Temporomandibular Dysfunction Pain Syndrome. Orthognathic Surgery
Machine translation
Original article is written in ES language (link to read it) .
Introduction
Crossbite occurs in 10% of the adult population and is often associated with a dislocation, with or without reduction of the meniscus, of the temporomandibular joint (TMJ). Approximately 25% of patients with non-reducible meniscus dislocation have unilateral crossbite. Likely, in the juvenile stage of the patient, orthodontic treatment should be considered as a preventive measure; however, the same cannot be concluded for the correction of unilateral crossbite in an adult.
There is an ongoing debate, which is still unresolved, about whether orthodontics and/or orthognathic surgery for the treatment of jaw deformities with malocclusion are responsible for the reduction or resolution of the signs and symptoms of the joint. In a high percentage of patients, orthognathic surgery is responsible for the genesis of new joint problems, especially in patients who are not properly operated on or without a plan that has taken into account the previous joint pathology.
Clinical case
A 34-year-old patient comes to the office with pain and joint dysfunction. She has been experiencing clicking and limited opening (27 mm) for the past two years. The pain is more pronounced in the afternoon, radiating to the temporal area. The patient has been treated with physiotherapy and NSAIDs, but without improvement.
Diagnosis
This is a patient with joint symptoms who presents pain and dysfunction with occasional locking during opening. The origin of the joint problem is a functional lateral deviation of the mandible to the left, secondary to a premature contact due to maxillary compression.
Upon functional examination, we discovered the existence of an easily explored interference in the canines on the left side. This interference causes a discrepancy between maximum intercuspation and centric relation, generating a double occlusion. The left lateral deviation of the mandible is not skeletal but functional, originating from the interference in the canines due to maxillary compression.
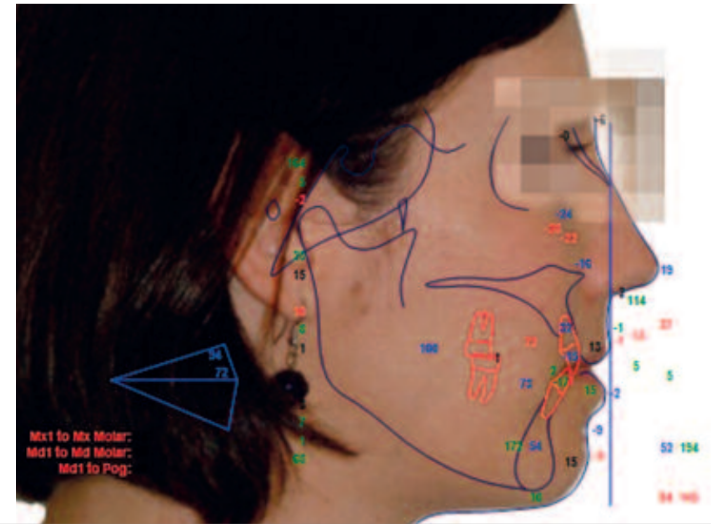
Facial Examination

Facially, there is a slight mandibular asymmetry towards the left, of functional origin. Likewise, there is also a severe bilateral maxillary compression, more pronounced on the left side, and a maxillary vertical excess, with a significantly increased lip-to-tooth relationship, both anteriorly and posteriorly. The upper midline is centered relative to its bony base and slightly tilted to the left. Anteroposteriorly, it presents a straight profile, with a slight maxillomandibular retrusion.
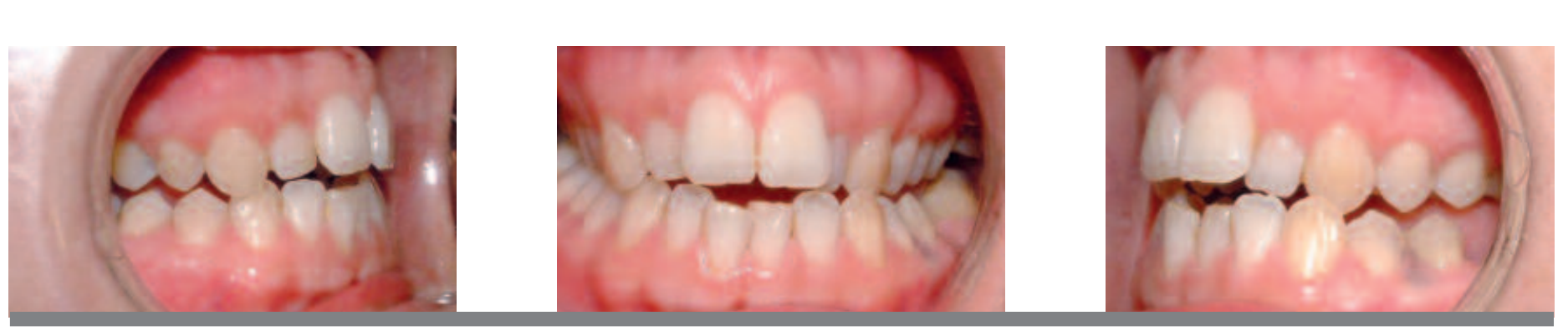
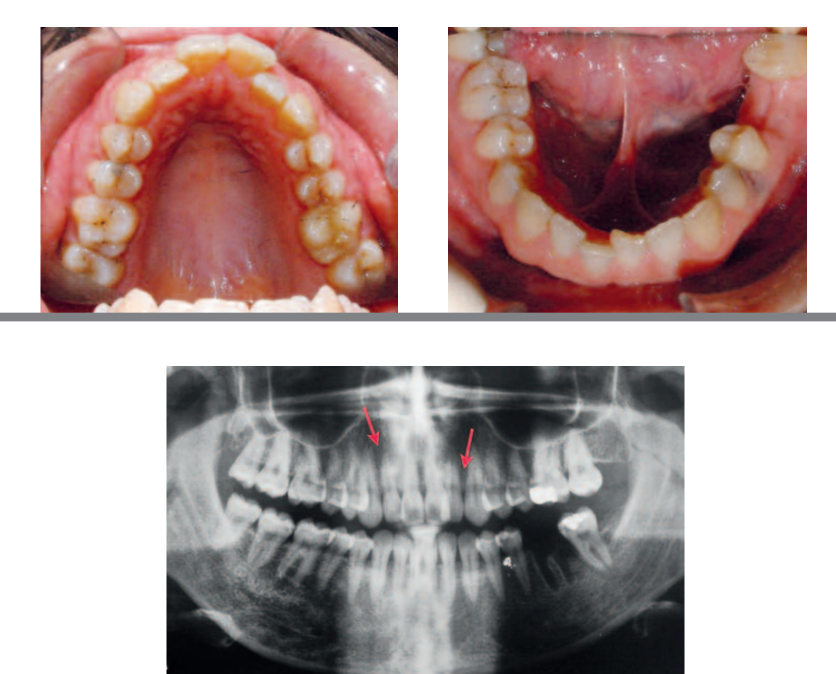
Intraoral Examination

In the functional examination, we discovered the existence of an interference in canines, which causes a discrepancy between maximum intercuspation and centric relation, and is the origin of a double occlusion. In maximum intercuspation, the patient presented class II canine and molar, with a crossbite of the lateral incisor to the second molar on the left side, and a discrepancy of midlines. In centric relation, the midlines are centered, as it is a functional deviation.
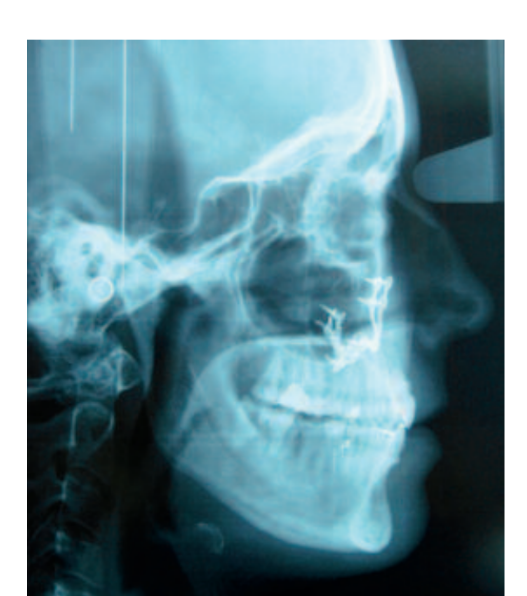
Study of X-rays
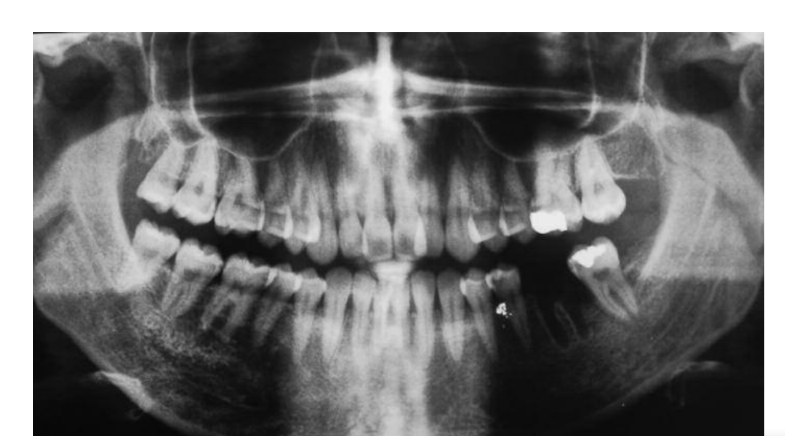
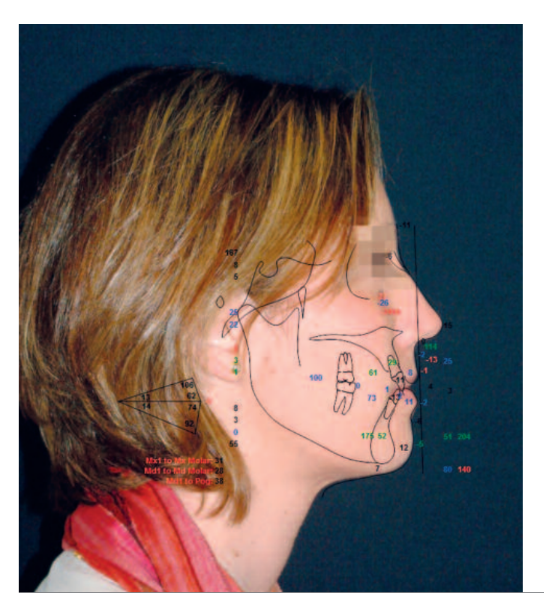
The maxillary transverse problem will be solved with maxillary fragmentation, after orthodontic decompensation. A surgical maxillary expansion of 2 mm on each side is estimated. The monomaxillary surgery consists of a bilateral segmented Lefort, with anterior and posterior impaction and a slight advancement of 3 mm.
Skeletal treatment plan
Functional treatment plan
By being able to easily register the centric relation in a repeatable and stable position, we discard the option of placing a diagnostic splint before orthodontic decompensation. During the pre-surgical orthodontic preparation, it will be necessary to stabilize the occlusion with posterior bite raises at the minimum vertical dimension. The goal is to avoid interferences and promote bilateral function.
Pre-surgical dental treatment sequence

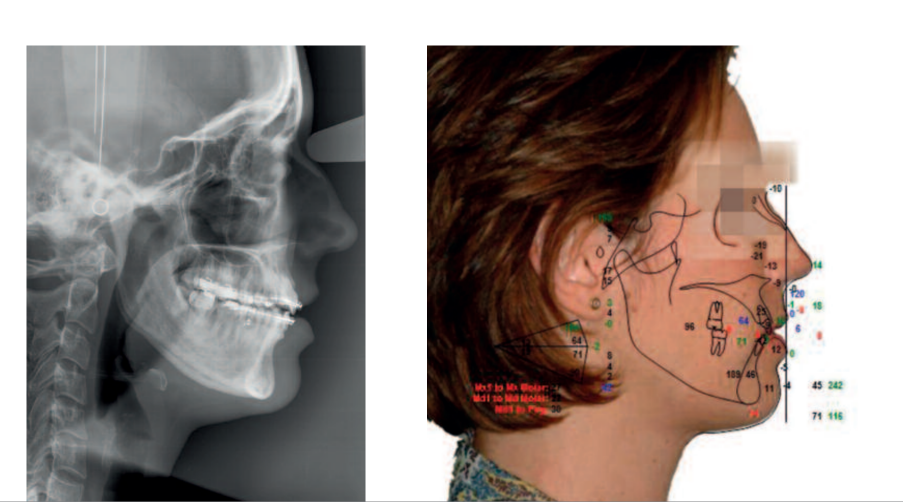
The orthodontic treatment plan aims to compensate the arches anteroposteriorly, recovering the inclination of the incisors according to the norm. Vertically, the Spee curve will be leveled and transversely the torsion of the teeth in the posterior sectors will be recovered, leveling the Wilson curve. Our orthodontic treatment sequence indicates that, after recovering the dental inclinations, pre-surgically we will have a crossbite on the left side, with a need to surgically expand the maxilla by 3 mm at the canine level and 6 mm in the molar area. It is decided to fragment between laterals and canines. Our treatment plan aims to generate root divergences pre-surgically.
Surgical procedure
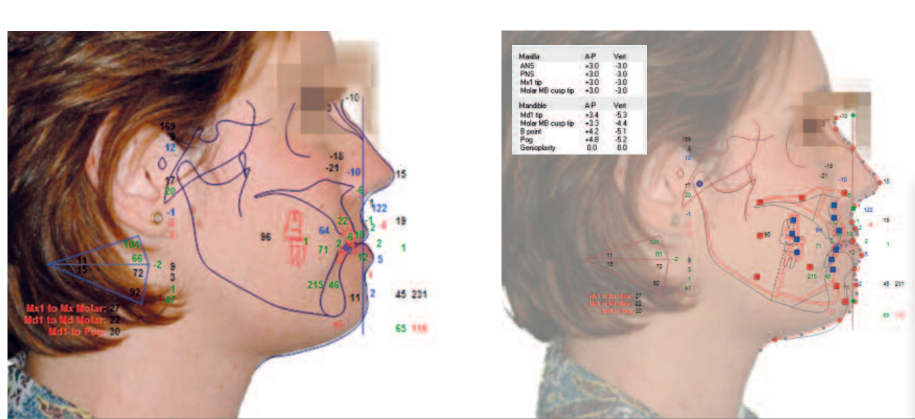
The surgery consists of a segmented Lefort I monomaxillary. Under general anesthesia, a vestibular incision is made to first carry out the marking of the vertical osteotomies between the lateral and the canine. In this case, we perform them with a BTI ultrasonic scalpel to avoid periodontal and vestibular complications. The osteotomy impacts 3 mm in the maxilla with an advancement of 3 mm.
The maxilla expands 2.5 mm at the height of the canine and 6 mm at the molar. The osteotomies are fixed semi-rigidly with plates of 1.6 mm and 2 mm. Subsequently, the passive fit to the splint fixed in the mandible is checked, verifying the accuracy of the movements with model analysis. A wire is placed in ANS for orthodontic traction of the premaxilla. The mandible is advanced freely, moving forward 4.7 mm and ascending 5 mm, taking the pogonion as a reference.
It is decided to remove the splint in the operating room, as it presents a stable occlusion that we would maintain in the first few days with soft elastics. The patient remains hospitalized for 24 hours and maintains a semi-soft diet for three weeks.
Post-surgical treatment


Weekly, the fragmented arches were replaced by continuous arches, which were changed progressively. The thickness of the latter was: 0.16 Niti, 16 x 22 Niti, 19 x 25 Niti, and 19 x 25 steel, to actively maintain, buccally, the control of the maxillary fragmentation. We tried to increase the thickness of the arches as soon as possible for transverse control.
Nightly cross elastics were used on premolars during the 16 x 25 Niti and 19 x 25 Niti, to ensure maxillary expansion.
At the end of the treatment, we took care of the aesthetic aspects: Bolton discrepancy (which the patient decided not to restore with composite veneers on upper laterals), whitening, and gingivectomy.

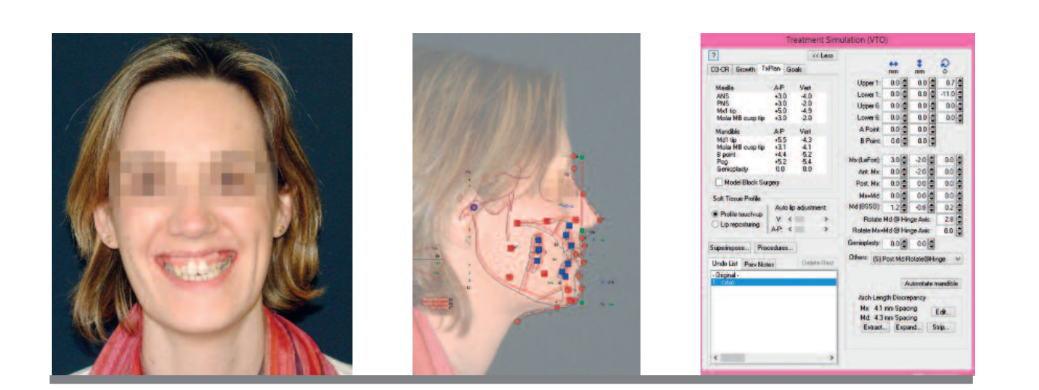
Facial Change
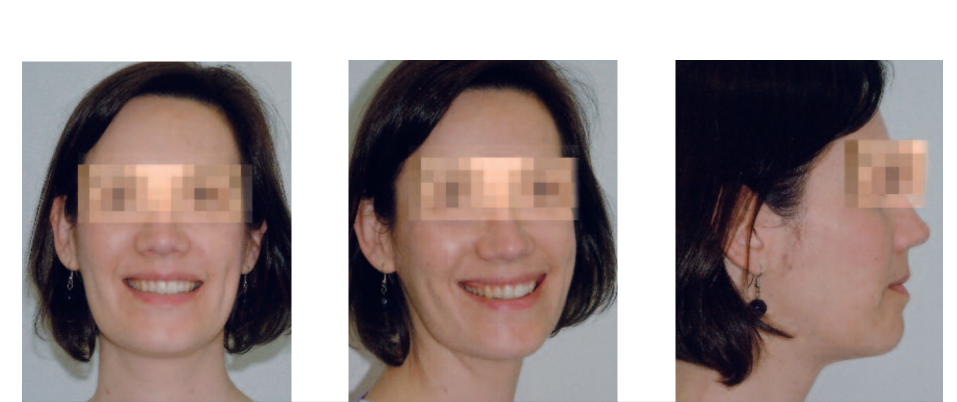
Before and after

After three years with a fixed retention from canine to canine and a removable upper retention of the exiss type, the results remain stable and the patient has no joint discomfort. A slight relapse of the expansion on the left side in the molar area is observed.
The rehabilitation of the absence of the lower left molar was performed in a more vestibular position than we would have liked and was compensated with good selective carving. The patient functions bilaterally in minimal vertical dimension.
Intraoral Change

Discussion
The treatment of patients with joint pathology and concomitant dentofacial deformity constitutes an unresolved issue and is subject to debate. Many researchers believe that orthognathic surgery helps improve joint problems and that restoring occlusal harmony leads to the resolution of symptoms. However, authors like Wolfort argue the opposite: that in patients with orthognathic surgery and unresolved joint pathology, joint symptoms worsen and there is a higher likelihood of occlusal instability, joint dysfunction, condylar resorption, and overall joint deterioration, which will result in relapse, resorption, pain, and/or malocclusion.
Patients with meniscus displacement after surgery will undergo an adaptation process in the bilaminar zone with potential occlusal influences. In patients where condylar fixation causes overload, a change in the condylar surface will occur most of the time, flattening and resorbing the cartilaginous matrix. Additionally, restoring a dynamic and physiological occlusion promotes adequate joint function.
In this patient with pain, parafunctions, and joint alteration, an improvement in her pathology was observed thanks to an integrated restorative treatment. As a general rule, patients with joint pain and dysfunction should be treated beforehand. The correction of altered occlusion dynamically and statically influences the neuromuscular programming of the joint. In a very high percentage, joint function improves after correction with orthodontics and orthognathic surgery. In this patient, a total resolution of symptoms was observed, as well as an aesthetic and respiratory occlusal improvement after the combined treatment.
César Colmenero Ruiz, Elena Bonilla Morente, Silvia Rosón Gómez, Carmen Torres de la Torre
Bibliography
- Roth RH, Ware WH. Orthognathic treatment in patients with TMJ pain dysfunction. J. Clin. Urthod.1980: 108-120.
- Wolford VM, Reiche-Fiscle O, Mehra P. Changes in the TMJ dysfunction after orthognathic surgery. J. Oral Maxillofac. Surg. 2002; 61: 655-659.
- Westermark A, Shayeghi F, Thor A. TMJ dysfunction in 1516 patients before and after orthognathic surgery. Int. J. Adult Orthodon. Orthognathic Surg. 2001; 16: 145-51.
- Katabef RW, Westenson R, Tallen NR. Orthodontics and TMJ internal derangements. Am. J. Orthod. Dentofacial Orthod. 1996; 109:515-20.
- Kirveskari P, Bell Y, Solonem M. Effect of elimination of occlusal interference of signs and symptoms of craniomandibular disorder in young adults. J. Orth. Rehabilit. 1987; 16-71-26.
