Clinical Treatment Concepts for Severe Periodontal Diseases
Machine translation
Original article is written in DE language (link to read it) .
The systematic periodontal therapy requires, especially in severely compromised situations, an interdisciplinary treatment concept. In the first case documentation, the limits of tooth preservation from periodontal perspectives are explained, and the "success" of an implant-supported restoration is documented over a five-year period. The second and third patient documentation discusses possible indications for preservation or extraction.
Case 1
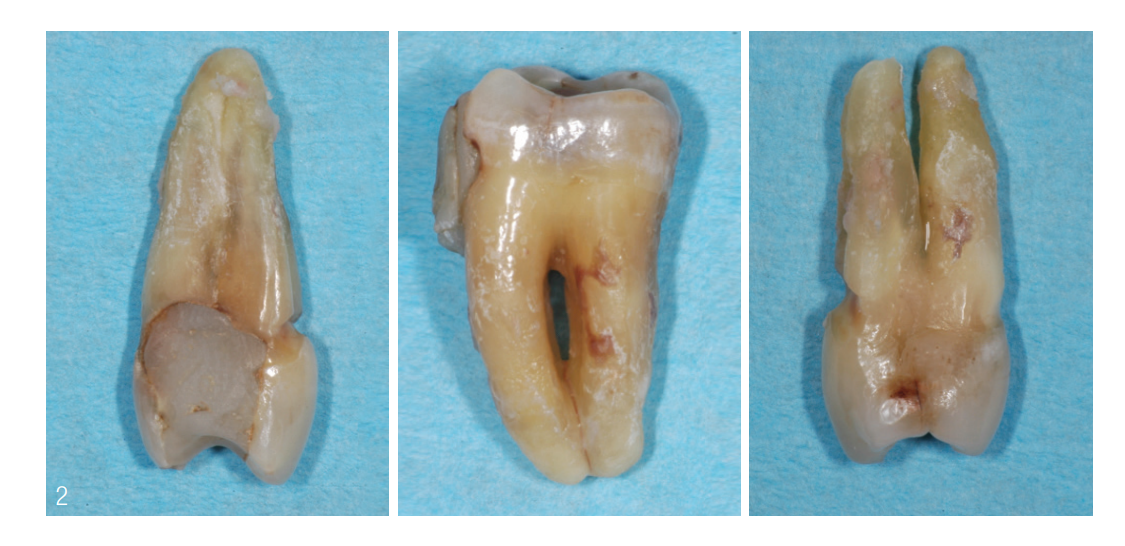
A 59-year-old generally healthy patient presented with the desire for functional rehabilitation. At the time of the initial presentation, there was a periodontally compromised situation, which was accompanied by a high degree of conservative restoration. In both the upper and lower jaws, there was horizontal bone loss of 50 to 70 percent in single-rooted teeth and 50 to 80 percent in multi-rooted teeth. The periodontal situation of the molars and premolars was dominated by increased probing depths (PD) of furcation involvements (Grade II to III) and degrees of mobility (II to III) (Fig. 1 and 2). According to the new classification, there was a periodontal stage III, grade B.

The treatment plan included the following steps:
- Anti-infective therapy with extraction of teeth 16, 15, 14, 26, 27, 37, 36, 46, 47 – the closed dental arch should always be preserved if possible. In this situation, the molars in the lower jaw and second quadrant were affected by deep root caries and caries in the furcation area and could not be preserved despite treatment attempts.
- Reevaluation of the periodontal findings after three and six months before the start of the implant treatment phase
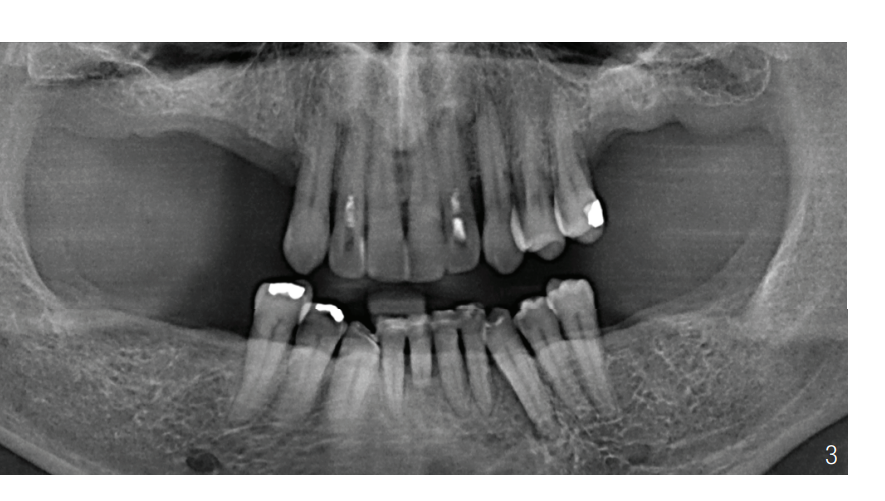
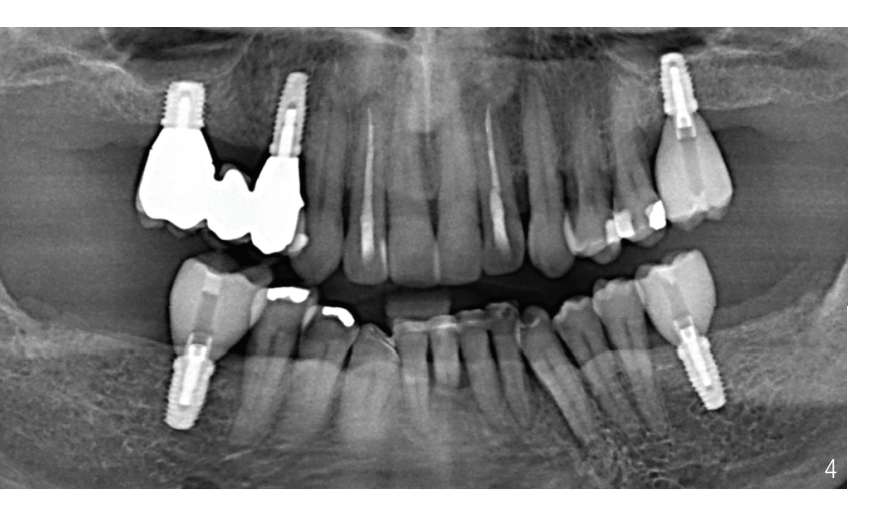
- Implantation in regions 16, 14, 26, 36, and 46 and prosthetic restoration (Fig. 3 and 4)
Implant prosthetic restoration
After a healing phase of six months, the patient could be provided with implants without the need for augmentative measures. Bypassing a sinus floor augmentation – but weighing the higher risk for short implants – an implant with a length and diameter of 6 mm was inserted in the first quadrant in region 16. The diameters of the remaining implants ranged between 3.5 mm and 4 mm with a uniform length of 10 mm.
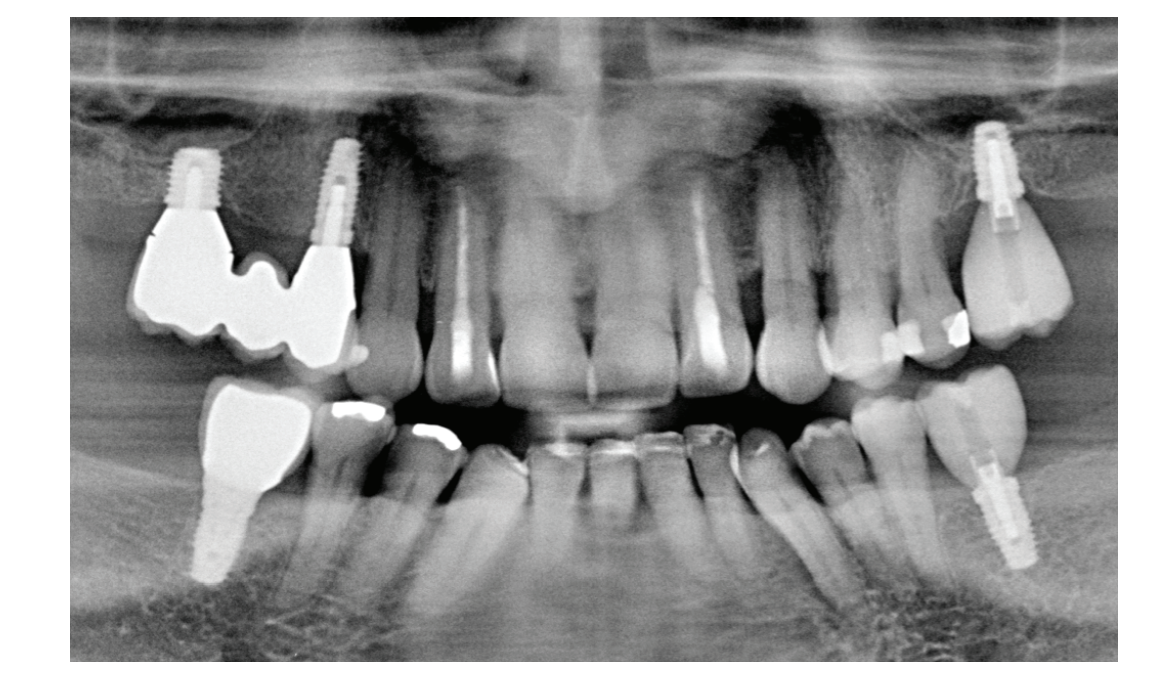
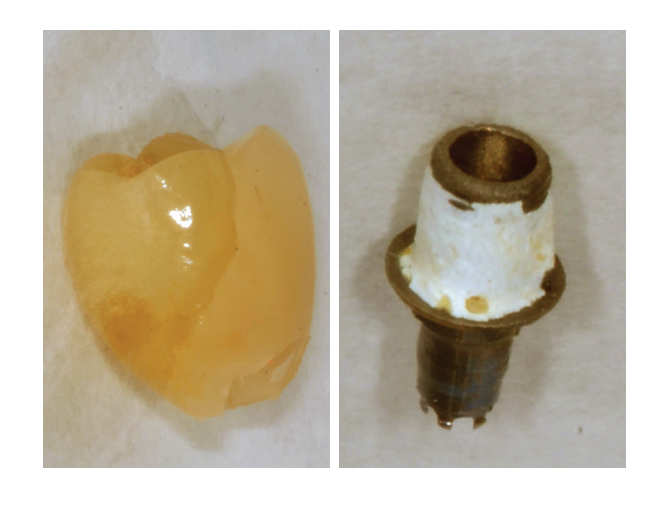
Control after four years of functional time
During the functional period, the patient regularly participated in supportive periodontal therapy (UPT) and demonstrated very good compliance regarding home oral hygiene. After the prosthetic restoration, bone remodeling occurred at all implants between 0.5 mm and 1 mm (Fig. 5). The probing depth at the implants ranged from 3 mm to 5 mm. Sites that reacted positively to Bleeding on Probing (BOP) were regularly treated submucosally in the UPT with powder-water jet application. Throughout the four-year wear period, technical complications were observed on the occlusally screwed superstructures 26, 36, and 46. In addition to ceramic fractures (lithium disilicate), a debonding of the ceramic crown from the bonding base was noted (Fig. 6). This may be attributed to the relatively low height of the bonding base compared to the crown height.
Discussion
Due to the closed dental arch, the initial situation could not have been better. Unfortunately, even in these situations, it is not always possible to preserve all teeth. Especially when some teeth are not worth preserving, no compromises should be made regarding long-term success. This leads to teeth with increased ST in direct proximity to later placed implants being more likely to be removed. Often, in these treatment plans, "only" the molars need to be removed, as the anterior teeth in both the upper and lower jaw can be well splinted with fiberglass bands – if necessary. For the patient in this case, the treatment meant that he did not need a temporary prosthesis after the extractions and maintained his external appearance. By avoiding a tooth-supported and removable prosthesis, the remaining teeth were also preserved.
Case 2
At the time of treatment transfer, the patient was 57 years old. Due to a heart attack, she had been a non-smoker for five years (after about 25 years of smoking). The patient was on medication with dual antiplatelet therapy (ASA, Clopidogrel).
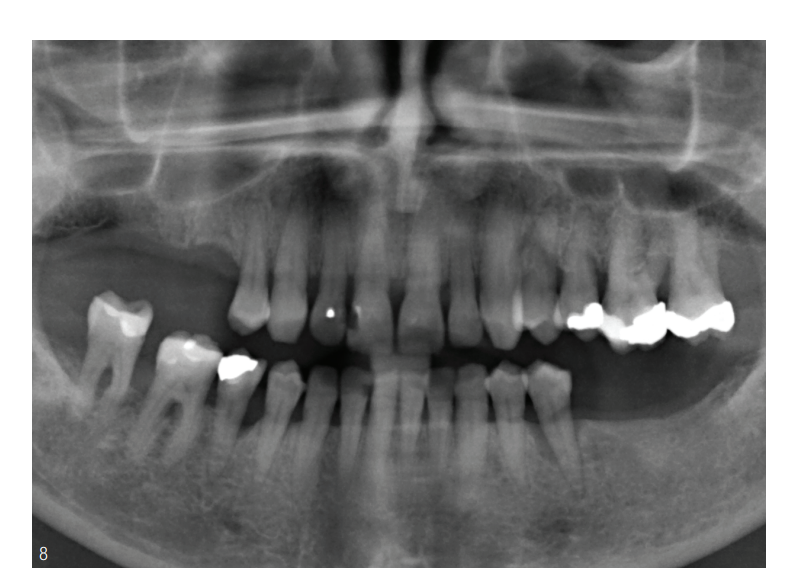
The reason for the presentation and her main concern was, in addition to tooth preservation, a fixed restoration of the free-end situation. At the time of the initial presentation, there was a conservatively periodontal and prosthetically insufficient dental situation (Fig. 7).

Initial findings at the start of anti-infective therapy
In the upper jaw, there is predominantly horizontal bone loss of 20 to 30 percent at the single-rooted teeth and a bone loss of 50 to 70 percent at the multi-rooted teeth. Tooth 24 showed a vertical collapse. In the lower jaw, teeth 35 and 45 exhibited a vertical bone collapse. Teeth 46 and 47 had discolorations in the bifurcation.
Clinically, the premolars showed degrees of mobility II to III, which were attributed to the loss of support zones in the first and third quadrants. Tooth 24 exhibited a mobility degree as well as a furcation degree III (Fig. 8).
Periodontal Diagnoses
According to the updated classification, the following diagnoses were made based on the assessment of the existing periodontal findings:
- localized moderate to severe chronic periodontitis (Staging III, Grading B)
- secondary occlusal tooth trauma on the terminal premolars due to a prosthetically insufficient restoration
Preliminary Prognostic Assessment
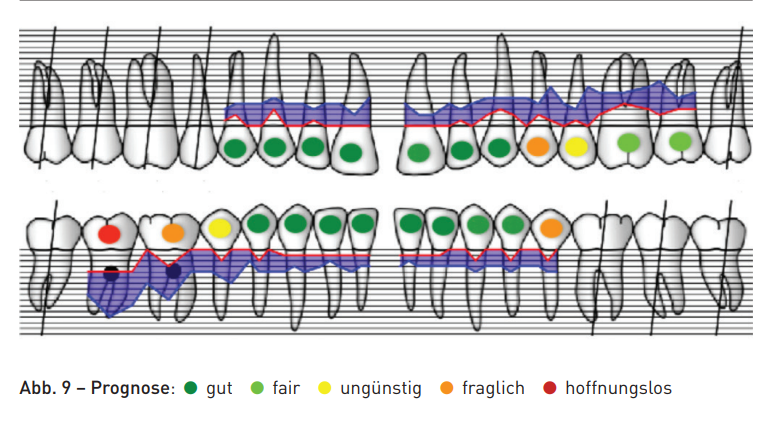
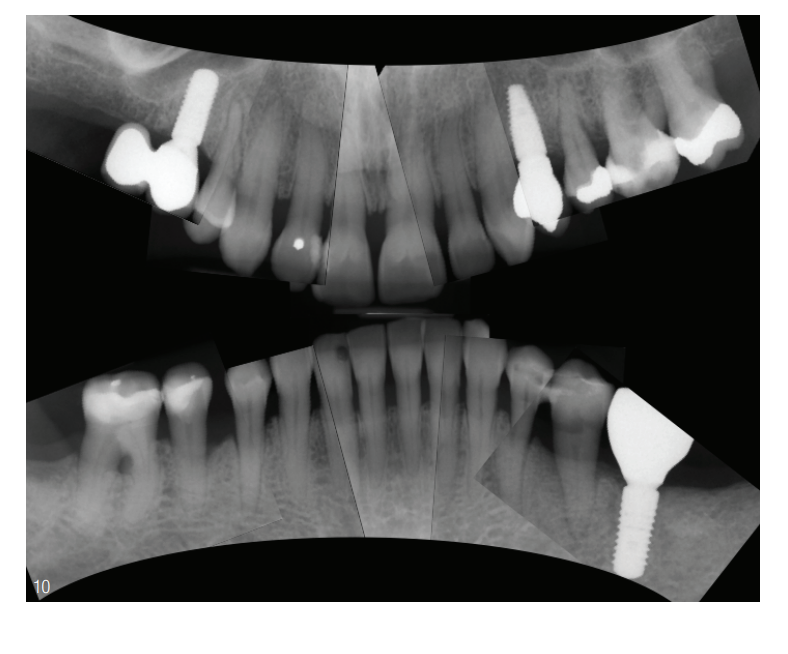
Based on the percentage of attachment loss, only tooth 47 had a hopeless prognosis due to its elongated position. Teeth 24 and 46 had a questionable prognosis due to furcation grade III, as did tooth 35 due to mobility grade III and advanced attachment loss (Fig. 9). The treatment plan aimed to stop the progression of the periodontal disease through systematic periodontal therapy. In addition to a regenerative therapy procedure (GTR 35 and 45), a fixed restoration of the unilateral free-end situations in the upper and lower jaw was planned (Fig. 10).
The planning included the following steps:
- anti-infective therapy with periodontal splinting on tooth 35 and extraction of tooth 47
- extraction of tooth 24 regenerative periodontal surgery in region 45 and tunneling of tooth 46
- regenerative periodontal surgery in region 35 with implantation in region 36
- implantation in region 15 and 24 implant-prosthetic restoration in regions 15, 24, and 36
Discussion
After completion of the anti-infective therapy, tooth 24 remained unchanged. Due to the increased degree of mobility, tooth 24 caused the patient daily discomfort, leading to the recommendation for extraction. Due to the furcation involvement and, as is typical for premolars, significant attachment loss, it could not be assumed that the situation would improve with a surgical intervention. To keep the number of implants as low as possible, the concept of a shortened dental arch was applied, and only edentulous areas were treated. Due to the bone loss, tooth 24 was replaced with an implant rather than a bridge. The initial recall interval of three months was extended to twice a year over time.
Case 3
A 51-year-old patient with an unremarkable medical history presented with concerns about spontaneous tooth loss. At this time, there was a conservatively and prosthetically insufficient dental situation. No periodontal therapy had been performed so far. The patient reported being a lifelong non-smoker. Tooth 42, the reason for the visit, exhibited a mobility grade III with a vertical component. Tooth 46 also showed a mobility grade III with a furcation involvement grade III. The response to the cold test was negative for both teeth. In the initial findings, the percentage of sites with ≥ 6 mm was 30 percent. In addition to a significantly reddened and edematously swollen gingiva, multiple sites (regions 15, 26, 36, 42) showed signs of suppuration. Hard and soft deposits could be identified in supra- and subgingival areas, which were associated with a pronounced periodontal inflammation situation (Fig. 11). Using the new classification of periodontal diseases, a periodontal disease stage III, grade A was present.

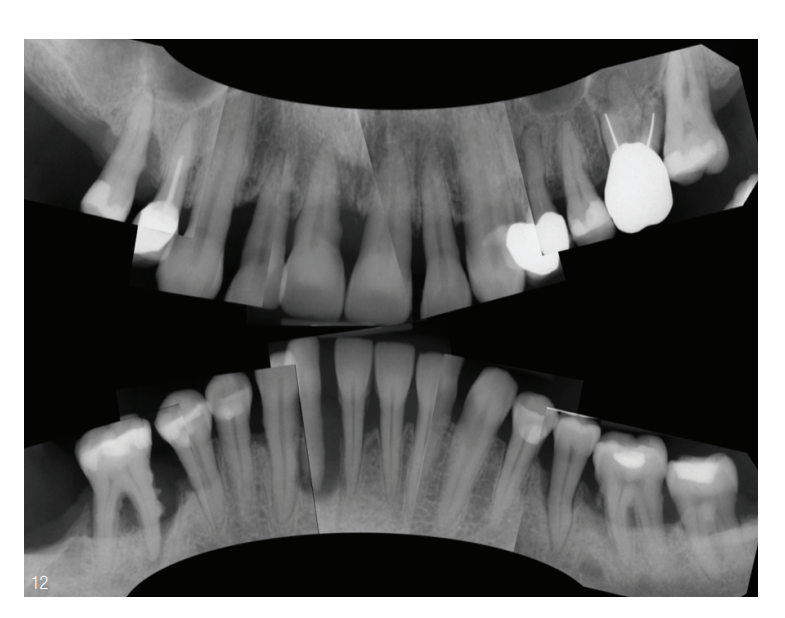
Clinical findings (November 2014) The single film status shows generalized horizontal bone loss between 30 and 90 percent in the upper jaw. Additionally, teeth 26 and 27 show intraradicular radiolucencies indicative of furcation involvement. Tooth 15 shows a vertical bone defect with calculus formation mesially. In the lower jaw, there is generalized bone loss between 10 and 50 percent, which is further characterized by vertical bone defects at teeth 37, 35, 42, and 46. Tooth 42 shows 100 percent bone loss at the mesial root surface with apical radiolucency. Furcation involvements were present at teeth 37 and 46 (Fig. 12).
Periodontal Diagnoses
According to the classification of the American Academy of Periodontology4, the following diagnoses were made after assessing the available findings:
- severe generalized chronic periodontitis (new classification Stage III, Grade C)
- Paro-Endo lesion on tooth 46
- Endo-Paro lesion on tooth 42
Preliminary Prognostic Assessment
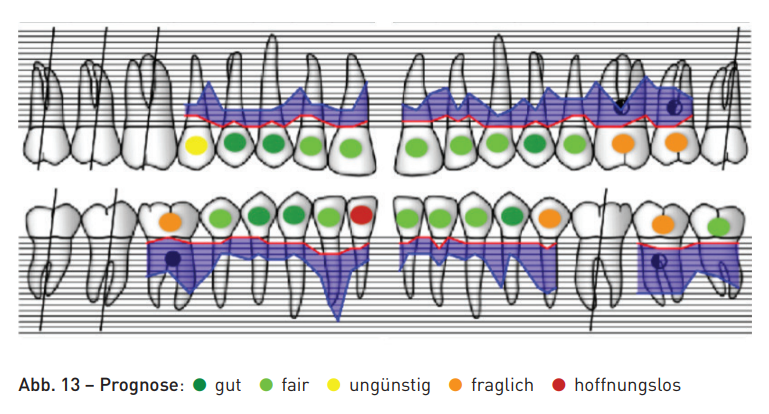
Tooth 42 was classified as hopeless due to the attachment loss reaching the apex. Teeth 26, 27, and 46 were classified as questionable due to furcation involvement and severe attachment loss. The initially determined hopeless prognosis for tooth 42 did not necessarily mean extraction in this case, but was primarily oriented towards the success of the anti-infective treatment (Fig. 13).
The planning included the following steps:
- periodontal pre-treatment (hygiene phase, periodontal splinting, and endodontic pre-treatment of teeth 42 and 46)
- anti-infective treatment (scaling and root planing with adjunctive antibiotic administration)
Periodontal Pre-Treatment
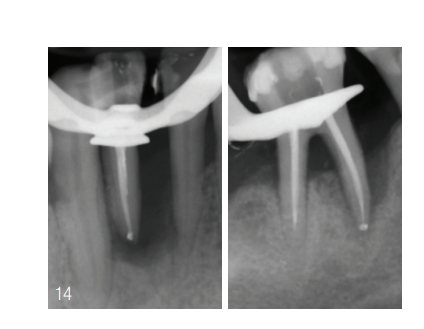
Initially, the patient was demonstrated the establishment of optimal oral hygiene (modified Bass technique, interdental brushes). Before the start of the endodontic therapy, teeth 42 and 43 were primarily bonded using adhesive technique and a fiberglass band. The endodontic therapy on tooth 46 was performed without primary bonding (Fig. 14).
Conservative Periodontitis Therapy The non-surgical periodontal treatment was performed with Gracey curettes and ultrasonic scalers in two sessions within 24 hours. After the completion of the second appointment, the patient was prescribed a combination of 500 mg Amoxicillin and 400 mg Metronidazole three times daily for seven days (van Winkelhoff cocktail).
First Reevaluation (three months) Within the first reevaluation period, the proportion of probing depths of ≥ 6 mm could be reduced from 30 to 13 percent. The degrees of mobility documented in the initial findings were decreasing for all teeth and were at a maximum of Grade I. By repeating the non-surgical treatment in areas with probing depths of 4 mm to 6 mm, further reduction could be achieved during the second reevaluation period.
After the completion of the non-surgical therapy phase, the following therapeutic steps were initiated:
- endodontic revision of teeth 24, 26
- partial resection and tunneling of tooth 26
- sinus floor augmentation in region 16 and periodontal regeneration at tooth 15
- prosthetic restoration of teeth 24, 25, and 26
- implantation in region 16 and implant-prosthetic rehabilitation
The anti-infective therapy was continued during the surgical phase as an accompanying treatment at three-month intervals.
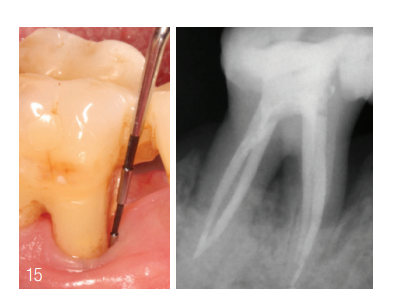
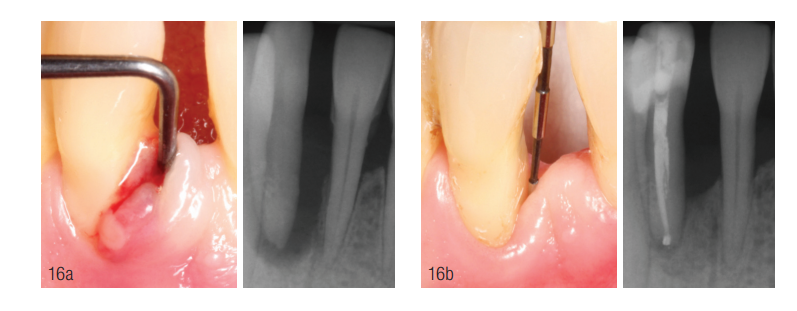
Periodontal follow-up During the surgical therapy phase, the sites with initial infraosseous components showed physiological ST. The formerly vertical periodontal defect on tooth 15, which was treated regeneratively as part of the sinus floor augmentation, showed clinically unremarkable ST and no signs of inflammation. The areas 33 and 36 also showed radiological signs of consolidation of the formerly vertical defects (Fig. 15). Twelve months after the start of the endodontic and anti-infective therapy, the radiological course showed signs of mineralization in the area of the former periodontal and endodontic defects of teeth 42 and 46 (Fig. 16).
Preliminary conclusion report
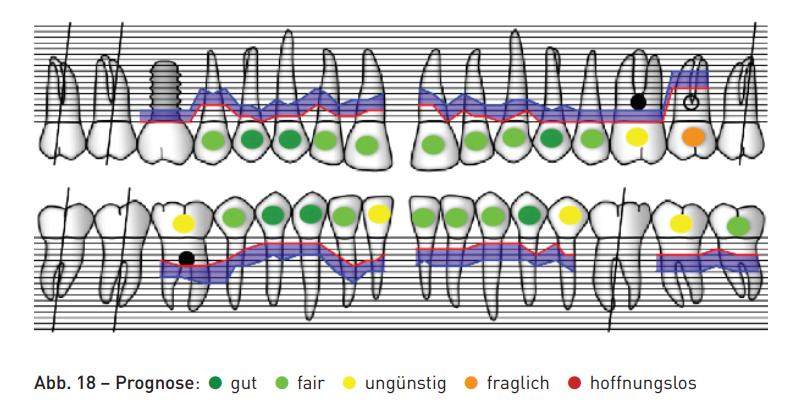
In the 27-month active therapy phase, the periodontal situation could be increasingly stabilized. Residual pocket depths of 4 mm and 5 mm were still present at tooth 27. The Grade III furcations at teeth 26 and 46 were tunneled and were cleaned by the patient with interdental brushes (Fig. 17). The individual tooth prognoses were improved through periodontal and endodontic measures during the active therapy phase (Fig. 18). The continuation of periodontal maintenance therapy was carried out at three-month intervals after the completion of active treatment.

Discussion
The preservation of primarily hopeless teeth is often very promising, provided there is no acute pain. Teeth with attachment loss, but without increased probing depths in direct proximity to implants, help avoid extractions. Especially mandibular anterior teeth can be preserved through endodontics and splinting without complications. Furcation involvement and bone loss up to the apex are, depending on the situation, not a direct reason for extraction.
Conclusion
The presented case presentations clearly show that a structured and interdisciplinary approach is particularly necessary for periodontally compromised patients. It can be noted that teeth initially classified as questionable stabilize during the course of anti-infective therapy and their prognosis improves. Especially in periodontitis patients, the maximum preservation of teeth is the priority. A closed dental arch should always be preserved if possible. Necessary extractions should therefore only take place after reevaluation. It becomes evident that for the treatment of these patients, often the involvement of all dental specialties is essential for a successful concept. In conclusion, implant therapy in stable periodontitis patients can be assessed as a complementary option with well-predictable results. Furthermore, implant therapy can help preserve teeth in the long term when tooth-supported dentures can be avoided.
