Soft Tissue: Differences - Optimization - Influence
Machine translation
Original article is written in DE language (link to read it) .
Without functioning soft tissue, problems and pain are preprogrammed. That soft tissue is not just soft tissue is shown by a simple, almost untrained look into the oral cavity: tongue, cheek, palate, everything looks different, has a different structure and different functions. But every soft tissue usually heals quite well. Transplants are possible. The soft tissue protects the bone, but without bone, the soft tissue is also worthless.
There are numerous ways to distinguish and describe the different types of tissues in the mouth. However, the most important difference is whether the soft tissue is “attached,” meaning fixed/stabilized, or not “attached” and mobile. Other parameters for distinguishing soft tissue include keratinization, thickness, texture, or generally the phenotype. As important as the quality and quantity of soft tissue is, we desire attached soft tissue around teeth and especially around implants. Whether this is ultimately keratinized or not is secondary, as long as the soft tissue is attached.






Soft tissue around teeth
The emergence profile of the teeth through the soft tissue is characterized by the sulcus and the usually firm gingiva that directly adheres to the tooth. This runs in a scalloped shape and, depending on the phenotype, shows either four or triangular teeth. The highest point of the gingiva is the papilla, which fills the interproximal space. The lowest point is usually near the center of the tooth crown and slightly displaced distally. Further apically, the unattached gingiva can be found, which is separated from the attached gingiva by the mucogingival junction (MGJ). The MGJ is particularly important for the classification of recessions and, in the case of recession coverage, for the selection of the optimal coverage technique.
The soft tissue around teeth should not be too prominent when laughing (Gummy Smile), but still visible to a sufficient extent.
Soft Tissue Around Implants
For aesthetic requirements, the same rules apply to implants as to teeth. A thicker phenotype is desirable, as it is more resistant to recessions and external influences. As much as we assumed that optimal soft tissue has a direct positive impact on the incidence of peri-implantitis, it is all the more disappointing that this is not the case. Ideal soft tissue around implants positively affects plaque and bleeding indices. The soft tissues benefit, but there is no direct influence on the bone.
If a modification of the soft tissue is necessary, it is less important whether the modification took place before, during, or after the bony augmentation. What is crucial is that the soft tissue optimization is as complete as possible at the time of crown provision, as later interventions carry a higher risk of failure.
Optimization of Soft Tissue
The optimization options for soft tissue around teeth and implants are diverse: from tried-and-true methods, such as connective tissue grafts (CTG) or free mucosal grafts (FMG), to various densities of collagen matrices or techniques that rely solely on enamel matrix proteins or hyaluronic acid.
The optimization of soft tissue is not comparable in any way. Even if somewhat similar techniques are used, the conditions and success rates vary greatly. If one must work around teeth with the given situation, which can only be maximally altered through orthodontic therapy, a situation should be created around implants that ideally does not deteriorate.
Techniques
Whether standardized recession coverage using classic or modified tunnel techniques or coronal advancement flaps – connective tissue grafts or substitute materials have proven to be advantageous for this application. Although the gold standard remains the autologous graft, the results with these techniques around teeth are stable over a long period of several years, provided that the primary healing was successful. Often, the initial situation is crucial for this. The more unfavorable it is, the more likely it is that complete coverage cannot be achieved.
If the outcome around teeth is well predictable, the success rates for recession coverage around implants are significantly worse. Even with the use of autologous grafts, recessions around implants cannot be reliably covered. For this reason, thorough preparation is essential.
Another technique that is unjustly labeled as very invasive is the free mucosal graft. The indication for this technique can be reduced to a few situations: on the one hand, the anterior mandible with recessions around teeth, with a rather thin phenotype and lack of attached gingiva, and on the other hand, in situations without attached mucosa around implants in the mandible before or after prosthetic treatment. In the maxilla, the lack of attached mucosa can usually be established through a flap procedure during the exposure.
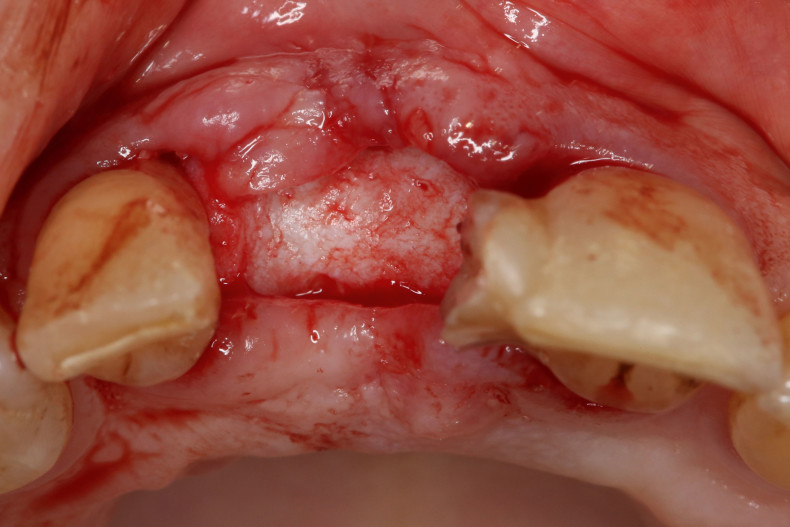
In all cases, autologous grafts are harvested from the palate. There are two basic techniques available for obtaining a BGT: harvesting as a subepithelial graft, e.g., through a single incision or trap-door technique, as well as as a FST, which is then deepithelized. However, the tissues obtained in this way differ significantly from each other.
Subepithelial Graft
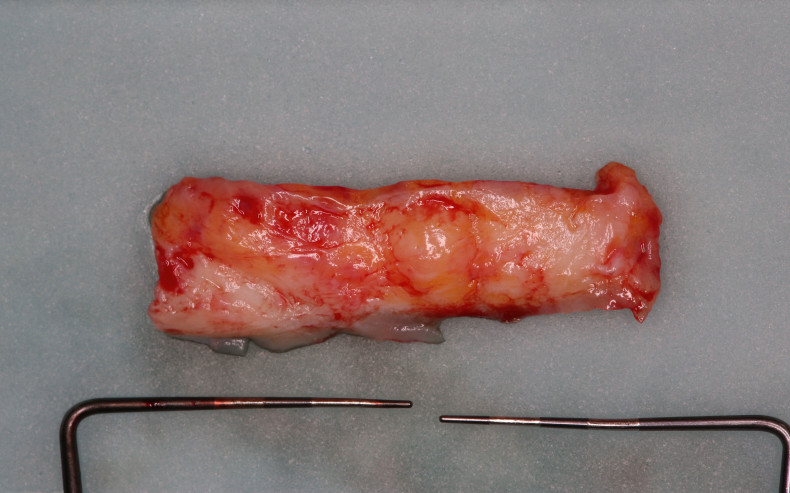
In the deeper layers, glandular and adipose tissue can be found, which are clearly visible in the harvested graft and often make up a large part of the graft.
De-epithelized FST
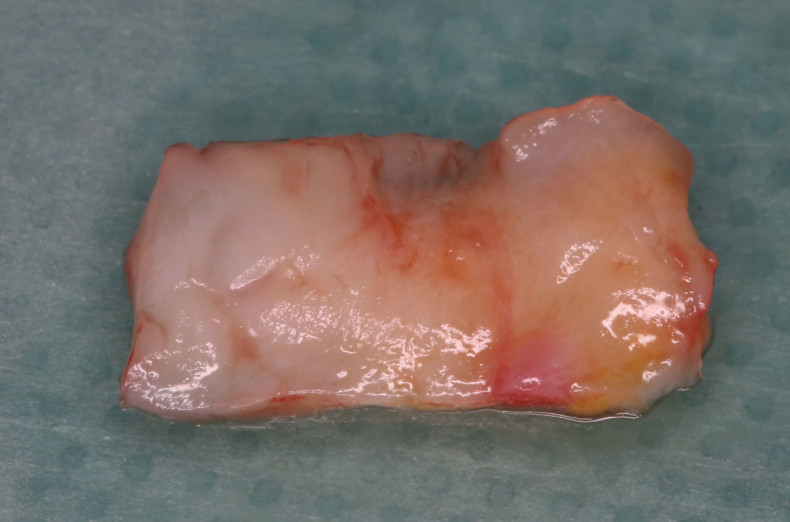
In the upper layers, there is hardly any glandular and adipose tissue. The harvested graft is very compact and consists almost entirely of connective tissue.
The difference is also noticeable intraoperatively and postoperatively. On one hand, the two grafts differ in handling. During the healing process, the subepithelial graft undergoes greater shrinkage, whereas the de-epithelized FST tends to proliferate somewhat over time.
But substitute materials also provide a valuable contribution to improving the soft tissue situation. In gap defects, these substitute materials can safely fill a small vestibular indentation or be used around teeth as part of recession coverage. It should only be noted that substitute materials should ideally not be exposed and that the same volume increase cannot be assumed as with the use of autologous grafts.
Influence on Soft Tissues and Wound Healing
The harvesting of soft tissue from the palate still represents one of the procedures with the highest morbidity. Although scientific data suggests that it is less the size of the grafts but rather the depth of harvesting that is crucial, it would be nice to have materials that not only accelerate wound healing to improve the outcome but also reduce discomfort for the patient.
PRP/PRGF – PRF
Autologous blood concentrates have a good reputation and are scientifically well studied. Besides the fact that blood collection is perceived as a very unpleasant procedure by some patients, the data for improved soft tissue healing is very good. In the surgical area, improved wound healing, reduced swelling, and decreased morbidity can be observed. In combination with bone augmentations, blood concentrates can create a “Sticky Bone,” which simplifies handling and improves the outcome.
If a blood concentrate is used for the surgical procedure, there is nothing against additional application on the palate.
Collagen
Collagen membranes have proven effective not only for improved healing but also as a carrier medium or for bleeding prophylaxis. Here too, the data shows a significant improvement in wound healing and less scar tissue. By omitting the use of collagen matrices on BGT/FST, morbidity is massively reduced. The additional costs and the source of the collagen (mostly porcine) should not go unmentioned.
Enamel Matrix Proteins
When working with enamel matrix proteins in the context of recession coverage, a remainder can be applied without hesitation in the area of the palatal wound. The data here is very clear and shows a significantly faster revascularization in the first days after the operation. Enamel matrix proteins can also be used solely for wound healing, although they tend to realize their full potential more in the area of periodontal regeneration.
Hyaluronic Acid (Hyaluronan)
Hyaluronic acid has worked its way from a niche to the spotlight in recent years. The hyaluronic acid produced today through bacterial fermentation is identical to that found in humans. Hyaluronic acid has a positive effect on reducing swelling, decreasing morbidity, and additionally leads to reduced scar formation. When used with bone augmentations, hyaluronic acid can stabilize the graft, similar to "Sticky Bone" made with autologous blood concentrates. If hyaluronic acid is used during surgery, it can also be applied to the palate to improve wound healing. Here, too, the use of a carrier material is advantageous to further extend the duration of action.
Summary
Soft tissue management is an important part of almost all surgical procedures. In bony augmentations, it ensures that there are no dehiscences and that the bone heals more predictably. Around implants, it leads to reduced bleeding and plaque indices, and around teeth, it restores natural aesthetics. Sufficiently thick soft tissue protects the bone from resorption. No matter how important soft tissue is, we should not forget that it is just a small piece of the mosaic that leads to the desired success. Hard tissue is no less important. But patient factors should also not be overlooked. Finally, Prof. Dr. Stefan Fickl can be quoted: “Bone stands hard, but the soft tissue is the guard!”
This article was published in the Implantology Journal.
