Horizontal bone regeneration in the frontomaxillary region with resorbable membrane: periodontal, prosthodontic, and surgical approach
Machine translation
Original article is written in ES language (link to read it) .
Summary
Guided bone regeneration is currently considered a therapy of great importance in implantology to promote bone regeneration in maxillary bone defects; the aim is to create an adequate bed for the positioning of implants. Horizontal guided bone regeneration is based on the use of resorbable membranes in combination with filling biomaterials, such as autologous, homologous, or heterologous bone, as well as alloplastic materials with mechanical barrier functions, aimed at excluding epithelial and connective cells from the repair area and favoring colonization by osteoprogenitor cells.
The combined treatment of periodontal surgical techniques with implantological techniques, such as grafts or certain flaps, determines the success of implant rehabilitations.
Introduction
After a dental extraction, several physiological phenomena occur that affect the alveolar bone surrounding the extraction site. It is common to find limited bone availability after extraction, which can hinder the placement of dental implants. A key requirement for aesthetically pleasing and predictable results over time is an adequate three-dimensional bone volume, including a vestibular bone wall of sufficient thickness and height. Histological studies in humans and animals show the existence of three phases in bone remodeling: an inflammatory phase, a proliferative phase, and a bone remodeling phase, which involves the formation of a clot, the maturation of trabecular and lamellar bone, and complete remodeling, which can last up to 6 months. Therefore, it is extremely important to understand the alteration of the alveolus for the success of the implant intervention and the treatment timelines. Tan et al. reviewed the changes in the alveolar ridge in humans up to 12 months after tooth extraction. This systematic review demonstrated that horizontal reduction (3.79 mm) was greater than vertical reduction (1.24 mm in the vestibular, 0.84 mm in the mesial, and 0.8 mm in distal sites) at 6 months. The percentage of horizontal bone resorption was from 29% to 63%, and the vertical percentage was from 11% to 22% at 6 months. These studies demonstrated rapid volume reductions in the first 3-6 months, followed by gradual bone resorption.
When we find ourselves in a situation of bone deficiency for the placement of implants, guided bone regeneration (GBR) is the best documented method to increase bone in localized alveolar defects.
The main idea of guided bone regeneration is the use of membranes to isolate from epithelial cells, which have a high turnover, and to promote with the use of biomaterials the migration of the desired cells (particularly, osteoblasts) to the wound space. The use of autologous bone is considered the gold standard for the reconstruction of hard tissues. The equal combination of autologous bone and xenograft has shown better results in terms of horizontal augmentation and long-term stability.
To carry out an implant rehabilitation according to the three-dimensional parameters of the bone, there are different approaches, although they can be broadly summarized as performing regeneration before (6-12 months) the implant surgery or during the placement of implants (in the same procedure). This clinical case shows a technique of horizontal guided bone regeneration based on the use of particulate bone and a resorbable collagen membrane.
Case Presentation
This is the case of a 73-year-old woman, categorized as ASA I on the preoperative risk index of the American Society of Anesthesiologists (ASA), who presented with purulence and increased probing in teeth 11 and 21. She visited the clinic because she noticed pain in the mentioned teeth and mobility.
The patient was a non-smoker and showed oral hygiene with a plaque index of less than 25% and a bleeding index of less than 10% 13. She was asked to sign an informed consent.
Diagnosis and Treatment Plan
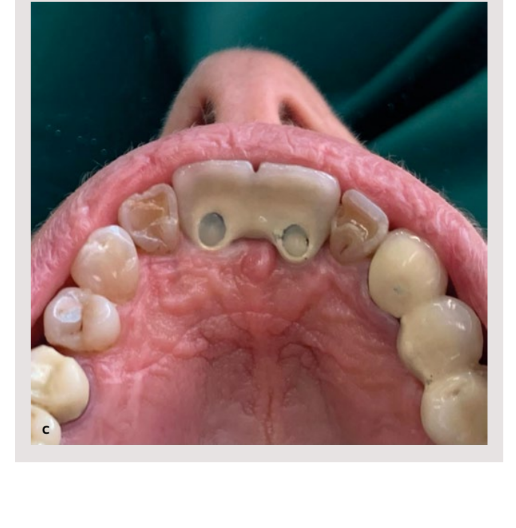
In the intraoral examination, a violaceous gingival margin was observed, with a probing depth of 6 mm in the area of tooth 11 and 5 mm in tooth 21. A cone beam computed tomography (CBCT) was performed to study the bone defect. It showed a marked presence of a lateral periodontal cyst between teeth 11 and 21.
The goal of the treatment plan was to restore the function and aesthetics of teeth 11 and 21 and to restore gingival harmony by closing the diastema with a prosthesis. The planning included diagnostic waxing, the study with CBCT, and horizontal bone regeneration of the identified defect. Special attention was given to the type of flap to be performed, the type of membrane to be used, and the execution of successive gingival grafts.
Prophylaxis treatment was performed with ultrasounds in the weeks prior to the treatment.

Development of the intervention
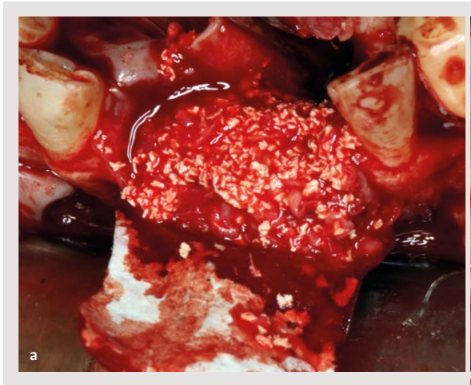
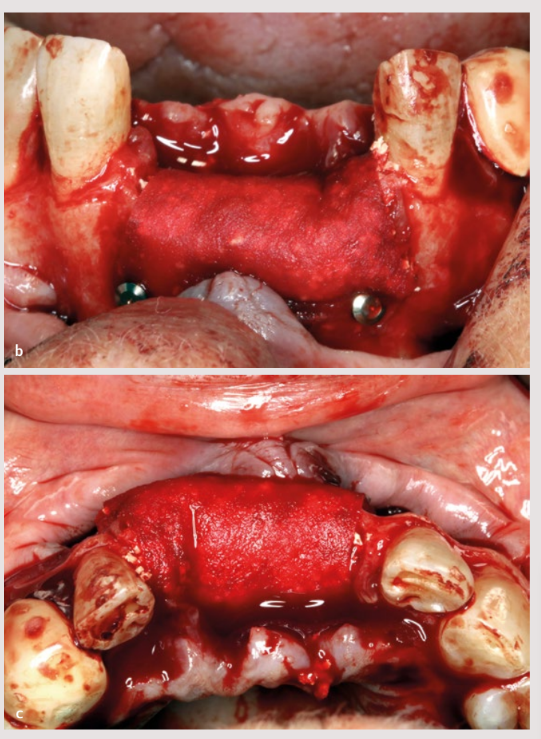
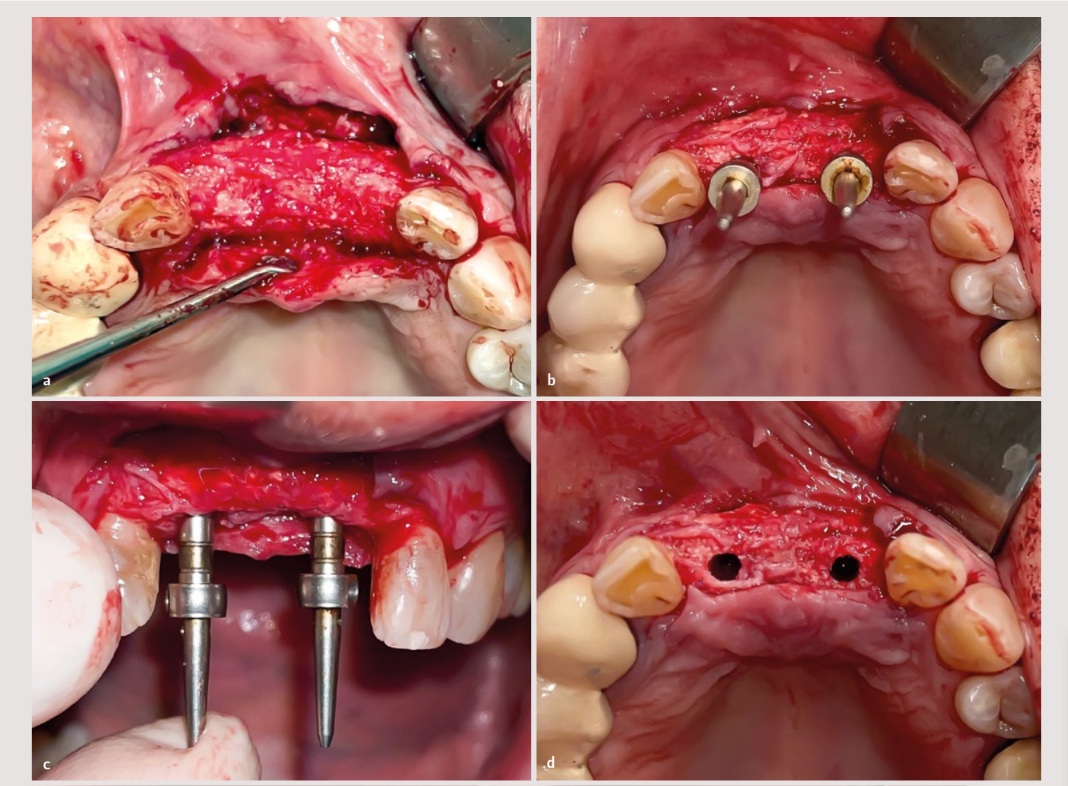
The patient was treated using the horizontal guided bone regeneration technique with the use of a 20 × 30 mm OsteoBiol® Derma membrane (Tecnoss) and particulate bone made up of equal parts of autologous bone obtained from the mandibular ramus and bovine spongy xenograft (Cerabone®, Botiss).
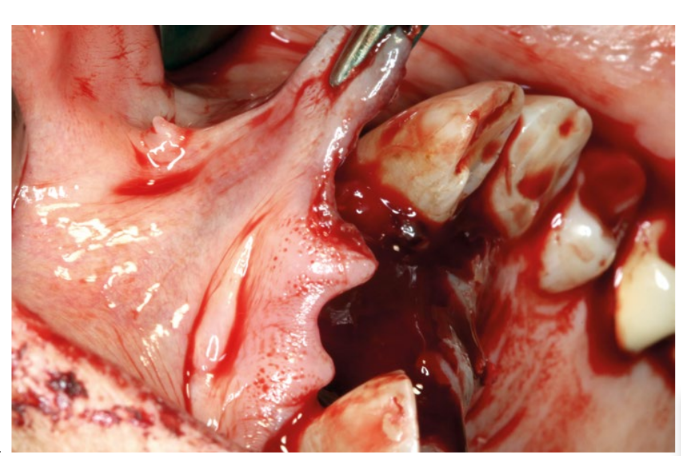
After the application of infiltrative anesthesia with articaine at the bottom of the vestibule, the extractions were performed. These began with careful intrasulcular incisions using a micro-scalpel, followed by interproximal luxation, and finally, with as much delicacy as possible, the teeth were extracted using an incisor forceps.
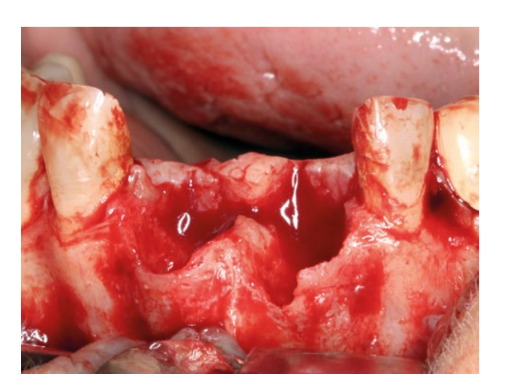
A trapezoidal or Newman-type flap was created with vertical incisions distal to the canines 13 and 23, incising in the area of the papilla in the shape of a hockey stick. The flap was detached and the granulation tissue was curetted.
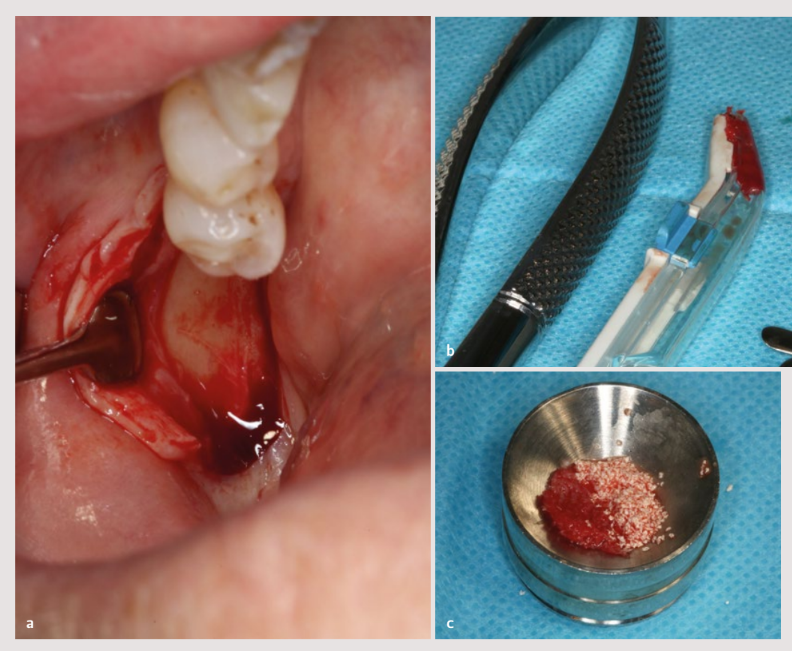
Next, the collection of autologous bone was initiated from the ramus using a single-use bone scraper, and the obtained tissue was mixed 50% with particulate xenograft of 0.5-1.0 mm (Cerabone®, Botiss).
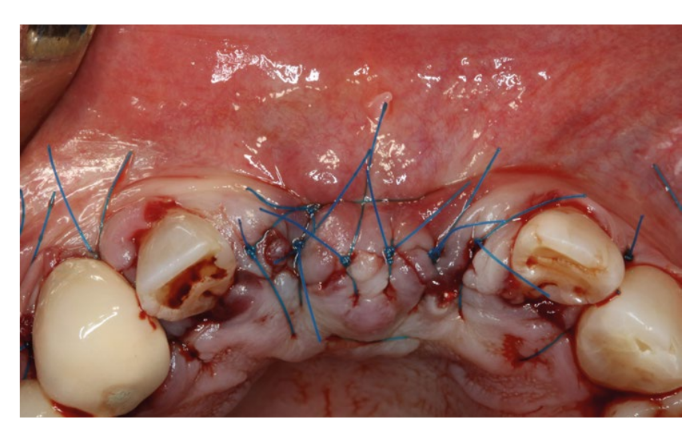
The membrane was fixed in the vestibular area with two apical pins at the ends, and the biomaterial was packed to promote the closure of the grafted content with a single one piece movement and two palatal pins (or 27.5). The flap was then released to provide it with passive tension with a single cut in the periosteum.
A 5-0 nylon suture was applied without any tension, and after two weeks, complete closure by primary intention was confirmed. Internal tension-reducing sutures were applied to flap 14 before placing horizontal mattress sutures and simple sutures that sealed the wound.
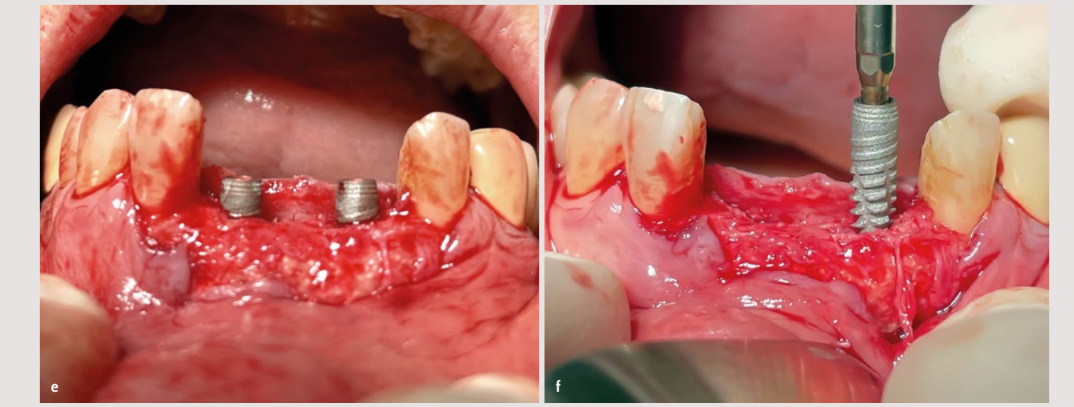
The pre- and post-operative radiographs indicated the stability and homogeneity of the graft.

As postoperative measures, the patient was prescribed an antibiotic (amoxicillin 750 mg with 125 mg of clavulanic acid), a pain reliever (ibuprofen 600 mg), and 0.12% chlorhexidine for 14 days. She was instructed not to pull on her lip and not to brush the area. The patient returned for a check-up one week later; the suture was removed after 15 days.
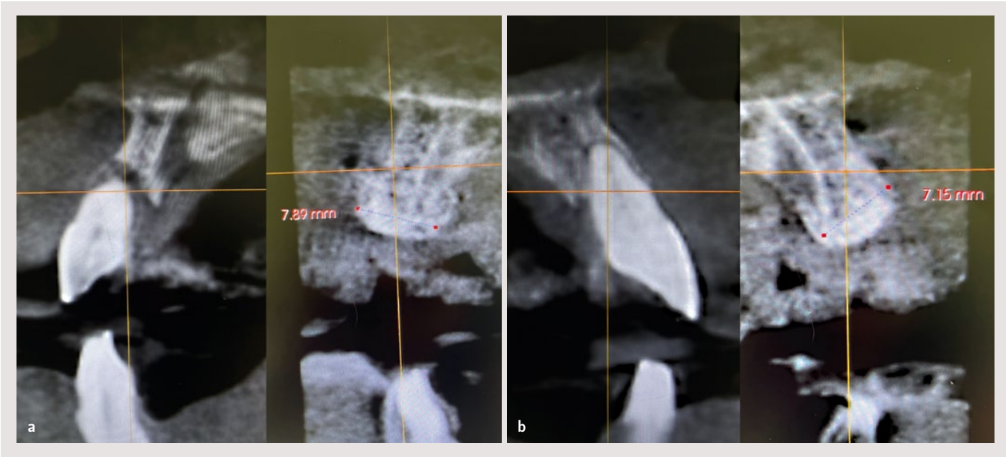
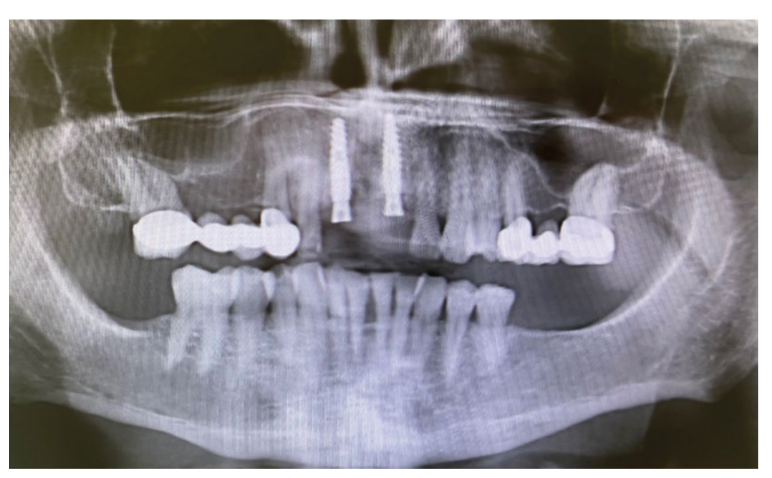
At 8 months post-guided bone regeneration, the axial cuts of the CBCT already suggested good bone formation. On the other hand, healthy but poorly keratinized soft tissue was observed, with little vestibular depth.
At this point, the placement of two implants of 3.6 mm × 12 mm (Vega®+, Klockner) was carried out following the standard guidelines for biphasic implants.
After 3 months, integration was verified, and the second phase was performed with a free gingival graft to increase the thickness of the soft tissue and the vestibular depth.
Subsequently, the patient was referred to the prosthodontics department to begin rehabilitation after a healing period of 3 weeks.
A digital record of the patient's situation was made using the Medit i500 intraoral scanner (Medit), following the procedure recommended by the manufacturer. The maxillae were scanned and then the digital record of the occlusion was carried out.

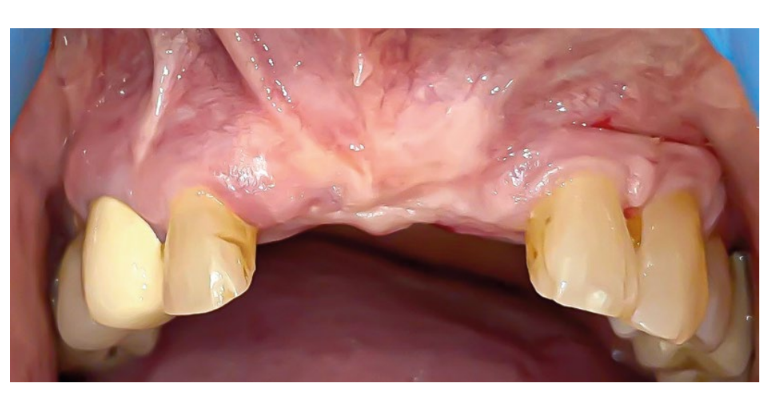

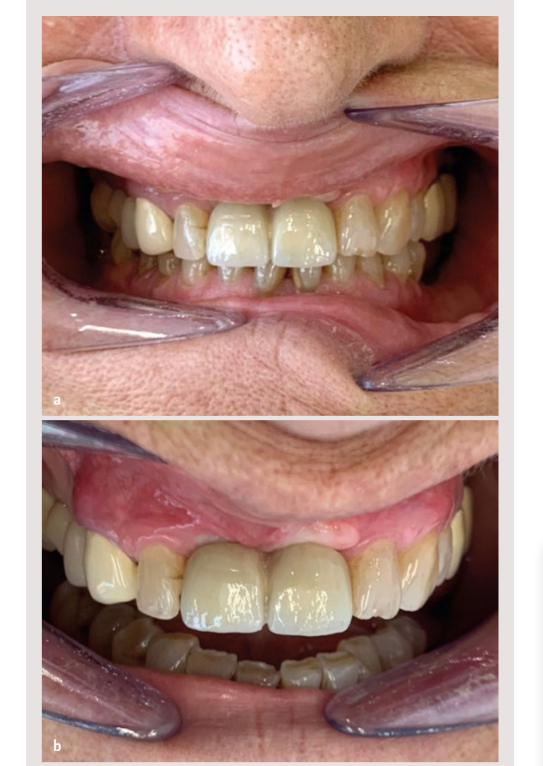
Lastly, the scanning of the implants was performed with scanbodies made of treated metal 15 and originals (Archimedes®). Once the passivity of the structure over the implants was verified, both by radiographic means and with the screw test (Sheffield test) 16, the laboratory was requested to complete the prosthesis with a lithium disilicate coating, emphasizing the emergence profiles of the rehabilitation 17,18. The case was finalized by placing the prosthesis with original Vega®+ prosthetic screws of 3.6 mm (Klockner) at 30 Ncm of torque using a controlled torque wrench (or 27.15). A periapical radiograph was taken to check the correct positioning and, therefore, the passivity of the restoration. Prior to the patient's discharge, the occlusion in maximum intercuspation and during protrusive movements was checked with 40 µm articulating paper.
Discussion
The results of this clinical case are consistent with those found in the literature, which present the use of resorbable membranes as a successful therapeutic approach in horizontal regeneration procedures.
Bovine-derived xenografts are characterized by having osteoconductive properties, without inducing adverse reactions on the recipient bed and with a high success rate. Studies with block intraoral grafts have reported a high survival rate of implants; however, they are associated with varied morbidity depending on the donation site. Intraoral block bone grafts from the ramus offer many advantages by maintaining bone density and presenting minimal resorption. However, their use may be limited if the thickness of the ramus is less than 1 cm, or when the patient has opening limitations or any temporomandibular disorder, in addition to being contraindicated for large bone defects, as was the case in our situation.
Guided bone regeneration for horizontal augmentation has been documented with high success rates and low complications when used with autologous bone and barrier membranes.
In a systematic review conducted by Kuchler U et al. in 2014, it was concluded that when horizontal ridge augmentations were performed in the anterior area with simultaneous or delayed placement of implants, a total survival success was achieved with a 4-year follow-up. The success of implant placement directly depends on adequate bone volume. Alveolar ridge augmentation is traditionally performed using autogenous bone graft; however, considerable morbidity is caused to the patient by resorting to other anatomical areas for bone procurement.
Conclusions
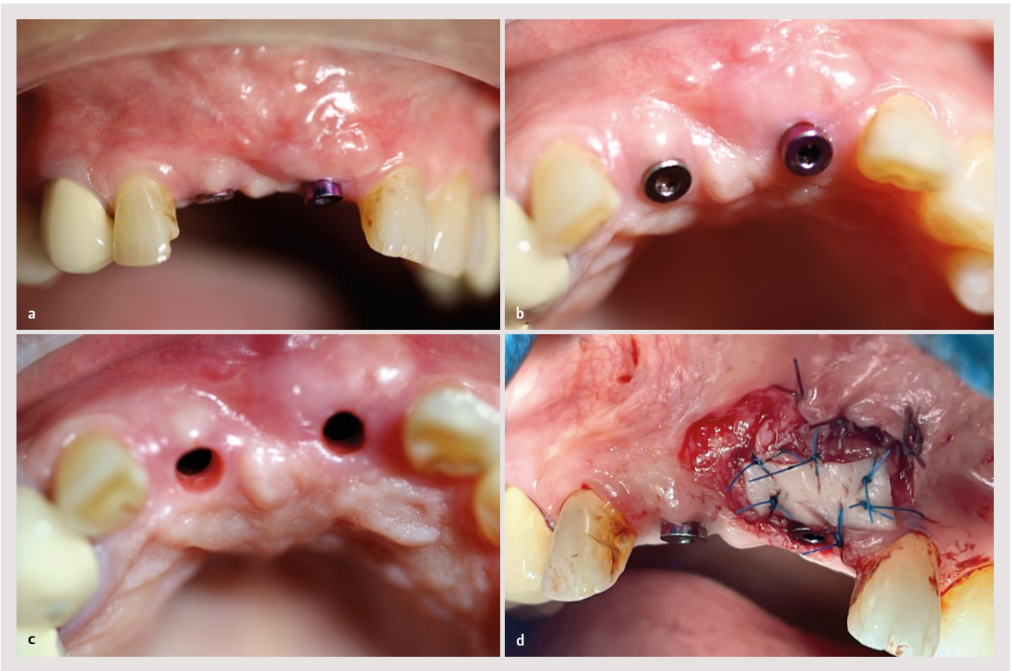
With the limitations inherent to a clinical case, we have shown that with the use of resorbable barriers, successful guided bone regeneration was achieved, making it possible to place implants in the treated area and the rehabilitation was favorable. Additionally, an increase in keratinized tissue was performed with a free graft, which, as highlighted in the literature, favors better plaque control afterwards and greater survival of the implants.
G. Perrone, J. Medina Moya
Bibliography
- Sculean A, Stavropoulos A, Bosshardt DD. Self-regenerative capacity of intraoral bone defects. J Clin Periodontol. 2019;23:34-36.
- Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19 Suppl:43-61. PMID: 15635945.
- Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005 Apr;25(2):113-119.
- Trombelli L, Farina R, Marzola A, Bozzi L, Liljenberg B, Lindhe J. Modeling and remodeling of human extraction sockets. J Clin Periodontol. 2008 Jul;35(7):630-9. Epub 2008 May 21. PMID: 18498382.
- Barone A, Aldini NN, Fini M, Giardino R, Calvo Guirado JL, Covani U. Xenograft versus extraction alone for ridge preservation after tooth removal: a clinical and histomorphometric study. J Periodontol. 2008 Aug;79(8):1370-7. PMID: 18672985.
- Araújo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implants Res. 2009 Jun;20(6):545-9. PMID: 19515033.
- Cardaropoli G, Araújo M, Lindhe J. Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J Clin Periodontol. 2003 Sep;30(9):809-818.
- Tan WL, Wong TL, Wong MC, Lang NP. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res. 2012 Feb;23 Suppl 5:1-21.
- Sanz-Sánchez I, Ortiz-Vigón A, Sanz-Martín I, Figue- ro E, Sanz M. Effectiveness of Lateral Bone Augmentation on the Alveolar Crest Dimension: A Systematic Review and Meta-analysis. J Dent Res. 2015 Sep;94(9 Suppl):128S-142S.
- Hämmerle CH, Jung RE, Yaman D, Lang NP. Ridge augmentation by applying bioresorbable membranes and de- proteinized bovine bone mineral: A report of twelve consecutive cases. Clin Oral Impl Res. 2008;19:19-25.
- Cordaro L, Amadé DS, Cordaro M. Clinical results of alveolar ridge augmentation with mandibular block bone grafts in partially edentulous patients prior to implant placement. Clin Oral Implants Res. 2002 Feb;13(1):103-11.
- Esposito M, Grusovin M, Felice P, Karatzopoulos G, Worthington H, Coulthard P. Interventions for replacing missing teeth: Horizontal and vertical bone augmentation techniques for dental implant treatment. Cochrane Database Syst Rev. 2009;4:CD003607.
- Mayhew D, Mendonca V, Murthy BVS. A review of ASA physical status - historical perspectives and modern developments. Anaesthesia. 2019 Mar;74(3):373-379. Epub 2019 Jan 15. PMID: 30648259.
- De Stavola L, TunKel J. The role played by a suspended external-internal suture in reducing marginal flap tension after bone reconstruction: a clinical prospective cohort study in the maxilla. Int J Oral Maxillofac Implants. 2014 Jul-Aug;29(4):921-6. PMID: 25032773.
- Revilla-León M, Fogarty R, Barrington JJ, Zandinejad A, Özcan M. Influence of Scan Body Design and Digital Implant Analogs on Implant Replica Position in Additively Manufactured Casts. J Prosthet Dent. 2020;124(2):202-210.
- Figueras-Alvarez O, Cantó-Navés O, Real-Voltas F, Roig M. Protocol for the Clinical Assessment of Passive Fit for Multiple Implant-supported Prostheses: A Dental Technique. J Prosthet Dent. 2020 Nov 2;S0022-3913(20)30488-1.
- Su H, Gonzalez-Martin O, Weisgold A, Lee E. Considerations of Implant Abutment and Crown Contour: Critical Contour and Subcritical Contour. Int J Periodont Restorative Dent. 2010;30(4):335-343.
- Hentenaar D, De Waal Y, Van WinKelhoff AJ, Raghoebar G, Meijer H. Influence of Cervical Crown Contour on Marginal Bone Loss around Platform-switched Bone-level Implants. Clin Oral Implants Res. 2019;30.S19 (2019): 359. Web.
- Buser D, Ingimarsson S, Dula K, Lussi A, Hirt HP, Belser UC. Long-term stability of osseointegrated implants in augmented bone: A 5-year prospective study in partially edentulous patients. Int J Periodontics Restorative Dent. 2002;22:109-117.
- Oryan A, Alidadi S, Moshiri A, Maffulli N. Bone regenerative medicine: classic options, novel strategies, and fu- ture directions. J Orthop Surg Res. 2014;9(1):18. Published 2014 Mar 17.
- Aghaloo T, Moy P. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007;22:49-70.
- Jensen J, Sindet-Pedersen S. Autogenous mandibular bone grafts and osseointegrated implants for reconstruction of the severely atrophied maxilla: a preliminary report. J Oral Maxillofac Surg. 1991;49:1277-1287.
- Misch C. Comparison of intraoral donor sites for onlay grafting prior to implant placement. Int J Oral Maxillofac Implants. 1997;12(6):767-776.
- Buser D, Bragger U, Lang N, Nyman S. Regeneration and enlargement of jaw bone using guided tissue regeneration. Clin Oral Implants Res. 1990; 1(1):22-32.
- Jovanovic S, SpieKermann H, Richter E. Bone regeneration around titanium dental implants in dehisced defect sites: A clinical study. Int J Oral Maxillofac Implants. 1992;7(2):233-245.
- Kuchler U, Von Arx T. Horizontal ridge augmentation in conjunction with or prior to implant placement in the anterior maxilla: A systematic review. Int J Oral Maxillofac Implants. 2014;29:14-24.
- Chiapasco M, Abati S, Vogel G. Clinical outcome of autogenous bone blocks or guided bone regeneration with e-PTFE membranes for the reconstruction of narrow edentulous ridges. Clin Oral Implants Res. 1999;10:278-288
