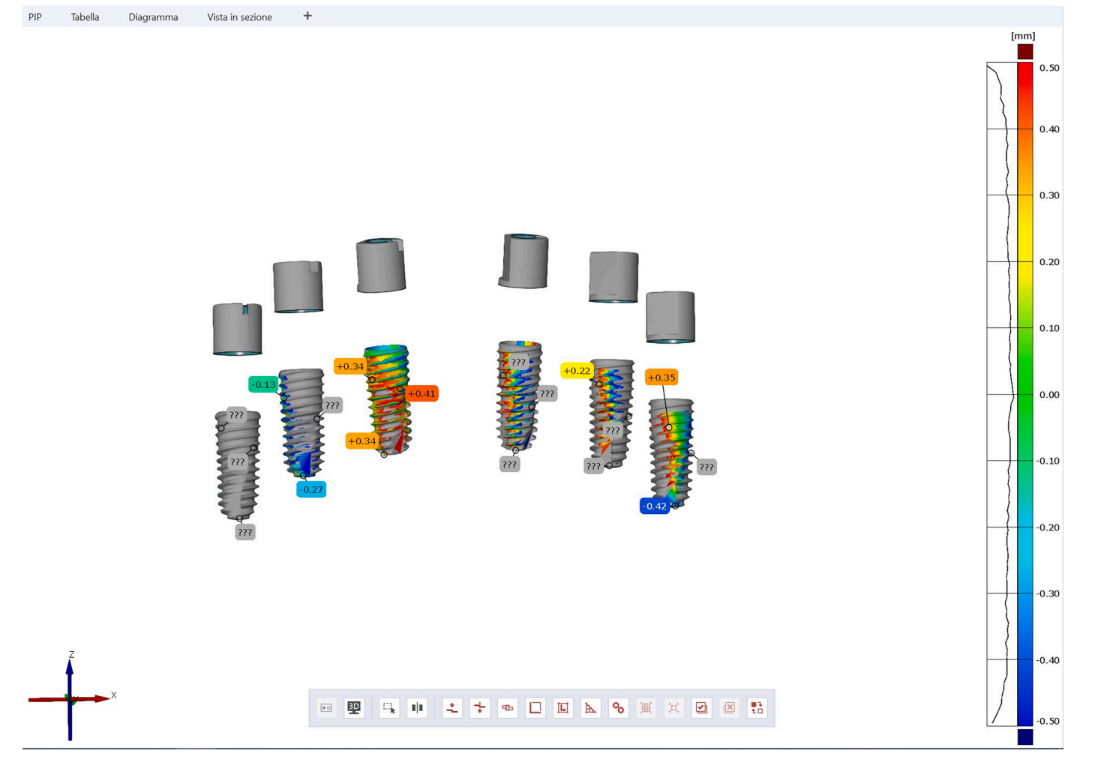
Outcome measures were surface deviation and accuracy, established by measuring (Optical RevEng 4.0, Open Technologies, Rezzato (BS), Italy) the difference between the digitalized scan abutments position (postoperative STL, Standard Triangle Language file), matched with the original STL file, derived from the virtual implant plan, used as a reference. The reference and the digitalized models were superimposed and registered, and the deviation values between the two surfaces were calculated as surface comparison (horizontal and angle), while, the accuracy was evaluated as the combination of trueness and precision.
The “trueness”, defined as the “closeness of agreement between the arithmetic mean of a large number of test results and the true or accepted reference value”, was evaluated using GOM Inspect Profes- sional (GOM, Braunschweig, Germany) by assessing the deviations values between planned and real placed implants. The qualitative analyses were presented using colorimetric scale measurements. Deviations at tolerance levels from ±0.5 mm were analyzed (Figs. 8, 9). Meanwhile, “precision” was defined as “the closeness of agreement between different test results”. The precision was assessed as the horizontal and angular deviations between the digitalized and original scan abutments positions, calculated along the long axis of each scan abutment (Rhino 6, McNeel Europe SL, Barcelona, Spain).
A blinded, expert, dental technician performed all of the measurements. An independent assessor, not previously involved in the study, performed all the measurements.
Statistical analyses were performed using NUMBERS, version 11.2 (Apple Inc., Cupertino, CA, USA) and online calculators (ANOVA calculator, https://www.statskingdom.com/180Anova1way.html). Mean values and standard deviation (SD) were calculated. Comparisons between groups for continuous outcomes (students versus expert and screwed versus pushed pins) were made by unpaired tests, in order to detect any changes in the accuracy. One-way analysis of variance (ANOVA) was conducted to determine the effect of the different guide designs on the final accuracy. An independent clinician not previously involved in the study, with expertise in medical statistics, performed all the analyses.
Results
A total of 12 surgical templates were printed and used, and a total of 72 fully guided implants (Dummy fixture, Osstem Implants, Seoul, South Korea) were placed according to the manufacturers’ instructions. The accuracy of the surgical templates in each group were compared in different scenarios. All the data are summarized in Tables 2-7.
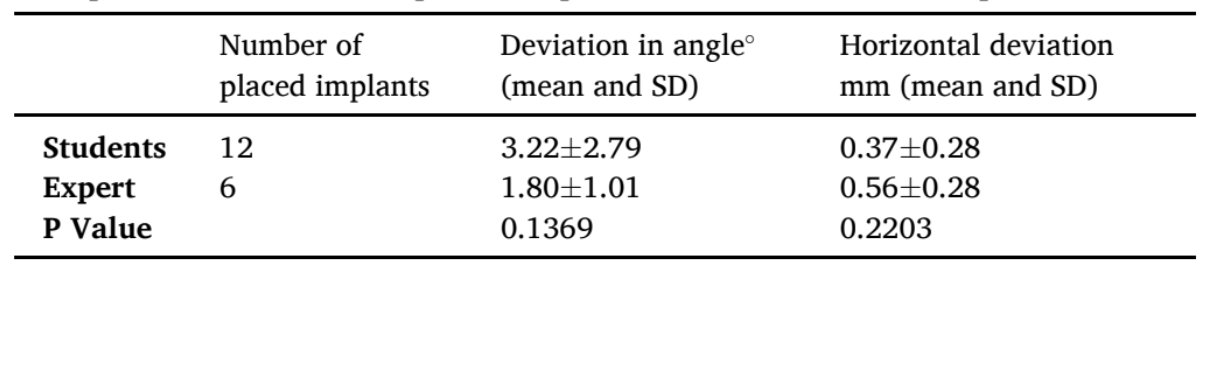
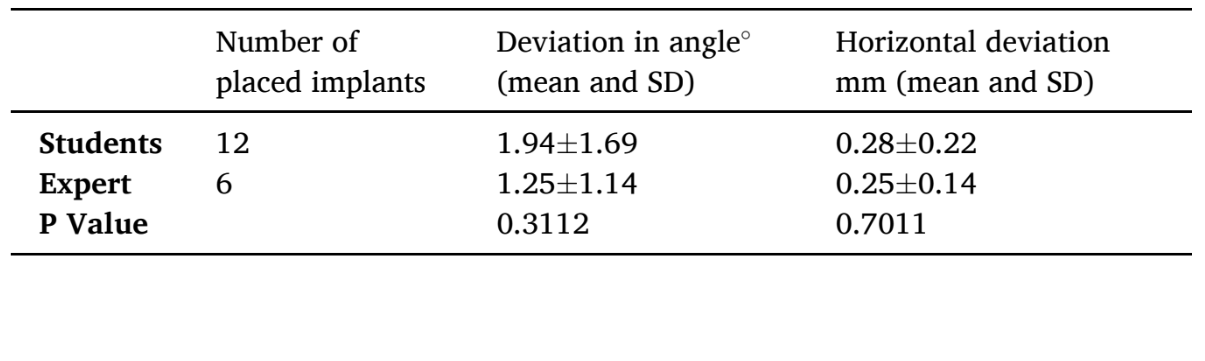
3.1. Differences between groups by expert and students
Although there is a trend of higher accuracy when the implants were placed by the expert clinician, no statistically significant difference was found except the deviation in an angle value (students 2.13±1.46° versus expert 0.90±0.91°; P Value=0.0447), reported in the group 3, when the modular guide was used in the combination with a bone reduction (Table 4).
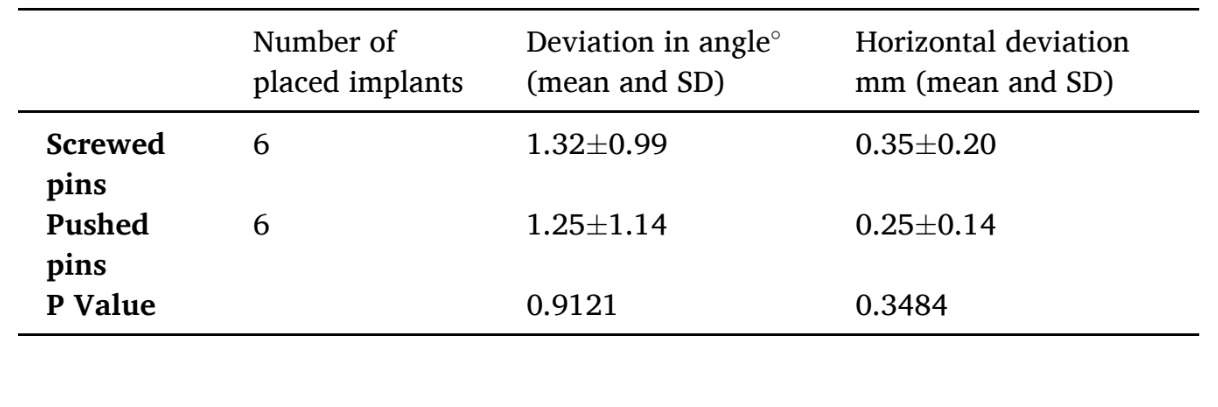
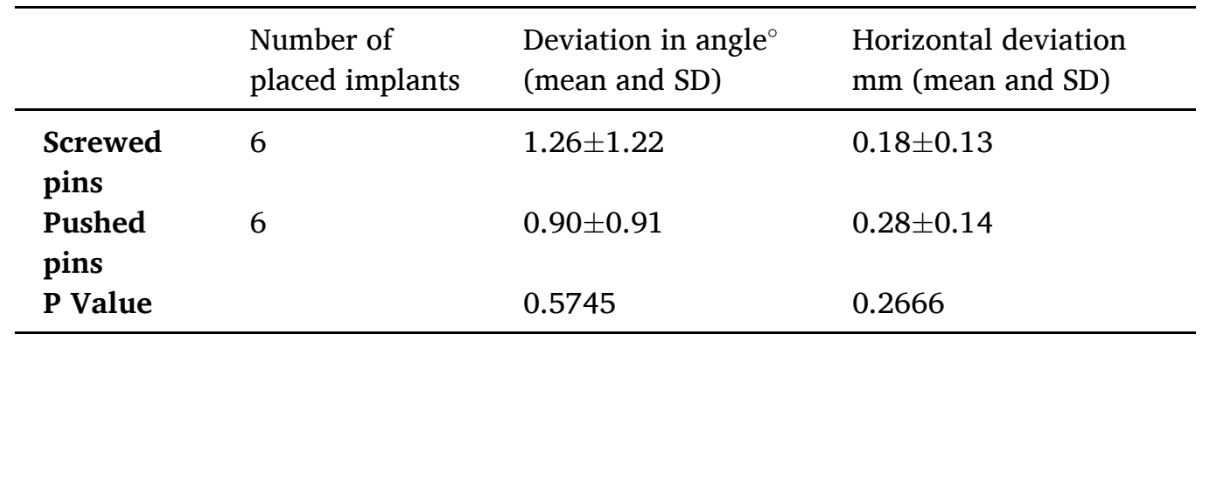
3.2. Differences between screwed versus pushed pins
When screwed versus pushed pins were compared, a statistically significant difference was found in favor of screwed anchor pins, in the group 1, in horizontal deviation (screwed pins 0.18±0.13 mm versus pushed pins 0.56±0.28 mm; P Value=0.0124; Table 5). In the same group, deviation in an angle was found to be not statistically significant different, even if a trend of better accuracy can be suggested for screwed pins (1.42° versus 1.80°). In the group 2 and 3 no statistically significant differences were found (Table 6 and 7).
3.3. Effect of different guide designs on final accuracy
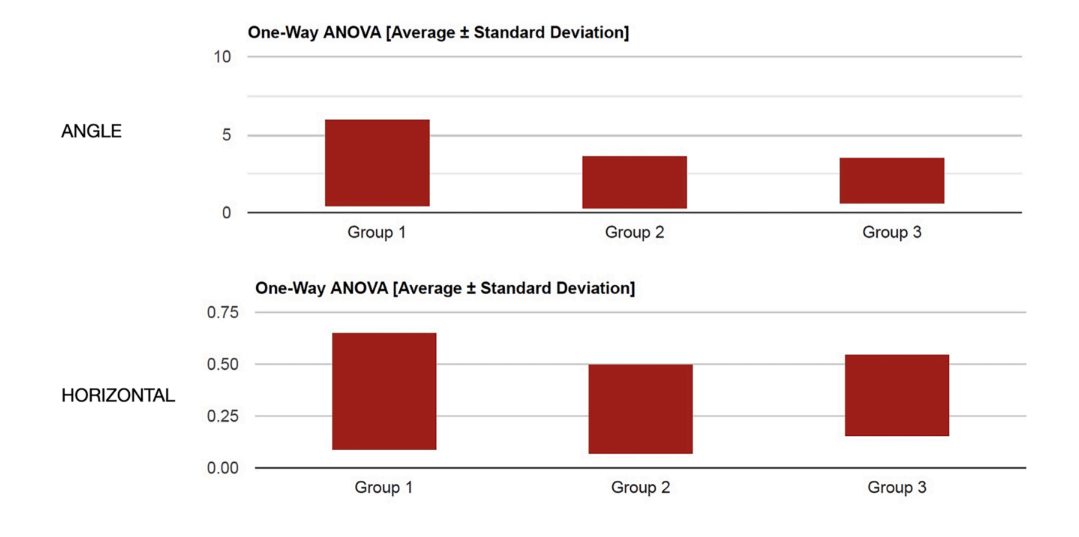
Although the overall accuracy got better with practice, no statistically significant difference was found between different template designs when the fully guided implants were placed by students, in both angle and horizontally (P = 0.2787 and P = 0.6601, respectively, Fig. 10). Nevertheless, the most complex treatment was performed lastly.
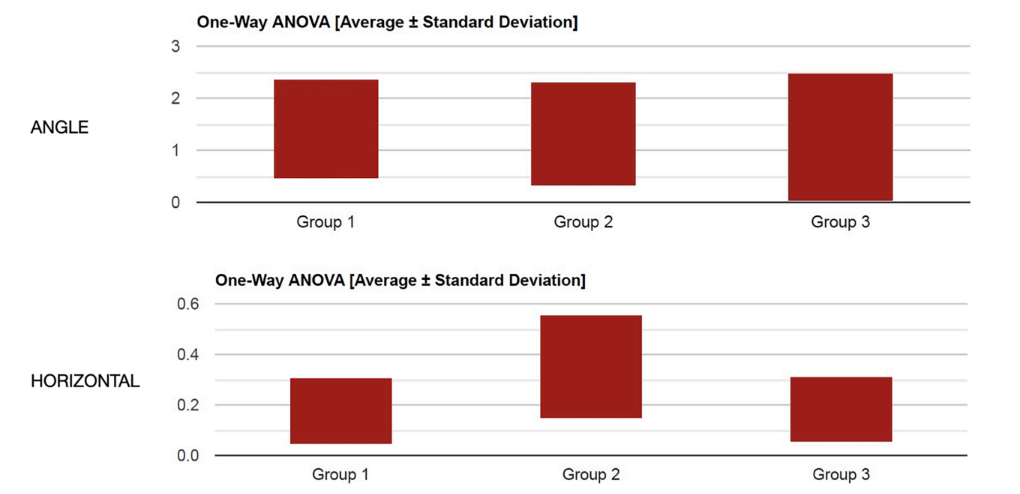
Similarly, no statistically significant difference was found between groups when the implants were placed by an expert, using pushed anchor pins, in both angle and horizontal plane (P = 0.9671 and P = 0.1349, respectively, Fig. 11). On the contrary, a statistically significant difference was found between groups when the implants were placed by an expert clinician, with better value using screwed anchor pins, in the horizontal plane (P = 0.0293) but not in angle (P = 0.3380, Fig. 12).
Discussion
This in-vitro research was performed to evaluate the accuracy of modular surgical templates for fully guided implant placement in complete arch restorations, with and without bone reduction. Pre-clinical results demonstrated that similar accuracy can be achieve using modular guides compared with conventional (one piece template) templates. However, modular guides may offer additional benefits as guidance for easier, pre-planned bone reduction, and/or faster and more accurate screw-retained, temporary prosthesis delivery.
All the tested surgical templates have been proved to be safe, showing level of discrepancy between the planned and the real implants position, within the error margins already suggested in the literature (about 1.5–2 mm). The possible reason why expert and students experienced similar results was probably due to the in-vitro nature of the study. Using a surgical template, the error margin should be limited to the tolerance of the sleeves. However, in vivo, there are several factors that could influent the final accuracy of the placed implants. For the latter, the results of the present preliminary in-vitro research, should be interpretate with caution. However, the final accuracy of modular guides is encouraging for its application in daily practice, mainly by expert clinicians. Then, less experienced clinicians should start with simple cases and simple guides, such and non-aesthetic areas of partial edentulous ridges. Such learning curve allows to master the technique and digital workflow in implant dentistry. In addition, it is well documented that the accuracy is higher in case of teeth supported templates compared with mucosa supported guides.
There are two important data that must to be considered from the present research. The first result was that within students, the overall accuracy improved with practice. This result is in agreement with another in-vitro research published by Cushen and Turkyilmaz, concluding that, the experience level of the operator contributes to the final accuracy of the placed implants. Although students reached successful results within the safety margins up to 2 mm, statistically significant higher accuracy was found in angle deviation, in case of modular guide with bone reduction. Moreover, higher accuracy was found case by case, demonstrating that more experienced operators place implants more accurately.
The second data confirmed that expert clinicians can provide a trend of higher level of accuracy, even in case of modular templates and bone reduction. In the literature, several surgical guides and protocols have been proposed to perform bone reduction before implant placement. When required, bone reduction is an useful step to obtain suitable width of the bone, flattening the bone crest, and to provide the required restorative space based on material selection. Using digital technologies, such as in the present research, bone reduction and implant placement can be accomplished guided and in the same surgical procedure. Digital planning allows to plan in advance the amount of bone to be reduced, guiding the clinician during surgery, minimizing trauma and stress for the patient, and making immediate loading easier and faster. Moreover, after bone reduction, vertical dimension and maxilla-mandibular relationship are compromised. Modular guides allow to plan in advance the interim restoration, making easier the immediate loading procedures, including stabilization of the temporary prosthesis at the correct vertical dimension and occlusion. However, flawless data collection, proper virtual planning, accurate guide design and printing, as well as proper clinical execution are all mandatory to obtain overall successful results.
Last but not the least, screwed pins demonstrated higher accuracy than pushed pins. Screwed pins should be used when the base portion of the modular guide must not to be removed. On the contrary, screwed pins can lose stability when they are unscrewed and then screwed back again. In such cases, pushed pins may be chosen.
Looking at some further consideration, there are some other fields of application of modular templates, such us immediate implants in patient with failing dentition, and definitive prosthesis delivery at the day of the surgery. However, further studies are needed to validate modular guides in case of immediate implants.
The main limitation of the present research is the in-vitro nature that may underestimate some clinical factors. Then, the next limitation is that all modules used in this study were fixed together with metallic mini screws. Modular guides are already used in daily practice, and digital technologies development provide new possibilities to design and produce fixing elements including magnetic connectors, conical pins and others. Even if these results are encouraging, there is still need for further researches to confirm these preliminary results, and test all possibilities of modular templates.
Conclusions
- With the limitation of the present in-vitro research, the following conclusions can be drawn:
- Modular templates may be safely used showing similar level of accuracy then one-piece conventional guide.
- Although students showed lower level of accuracy than expert, the mean values were within the error margin of the software.
- Within students, accuracy improved with practice, highlighting the importance of the learning curve.
- Screwed pins should be used to fix the base portion in case of modular surgical guides.
Marco Tallarico, Łukasz Zadrożny, Fabio Pia, Anna Di Marzio, Silvio Mario Meloni, Francesco Grande, Santo Catapano, Milena Pisano
References
- P.M. Soares, G.D.A. Silveira, L.S. Gonçalves, A. Bacchi, G.K.R. Pereira, Maintenance protocols for implant-supported dental prostheses: a scoping review, J. Prosthet. Dent. (2022).
- I. Darby, Risk factors for periodontitis & peri-implantitis, Periodontol. 2000 90 (1) (2022) 9–12.
- M. Tallarico, M. Czajkowska, M. Cicciù, F. Giardina, A. Minciarelli, Ł. Zadrożny, C. J. Park, S.M. Meloni, Accuracy of surgical templates with and without metallic sleeves in case of partial arch restorations: a systematic review, J. Dent. 115 (2021) 103852.
- Ł. Zadrożny, M. Czajkowska, M. Tallarico, L. Wagner, J. Markowski, E. Mijiritsky, M. Cicciù, Prosthetic Surgical Templates and Dental Implant Site Time Preparation: an In Vitro Study, Prosthesis 4 (1) (2022) 25–37.
- S. Chandran, L. Sers, G. Picciocchi, F. Luongo, H. Lerner, M. Engelschalk, S. Omar, Guided implant surgery with R2Gate®: a multicenter retrospective clinical study with 1 year of follow-up, J. Dent. 127 (2022) 104349.
- S. Li, C. Yi, Z. Yu, A. Wu, Y. Zhang, Y. Lin, Accuracy assessment of implant placement with versus without a CAD/CAM surgical guide by novices versus specialists via the digital registration method: an in vitro randomized crossover study, BMC. Oral Health 23 (1) (2023) 426.
- T. Elliott, A. Hamilton, N. Griseto, G.O. Gallucci, Additively Manufactured Surgical Implant Guides: a Review, J. Prosthodont. 31 (S1) (2022) 38–46.
- F. Luongo, H. Lerner, C. Gesso, A. Sormani, Z. Kalemaj, G. Luongo, Accuracy in static guided implant surgery: results from a multicenter retrospective clinical study on 21 patients treated in three private practices, J. Dent. 140 (2024) 104795.
- M. Tallarico, D. Galiffi, R. Scrascia, M. Gualandri, Ł. Zadrożny, M. Czajkowska, S. Catapano, F. Grande, E. Baldoni, A.I. Lumbau, S.M. Meloni, M. Pisano, Digital Workflow for Prosthetically Driven Implants Placement and Digital Cross Mounting: a Retrospective Case Series, Prosthesis 4 (3) (2022) 353–368.
- J.-Y. Park, Y.W. Song, S.-H. Park, J.-H. Kim, J.-M. Park, J.-S. Lee, Clinical factors influencing implant positioning by guided surgery using a nonmetal sleeve template in the partially edentulous ridge: multiple regression analysis of a prospective cohort, Clin. Oral Implants Res. 31 (12) (2020) 1187–1198.
- C.R. Hatz, B. Msallem, S. Aghlmandi, P. Brantner, F.M. Thieringer, Can an entrylevel 3D printer create high-quality anatomical models? Accuracy assessment of mandibular models printed by a desktop 3D printer and a professional device, Int. J. Oral Maxillofac. Surg. 49 (1) (2020) 143–148.
- C. Berli, F.M. Thieringer, N. Sharma, J.A. Müller, P. Dedem, J. Fischer, N. Rohr, Comparing the mechanical properties of pressed, milled, and 3D-printed resins for occlusal devices, J. Prosthet. Dent. 124 (6) (2020) 780–786.
- K.C. Oh, J.M. Park, J.S. Shim, J.H. Kim, J.E. Kim, J.H. Kim, Assessment of metal sleeve-free 3D-printed implant surgical guides, Dent. Mater. 35 (3) (2019) 468–476.
- D. Kaewsiri, S. Panmekiate, K. Subbalekha, N. Mattheos, A. Pimkhaokham, The accuracy of static vs. dynamic computer-assisted implant surgery in single tooth space: a randomized controlled trial, Clin. Oral Implants Res. 30 (6) (2019) 505–514.
- C.M. Cristache, S. Gurbanescu, Accuracy Evaluation of a Stereolithographic Surgical Template for Dental Implant Insertion Using 3D Superimposition Protocol, Int. J. Dent. 2017 (2017) 4292081.
- P. Smitkarn, K. Subbalekha, N. Mattheos, A. Pimkhaokham, The accuracy of single-tooth implants placed using fully digital-guided surgery and freehand implant surgery, J. Clin. Periodontol. 46 (9) (2019) 949–957.
- A.M. Greenberg, Advanced dental implant placement techniques, J. Istanb. Univ. Fac. Dent. 51 (3 Suppl 1) (2017) S76–s89.
- S. Chandran K R, M. Goyal, N. Mittal, J.S. George, Accuracy of freehand versus guided immediate implant placement: a randomized controlled trial, J. Dent. 136 (2023) 104620.
- H. Arora, S. Ivanovski, Clinical and aesthetic outcomes of immediately placed single-tooth implants with immediate vs. delayed restoration in the anterior maxilla: a retrospective cohort study, Clin. Oral Implants Res. 29 (3) (2018) 346–352.
- T. Cantoni, P. Giovanni, Implant treatment planning in fresh extraction sockets: use of a novel radiographic guide and CAD/CAM technology, Quintessence Int. 40 (9) (2009) 773–781.
- N. Khzam, H. Arora, P. Kim, A. Fisher, N. Mattheos, S. Ivanovski, Systematic Review of Soft Tissue Alterations and Esthetic Outcomes Following Immediate Implant Placement and Restoration of Single Implants in the Anterior Maxilla, J. Periodontol. 86 (12) (2015) 1321–1330.
- R. Ellis, S. Chen, H. Davies, W. Fitzgerald, J. Xu, I. Darby, Primary stability and healing outcomes of apically tapered and straight implants placed into fresh extraction sockets. A pre-clinical in vivo study, Clin. Oral Implants Res. 31 (8) (2020) 705–714.
- T. Chackartchi, G.E. Romanos, L. Parkanyi, F. Schwarz, A. Sculean, Reducing errors in guided implant surgery to optimize treatment outcomes, Periodontol. 2000 88 (1) (2022) 64–72.
- D. Schneider, M. Sancho-Puchades, J. Mir-Marí, S. Mühlemann, R. Jung, C. Hämmerle, A Randomized Controlled Clinical Trial Comparing Conventional and Computer-Assisted Implant Planning and Placement in Partially Edentulous Patients. Part 4: accuracy of Implant Placement, Int. J. Periodontics Restorative Dent. 39 (4) (2019) e111–e122.
- J. Li, P.C. Meneghetti, M. Galli, G. Mendonca, Z. Chen, H.-L. Wang, Open-sleeve templates for computer-assisted implant surgery at healed or extraction sockets: an in vitro comparison to closed-sleeve guided system and free-hand approach, Clin. Oral Implants Res. 33 (7) (2022) 757–767.
- F. Raes, T. Eccellente, C. Lenzi, M. Ortolani, G. Luongo, C. Mangano, F. Mangano, Immediate functional loading of single implants: a multicenter study with 4 years of follow-up, J. Dent. Res. Dent. Clin. Dent. Prospects. 12 (1) (2018) 26–37.
- R. Fürhauser, D. Florescu, T. Benesch, R. Haas, G. Mailath, G. Watzek, Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score, Clin. Oral Implants Res. 16 (6) (2005) 639–644.
- G. Tonellini, R. Saez Vigo, G. Novelli, Double Guided Surgery in All-on-4(®) Concept: when Ostectomy Is Needed, Int. J. Dent. 2018 (2018) 2672549.
- S. Chandran, L. Sers, G. Picciocchi, F. Luongo, H. Lerner, M. Engelschalk, S. Omar, Guided implant surgery with R2Gate®: a multicenter retrospective clinical study with 1 year of follow-up, J. Dent. 127 (2022) 104349.
- M. Colombo, C. Mangano, E. Mijiritsky, M. Krebs, U. Hauschild, T. Fortin, Clinical applications and effectiveness of guided implant surgery: a critical review based on randomized controlled trials, BMC. Oral Health 17 (1) (2017) 150.
- J. Mouhyi, M.A. Salama, F.G. Mangano, C. Mangano, B. Margiani, O. Admakin, A novel guided surgery system with a sleeveless open frame structure: a retrospective clinical study on 38 partially edentulous patients with 1 year of follow-up, BMC. Oral Health 19 (1) (2019) 253.
- Ł. Zadrożny, M. Czajkowska, M. Tallarico, Multi goal, guided approach as a minimally invasive treatment: a case report, J. Dent. 121 (2022) 104012.
- E. Mijiritsky, H. Ben Zaken, M. Shacham, I.C. Cinar, C. Tore, K. Nagy, S.D. Ganz, Variety of Surgical Guides and Protocols for Bone Reduction Prior to Implant Placement: a Narrative Review, Int. J. Environ. Res. Public Health 18 (5) (2021).
- Proceeding of the International Digital Dentistry Society World Congress, in: Baden Baden 2019, 19, BMC Oral Health, 2019, p. 257.
- J. Krithikadatta, V. Gopikrishna, M. Datta, CRIS Guidelines (Checklist for Reporting In-vitro Studies): a concept note on the need for standardized guidelines for improving quality and transparency in reporting in-vitro studies in experimental dental research, J. Conserv. Dent. 17 (4) (2014) 301–304.
- R.H. Putra, N. Yoda, E.R. Astuti, K. Sasaki, The accuracy of implant placement with computer-guided surgery in partially edentulous patients and possible influencing factors: a systematic review and meta-analysis, J. Prosthodont. Res. 66 (1) (2022) 29–39.
- A. Tahmaseb, V. Wu, D. Wismeijer, W. Coucke, C. Evans, The accuracy of static computer-aided implant surgery: a systematic review and meta-analysis, Clin. Oral Implants Res. 29 (16) (2018) 416–435. Suppl.
- S.E. Cushen, I. Turkyilmaz, Impact of operator experience on the accuracy of implant placement with stereolithographic surgical templates: an in vitro study, J. Prosthet. Dent. 109 (4) (2013) 248–254.
- J. Abduo, D. Lau, Duration, deviation and operator’s perception of static computer assisted implant placements by inexperienced clinicians, Eur. J. Dent. Educ. 26 (3) (2022) 477–487.
- S. Rothlauf, S. Pieralli, C. Wesemann, F. Burkhardt, K. Vach, F. Kernen, B.C. Spies, Influence of planning software and template design on the accuracy of static computer assisted implant surgery performed using guides fabricated with material extrusion technology: an in vitro study, J. Dent. 132 (2023) 104482.
- F.A. Dulla, E. Couso-Queiruga, V. Chappuis, B. Yilmaz, S. Abou-Ayash, C. Raabe, Influence of alveolar ridge morphology and guide-hole design on the accuracy of static Computer-Assisted Implant Surgery with two implant macro-designs: an in vitro study, J. Dent. 130 (2023) 104426.

/public-service/media/default/446/xUzvr_671a187c9aa46.png)
/public-service/media/default/455/zGYoq_671a1ed13fef9.jpg)
/public-service/media/default/454/7jN0r_671a1b5b648ff.jpg)
/public-service/media/default/456/3eXLd_671a1f18319d2.jpg)