Tentpole Technique Supported by Cross-Linked Hyaluronic Acid
Machine translation
Original article is written in DE language (link to read it) .
The successful reconstruction of an atrophic maxilla using a modified GBR technique is presented. By stabilizing the bone particles with cross-linked hyaluronic acid and supporting the collagen membrane with several tenting screws, sufficient augment stability is achieved, allowing for the omission of the technique-sensitive application of bone blocks or shells. Furthermore, cross-linked hyaluronic acid promotes improved wound healing and significantly accelerates the bone healing of the slowly resorbing augment.
To enable an implant-supported restoration in the edentulous maxilla even in cases of severe atrophy, extensive augmentative measures are necessary. These fundamentally include either block grafts or the membrane-supported construction with particulate bone substitute material (guided bone regeneration, GBR).
The surgically easy-to-apply GBR technique is preferred by many practitioners. However, its effectiveness is limited, as the wound closure and the associated soft tissue pressure lead to an apical movement of the augment, resulting in incomplete filling of the defect. This phenomenon can only be circumvented by immobilizing the augment to create a stable space between hard and soft tissue. For this reason, procedures with "position-stable" augments are mostly used for a predictable treatment of these defects.
The best-documented methodology here is the use of autologous bone blocks, often in combination with a slowly resorbable biomaterial and a membrane.
Autogenous bone blocks have always been regarded as the material of choice for horizontal regeneration. However, the use of autogenous bone has disadvantages, such as limited availability and the need for time-consuming harvesting, with the risk of morbidity at the donor site and resorption at the recipient site.
Allogeneic bone blocks are often described as an equivalent alternative to autologous ones, but it is still unclear whether the expected success rates and long-term results are comparable.
To enable a less invasive and as complication-free as possible treatment concept for the patient, the GBR methodology with a particulate biomaterial and a suitable barrier membrane is recommended. However, appropriate measures must be taken to optimize the positional stability of the graft particles to ensure space maintenance and the supporting function of the membrane.
Tentpole Technique for Membrane Stabilization
The tentpole technique offers a minimally invasive treatment option that has primarily been used for the regeneration of vertical defects. Osteosynthesis screws can prevent membrane collapse due to the pressure of the flap, thus ensuring a stable space for regeneration. Augmentation can now be performed with a particulate bone substitute. A barrier membrane is used to cover the augment and osteosynthesis screw.
The author uses either so-called umbrella screws or osteosynthesis screws with a wide and flat head to ensure membrane stabilization and to avoid perforation of the membrane and the overlying flap. Nevertheless, there is still a fundamental risk of destabilization of the graft particles, especially when using a rapidly resorbable collagen membrane. This would lead to increased soft tissue pressure on the osteosynthesis screw, which would then perforate the gingiva over time, resulting in volume loss. For this reason, cross-linked hyaluronic acid is used, which serves both to mix the bone substitute and to "impregnate" the membrane.
Augmentation with Sticky Bone
The author uses a slowly resorbable biomaterial to ensure a volume-stable situation of the augmentation. Instead of the bovine treatment standard DBBM, a porcine bone substitute material (SMARTGRAFT, REGEDENT) is used, which also allows for high volume stability of the augmentation but integrates better into the new bone than bovine bone substitute material.
By mixing the porcine bone mineral with cross-linked hyaluronic acid (xHyA – hyaDENT BG, REGEDENT), a moldable paste is obtained that significantly improves the positional stability of the bone particles. Other advantages of hyaluronic acid, which shows a positive effect in all phases of wound healing, range from reduced swelling in the early phase, accelerated revascularization, to a significantly shorter healing time and a significantly better bony integration of the biomaterial.
It is also known that cross-linked hyaluronic acid slows down the degradation profile of native collagen membranes. The longer residence time of the membrane protects the augmentation material and the osteosynthesis screws from infiltrating soft tissue for a longer period.
The great potential of cross-linked hyaluronic acid in GBR was demonstrated in a recently published clinical study, where a lateral augmentation in the mandible was performed either with a classic GBR protocol using DBBM and a native collagen membrane or with a combination of DBBM/membrane and cross-linked hyaluronic acid. After six months, the xHyA group showed a significantly better volume gain (8 mm width gain vs. 4 mm). An analysis of the bone structure showed significantly more newly formed bone and significantly fewer residual particles of the avital KEM in the xHyA group.
Case Report
The 85-year-old patient presented with a severely pronounced pocket abscess in the region of 14/15. Both clinically and radiologically, there was a far-advanced periodontal destruction, which resulted in the removal of the teeth. Initially, we were rather cautious about the patient's desire for a fixed dental prosthesis due to the massive clinical inflammation and the very advanced bone loss. In addition, there was also a pronounced volume loss in the anterior maxilla (Fig. 1–4).


In the first session, the non-salvageable teeth 14 and 15 were extracted, and the patient was scheduled for the augmentative procedure four weeks later after soft tissue healing.
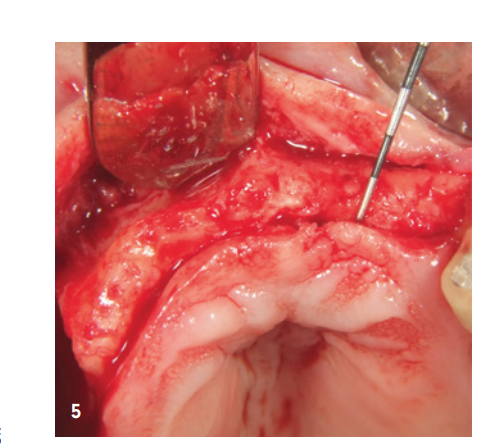
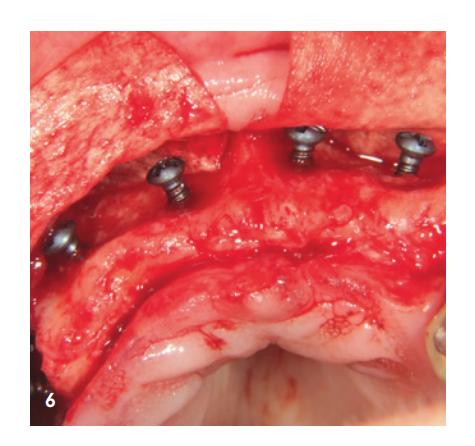
After local anesthesia, a crestal incision was made and a mucoperiosteal flap was prepared. There was pronounced bone atrophy in the form of a narrow bone lamella in the anterior area and a particularly pronounced bony defect in the posterior and sinus area of Q1 (Fig. 5). To obtain sufficient bony material for the planned restoration supported by four implants, a sinus lift and a lateral augmentation in the sense of GBR with barrier membrane and KEM were to be performed. For this purpose, a porcine KEM with a slow resorption profile (SMARTGRAFT, REGEDENT) was mixed with cross-linked hyaluronic acid (hyaDENT BG, REGEDENT) to achieve more precise augmentation and better position stability. To provide additional stability for the augmented area and support the collagen membrane, several tenting screws (USTOMED, length 8 mm, Ø 1.4 mm) were inserted (Fig. 6).
The anterior area was filled with xHyA-stabilized porcine bone mineral, covered with a native collagen membrane (SMARTBRANE, REGEDENT), and closed with horizontal mattress sutures in combination with single knot sutures to achieve a tension-free wound closure (Fig. 7). Due to the limited soft tissue availability in the posterior area of Q1, a complete wound closure was not desired to generate keratinized tissue through open granulation, the second phase of wound healing. For this reason, after filling the sinus and lateral augmentation, the defect was covered with a long-term stable sugar-crosslinked membrane (OSSIX Plus, REGEDENT). The membrane was not fully covered and was fixed with deep mattress sutures to ensure adequate stability (Fig. 8).
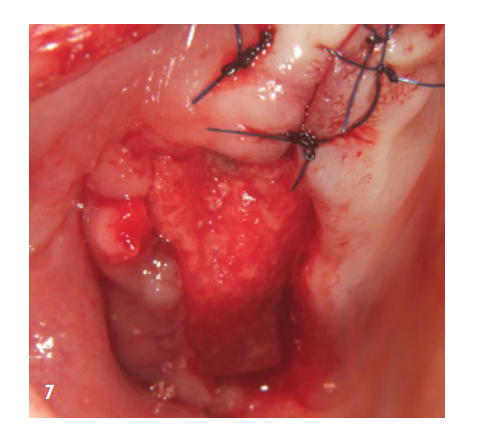
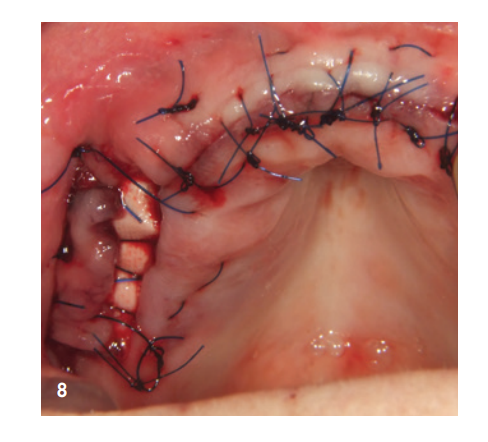
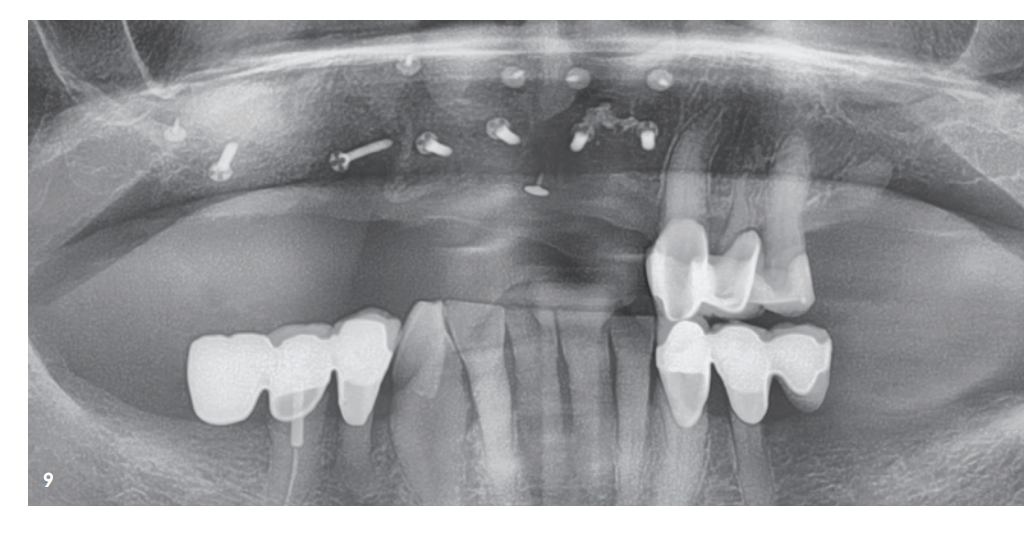
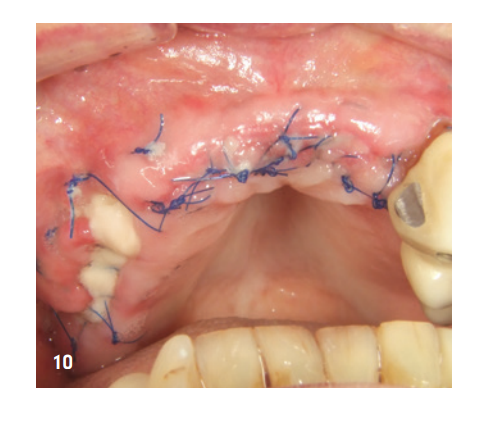
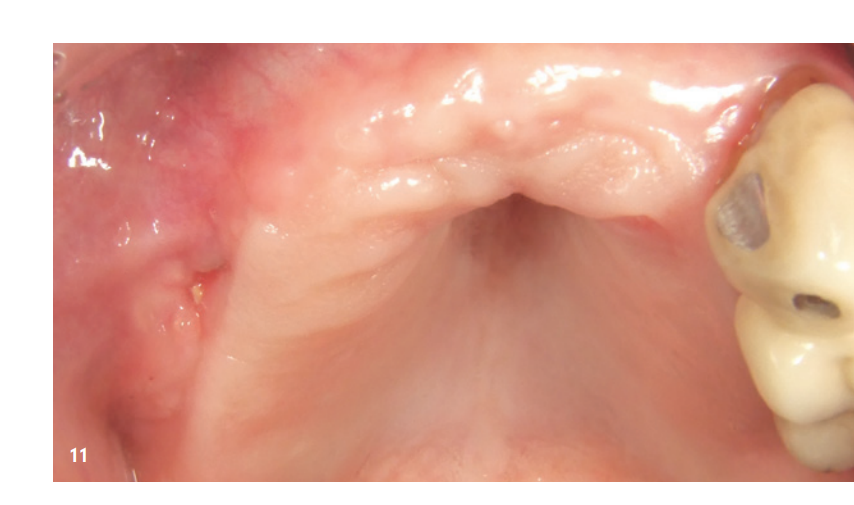
Figure 9 shows the X-ray image immediately after augmentation. The patient was informed postoperatively and was shielded with both antibiotics and analgesics. Antiseptic mouth rinse is recommended in our practice only from the third day post-op to avoid reducing fibroblast expression in the initial wound healing phase. Suture removal took place after ten days. There was good early wound healing, even in the area of the exposed membrane, which was already partially covered by secondary epithelialization (Fig. 10). The further healing phase proceeded without complications. After four weeks post-op, a non-irritated gingiva was observed, and the formerly exposed posterior area of Q1 was completely closed (Fig. 11).
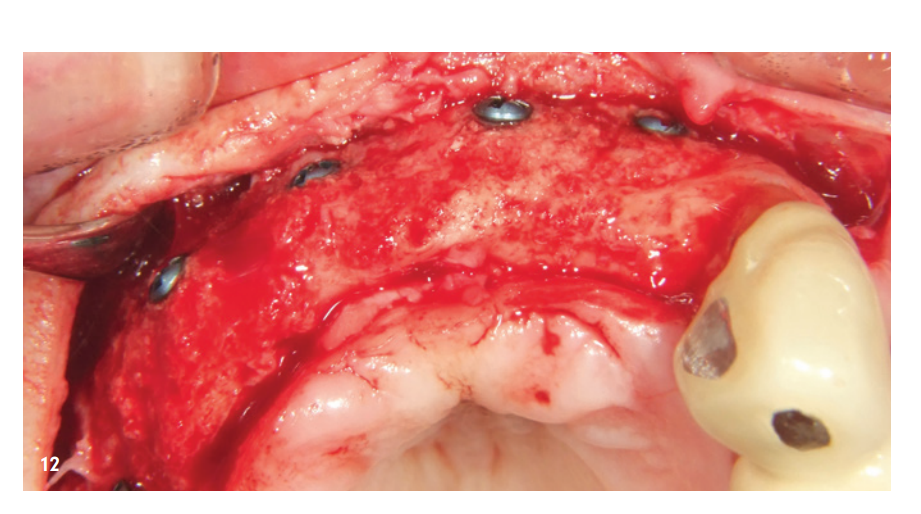
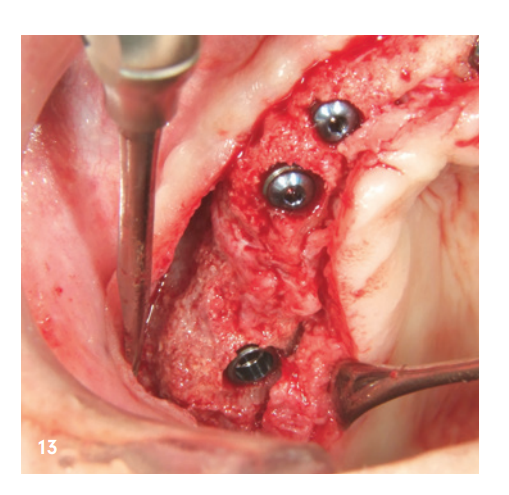
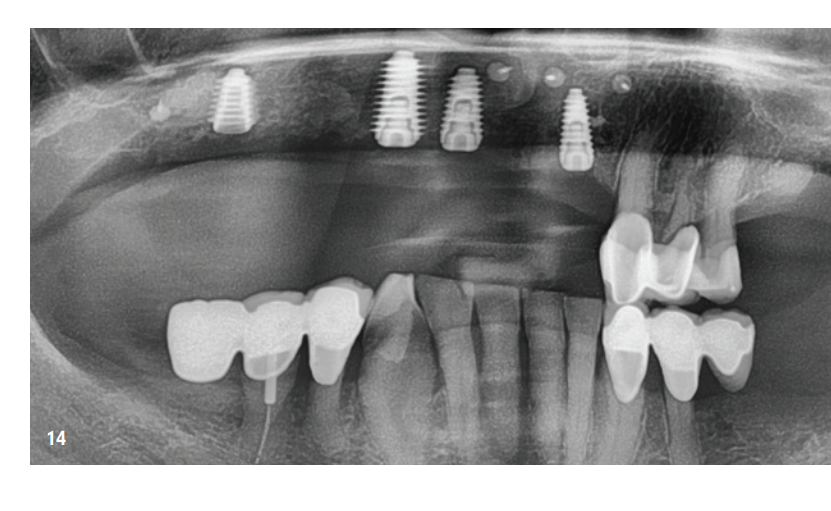
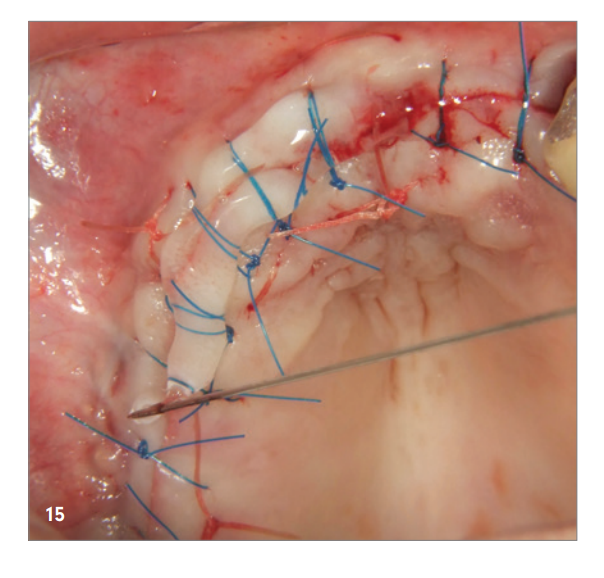
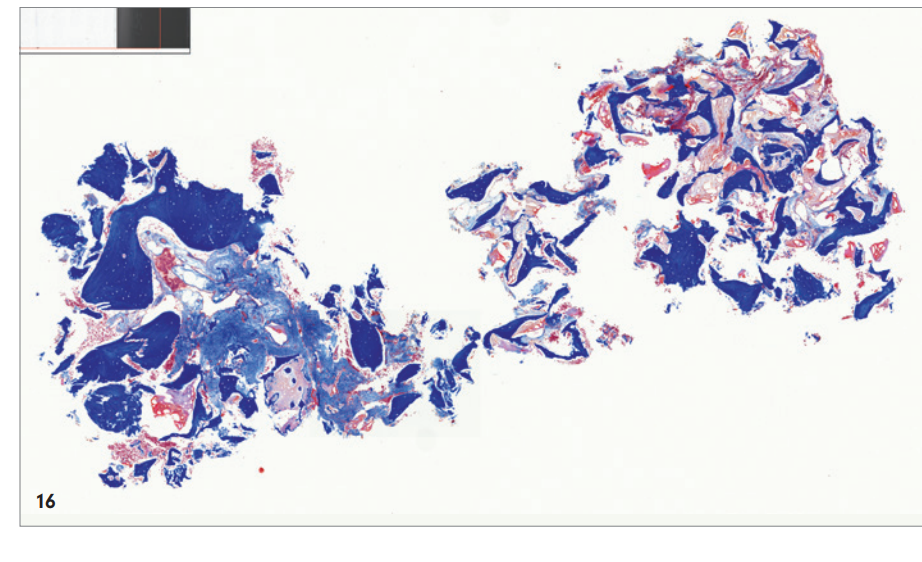
The reentry took place six months after bone augmentation. After the formation of a mucoperiosteal flap, an excellently consolidated jaw ridge was observed without signs of graft resorption. The volume was completely preserved up to the screw heads (Fig. 12). The screws could be removed without any problems, and the insertion of four implants (MegaGen AnyRidge) was possible in the correct position due to the sufficient bone availability (Fig. 13–15). A histological examination of a bone sample taken before implantation showed a very good bone structure, characterized by a high proportion of mineralized tissue, primarily consisting of newly formed bone (blue) and only a few residual particles of the graft material (red; Fig. 16).
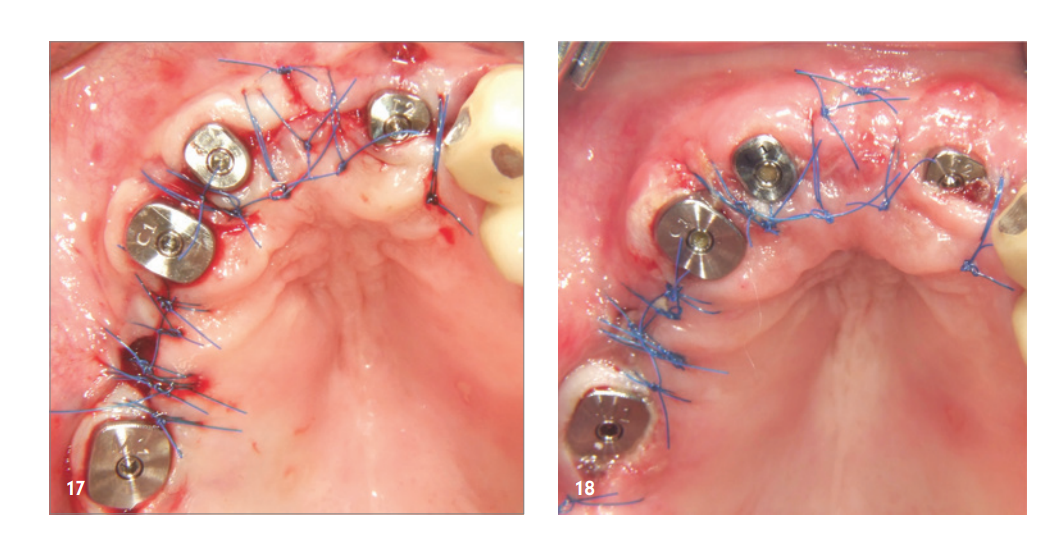
The healing process as well as the further care were unremarkable (Fig. 17–19). Figure 20 shows the clinical situation after the final restoration was placed.

Summary
By stabilizing bone particles with cross-linked hyaluronic acid and supporting the collagen membrane with multiple tenting screws, it is possible to reconstruct even complex augmentations and large defect situations using the GBR technique. This allows our patients to avoid additional bone harvesting or the use of allogeneic transplants (bone blocks or plates).
The advantages of this technique lie particularly in the volume stability of the augmented area and a significantly better integration of the slowly resorbing graft particles due to the cross-linked hyaluronic acid. Additionally, the reduction of swelling and the favored hard and soft tissue healing also reduce patient morbidity and postoperative risk.
