Influence of orthopedic-functional treatment on the width of the nasopharynx
Machine translation
Original article is written in IT language (link to read it) .
Summary
It is well known that mouth breathing plays a crucial role in the onset of dysgnathias at an early age. With the aim of determining which treatment is most appropriate in relation to an etiopathogenic approach, and to compare the results obtained, the following study was conducted. The sample consisted of 36 dysgnathic patients, aged between 4 and 14 years, divided into three groups. "Group A": no treatment (control group), consisting of 15 patients (41.66%); "Group B": treated with Functional Orthopedics, consisting of 14 patients (38.88%); "Group C": treated with Orthodontics, consisting of 7 patients (19.44%). All were randomly selected. The upper airway width was measured, based on lateral cephalometric radiographs taken with an interval of no less than 10 months in the city of La Plata, capital of the Province of Buenos Aires, and in the city of Neuquén, capital of the Province of Neuquén, both in the Republic of Argentina, from a universe consisting of 2500 patients. Five parameters of the pharyngeal cephalogram were used for the measurements, observing that in "Group A", there was an average decrease of -0.49mm. If we consider the evolution of this control group as a reference, we can say that there was an increase in the pharyngeal width in all treated patients: in "Group B" by 100% (1.49mm) and in "Group C" by 75% (0.99mm), as an evident conclusion, the patients treated with Functional Orthopedics achieved the greatest increase in the upper airway width.
Introduction
When delving into the etiology and the etiopathogenic mechanisms of dysgnathias, we encounter a recurring, almost omnipresent theme: mouth breathing.
Since last century, and mainly after the studies of Linder-Aronson, to mention the most important one, the deleterious effect that mouth breathing has on the growth of the maxillofacial skeleton has been out of discussion.
It is well known that functional bimaxillary appliances primarily aim to reorganize the functional matrix, mainly the tongue and the labial and buccal strap, in order to generate the necessary stimuli for eumorphic growth.
Thus, the modifications obtained with this therapy in different areas have been well studied to date, among which we will mention, considering it a determining factor, the anterior, middle, and posterior oral sealing.
But nothing has been said about the possibility that such appliances could also have an effect on the nasopharynx, considered as the upper portion of the pharynx, which has as its lower limit the extension of the palatine plane.
This hypothesis, which at first seems to want to force things, does not sound far-fetched if we remember that some bundles of the buccinator have their posterior insertion in the pharyngeal wall, thus closing what Moss referred to as the functional capsular buccopharyngeal matrix.
Based on circumstantial observations in cephalometric radiographs of small patients undergoing orthopedic treatment, the concern arose about the possibility that this treatment was also producing modifications in the upper airways, more precisely in the lumen of the rhinopharynx.
It was in order to confirm or deny this a priori assumption that the present research was designed. For this purpose, the lumen of the upper airway was measured on casts of lateral cephalometric radiographs taken with an interval of no less than 10 months in 36 dysgnathic patients, in growth ages, divided into three groups: without treatment (control group), with functional orthopedic treatment, and with orthodontic treatment.
If some of the parameters of the pharyngeal cephalogram were used for this measurement; it was observed that there was an increase in the pharyngeal lumen in all treated patients, but to a greater extent in those treated with functional bimaxillary appliances.
Objectives
The aim of this research is to assess the difference in the size of the nasopharyngeal lumen in dysgnathic patients treated with Orthodontics and with Functional Orthopedics, taking as a reference a control group without treatment.
The hypothesis that is being tested is that patients treated with functional bimaxillary appliances have a greater gain in the widening of the nasopharyngeal lumen than those treated with orthodontic appliances and that the control group without treatment.
Materials and methods
A longitudinal descriptive study was conducted on dysgnathic patients who presented for dental consultation.
Geographical scope: City of La Plata, capital of the province of Buenos Aires, and the city of Neuquén, capital of the province of Neuquén, both in the Republic of Argentina.
Population: A sample of 36 children aged between 4 and 14 years.
Statistical unit of observation: Pharyngeal cephalogram, performed on cephalometric casts from lateral cephalometric radiographs of profile head of dysgnathic patients, initial and control, with a difference between both of 10 to 14 months. The casts and measurements were performed by the same professional and within the same time period. The following were measured:
- Angle O: formed by the Basion-Nasion planes and palatal plane (anterior nasal spine-posterior nasal spine), measures the height of the middle third of the face, providing the vertical framework for the air entry. The norm is 28° ± 3°.
- Depth angle: formed by the AA-S planes (most anterior point of the atlas-center of the sella turcica) and S-ENP (center of the sella turcica-posterior nasal spine). Measures the possible anteroposterior magnitude of the pharyngeal space. The norm is 48° ± 5°.
- Adenoid tissue 1: Measured on the ENP-Ba plane, from ENP to the posterior wall of the pharynx. Reflects the magnitude of the pharyngeal lumen at the retro-pharyngeal level. It should measure 20mm at 6 years and 26 mm at 16 years, with a variation in both cases of ± 5mm.
- Adenoid tissue 11: Measured on a perpendicular line from ENP to the S-Ba plane. From the posterior nasal spine to the posterior wall of the pharynx. Measures the lumen at the epipharyngeal level. It should measure 15mm at 6 years, up to 22 mm at 16, in both cases, ± 4mm. Measures the lumen of the epipharynx.
- Adenoid tissue 11 1: Measures the distance between the V pt (pterygoid vertical) and the posterior face of the pharynx, 5mm above the ENP. Its normal value is 7mm at 6 years, up to 14mm at 16, with a variation of ± 4mm.
Collection method: Dysgnathic patients presenting to the dental office. None of them had undergone orthodontic and/or orthopedic treatment, nor speech therapy, nor surgical treatment of the upper airways prior to the initial telerradiography.
After the initial examination, "group A," consisting of 15 children which corresponds to 41.66% of the sample, did not start their treatment for personal reasons, having returned to the consultation after an approximate period of one year, when new studies were conducted, taking this group as a control.
"Group B," consisting of 14 children representing 38.88%, began their orthopedic treatment.
"Group C," made up of 7 children representing 19.44%, began their orthodontic treatment.
3.5. Grouping: The sample was observed in age groups every 2 years, finding a greater number of untreated children at younger ages, and in older age ranges a majority with orthodontic treatment.
Results
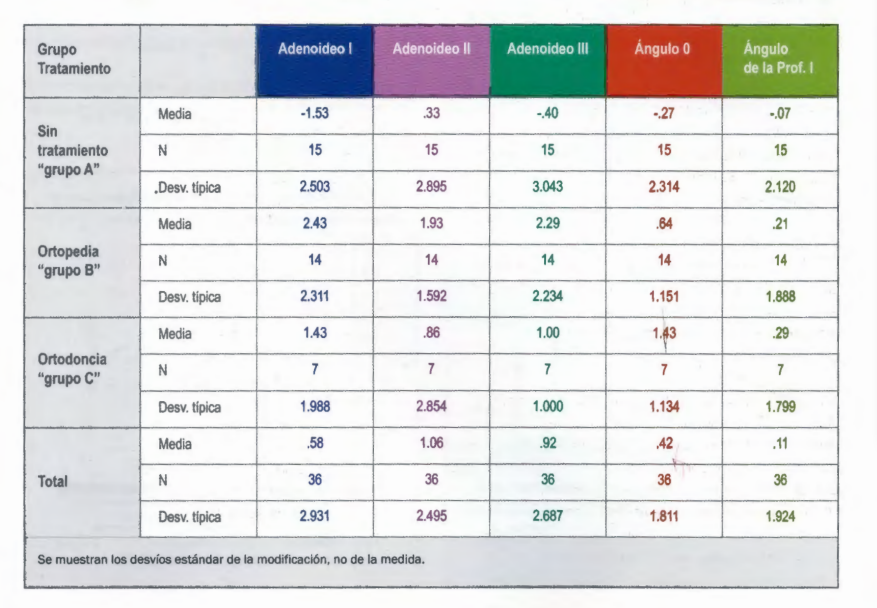
The following table shows the data as it was collected based on future or random interpretations:
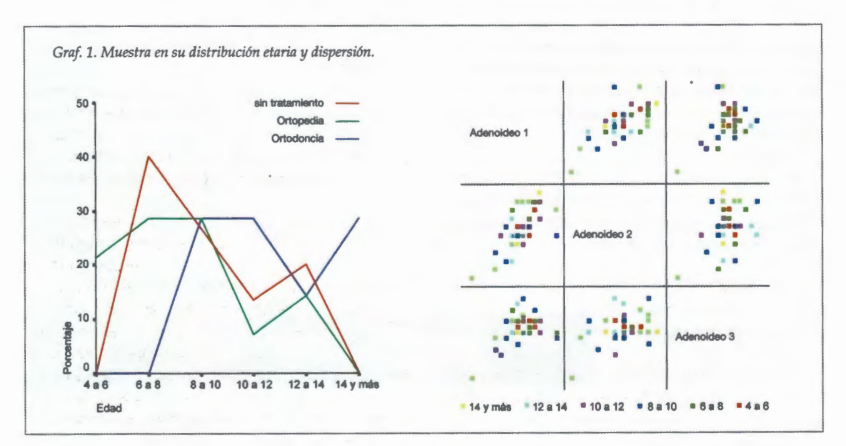
From the reading of the left graph, it can be seen that there is no uniform age distribution in the sample. A greater number of young children is observed among the patients treated with Functional Orthopedics, and a greater number of patients at the upper age limit of the sample is found in the orthodontically treated group. The table on the right is the verification of the validity of the sample by dispersion.
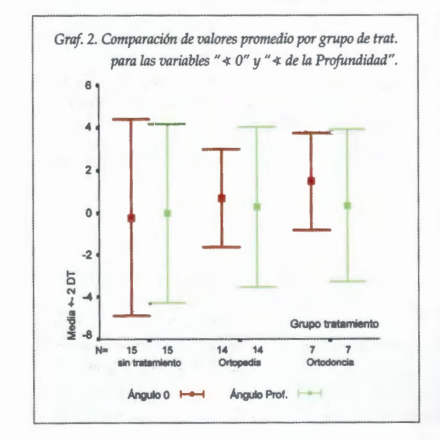
In graph 2, the comparison of average values by treatment group for the variables Angle O and Depth Angle is observed. The Depth Angle, that is, the anteroposterior skeletal framework of the nasopharynx, increased in amplitude (average data at the height of the rectangle) in the treated patients, although to a slightly greater extent in those treated with Orthopedics. The Angle O, which shows the distance between the anterior cranial base and the palatal plane, that is, the air intake tube measured vertically, increased in both patients treated with Orthopedics and with Orthodontics. However, the most benefited in this aspect are the latter.
The graph 3 compares the evolution of the pharyngeal airway in the three levels, and we understand it is the most substantial among all. It can be seen that the center of the control group's values shows that they have had the least gain in the modification of the pharyngeal airway over time. Meanwhile, if we observe the group treated with Functional Orthopedics, we will see that the three parameters measured on the pharyngeal airway have gained substantial airflow. When observing the group of patients treated with Orthodontics, their airway passages have expanded but in a lower range.
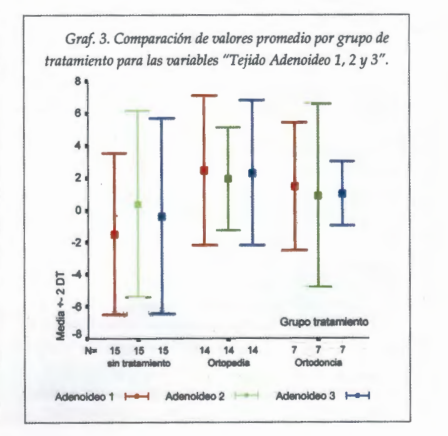
In graph 4, the average values by treatment group for the five variables are compared, showing the 5 data points from the three groups. If we observe the average, we will see that the most advantageous group in relation to the development (expansion) of the upper airway is undoubtedly that of patients treated with Orthopedics, except for the value of the "Angle O".

Discussion
In all treated patients, there has been an increase in the size of the skeletal framework of the airway (Angle O and Depth Angle). The Angle O (anterior cranial base palatal plane) increased in size to a greater extent in patients treated with orthodontic appliances. We understand that since no direct relationship was found between dental movements and the inclination of the palatal plane, we must attribute this result to the composition of the sample, which includes a higher number of prepubescent or pubescent patients among those treated with fixed appliances, which signifies the effects of somatotropic hormone on the nasal septum. In a word, we attribute this increase to growth factors.
The rest of the evaluated parameters show a favorable behavior in patients treated with functional bimaxillary appliances, compared to those treated with fixed appliances and the control group.
Conclusions
The nasopharyngeal space increased to a greater extent in the treated patients than in the control group; and among the treated patients, the pharyngeal space increased to a greater extent in those subjected to functional bimaxillary therapy.
I would like to remind here the definition we use for the term dysgnathia, a concept taken from Prof. Dr. Nelson Anunciatto: "A dysgnathia is a morphofunctional disorder in the cranio-cervico-maxillofacial area." Not only is there no stability in the results of a treatment if a morphofunctional balance is not achieved, but also, in growth ages, we do not have the right to order the dental arch while allowing the set of deformities to continue expressing themselves, fueled by dysfunction.
The path to rehabilitating morphofunctionally a growing dysgnathic child is long, and we understand that it must be done from conception and with the therapeutic means of Functional Orthopedics.
Graciela I. Lorenz, Silvia Galetti, Yamila Sarin
Bibliography
- Linder-Aronson, S. Their Effect on Mode of Breathing and Nasal Airflow and Their Relationship to characteristics or the facial skeleton and the dentition: Acta Otolaryngologica. Supplementum 265. 1970.
- Linder-Aronson, S; Henrickson, C.O.; Westborg B. Roentgenological changes in anteroposterior nasopharyngeal dimensions in 6 to 15 year olds. Practica otorhinolaryngologica, 1973 (Swiss).
- Handelman, C.; Osbornem, G. Growth of the nasopharyngeal and adenoid development from one to eighteen years; Angle Orthodontist. 1968 forum on the tonsil and adenoid problem in orthodontics; Am. J. Steele, Fairchild, Ricketts: F Orthod. 34: 485-514, 1968.
- Rocabado, M. Biomechanical cranio-cervical analysis through a lateral teleradiography. Revista Rjnserción.
- Balters, W. Guide to the Bionator Technique. Círculo Argentino de Odontología, Buenos Aires.
- Breuer, J. The mouth-breathing patient. Revista de la Asociación Odontológica Argentina. Vol 77, number 3 and 4 - 5 and 6. May-August; September-December 1989.
- Frankel, R. Functional Orthopedics of the jaws and the oral vestibule as a basis for appliances. Editorial Beta S.R.L. Buenos Aires, 1969.
- B. Rakosi, T.; lrmtrud, J. Atlas of Maxillary Orthopedics. Diagnosis. Editorial Masson-Salvat. Scientific and technical dental editions S.A. 1992 Barcelona. Spain.
- Anunciatto, N. Neuroanatomy of the Stomatognathic System. The importance of therapy on the Nervous System. International course taught at the Argentine Association of Functional Orthopedics of the Jaws on November 5 and 6, 1999. Transcribed and recorded by Dr. María del Carmen Attene.
