"The Perfect Screw" in Older Patients (Part 3)
Machine translation
Original article is written in DE language (link to read it) .

The increasing proportion of older patients presents us with special challenges in everyday practice. In connection with advanced age and the resulting slowed regeneration potential, there are often specific health deficits that lead to significantly poorer wound and tissue healing. Not only do interactions from existing medications such as bisphosphonates play a role, but also frequently occurring general diseases such as periodontitis, diabetes, or coronary heart disease.
If one or more risk factors are present, even atraumatic treatments, such as non-surgical periodontitis therapy, can lead to significant complications. For this reason, the use of so-called biologics has proven to be very effective, especially in these patients. These not only enable significantly improved wound healing but also reduce postoperative swelling and pain perception. Furthermore, some biologics even lead to significantly improved periodontal and bone healing.
Through a tailored patient-oriented practice concept, it is possible to perform highly complex treatments with a higher risk profile, such as immediate implantation in older patients with existing risk factors.
Case Report
The 84-year-old male patient presented to our practice with complaints of pain in the upper front jaw. He had a medically controlled hypertension and an unremarkable general medical history. In the specific dental examination, risk factors such as existing periodontitis and peri-implantitis on an already present implant were identified.
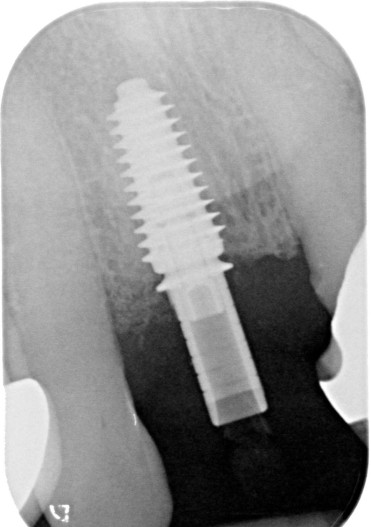
Clinically, inflamed soft tissue was observed along with a fractured tooth (Fig. 1). Radiologically, significant secondary caries and an apical lesion were detected (Fig. 2).

The patient expressed the desire for tooth extraction followed by prosthetic treatment. After weighing the clinical starting situation and the prosthetic options, an implantological treatment in the sense of immediate implantation would provide the best conditions for optimal tissue preservation without further surgical additional interventions.
However, due to the advanced age of the patient and the influencing factors present, there was a significantly increased risk profile in terms of potential wound healing disorders. For this reason, our practice- and patient-oriented concept, which is particularly characterized by minimally invasive procedures, includes the use of the wound healing accelerator hyaluronic acid to safely and predictably carry out such treatments with a higher risk. The patient presented for extraction with simultaneous implantation in the sense of a classic immediate implantation. Furthermore, it was planned to provide the patient with a fixed provisional restoration in the sense of immediate loading.
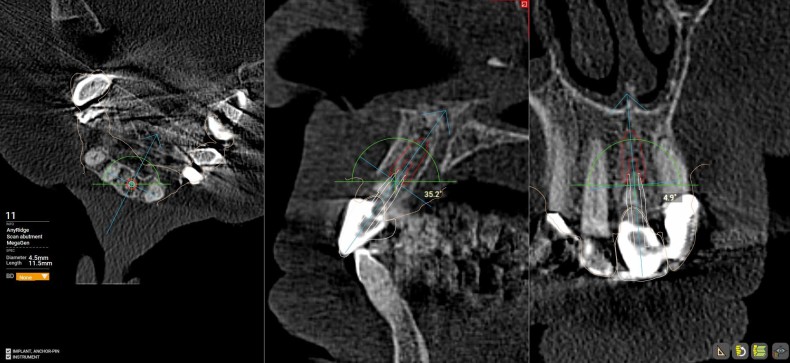
In advance, a digital planning was carried out using DVT and the planning software R2Gate (MegaGen). This allowed the intraoperative implant position, bone conditions, and later crown position to be determined. This approach, along with the so-called "Backward Planning," can make the treatment process safer and significantly increase planning reliability.
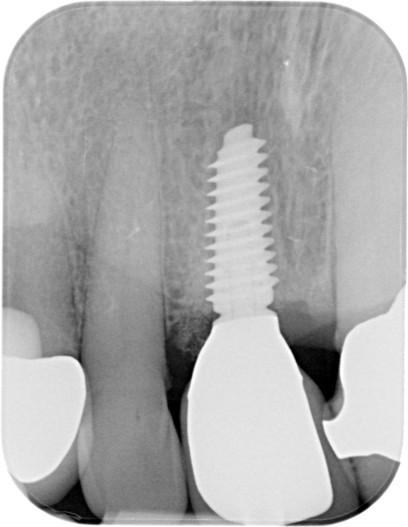
The existing root remnant was carefully removed along with the apical granulation tissue, so that the maximum amount of bone could be preserved (Fig. 4). The exact implant position was determined and executed using Guided Surgery, allowing the implant to be inserted in both vertical and horizontal perfect positions (Fig. 5). An implant with a diameter of 4.5 and a length of 11.5 mm was placed (MegaGen AnyRidge). Due to the special implant design, a very high primary stability can be achieved through the protruding thread flanks. With a constant core diameter but an increasing implant diameter, the maximum bone preservation is prioritized here. The BIC (Bone–Implant Contact) was determined using the so-called Mega ISQ via a SmartPeg (Fig. 6). An ISQ value of 74 was achieved. Values of > 70 indicate high primary stability, and immediate loading can be performed on single-tooth implants. We standardly fill the so-called Jumping Distance (space between the implant and residual bone) with bone substitute material, as this leads to better preservation of the buccal contour and a more aesthetic result.



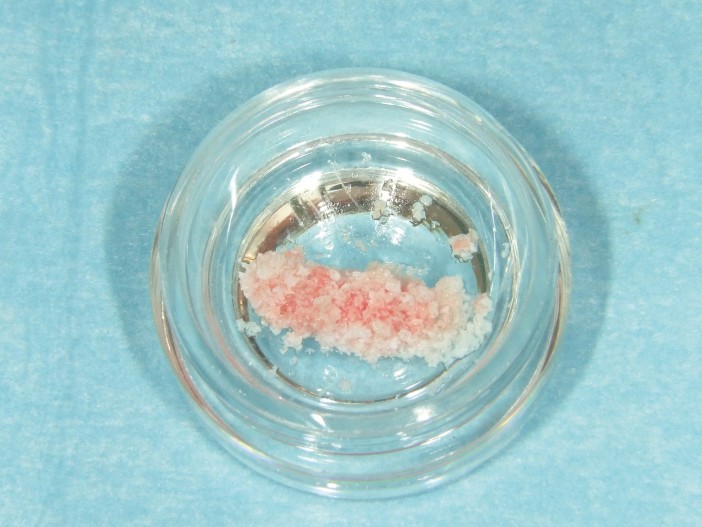
We augment in our practice using the "Sticky Bone" principle. For this, we use a porcine bone substitute material with a slow resorption profile (SMARTGRAFT, REGEDENT), which allows for better volume preservation during immediate implantation compared to rapidly resorbing bone substitute materials. We pre-mix the porcine material with cross-linked hyaluronic acid (hyaDENT BG, REGEDENT), not only to achieve a more precise augmentation and better positional stability (Fig. 7). It is known that cross-linked hyaluronic acid not only promotes improved wound healing, but it also leads to better bony integration of the bone substitute material particles, resulting in increased bone-implant contact of the immediate implant.
Subsequently, the provisional crown was fitted, thus closing the extraction socket (Fig. 8). Figure 9 shows the postoperative X-ray immediately after implantation and after fitting the provisional crown.

The provisional restoration was removed from function, and the patient was strongly instructed to avoid any possible early loading of the implant.
The patient was informed postoperatively and was shielded both antibiotic and analgesic. Antiseptic mouth rinse is recommended in our practice only from the third day post-op to avoid reducing fibroblast expression in the initial wound healing phase.
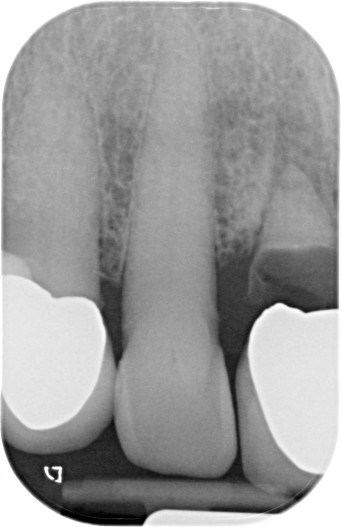
After a healing period of four months, the definitive restoration was completed. Figure 10 shows the clinical situation after fitting the definitive crown, which was screw-retained occlusally. Radiologically, a stable bony situation and perfect fit of the restoration are evident (Fig. 11). Even after one year, clinically stable and inflammation-free soft tissue conditions are observed despite adjacent plaque accumulation (Fig. 12). In Figure 13, stable bony conditions are evident without signs of bone resorption.