Facial Asymmetries: Orthodontics and Orthognathic Surgery
Machine translation
Original article is written in ES language (link to read it) .
Analysis
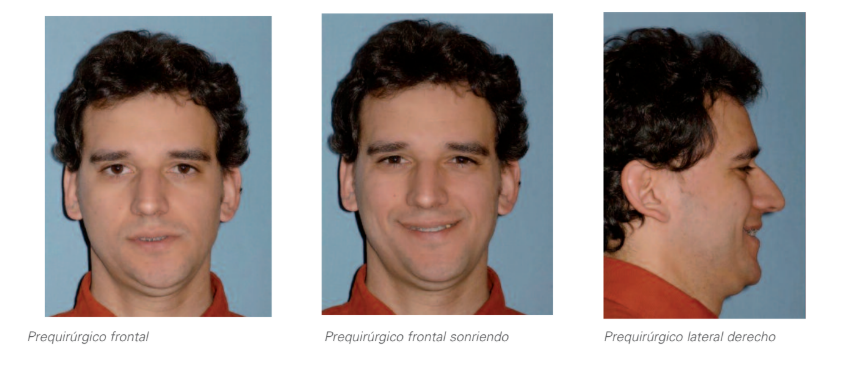
The patient came for evaluation and treatment of dentofacial deformity, consisting of maxillary and mandibular asymmetry and left-sided temporomandibular dysfunction pain syndrome.
The examination showed significant asymmetry with mandibular deviation to the left and significant inclination of the occlusal plane. Additionally, the left temporomandibular joint experienced joint locking with reduction and intermittent episodes of pain and functional incapacity. There were multiple dental compensations, so the patient was referred to the orthodontist for proper preoperative preparation.
Anamnesis
Name: C.G.
Age: 34 years and 9 months.
Medical history: No interest
Reason for consultation: Referred by his maxillofacial surgeon due to his asymmetry.
Diagnosis
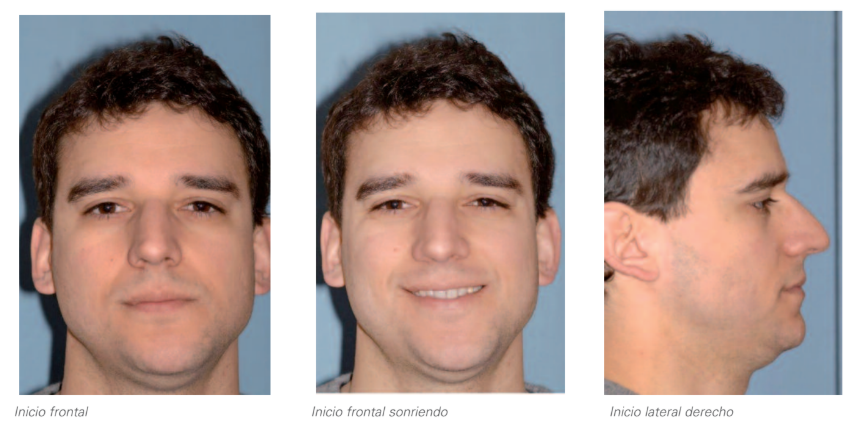
1. Extraoral analysis
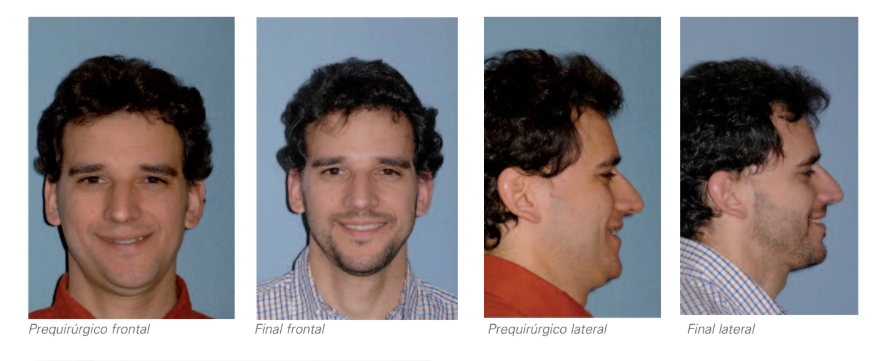
- Facial asymmetry: Deviation of the chin to the left.
- Facial thirds are proportionate.
- Adequate exposure of incisors at rest and in smile.
- In smile, the inclination of the upper occlusal plane and the upper dental midline is observed.
- Straight profile.
- Minimal mandibular contour.
- Double chin due to excess submental fat deposition.
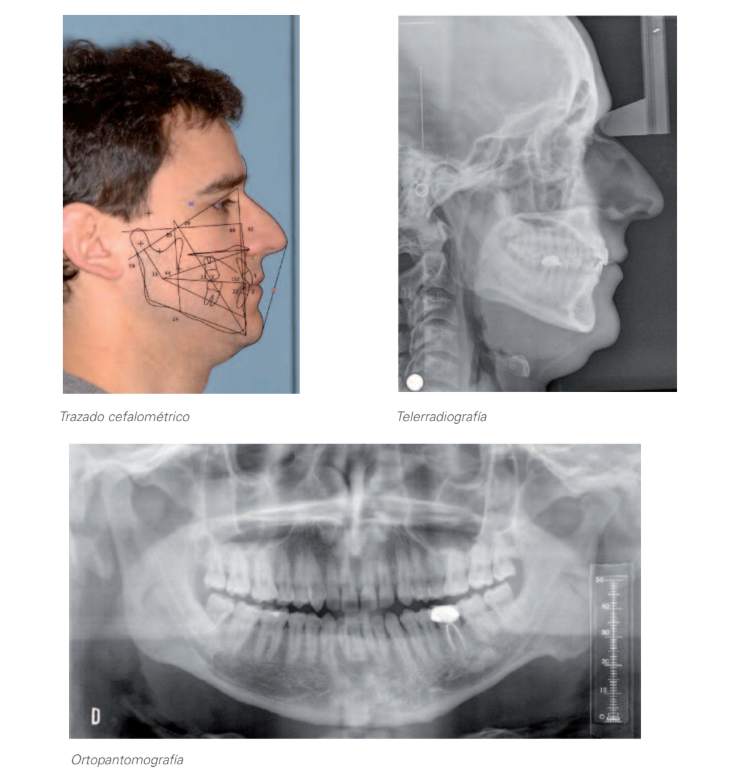
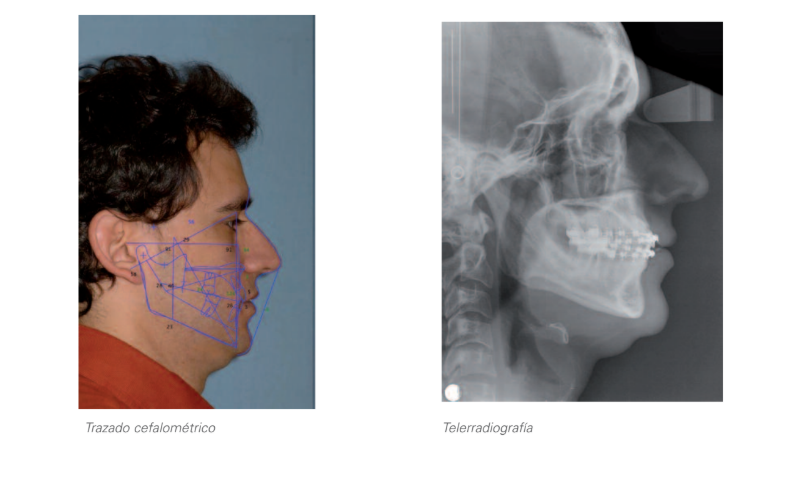
2. Radiographic analysis
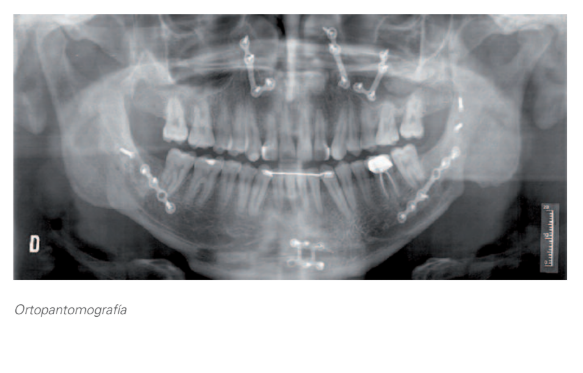
2.1. Orthopantomography:
- Permanent dentition.
- Morphological alteration in the left condyle which is also smaller in size.
- Presence of erupted wisdom teeth.
2.2.Lateral cephalometric radiography and cephalometric tracing:
- Mesofacial.
- Class I skeletal.
- Incisors correctly positioned relative to their bony bases.
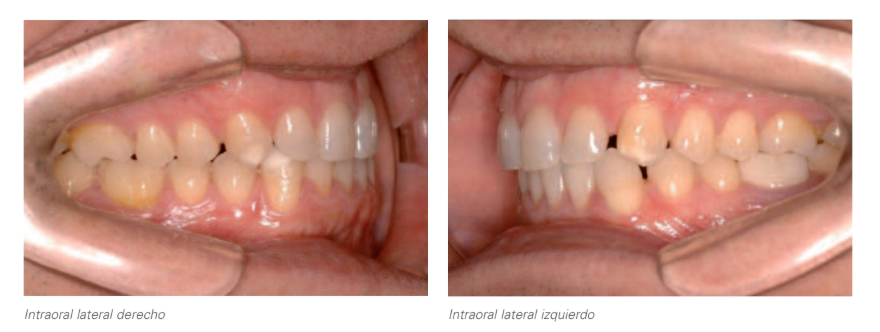
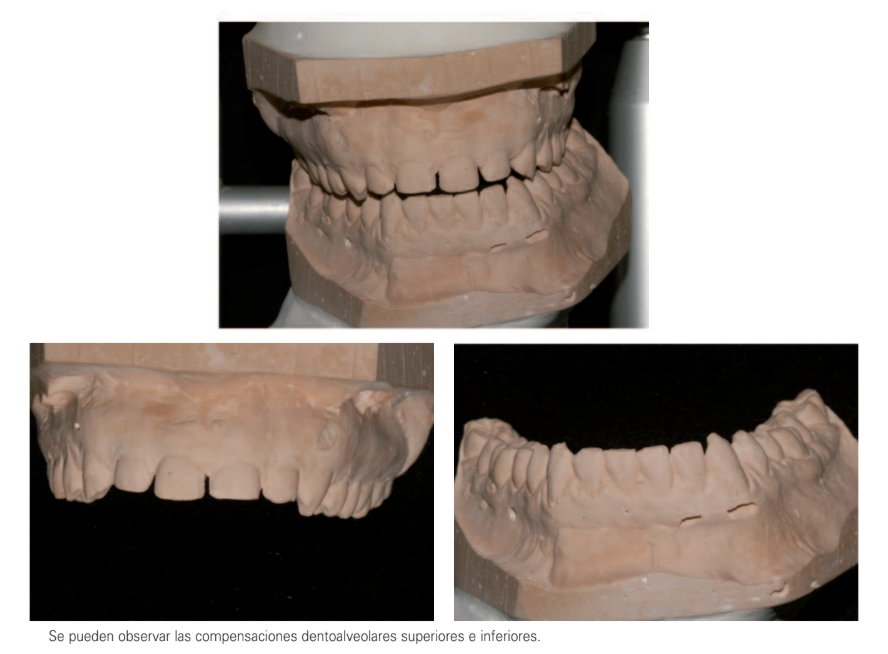
3. Intraoral analysis
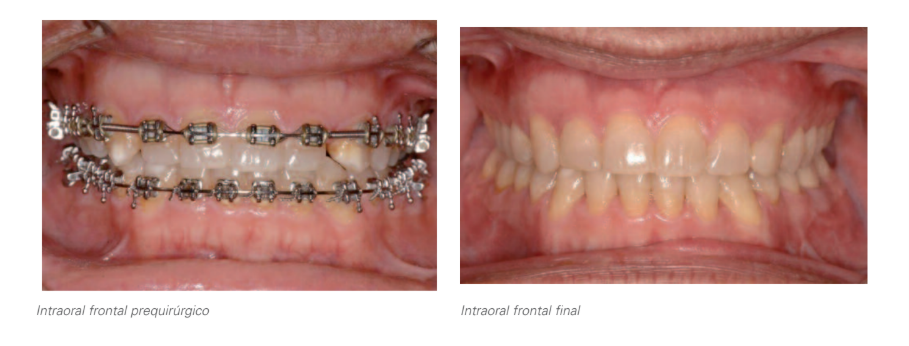
- Deviation of the lower midline to the left by 2.5 mm due to bony cause (alteration of the morphology and size of the left condyle).
- Inclination of the anterior and posterior occlusal plane.
- Dentoalveolar compensations to the asymmetry in both arches:
- First and third quadrants with excessive corono-lingual torque (except for 38 which presents a marked corono-buccal torsion).
- Second and fourth quadrants with marked corono-buccal torque, being more pronounced at the level of 48.
- Increased right canine prominence. Decreased left canine prominence.
- Crossbite of 18-48 and 28-38.
- Overjet: 2.5 mm.
- Positive skeletal-dental discrepancy in both arches.
- Superior Bolton discrepancy due to maxillary deficiency.
- Right side: Class III molar and Class I canine.
- Left side: Class I molar and canine.
- Overbite: 2 mm.
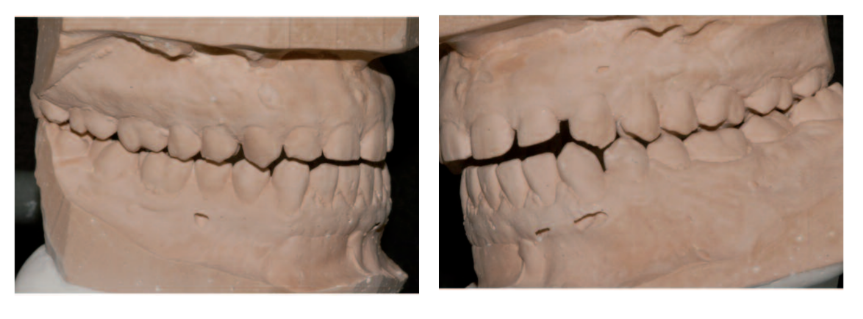
Initial Study

Mounting on articulator
Treatment plan
Once the skeletal etiology of the asymmetry was identified, as well as the generated dentoalveolar compensations, a combined treatment of orthodontics and orthognathic surgery was proposed to the patient, in which the pre-surgical orthodontic phase would consist of:
- Eliminating or reducing the existing dentoalveolar compensations in both arches.
- Opening spaces distal to the upper lateral incisors for subsequent reconstruction with composite in order to adjust the upper tooth size to the lower one.


Surgery
Under general anesthesia, nasotracheal intubation was performed.
A multisegmental Lefort I osteotomy was performed to achieve expansion and level the upper arch. The more aesthetic plan considered was to lower the left maxilla, using the right maxilla as a filter, and non-resorbable hydroxyapatite wedges were placed that lowered the left posterior maxilla by 6 mm at the level of the first molar and 3 mm at the level of the canine. The right maxilla pivoted at the level of the first molar and the maxilla was advanced 6 mm sagittally.
The osteotomies were rigidly fixed with plates and screws on the intermediate splint.
Subsequently, passive adaptation to the intermediate splint was verified and septoplasty was performed.
Once the maxilla was fixed, a significant premature contact was generated on the left side due to the maxillary descent, which posteriorly rotated the mandible, thus increasing the magnitude of left to right translation to be performed by the mandible.
The left mandibular segment advanced 11 mm and rotated counterclockwise, while the right segment advanced 3 mm to center in order to achieve occlusion with the maxilla advanced sagittally.
The osteotomies were fixed with bicortical plates and screws.
Finally, advancement genioplasty, right translation, and vertical augmentation were performed.
The postoperative course was marked by moderate inflammation, and the patient was discharged from the hospital after 36 hours.
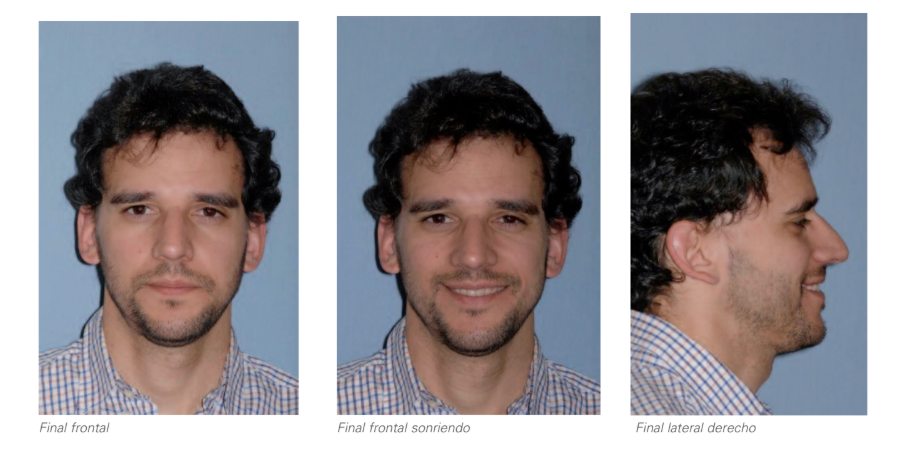
Final study





Discussion
Faces are rarely symmetrical. Asymmetries must be considered in three dimensions. In this case, it included the maxilla and mandible with a significant inclination of the occlusal plane. In preparing these cases, both the anterior and posterior inclination of the plane must be taken into account, along with that of the mandibular ridge.
The maxillary inclination is clinically evaluated based on a measurement at the inner angles. If these are symmetrical and there are no orbital alterations, it is subsequently verified on articulated models in an articulator with facial arc transfer.
In this patient, after a thorough study, it was decided to resolve the inclination by lowering the maxilla to elongate the face and sagittally project the maxilla and subsequently the mandible. The contralateral side was taken as the fulcrum point.
The mandible on the left side, when posteriorly rotated, required a significant advancement to achieve centering, and extremely rigid fixation was used.
The genioplasty ultimately centered and elongated the chin.
This way, the inclination was altered and simultaneously the lower third of the face was elongated, resulting in a longer face, without the stigmas of a long face, and along with the advancement of the maxillae, skeletal support was increased, leading to better soft tissue support and, of course, a symmetrical face was also achieved.
The examination of the face and the understanding of the repercussions that vertical changes in the maxilla have on the mandible when subsequently transferring it horizontally are key to improving the balance and harmony of the face, while also achieving skeletal expansion.
Technically, the management of the mandibular angles in these three-dimensional alterations is complicated and often requires modifications to the design of the Obwegeser sagittal osteotomy.
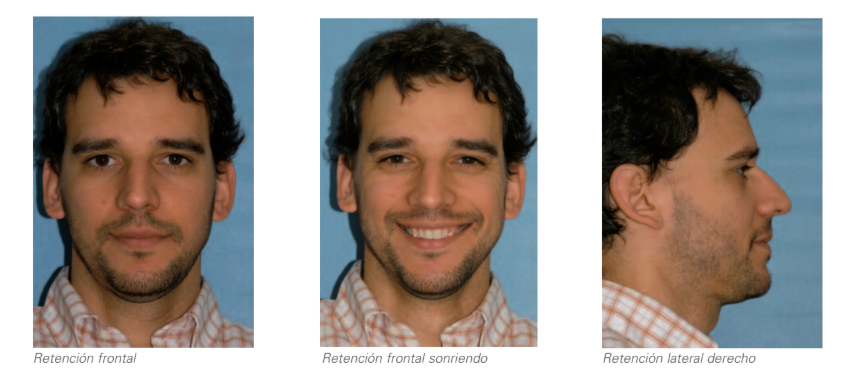
Pre-surgical comparison/final situation
César Colmenero Ruiz, Fe Serrano Madrigal, Javier Prieto Serrano, Martínez Iturriaga
Bibliography
- Reyneke JP. Essentials of orthognathic surgery, pp. 240-245.
- Buton KW. The use of triangle analysis cephalometric analysis in three dimensions J. Oms 1984, chap. 12, pp. 62-70
- Rosen HN. Aesthetic refinements in genioplasty the role of facial dysfunction. PRS. 95, pp. 463-471, 1995.
- Obwegesser HL. Mandibular growth anomalies. Rou 2, pp. 215-231.
