Non-surgical treatment of an inflamed peri-implant defect
Machine translation
Original article is written in DE language (link to read it) .
The non-surgical treatment of periodontal and peri-implant defects through mechanical instrumentation in combination with a sodium hypochlorite cleaning gel and the subsequent application of cross-linked hyaluronic acid in the cleaned wound area represents a minimally invasive first therapy option for severe periodontal and peri-implant defects in general.
Introduction
The main cause of periodontitis and peri-implant diseases is the accumulation of a pathogenic biofilm in the pockets around the teeth or implants, which often leads to uncontrolled tissue resorption.
The first step and core element for successful removal of the biofilm is the subgingival instrumentation of the periodontal or peri-implant pocket. In clinical practice, very predictable results can be achieved for mild to moderate periodontal defects. For severe periodontal and peri-implantitis defects in general, the treatment success is significantly lower. In particular, the implant surface has a thread structure that is difficult for instruments to access, as well as a microstructured surface that cannot be cleaned with classical hand instruments. Therefore, unfortunately, the less invasive non-surgical therapies often do not lead to a lasting improvement of the local inflammation in most cases (Renvert 2015).
This can, if at all, only be achieved through invasive surgical procedures involving flap preparation and cleaning of the tooth or implant surface (Schmidlin 2012, Renvert 2009, Almohandes 2019).
In addition to resolving local inflammation, we ideally desire regeneration of the bone defect and restoration of the periodontal ligament or reossification of the implant for long-term success of the treatment (Almohandes 2019).
As of today, no treatment standard has emerged for the management of peri-implant defects. Typically, peri-implantitis therapy is carried out through a multi-step treatment sequence (Smeets 2014).
Cleaning and Decontamination
The greatest challenge lies in the successful removal of the biofilm and the infected granulation tissue present in the pocket. In a non-surgical approach, complete cleaning of the implant surface and the peri-implant defect filled with infected granulation tissue is not achieved through mechanical instrumentation alone. The addition of chemical adjuncts also has no significant impact (Koo 2019, Stavropoulos 2019, Mordini 2021).
For this reason, the best results are generally achieved through surgical visualization of the defect and careful, multi-stage cleaning through mechanical instrumentation under direct vision (Heitz-Mayfield 2014, Schwarz 2015).
We use an adjunct to non-surgical instrumentation of periodontal and peri-implant defects, a cleaning gel based on sodium hypochlorite (NaOCl, PERISOLV, REGEDENT). It consists of a 0.95% NaOCl solution, which is buffered with an amino acid solution before use.
The cleaning gel effectively removes biofilm (Jurczyz 2015), both on dentinal and on rough implant surfaces (Bach 2016).
Another advantage of the gel is its degranulating property. This improves the cleaning of the infected pocket and especially the complex implant surface (Bach 2016).
Due to its special composition, PERISOLV® specifically targets degenerated infected tissue structures. The gel is well tolerated and no longer has the tissue-irritating properties known from hypochlorite alone.
In the treatment of periodontal and peri-implant bone defects, multiple applications of the gel during mechanical instrumentation are recommended. This can improve the cleaning of the infected pocket and especially the implant surface.
In the treatment of periodontitis, the adjunctive use of the cleaning gel during non-surgical treatment of periodontal pockets results in a statistically significant improvement in all measurement parameters (TST, CAL, BAS) (Iorio-Siciliano 2021).
The same applies to the closed treatment of peri-implant mucositis (Iorio-Siciliano 2020). The incidence of probing bleeding (BAS) was reduced by 70 percent after one month (compared to 53 percent in the control group without gel application). Unfortunately, this promising short-term result could not be maintained in either group. After six months, only 45 percent of the implants in the gel group and 32 percent in the control group showed no signs of inflammation.
To avoid reinfection of the pocket, we use special biologics after instrumentation. This aims to promote faster healing and "seal" the pocket to prevent recontamination with biofilm.
Support for Wound and Soft Tissue Healing with Cross-Linked Hyaluronic Acid
Hyaluronic acid (HA) accelerates all healing processes, which can be crucial for treatment success, especially in compromised situations such as periodontal and peri-implant defects. HA can stabilize the wound area, as it immediately binds the blood in the defect space after application due to its strong "adhesive effect" (1 g of HA can absorb up to six liters of water; Rajan 2013). In particular, cross-linked hyaluronic acid exhibits a pronounced bacteriostatic effect, thus protecting the wound area from recolonization by microorganisms (Carlson 2004, Zhu 2024).
Hyaluronic acid significantly improves all healing processes: it leads to faster neoangiogenesis post-op and shortens wound healing (Yildirim 2017, King 1991). Furthermore, HA stimulates true periodontal regeneration (Shirakata 2021) and even accelerates bone regeneration (Alcantara 2018, Stiller 2014). The combination therapy of the adjunctive use of sodium hypochlorite cleaning gel and cross-linked hyaluronic acid ("CLEAN&SEAL") shows superior results in the treatment of periodontal pockets compared to instrumentation alone. This has been demonstrated both in the use of AIT (Ramanauskaite 2023) and in UPT for the treatment of deep residual periodontal pockets (Benyei 2024). Thus, the transfer of the concept to the non-surgical treatment of peri-implant defects is a logical step.
Case Study
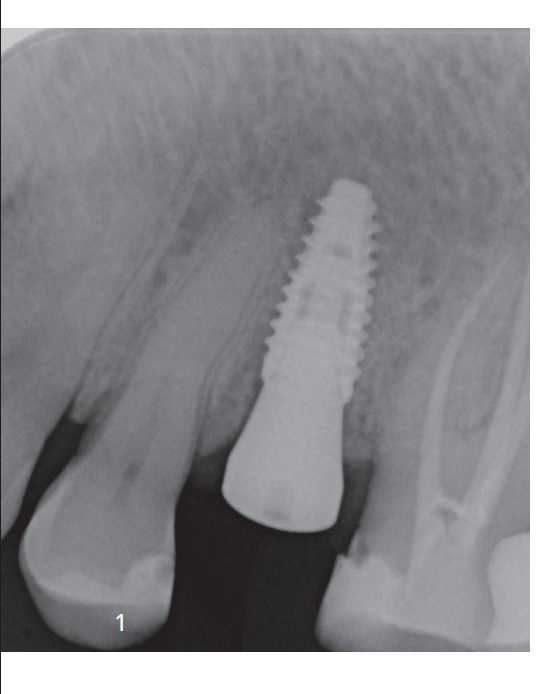
The patient presented to our practice regarding implantation and the desire to close the gap in region 24. According to the patient, the tooth extraction with simultaneous augmentation took place about twelve months ago. The bone quality during implantation was very good, and an implant could be inserted with primary stability without further augmentative procedures (Fig. 1). We opted for a transgingival healing process to shape the soft tissue at this stage and spare the patient another surgical procedure. The initial wound healing occurred without any particularities. During the follow-up treatment, combined with the patient's feedback, we noticed both clinical and radiological problems after three months. The patient reported a bad taste and a swollen gum area. Clinically, we observed increased probing depth (PD) and positive bleeding on probing (BOP) (Fig. 2).

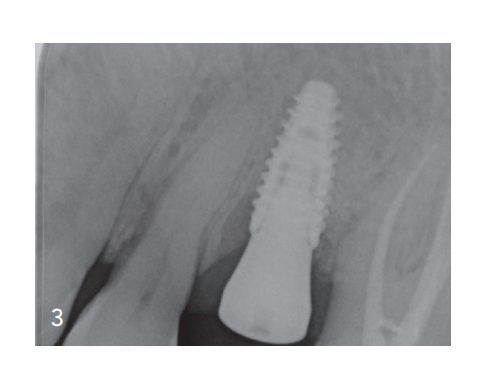
X-ray examination showed significant bone loss (Fig. 3). Especially in the early phase of treatment, this finding poses great challenges for us. One option would be explantation with subsequent bone reconstruction, which would mean further surgical procedures, time, and possibly additional costs for the patient. Another option is to leave the implant in place and perform augmentation of the existing defect. However, this seemingly "easier" path also entails another surgical procedure for the patient, and unfortunately, there is still a high risk that this augmentation will fail in the inflamed peri-implant region.
Instead, we opted for the minimally invasive and innovative treatment approach described above (CLEAN&SEAL).
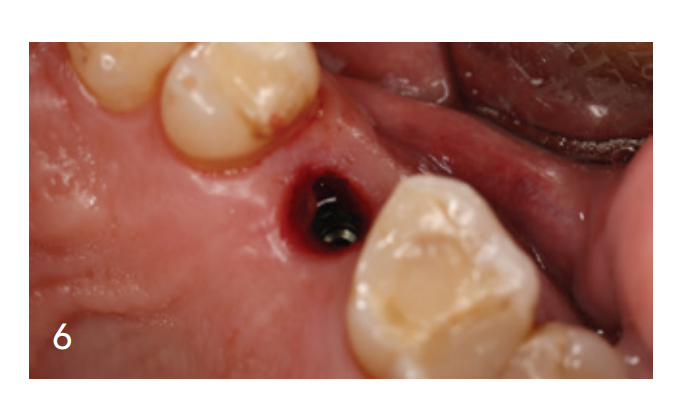
In just one treatment session, after the removal of the gingiva former, the cleaning solution (PERISOLV) was applied (Fig. 4). The exposure time and application were carried out according to our cleaning concept. Figure 5 shows how the granulation tissue detaches and the inflamed areas are cleaned. The granulation tissue can be very easily removed mechanically after application. After multiple applications and extensive repetition of the instrumentation, we found a cleaned peri-implant area (Fig. 6). The wound area was filled with a cross-linked hyaluronic acid (hyaDENT BG, REGEDENT) and then sealed with the cleaned gingiva former (Fig. 7 and 8). After four months, a completely healed bone defect is evident radiologically (Fig. 9). Clinically, a healed, inflammation-free soft tissue situation is observed, along with reduced TST and absence of BAS (Fig. 10).




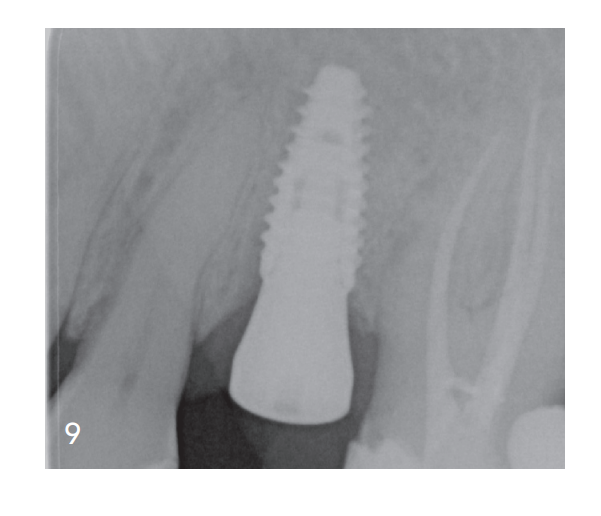


Through the minimally invasive and innovative treatment concept, a renewed surgical intervention and possible explantation could be avoided. The implant could be saved and the peri-implant bone level could be completely restored through a non-surgical peri-implantitis therapy.

