Delayed immediate implantation with volume-stable augmentation
Machine translation
Original article is written in DE language (link to read it) .
Implants placed simultaneously with an augmentation show a high survival rate. By filling smaller bone defects around implants with bone substitute material, the exposed implant surface can be significantly reduced, and the treatment time for our patients can be considerably shortened.
Barrier membranes can further improve the outcome of the augmentation of smaller bone defects with bone substitute material around the implant. Nevertheless, the classic augmentation concept, consisting of slowly resorbable bovine bone substitute material (KEM) and a rapidly resorbable native collagen membrane, carries a certain residual risk. It is often unclear to what extent complete defect regeneration can be achieved with this treatment approach.
From the treatment of extraction sockets with greater bone resorption (such as a deficient buccal plate), it is known that augmentation with slowly resorbable KEM and/or a native barrier membrane often leads to insufficient bony integration of the graft particles.
Furthermore, there are indications from the literature that during wound closure and the associated soft tissue pressure, there can be an apical movement of the augment and thus an incomplete filling of the defect.
A multicenter study showed that dehiscence defects around implants augmented with a slowly resorbable bovine bone substitute material and a native collagen membrane could only be filled on average by 55% in height and 70% in width. In further follow-up of the patients in this study, it was found that implants with residual dehiscences of > 1 mm after augmentations have a higher risk for peri-implant diseases than implants without residual defects. Implants with bony residual defects also showed more frequently soft tissue recessions, which can significantly compromise the aesthetic outcome.
Due to the aforementioned possible problems, we have adjusted our augmentative concept for simultaneous implantation with buccal contour augmentation as follows:
We fundamentally use adjunctively cross-linked hyaluronic acid (xHyA) as a wound healing accelerator for the "biologization" of the augmentate.
It is now known from the literature that xHyA leads to accelerated bone healing. When mixing particulate bone substitute material or autologous bone with xHyA, a pleasantly applicable and position-stable paste ("Sticky Bone") is created, which is comparable to that made from blood centrifugates.
Furthermore, the longevity of collagen membranes can be extended with xHyA. This allows augmentations to be planned more predictably and reduces treatment duration. Less swelling and reduced patient morbidity within the critical first seven days of the healing process are a pleasant side effect of hyaluronic acid.
Instead of bovine bone substitute material, we use bone material of porcine origin. Due to its greater porosity while maintaining high volume stability, it has a significantly higher remodeling rate than bovine preparations. To cover the augmentate, we use a porcine pericardial membrane with a significantly extended resorption profile compared to a classic native collagen membrane, thereby reducing the connective tissue encapsulation of the graft particles.
Case Report
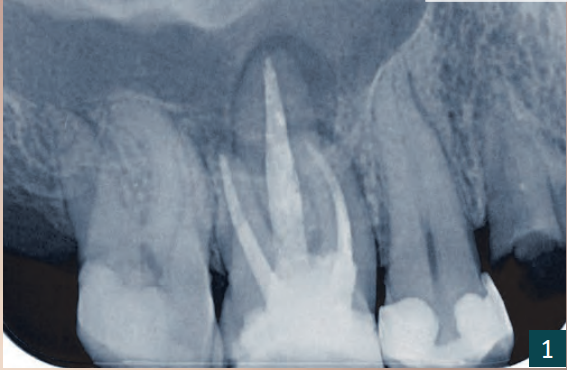
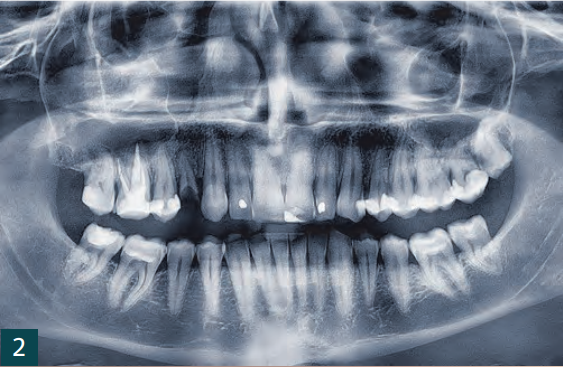
The 37-year-old male patient presented for the first time in our practice regarding the fractured tooth 14 in the upper jaw (Fig. 1, 2). He showed an unremarkable general medical history. In the specific dental examination, risk factors such as existing periodontitis and a positive smoking history were identified.
The patient expressed the desire for tooth extraction followed by prosthetic restoration. After weighing the prosthetic options, it was decided to proceed with an implant-supported restoration.
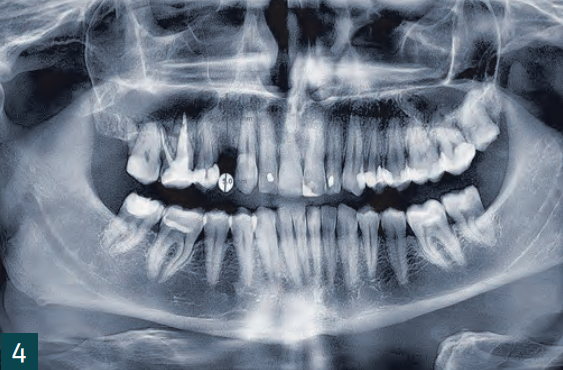
Since a possible apical infection at the fractured tooth 14 could not be ruled out, we opted for a delayed approach. As the first step, the root remnant was removed while preserving maximum hard and soft tissue (Fig. 3-5).


Implant Insertion
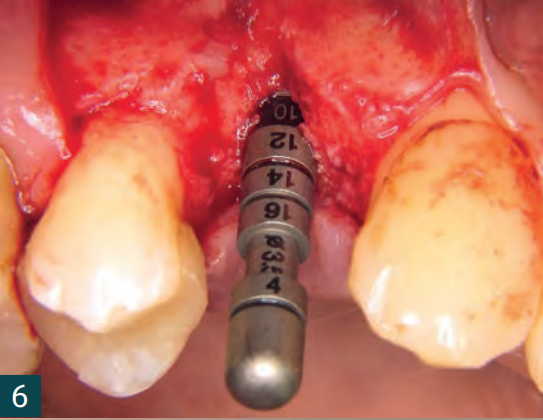
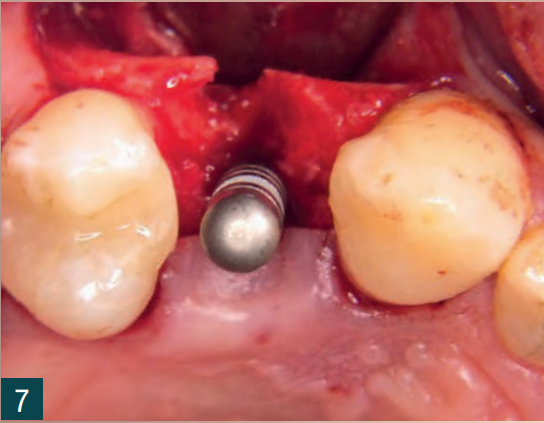
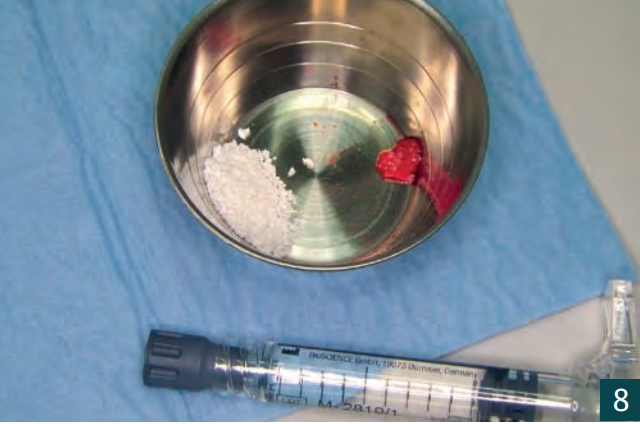
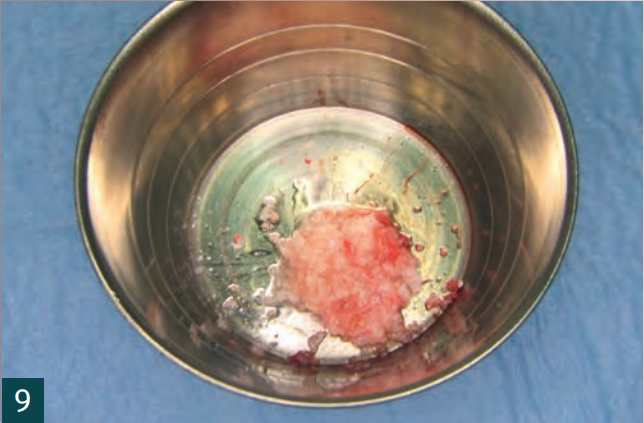
Eight weeks after the extraction of the tooth, the implant was inserted as part of a delayed immediate implantation (BL, ø 4.1 mm RC, SLA 12 mm, Roxolid, Straumann). The incision was made crestally with a single, C-shaped vertical relief incision extending distally (Fig. 6). Bone-wise, there was a deficient bone supply buccally. The implant could be inserted with primary stability into the existing bone (Fig. 7). The autologous bone collected during the preparation of the implant bed was mixed with the bone replacement material (Smartgraft (0.25 – 1.00 mm / 0.5cc, Regedent GmbH) (Fig. 8). The existing bony defect was augmented using "Sticky Bone" and covered with a porcine membrane (Smartbrane 15 mm x 20 mm, Regedent GmbH) (Fig. 10, 11). The Sticky Bone is created by adding cross-linked hyaluronic acid (hyaDENT BG, Regedent GmbH) to the bone replacement material and is characterized by significantly increased graft stability (Fig. 9).


Subsequently, the wound edges were adapted with a mattress suture and primarily closed with interrupted sutures (4-0 Biotex, Regedent GmbH) (Fig. 12).

Suture Removal
At the time of suture removal after seven days, the patient showed a wound dehiscence – presumably due to his heavy tobacco consumption (Fig. 13). Due to the otherwise unremarkable, stable condition and the already beginning granulation of the exposed area without any particle migration, surgical intervention was not performed. The patient was instructed to use a disinfecting mouth rinse and to avoid mechanical trauma.

The healing process was good (Fig. 14), at the second follow-up appointment 14 days postoperatively, the wound was completely closed (Fig. 15).


Exposure
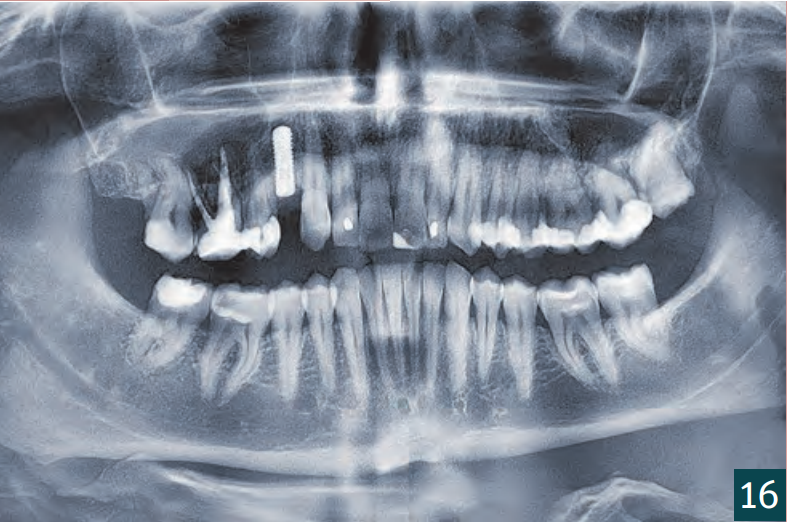
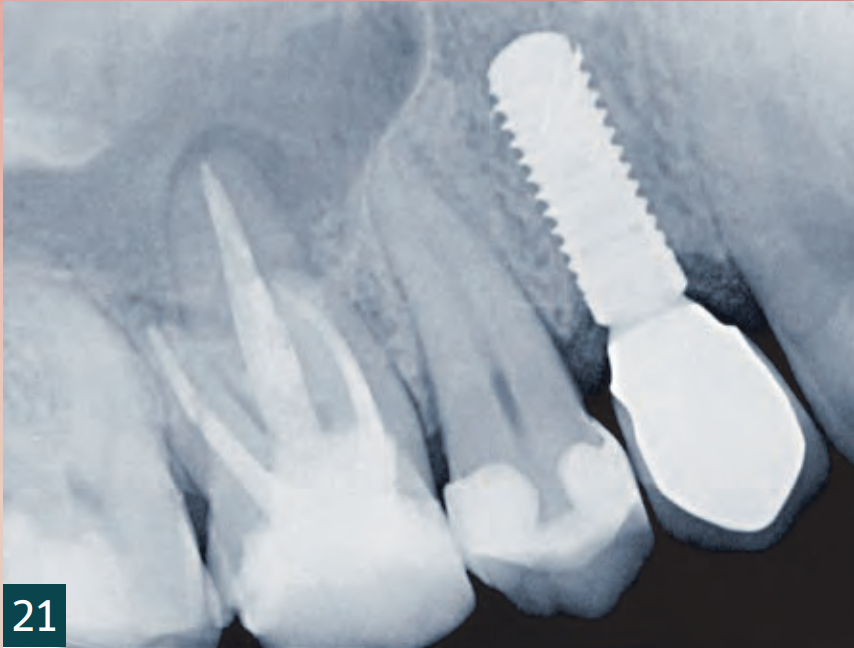
The exposure and placement of a gingiva former were performed after four months (Fig. 18). Due to delayed wound healing, the augmented area was exposed to check the bony result. A crestal incision was sufficient for this, which was subsequently closed again with two single-button sutures (5-0 Seralene, Serag Wiessner). A completely bony regenerated augment was observed without volume loss. Particularly in the critical crestal aspect, sufficient bony coverage of the implant was achieved despite the dehiscence (Figs. 16-18). The definitive restoration was performed five months after implantation with an occlusally screwed crown (Figs. 19-21).




Summary
Implants that are inserted in combination with an augmentation have a high survival rate; however, in practice, a complete defect filling is often not achieved. This increases the risk of peri-implant inflammation. The additional use of hyaluronic acid leads to better defect filling, as it achieves higher stabilization of particulate graft material, a reduction in postoperative swelling, and faster bone and soft tissue healing.
