Non-surgical treatment of deep persistent periodontal pockets
Machine translation
Original article is written in DE language (link to read it) .
Abstract
Persistent inflamed periodontal pockets present a significant challenge in our daily practice, especially when non-surgical approaches fail. For both us as practitioners and our patients, surgical intervention is often undesirable. Through the so-called "Clean & Seal" concept, which can be applied within the framework of AIT or UPT, we have an additional non-surgical treatment option to avoid surgical periodontal therapy (CPT). The concept is based on the combination of subgingival instrumentation supported by a hypochlorite-based cleaning gel, which serves to better remove biofilm and granulation tissue. This initial cleaning step is followed by the application of cross-linked hyaluronic acid, which supports the healing processes and leads to the "sealing" of the cleaned wound site, thus protecting against reinfection.
Combination Treatment and the New PAR Guidelines
Periodontal diseases are characterized by a biofilm-induced inflammatory response that initially affects the periodontal soft tissue and subsequently also attacks the tooth-supporting apparatus. The formation of pathogenic biofilms is favored by deep pockets or furcations, ultimately increasing the risk of tooth loss.
In 2021, the German implementation of the EFP-S3 guideline for the treatment of periodontitis was carried out by the German Society for Periodontology e.V. (DG PARO; https://www.dgzmk.de/Die-Behandlung-von-Parodontitis-Stadium-I-bis-III).
The diagnosis is made according to the stages of staging and grading. Core elements of the stepwise therapy concept are active periodontal therapy (APT) and supportive periodontal therapy (UPT).
If the patient does not respond to non-surgical treatment approaches and persistent deep pockets with signs of inflammation remain, surgical treatment is usually planned to allow for more effective removal of biofilm and granulation tissue "under visibility." However, these periodontal surgical measures are also associated with some disadvantages. The CPT is invasive and therefore often undesirable for our patients. Additionally, they are technically demanding and time-consuming, and should therefore only be performed by experienced practitioners. Due to the recent reduction of the GKV budget, the significantly reduced remuneration for surgical approaches is not commensurate with the time and technical effort involved.
For this reason, we are always looking for effective adjunctive, non-surgical protocols for subgingival instrumentation. However, established protocols so far have not shown any significant advantage in improving probing depths and clinical attachment compared to instrumentation alone.
Non-surgical instrumentation of deep periodontal pockets
A successful periodontal overall concept can only be realized through control and removal of the biofilm. In the new guideline, thorough mechanical subgingival instrumentation of the affected pockets with hand and/or ultrasonic instruments is the core element. In selected cases, accompanying systemic antibiotic administration or the use of local adjuncts may be considered.
In our practice, we try to improve the efficiency of non-surgical periodontal treatment through two core elements, initially through more efficient subgingival instrumentation using suitable adjuncts. Afterwards, we attempt to reduce the risk of recontamination and improve healing processes by "sealing" the cleaned pocket.
We apply the so-called "Clean & Seal" concept. For this purpose, an adjunct to mechanical cleaning is a cleaning gel based on hypochlorite (NaOCl), which is buffered with a special formulation containing amino acids (PERISOLV, REGEDENT GmbH). Subsequently, the defect is sealed with a cross-linked hyaluronic acid (hyaDENT BG, REGEDENT GmbH) to prevent reinfection of the periodontal pocket and to promote periodontal healing at the cellular level.
The cleaning gel is a two-component preparation, consisting of a 0.95% NaOCl and an amino acid solution. Both components are mixed together immediately before use (Fig. 5). In in vitro studies, the gel showed positive antimicrobial properties, particularly against a biofilm consisting of periodontal pathogenic microorganisms. Furthermore, the gel has a degranulating effect, thereby supporting the mechanical instrumentation of the defect area. In medicine, comparable preparations are used for the successful topical treatment of chronic diabetic wounds and skin ulcers.
In subgingival instrumentation, effective debridement of the wound area and thus a statistically significant improvement in wound healing can be achieved through repeated treatment with the gel during a session. Due to the special composition, the subgingival application of the cleaning gel has a controlled effect on infected granulation tissue without significantly affecting the surrounding healthy tissue. A randomized controlled clinical study demonstrated that the adjunctive use of NaOCl gel led to a statistically significant improvement in periodontal measurement parameters. After six months, significantly fewer sites with increased probing values were measured in the NaOCl group compared to the control group, and fewer signs of inflammation (probing bleeding) were also recorded. In another clinical comparative study, the effectiveness of the cleaning gel was compared to that of chlorhexidine (CHX), which is commonly used in practice for subgingival irrigation. In the group treated with the cleaning gel, all clinical parameters (probing depth, BOP, and CAL) were significantly improved compared to the CHX group. The most pronounced effect was observed in the change of clinical attachment, which was statistically significantly better in the cleaning gel group than in the CHX group.
Connected Hyaluronic Acid (xHyA) for Sealing
Hyaluronic acid (HA) has the potential to support the healing process, especially in compromised situations, such as deep or inaccessible periodontal pockets. 1 g of hyaluronic acid can absorb up to six liters of water. This allows HA to immediately bind the blood, leading to faster formation of a clot and thus stabilizing the cleaned wound area. HA has a bacteriostatic effect and can reduce the re-colonization of bacteria at the wound site. In surgical applications, HA promotes angiogenesis and accelerates wound healing. Even in compromised wounds, such as those in diabetic patients, HA has a positive effect.
Therefore, it is not surprising that the application of hyaluronic acid after mechanical instrumentation improves periodontal parameters compared to SRP treatment alone.
A review with meta-analysis showed that the adjunctive administration of HA can achieve both an improvement in clinical attachment and probing depth in the weighted mean difference of all evaluated studies compared to instrumentation alone.
HA also improves local inflammatory parameters, characterized by a significant reduction in bleeding on probing (BOP) compared to SRP alone.
Potential of Combination Therapy Cleaning Gel/Cross-Linked Hyaluronic Acid
The positive effect of the adjunctive application of the "Clean & Seal" concept has already been clinically proven in both AIT and UPT.
In a controlled comparative study, patients in the context of AIT were treated either by instrumentation alone or supported with the "Clean & Seal" protocol.
Nine months after treatment, the "Clean & Seal" group showed significantly better periodontal parameters, characterized by a > 1 mm greater pocket reduction, a > 1 mm higher attachment gain, and a > 30% reduced occurrence of bleeding on probing.
In a clinical case series, deep inflamed persistent pockets were instrumented instead of the planned CPT, supported with the
“Clean & Seal” protocol was performed. A significant reduction in probing depth as well as clinical attachment loss of more than 2 mm was achieved.
Furthermore, the local inflammatory parameters could be significantly reduced from almost 100% to 40.1%.
Case Report
The patient presented to our practice with periodontal complaints (Fig. 1). The patient reported having undergone periodontal treatment in the past. Additionally, the patient expressed a desire for prosthetic rehabilitation. As part of a holistic treatment concept, non-salvageable teeth were extracted, and a combination of fixed and removable dentures was planned for both the upper and lower jaw.

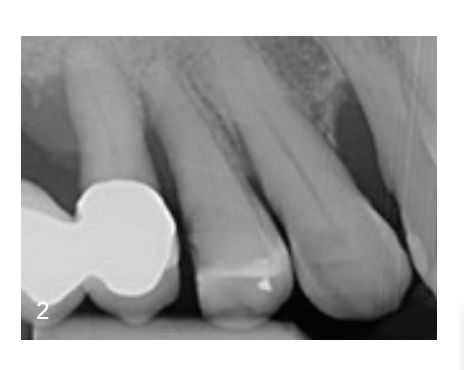
Periodontally, multiple deep pocket probing depths were observed. Particularly in the area distal to tooth 12, a pronounced radiologically visible bone loss was noted in combination with a probing depth of 7 mm and positive Bleeding on Probing (BOP) (Fig. 2 and 3).

We decided against a periodontal surgical therapy on the described tooth in the I. quadrant. Instead, we used the new non-surgical periodontal "Clean & Seal" procedure. As outlined in our protocol, a thorough scaling & root planing (SRP) was performed with hand and ultrasonic instruments under infiltration anesthesia and a concurrent application of the cleaning gel (PERISOLV, REGEDENT GmbH) to assist in biofilm removal. After mixing the two components (Fig. 4 and 5), the gel is introduced deeply into the pocket with a blunt cannula and after a contact time of about 60 seconds, mechanical scaling is continued. This procedure is repeated multiple times until no visible concretions emerge from the pocket. After completing the instrumentation, the pocket is filled with cross-linked hyaluronic acid (xHyA; hyaDENT BG, REGEDENT GmbH; Fig. 6) to promote the healing process (Fig. 7). The advantage of applying hyaDENT BG compared to enamel matrix proteins is that the wound site does not need to be dry or bloodless, and no conditioning of the root surface is required.




As part of a holistic approach, a subgingival instrumentation was applied in combination with the "Clean & Seal" concept both in the entire upper left quadrant and on other periodontally compromised teeth and implants with peri-implant inflammation. This was intended to significantly reduce the overall biofilm load and maximize the periodontal regeneration capacity. Subsequently, after the first three days following the therapy, cross-linked hyaluronic acid was placed into the deep pockets starting from a probing depth of 5 mm.
After a waiting period of six months, the findings were evaluated. Here, a significant reduction in probing depths and a resolution of inflammatory parameters could already be observed (Fig. 8 and 9). Furthermore, in the subsequent course, a beginning osseous healing was also evident radiologically, both around the formerly periodontally affected teeth and around the initially infected implants in the lower jaw (Fig. 8). Due to the success of the therapy using the "Clean & Seal" concept, the patient was spared a surgical intervention, and the dental prosthesis was successfully integrated. Figure 10 shows the radiological finding with significantly improved osseous consolidation of tooth 12 after twelve months.
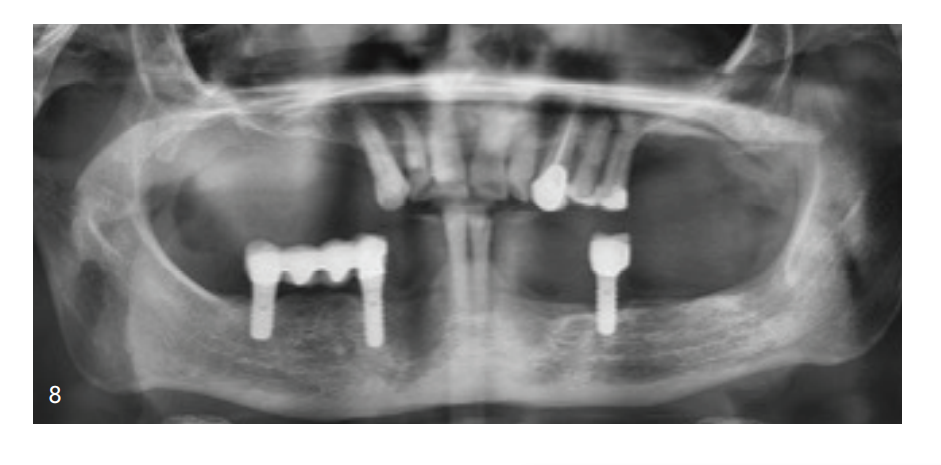

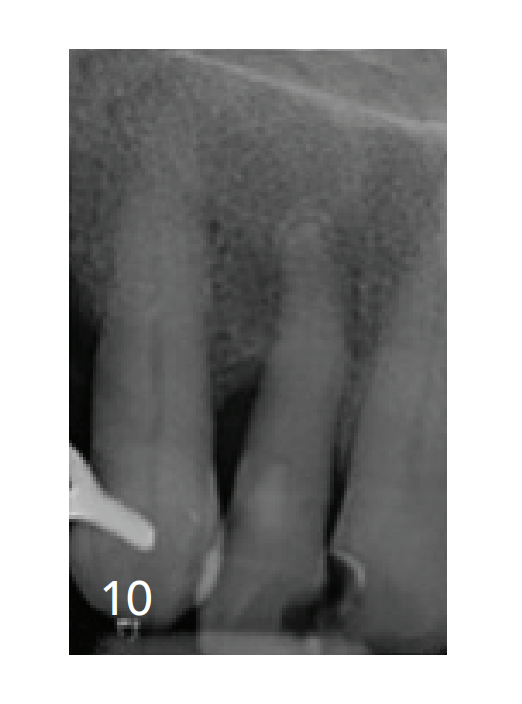
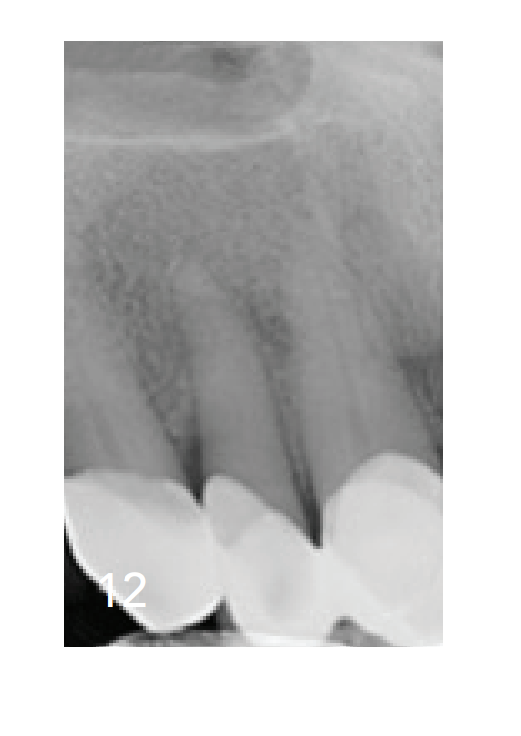
Even 18 months after "Clean & Seal," a stable periodontal situation is observed (Figs. 11 and 12). Continued low probing depths around tooth 12 of 3 mm and an almost complete radiological healing of the initial large-area defect. Additionally, a holistic view shows stable periodontal and peri-implant conditions. These are evident both clinically and radiologically.

Conclusion
The adjunctive use of a hypochlorite gel during closed subgingival instrumentation supports the mechanical removal of biofilm.
By subsequently sealing the wound area with cross-linked hyaluronic acid, wound area stabilization is improved, wound healing is accelerated, and regenerative processes for periodontal and peri-implant tissue regeneration are supported. This enhances relevant success criteria for a predictable regenerative treatment outcome in complex defects and further expands and optimizes the therapeutic spectrum of our non-surgical periodontal therapy.
Authors: Alexander Müller-Busch, Frederic Kauffmann
