Autotransplantation of Teeth
Machine translation
Original article is written in RU language (link to read it) .
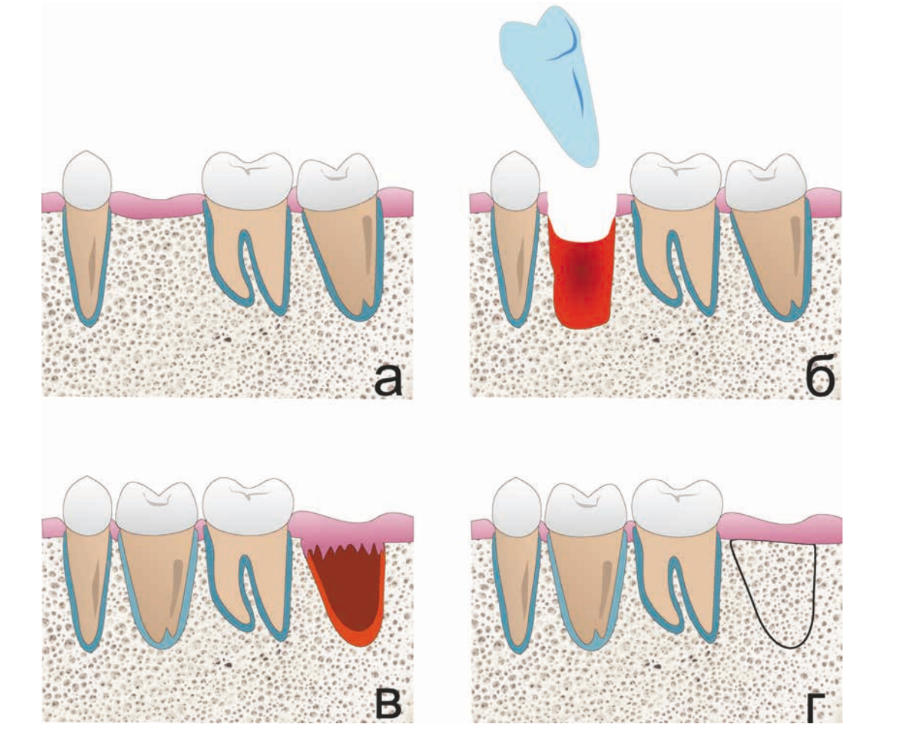
The method of autotransplantation in adults involves the transplantation of a wisdom tooth to the place of any other tooth in the lower or upper jaws. It can be performed either in the socket of the removed tooth or in a newly formed alveolus. Recent studies have shown that after the tooth integrates, a complete periodontal ligament is formed, and functionally the transplant does not differ from other teeth. Significant differences between tooth autotransplantation and implantation include integration times of up to 2 months and the formation of a complete periodontal ligament, which prevents bone resorption and simplifies prosthetics.
The aim of the study is to increase the effectiveness of treatment for adult patients with partial tooth loss through autotransplantation.
Materials and methods: the study was conducted on 64 patients aged 18 to 62 years without somatic diseases. Autotransplantation of 39 upper and 15 lower teeth was performed in natural and artificially created tooth sockets. Splinting was carried out with a non-rigid wire splint for 3 weeks. Endodontic treatment was performed within 2 weeks after the surgery. Results were evaluated using clinical and radiological methods at 6, 12, and 18 months after the surgery.
Results. According to the study, the success rate of this method was 82.4% (n = 56); mobility of II degree or higher was found in 1.5% (n = 1); ankylosis was determined in 4.5% (n = 3); 5.8% (n = 4) were removed due to inflammatory resorption.
Conclusions: the effectiveness of the autotransplantation method depends on many factors, such as the patient's age, the condition of the periodontal ligament of the donor tooth, and the techniques used during the operation. This should be taken into account when selecting a clinical case.
Introduction
Long-term observations prove that the effectiveness of autotransplantation is about 95% (tooth survival for more than 10 years). This method can be applied for the restoration of single included and terminal defects of the dental arch. Understanding the processes of periodontal complex regeneration has allowed the development of the most effective techniques for performing tooth-preserving surgeries. For example, using a wisdom tooth as a graft in the molar area allows for the creation of a full chewing unit within 2-3 months and, in most cases, does not require further prosthetics. It should also be noted that after complete regeneration, the functioning periodontal ligament serves as the basis for stable microcirculation and prevents bone resorption, which is a huge advantage over other methods. The increase in research on tooth transplantation, modification of the technique itself, as well as stable long-term results open new opportunities for dental care for patients.
Undoubtedly, the limitation on the number of possible transplant teeth does not place this method on the same level as implantation, but if the clinical situation allows for the use of a tooth instead of an implant, it may be the best solution for the patient.
Operations
Clinical case.
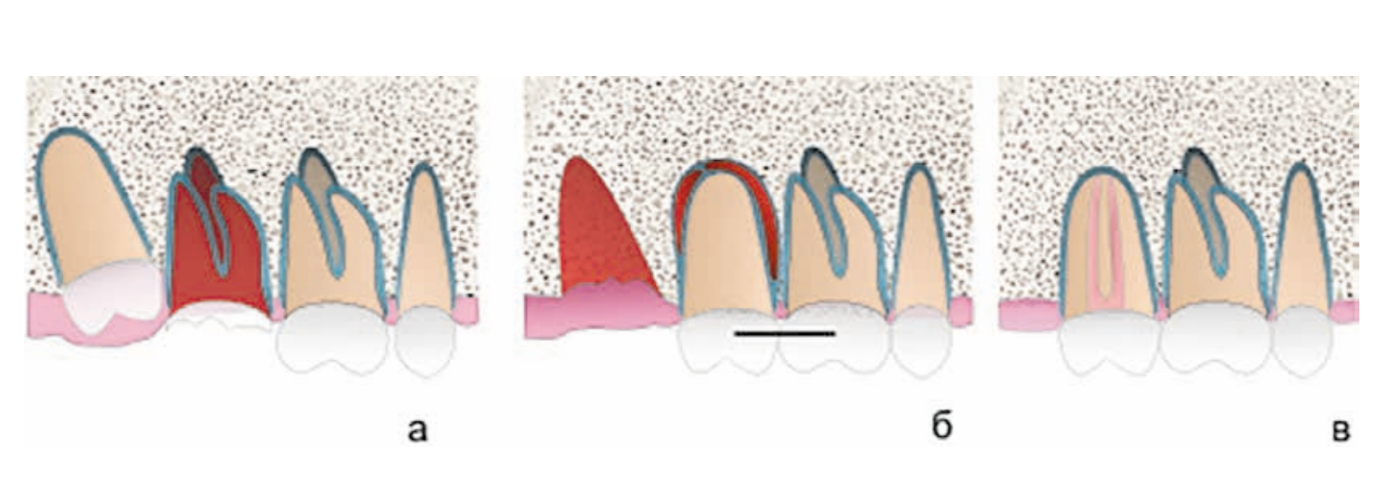
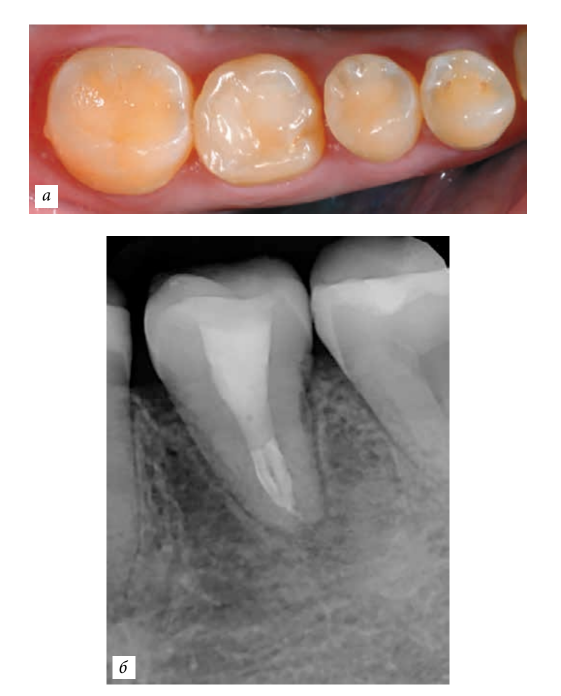
A 31-year-old female patient was referred by her treating physician for the extraction of teeth 1.7 and 1.8, followed by implantation and prosthetics in the area of tooth 1.7. After consulting with the referring physician, an alternative plan was proposed to the patient, which included the extraction of tooth 1.7 and autotransplantation of 1.8 into the socket of tooth 1.7. Since both teeth were to be extracted, the possibility of preserving one of them was decisive in choosing the optimal treatment plan.
1. Autotransplantation into the socket of the extracted tooth with a chronic inflammatory process
Clinical case.
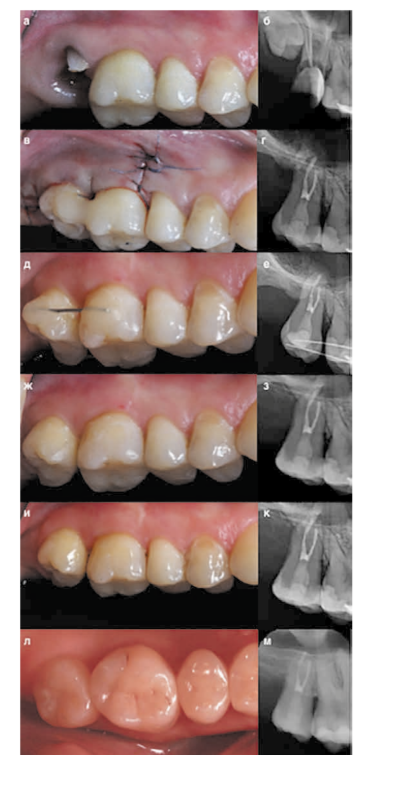
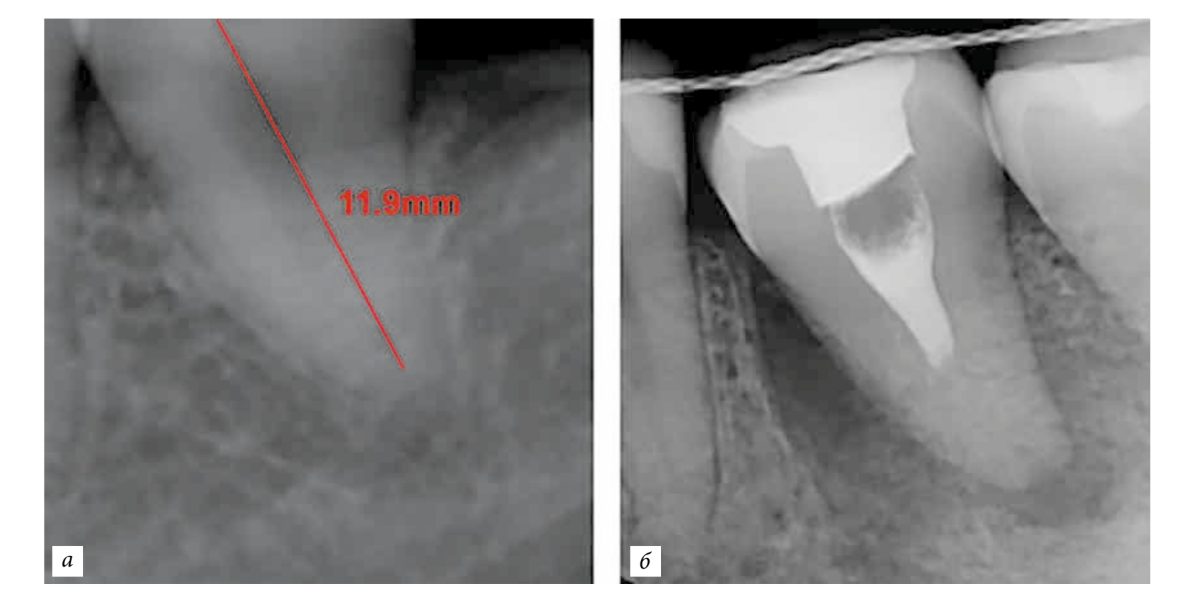
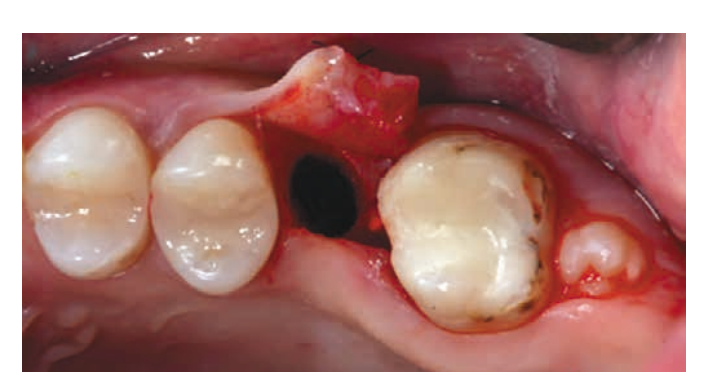
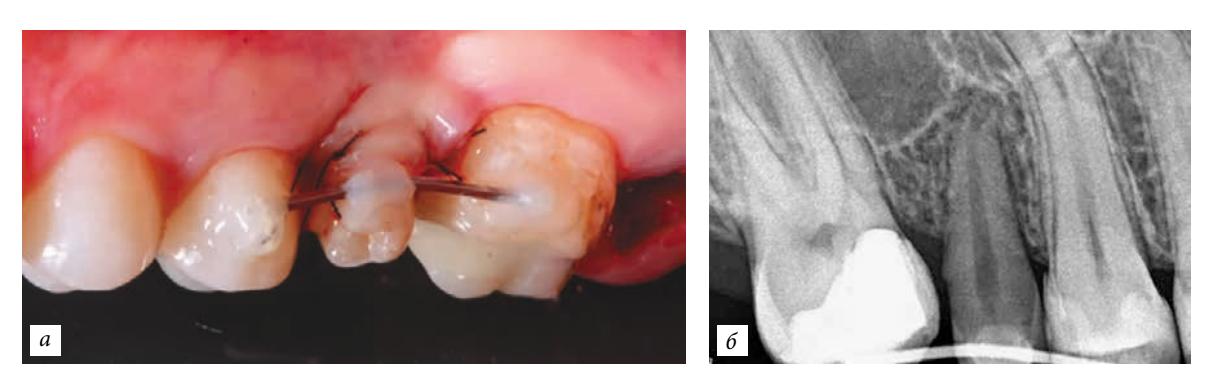
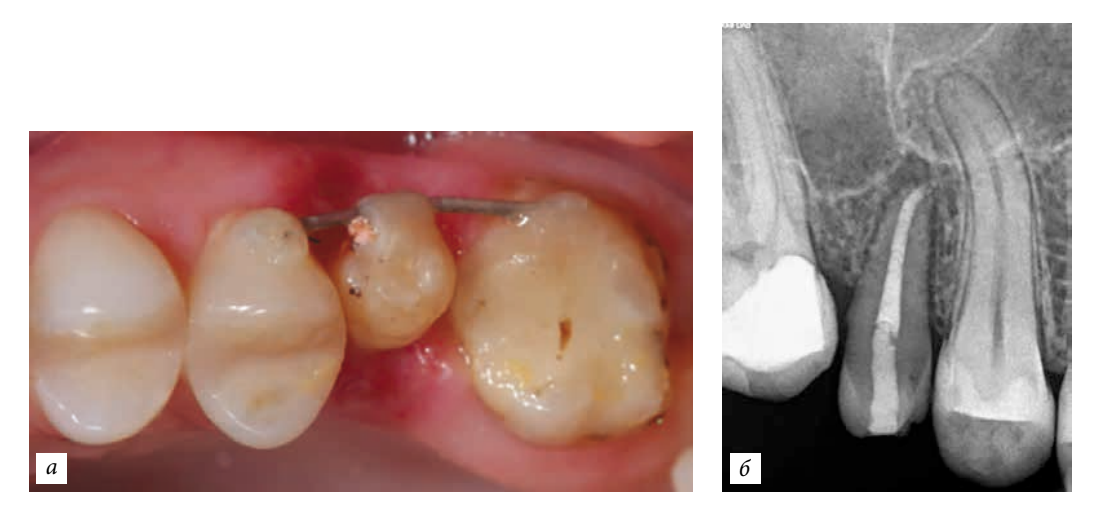
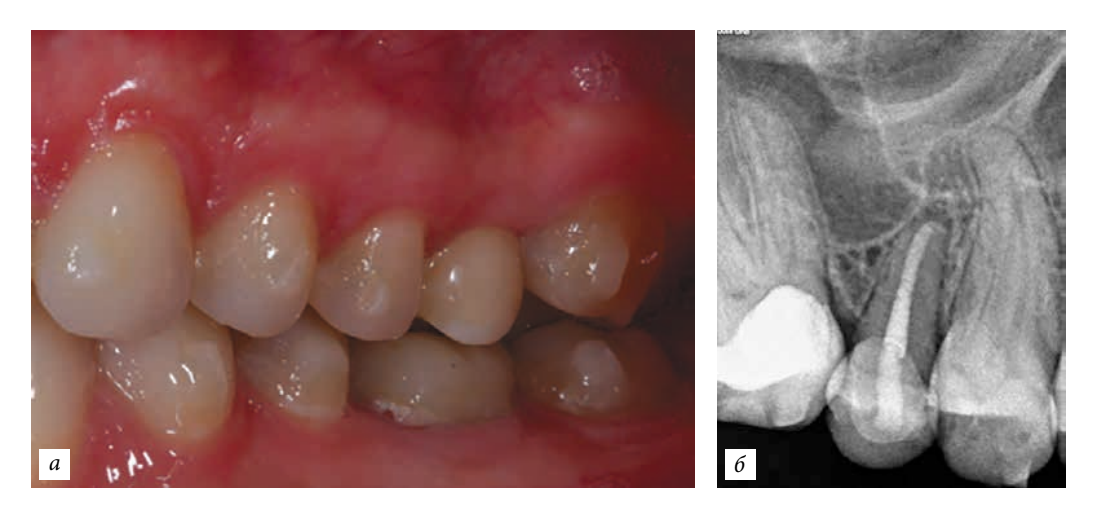
A 29-year-old female patient presented with complaints of aching pain in the area of tooth 4.6. The diagnosis was chronic periodontitis, root resorption. Tooth 4.8 has a conical root and does not participate in chewing. A decision was made to autotransplant tooth 4.8 into the socket of 4.6. Since the crown of tooth 4.8 was fully erupted, with full mouth opening, endodontic treatment was performed, and the canals were temporarily filled with calcium hydroxide. Subsequently, tooth 4.6 was extracted, followed by curettage of the socket and autotransplantation of 4.8. Fixation with a bilateral non-rigid splint. Soft tissue suturing. The splint was removed after 3 weeks.
2. Autotransplantation into an artificially created socket


Clinical case.
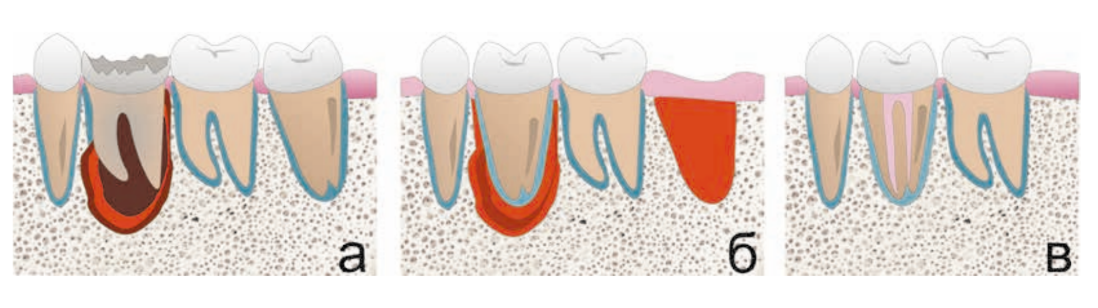
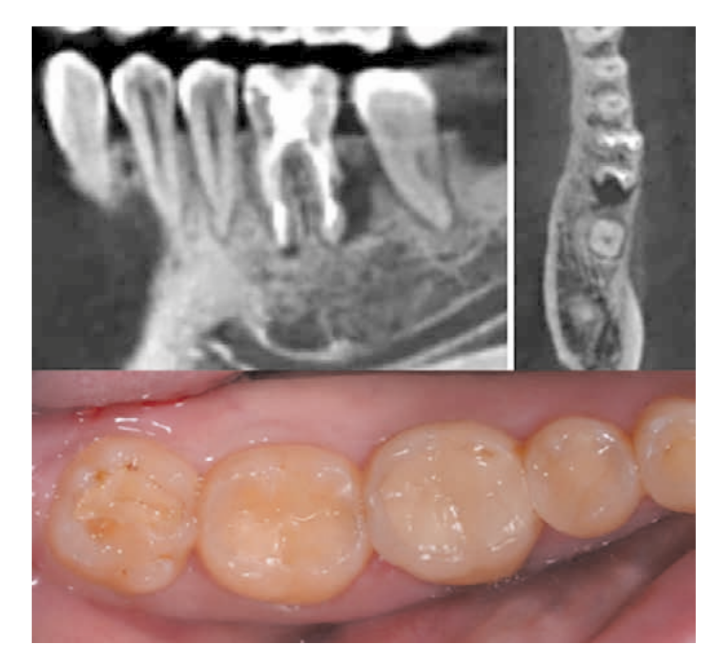
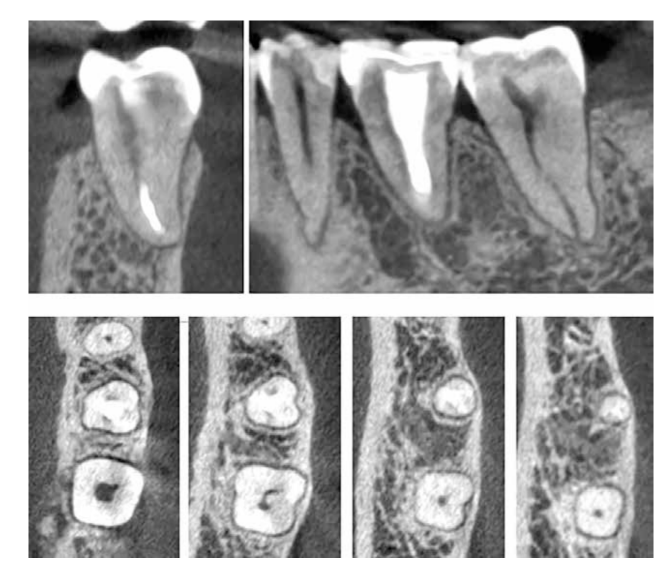
A 25-year-old female patient presented with the absence of tooth 1.6. The tooth had been extracted in childhood. Upon examination, tooth 1.7 was found to be mesially displaced, there was atrophy of the bone tissue in the area of 1.6, and microdontia of 1.8 was observed. To reduce surgical manipulations and the cost of procedures in the case of implant placement, an autotransplantation of tooth 1.8 was performed into an artificially created socket. The socket was formed taking into account the shape and size of the root of 1.8 using a custom piezo attachment. The attachment was modeled using a computed tomography scan and manufactured in the laboratory.

Conclusion
Operations of this kind are perceived by patients with great enthusiasm and are well tolerated. In the postoperative period, pain syndrome and swelling in the area of transplantation are absent, which indicates the biological nature of the method. The appointment of antibiotics is done selectively, for preventive purposes.
Transplantation of teeth from the same morphological group in most cases does not require further prosthetics, allowing for the restoration of the dental arch defect in one visit.
Undoubtedly, the limitation on the number of possible transplant teeth does not place this method on the same level as implantation, but if the clinical situation allows for the use of a tooth instead of an implant, it can be the best solution for the patient.
Authors: Badalyan V. A., Zedgenidze A. M.
Literature:
- Ichinokawa H., et al. The pathological analysis in the experiments on autotransplantation of teeth. Jpn J. Conserv. Dent. 1998; 41: 38.
- Ichinokawa H., et al. The pathological analysis in the experiments on autotransplantation of teeth part 2. The microstructural changes in the healing process. Jpn J. Conserv. Dent. 1998; 41: 91.
- Andreasen JO. Periodontal healing after replantation and autotransplantation of incisors in monkeys. Int J. Oral Surg. 1981; 10: 54—61. Tsukiboshi M. The criteria of implant or transplant. The Quintessence Yearbook. 1995; 132—44.
- Yamamura T., et al. Pathology and Healing. Tokyo: Ishiyaku; 1988.
- Andreasen J. O. Review of root resorption systems and models. Etiology of root resorption and the homeostatic mechanisms of the periodontal ligament. In: Biological Mechanisms of tooth Eruption and root resorption. EBSCO Media; 1988: 9—21.
- I-Kai Wang, Ho-Tai Wu, A retrospective survival analysis of autotransplanted molars in Taipei Veterans General Hospital 1996~2004. J. Dent. Sci. 2007; 2(4): 226—9.
- Yu-Kang Tu, Hsein Kun Lu, Outcomes of Autotransplanted Teeth with Complete Root Formation: A Systematic Review and Meta-Analysis. Art. J. Clin. Periodontol; 2014.
- Machado L. A., do Nascimento R. R. Long-term prognosis of tooth autotransplantation: a systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2016; 45: 610—7
- Abu-Hussein Muhamad, Nezar Watted Tooth Autotransplantation; Clin. Concepts J. Dent. Med. Sci.; 2017.
- Tsukiboshi M. Autotransplantation of teeth: requirements for predictable success. Dent Traumatol. 2002; 18: 157—80.
- Tobe O. Histological studies on periodontal tissue reactions following intentional replantation of incisors in monkeys: with special reference to computer-aided three-dimensional reconstruction of replanted teeth. Jpn J. Conserv. Dent. 1990; 33: 772—802. (in Japanese).
- Proye M. P., Polson A. M. Repair in different zones of the periodontium after tooth reimplantation. J. Periodontol. 1982; 53: 379—89.
- Andreasen J. O. Histometric study of healing of periodontal tissues in rats after surgical injury. I. Design of a standardized surgical procedure. Odontol. Revy. 1976; 27: 115—30.
