Morphofunctional Recovery of the TMJ Post-Condylectomy Treated with Functional Orthopedics of the Jaws.
Machine translation
Original article is written in ES language (link to read it) .
Summary
9-year-old patient presents to the consultation with mandibular laterodeviation, due to the absence of the right condyle which was removed as a "therapeutic attitude" following a fracture from a neck accident. The treatment is carried out with Functional Orthopedic appliances and after 3 years, it is functionally achieved that the jaw recovers the centric in its opening and closing movements. A growth of tissue resembling a condylar formation is observed.
Studies are conducted to verify the compensatory mechanisms that were achieved for a functioning close to normal.
Generalities
Talking about mandibular growth and development, and in particular about the A.T.M., is to talk about a very controversial topic, and on which there are different opinions regarding what the true mechanisms capable of governing it are.
Up to now, countless works and clinical, experimental, statistical experiences, etc., have been carried out to determine reliably what the generally established path in bone development and growth is by its own capacity, and what the main elements that govern it are.
The topic of mandibular growth and development is of significant importance for two major dental specialties: Functional Orthopedics and Oral and Maxillofacial Surgery, as both constantly deal with maxillofacial malformations, which not only have different etiologies but also require varying treatments according to each particular case, making it incorrect to apply a standardized therapy to solve similar pathologies. Hence, the importance of understanding the factors that produce the different anomalies, in order to carry out a treatment appropriate to each patient.
For all these reasons, the mandible cannot be studied in isolation; it must be correlated with a large number of other structures and functions.
Mandibular growth has been and continues to be a highly discussed topic.
There is a theory that assigns the fundamental role of governing the growth of the lower jaw to the cartilage of the condyle. Researchers who support this theory have conducted countless experiments in order to prove this position with concrete facts (Schmidhuber; Osborne and Ware; Sicher; Proweer; Samat and Engel; Engel and Brodie).
There are authors like Scott (1967), who establishes that cartilage would have a primary role and sutures a secondary and compensatory role, in terms of craniofacial growth, meaning that cartilages would act as true growth centers, separating the contiguous bony structures, and the sutures would be responsible for compensating that separation through bone neoformation.
Durkin (1972) histologically differentiated the cartilage of the condyle from the epiphyseal cartilage, noting that the main function of the former is to serve as an adaptation center and not a primary growth center like the latter.
There is another conception, called genetic, according to which the shape and size of the mandible and the entire craniofacial mass would be governed genetically.
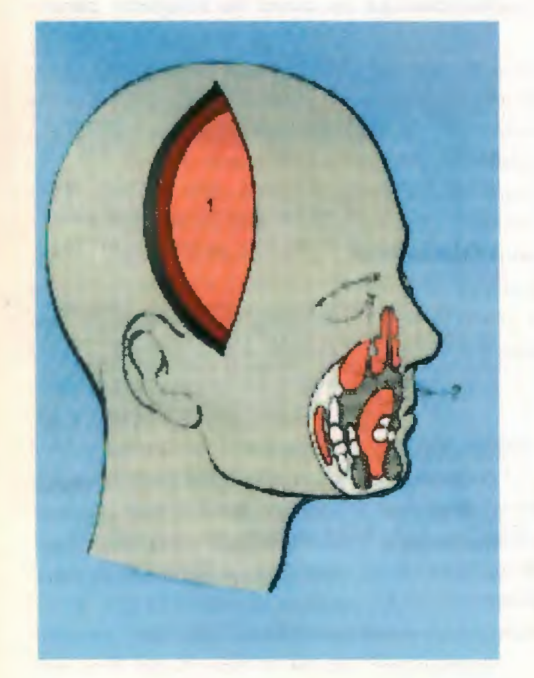
1 - Functional neurocroneal motor.
2 - Oro(ociol) capsular motor.
Van der Linden (1966) establishes that there is a permanent interaction between genetic factors and environmental factors in the growth and development of the craniofacial complex.
Another theory is the one initiated by Van der Klaauw (1952), and later followed by Melvin Moss (1960), which gives the function of the mandible the predominant role in its development, considering that there are certain genetic factors that govern growth, but which are then conditioned through what Moss called the Functional Matrix, which is represented by all the soft tissues that work and relate to its skeletal units.
The example that is commonly given is that of the muscle and its activity, although tendons, vessels, nerves, and in a very particular case, the teeth in the jaw, are also considered as functional matrices, due to their behavior on their alveolar skeletal unit. It is worth noting that each functional matrix acts independently on a skeletal unit, which may constitute only a part of what is considered bone in classical osteology.
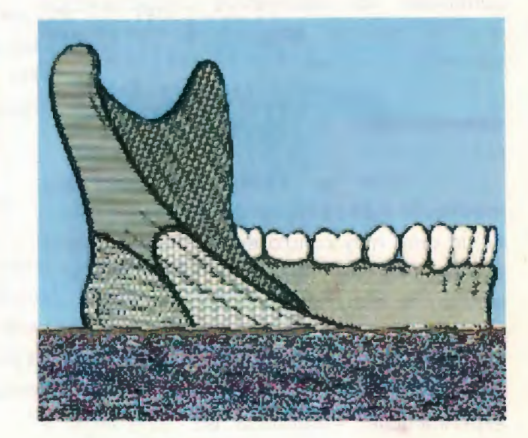
Such is the case of the mandible, which is made up of several micro-units such as the alveolar, the basal, the ascending ramus, the gonial angle, the coronoid process, and the mandibular condyle.
According to Enlow, bone does not grow by itself, but rather it grows due to the soft tissue matrix that covers it, with genetic and functional factors being determinants of its growth in the soft tissues, considering that growth is not governed by the calcified part of the bone itself, but by the muscles, lips, cheeks, mucosa, vessels, nerves, etc., that surround it.
Enlow considers that the condyle functions as a regional growth field, viewing it not as a master center, but as an element of local importance, with the growth of the mandible being the consequence of all the regional fields involved during it.
Another advanced conception of postnatal craniofacial growth is the cybernetic theory of Prof. Alexandre Petrovic, who studies the problems of physiological systems as true complex systems, which can only be solved through cybernetics and informatics.
Petrovic also establishes that condylar growth is subject to local control, of which mechanical forces are a permanently regulating part.

Clinical case
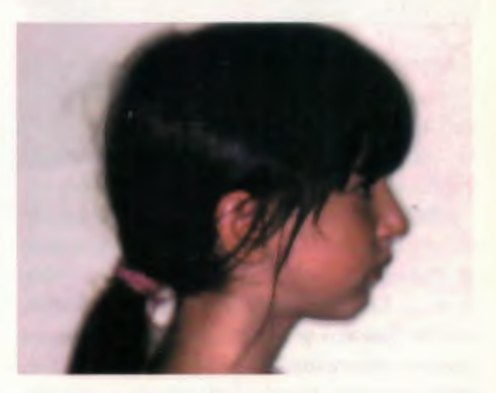
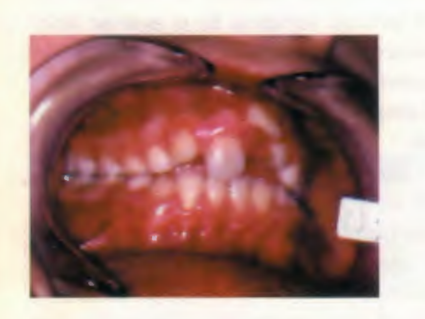
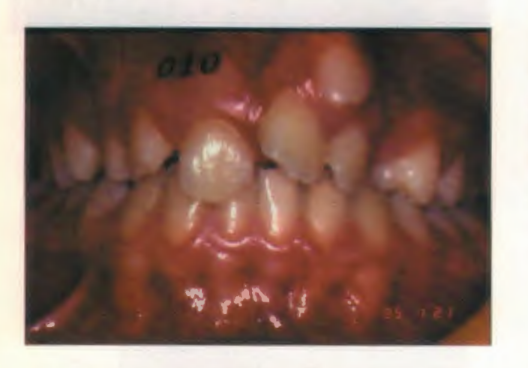
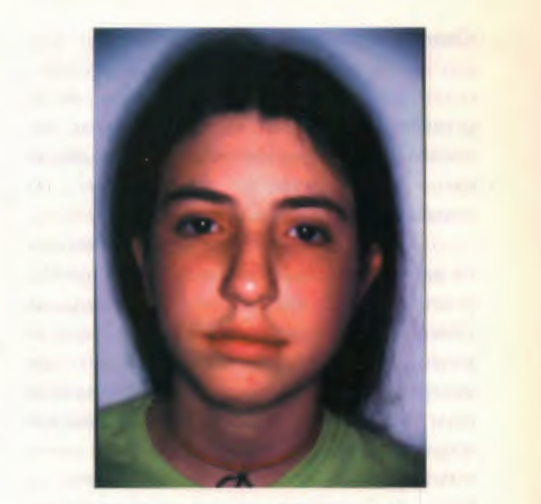
The patient Ana M., 9 years and 7 months old, presents to the consultation at the Functional Orthopedics course held at the Dr. Castro Rendón Hospital in the city of Neuquén, Neuquén Province, in April 1993, referred by a colleague who detected the presence of facial asymmetry.
The main background is an accident, which resulted in a fracture of the right condylar neck that was removed as a "therapeutic attitude." As a result of this, the patient had mandibular deviation upon opening.
At the time of the consultation, her general condition is normal, although a slight vertebral lordosis is detected. In the facial examination, right mandibular asymmetry is recognized, a short upper lip, and an everted lower lip. The labiomental groove is pronounced and the profile is convex.
From a functional point of view, the patient is a mouth breather, as a result of which she maintains a low tongue posture, with a short and hypotonic upper lip and a hypoactive lower lip, presenting anterior oral incompetence and a hyperactive chin.
When conducting the study of the A.T.M., we arrive at the most interesting part of this case, as it is the reason for the initial consultation and where curiosity is most stimulated.
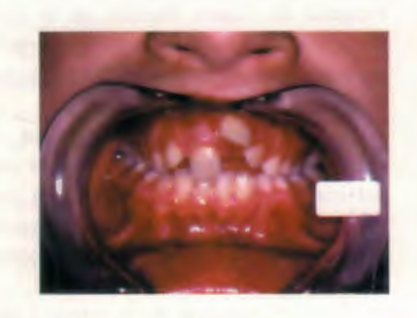

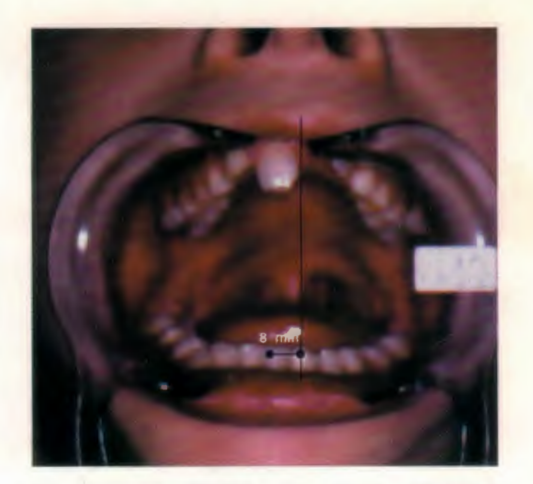

The most notable elements of this analysis are: a significant limitation in the aperture (which does not exceed 30 mm.) and a strong deviation to the right side at maximum aperture caused by the lack of the condyle.
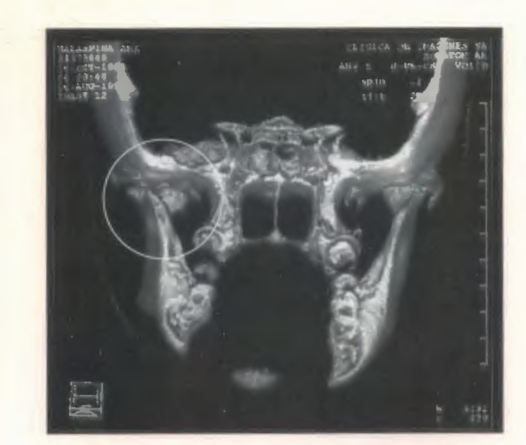
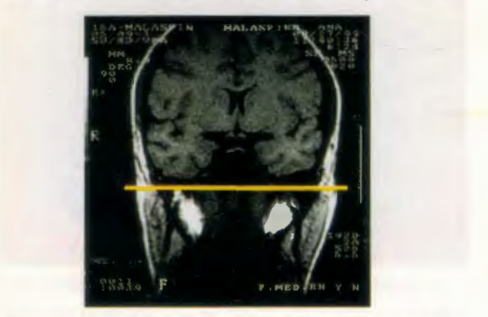
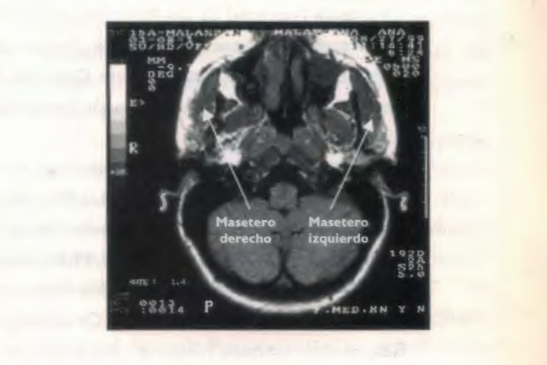
The study of the A.T.M. was completed with the information provided by the magnetic resonance imaging that was performed at the time of the accident. There it is clearly observed that due to the trauma that occurred at that moment, the condyle is almost 90° from its neck, and the report stated verbatim "fracture of the right condyle, with displacement of the free fragment inwards, forwards, and downwards." The articular meniscus appears to accompany the condylar fragment; the glenoid cavity has a normal morphology, with no structures inside. This study was what led the surgeon to perform the condilectomy.
The patient's mouth is then analyzed, and it is observed that the apical base is regular, and that the dental arches have reduced transverse diameters, both upper and lower, with the greatest discrepancy in the diameters 6:6.
In the sagittal sense, the overjet is slightly increased. The molar key is of normal occlusion and the canine is of slight distoocclusion. In the vertical sense, in some dental pieces the crossbite is increased and in others it does not reach the measurements considered normal.
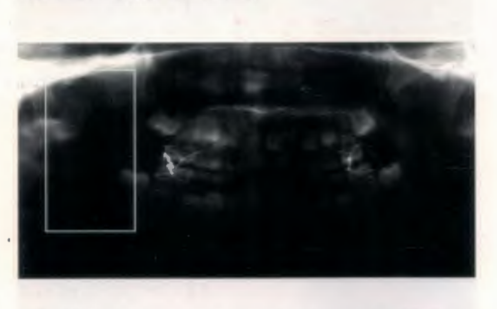

In the radiographic studies, adenoid proliferation is observed, generating difficulty in the airway passage. It also confirms the low posture attitude of the tongue, already clinically observed.
When performing cephalometric measurements, a noteworthy finding is the divergence of bases involving the lower jaw, the mandibular distortion, and a slight increase in the size of the upper jaw.
Once the patient's study is completed, the diagnosis is made. The morphological, functional, and structural problems of the patient must be addressed, and in this case, analyze the serious problem represented by the lack of the mandibular condyle. In summary, we are facing a structural mandibular laterodeviation, with the absence of the right condyle, distorrelation with base divergence, dental dystopias, and associated functional problems.
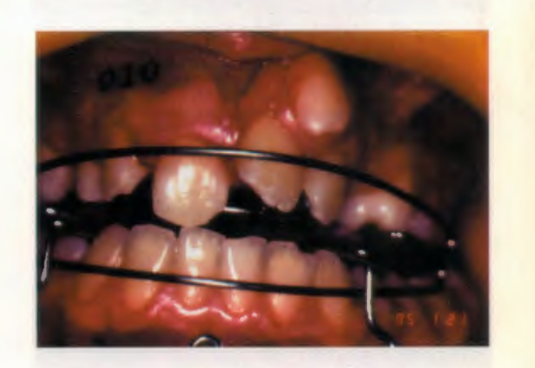
Anita was fitted with a Bionator 11 with lower retrolabial shields, and 16 months later it was replaced with an Elastic Open Activator by Klammt with lower retrolabial shields.
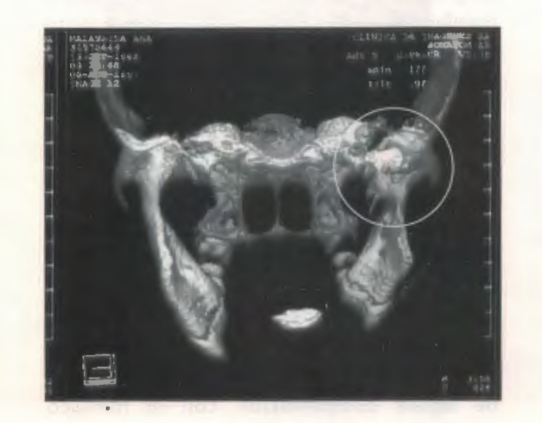
The main treatment objective was to rehabilitate the mandibular movement, guiding it in centric and generating a neuromuscular readaptation, which caused a functional change in the soft tissues surrounding the condylar remnant. In later studies with Computed Tomography, the formation of adaptive tissue in the condylar area was confirmed, recovering from centric to maximum opening the mandibular centric.



Analyzing another aspect, it can be said that when the dental arches were to be assembled, there was a transposition between the lateral (22) and the canine (23) on the left. Radiographically, it is confirmed that the roots of these dental pieces maintain the coronal transposition, which required respecting the location in the mouth, using fixed appliances for dental alignment.
It is important to highlight that the use of functional appliances combined with fixed appliances was always continued, as the pillar of the therapy was based on functional rehabilitation.
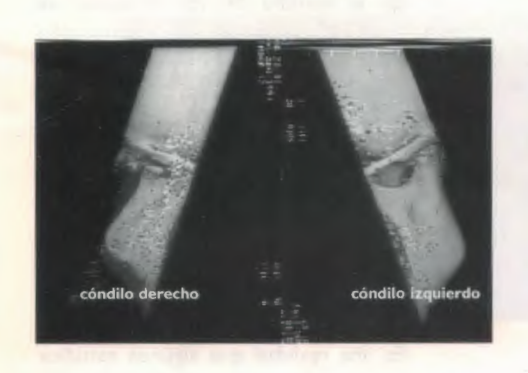
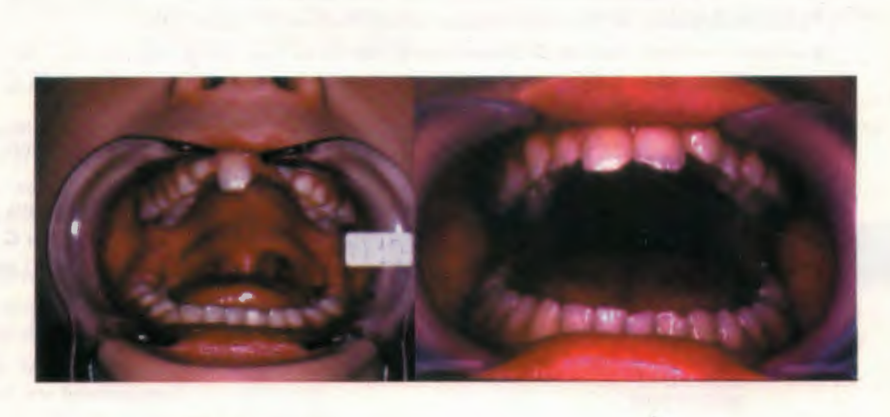
Through the implemented treatment, the growth of the right hemimandible was recovered, almost compensating for the asymmetry, and in the opening movement, from occlusion to maximum opening, no mandibular deviation is observed.
This is a case where, with Functional Orthopedics, and therefore from function, a system has been rehabilitated where an important element was missing: the condyle of the A.T.M.; through the rearrangement of the periarticular soft tissues and generating a centric enagram, the function was reordered based on the remaining components.

Conclusions
A point has been reached in the presentation where it is necessary to calm the spirits and delve into the sediments left by the clinical case treated, in order to gather the lessons that clinical experience provides.
The relevant fact is having treated a patient from whom the condyle was removed, and without the slightest intention of entering into a low criticism, in any bibliography that was searched, there was no indication for removal; on the contrary, it was advised to leave the condylar remnant in an acceptable position, so that it could at least serve as a matrix for its reconstruction. The search was intense, as at the moment the patient arrived, the gathered experience was null, and without feeling ashamed, a feeling of fear towards the unknown emerged, which perhaps gave more strength to seek information on the subject.
Here, functional concepts and the teachings of those masters who transmitted them were put into practice.
As the treatment progressed, it became evident that the chosen path was yielding the expected results and even more; it was never imagined that the therapy would restore almost all the lost anatomy, but there was a conviction that yes, functionality could be restored and the mandibular movements of opening and closing could be recovered, respecting the centric.
As a corollary, the salient facts of the clinical case will be reported: beyond what has been expressed so far, the latest studies conducted on the patient will be analyzed.

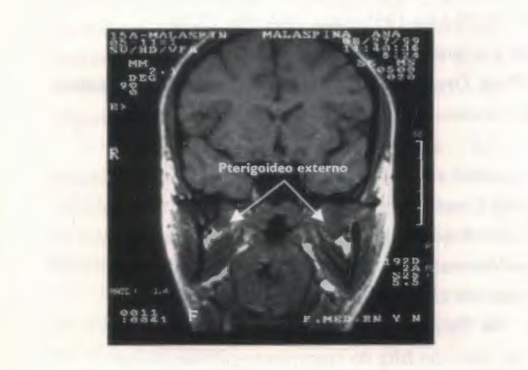
Recently, a new Magnetic Resonance Imaging was performed, where it was a new surprise to see that the "condylar stump" that was manifesting continued to "grow," showing that it had a height similar to that of the healthy side and in the study signal, it depicted lakes that were compatible with fat from spongy bone tissue.
A study of condylar mobility was conducted and it was found that the affected side moved under the same conditions as the healthy side and that at maximum opening, it achieved almost a bicondylar position. It was not possible to study with this method, due to the limitations of the equipment, the intimacy of the joint, especially the bilaminar complex, nor the possibility of any compensation with the articular meniscus, which was removed during the surgical intervention.
In the study of the muscles, it is observed that the direction of the external pterygoid has a more inferior direction, but with an increase in muscle mass on the right side, while there is hypotonia of the masseter on the same side. No change is evident in the muscle mass of the temporal muscle, nor in the direction of the fibers that compose it.
Having conducted the studies presented generates a sense of pride in having exhausted the elements available within the professional's reach.
It is a reality that some studies are left behind, such as a surface electromyography, with a reliable device, which is not available in the area, and doing it with a conventional electromyograph exposes the patient to a situation incompatible with ethics, given the discomfort this study causes. A new CT scan is soon to be performed, which would reveal the morphology of the remodeled elements.
But it is concluded, in our functional microcosm, that there is nothing more pleasant and exciting from this specialty than the rehabilitation that has occurred in our patient from a functional point of view. Being able to see that jaw, which deviated about 8 mm every time it had to perform a mouth opening, and today observing that only when it reaches its maximum opening, it deviates by just a few millimeters, fills with pride and satisfaction those who treated this patient.
As a humble contribution to the problems of maxillofacial dysfunctions and pain, we want to illustrate, as a farewell touch, pre and post-treatment photos of the patient's maximum opening, where she "suffered" the removal of her right condyle as a "therapeutic approach" following an accident that caused the fracture of the neck of the right condyle.
Authors: Ceccarelli Américo Alejandro, Rivas Norma Haidée, Lorenz Graciela Inés
Bibliography:
- Behavior of capsular and periosteal matrices after experimental surgery. Dr. Jorge Marcelo Perez Simón. Journal of the Argentine Association of Functional Orthopedics of the Maxillae. Vol. 18 No 55-56 July 1984-June 1985: Page 24-54.
- Growth of the human mandible and effectiveness of functional orthopedic appliances: biological causes of interindividual variability. Prof. Alexandre Petrovic, Dr. Jeanne Stutzmann, Translation: Emilio Erik Emborg. Journal of the Argentine Association of Functional Orthopedics of the Maxillae. Vol. 20 No 59-60 July 1986-June 1987: Page 23-50.
- Mandibular growth in relation to functional treatments. Dr. Hector O. Pistoni, Dr. Luis A. Miranda, Ora Gladys Salemi de Simes, Dr. Adolfo Cagliari, Dr. Carlos Ausbruch Moreno. Journal of the Argentine Association of Functional Orthopedics of the Maxillae. Vol. 17 No 53-54 July 1983-June 1984: Page 29-42.
- Post-natal maxillofacial development. Dr. Hugo Rios. Journal of the Argentine Association of Functional Orthopedics of the Maxillae. Vol. 29 No 77-78 July 1995-June 1996: Page 22-30.
- Mandibular laterodeviations, functional and skeletal. Their resolution from Functional Orthopedics. Dr. Lorenz Graciela, Prof. Dr. Rivas Norma, Dr. Ceccarelli Américo. Journal of the Argentine Association of Functional Orthopedics of the Maxillae. Vol. 30 No 1 May 1999: Page 27-48.
- Clinical maxillofacial orthopedics and appliances. Temporomandibular joint. Volume 111. Dr. John W. Witzig, Dr. Terrance J. Spahl. 1993. Scientific and Technical Publishing S.A.
- Diseases of the temporomandibular apparatus. A multidisciplinary approach. Dr. Douglas H. Morgan, D.D.S. Williams P. Hall, M.O. James Veinvas, D.D.S. and F.A.C.D. Mundi Publishing.
- Proprioceptive sensitivity and transverse anomalies of the closure path. Dr. A. Coutand, Dr. G. Demadre Maysson. Journal "Orthodontics" No 76 year XXXVIII. November 1974.
- Response to therapeutic functional stimulus in a child with growth deficiency caused by unilateral ankylosis. Prof. Dr. Carlos R. Guardo. Journal "Orthodontics" year XLVII vol 47 No 94 November 1983.
- Summary of the main characteristics of facial growth. Prof. Dr. Jean Delaire. Journal of the Argentine Association of Functional Orthopedics of the Maxillae. No 64 year 1981.
- Manual on facial growth. Dr. D. Enlow. Intermedica Publishing. Buenos Aires. Argentina. Year 1982.
- Neuromuscular physiology and Functional Orthopedics. Dr. Carlos Guardo et al. Journal of the Argentine Circle of Dentistry. No 3-142 year 1972.
- Clinical implications of the T.M.J. Dr. Robert M. Ricketts D.D.S., M.S. Journal "Orthodontics No 61, year XXXI April 1967.
- Orthopedic treatment in condylar-mandibular trauma. Dr. Nilda B. Bacigalupo, Dr. María N.T. de Duffy, Dr. Alberto N. R. Meroni, Dr. Carlos E. Meroni, Ora Liliana C. Spinedi. Journal of the Argentine Association of Functional Orthopedics of the Maxillae. Vol 13 No 42. Year 1978.
- The T.M.J. in motion. The sense of shape. Dr. Jean-Pierre Yung, Dr. Danielle Pajoni, Dr. Pierre Carpentier. Spanish Journal of Orthodontics. 17 (1987) - 179-192
