Preclinical randomized controlled trial of bilateral discectomy versus bilateral discopexy in Black Merino sheep temporomandibular joint: TEMPOJIMS – Phase 1-histologic, imaging and body weight results
Abstract
Introduction: The role of temporomandibular joint (TMJ) surgery is not well defined due to a lack of quality randomized controlled clinical trials, comparing different TMJ surgical treatments with medical and placebo interventions. The temporomandibular joint interposal study (TEMPOJIMS) is a rigorous preclinical trial divided in 2 phases. In phase 1 the authors investigated the role of the TMJ disc and in phase 2 the authors evaluated 3 different interposal materials. The present work of TEMPOJIMS e phase 1, aims to evaluate histopathologic and imaging changes of bilateral discectomy and discopexy in Black Merino sheep TMJ, using a high-quality trial following the ARRIVE guidelines.
Material and methods: This randomized, blinded and controlled preclinical trial was conducted in 9 Black Merino sheep to investigate histopathologic (primary outcome), imaging and body weight (secondary outcomes) changes after bilateral discectomy, discopexy and sham surgery.
Results: Significant changes were noticed in discectomy group, both in imaging and histopathologic analyses. Body weight changes were most pronounced in the discectomy group in the first 4 months after surgery with recovery to baseline weight 6 months after surgery. Discopexy induced nonsignificant changes in histopathologic, imaging and body weight analyses.
Conclusions: This study reinforces the importance of developing an effective interposal material to substitute the TMJ disc and the need to explore the molecular mechanisms that underlie TMJ cartilage degeneration. The study design proposed in TEMPOJIMS represents an important progress towards future rigorous TMJ investigations.
Introduction
In severe temporomandibular disorders (TMD) the standard treatment is mostly surgical (Dimitroulis, 2013). However, the role of temporomandibular joint (TMJ) surgery is not well defined (Dimitroulis, 2005) due to a lack of quality randomized controlled clinical trials, comparing TMJ surgical treatment with medical treatment and placebo (Reston and Turkelson, 2003; Souza et al.,2012). TMJ open surgical approaches for severe disorders include mostly discectomy or discopexy. In cases where nothing in the joint is salvageable, a total joint replacement may be necessary (Dimitroulis, 2013). Despite the large number of discectomy procedures performed annually, we are not aware of any rigorously performed, randomized, controlled trials that have investigated, in human or animal, the effectiveness of discectomy, compared with discopexy, bioengineered interposal material and sham surgical interventions. Previous studies stated a significant increase in TMJ osteoarthrosis (OA), following discectomy with and without replacement of the disc with an interpositional implant (93% and 100%, respectively). These authors presented a reduced incidence of OA (62%) when using discopexy. Still, this technique was associated with frequent relapse, requiring a secondary discectomy (Trumpy and Lyberg, 1995). These outcomes clearly demonstrate the importance of further studies to deeper understand the effects of surgery and progress for future development of interposal materials.
Most clinical trials use imaging to classify the TMJ degenerative process (Eriksson and Westesson, 2001). Computed tomography (CT) is a valuable tool to evaluate TMJ OA (Cordeiro et al., 2016) and it is used by most clinical studies to evaluate articular changes (Boman, 1947; Eriksson and Westesson, 1985; Hall, 1985; Kiehn and Desprez, 1962; Silver, 1984; Takaku et al., 1994; Tolvanen et al., 1988). Two important long-term follow-up clinical studies presented condylar flattening and sclerosis after discectomy, but these were not associated with TMJ symptoms (Eriksson and Westesson, 1985; Hall, 1985; Silver, 1984; Tolvanen et al., 1988). Opposingly, The Desprez group (1962) suggested an association of articular erosion with pain in the post-operative period (Kiehn and Desprez,1962). While imaging modalities are key measures in clinical research, preclinical studies provide a unique chance to also obtain histologic pathology to better understand TMJ surgery-induced changes and improve knowledge for interposal materials research. Previous preclinical studies have evaluated histologic and imaging outcomes using study designs with a potential sources of bias (selection bias, measurement bias, non-randomization, non-blinded outcome assessment) increasing risk of errors in the results of the study, and in further conclusions (Block and Bouvier, 1990; Choukas et al., 1969; Hagandora and Almorza, 2012; Laurell et al., 1987; Macher et al., 1992; Ogi et al., 1996).
The Temporomandibular Joint Interposal Material Study (TEM-POJIMS) was planned with a rigorous pre-published design (Ângelo et al., 2017) according to the ARRIVE guidelines (Kilkenny et al., 2010). This first high-quality randomized preclinical study, performed in Black Merino sheep, was required to increase the translational power of further studies and to progress in future treatment options for patients undergoing surgery for TMJ disc replacement. TEMPOJIMS is divided into phase 1 and 2. Phase 1 was a randomized, blinded preclinical trial designed to investigate the TMJ imaging (CT), histopathologic, and body weight changes in sheep after bilateral discectomy, discopexy or sham surgery. Phase 2 uses the same design to test different bioengineering scaffolds to replace the TMJ disc in sheep. It is critical that all assessments are performed and classified independently by two professionals, from each area, who are blinded to intervention. In both phases the primary outcome was the histological grading of TMJ pathology. The main goal of the present investigation was to examine the effects of bilateral surgery over the phase 1 outcomes.
Material and methods
Study design
The rationale and protocol for the TEMPOJIMS preclinical trial are publicly available (Ângelo et al., 2017). An independent data and safety monitoring board unblinded preclinical results. The study was approved by the Portuguese National Authority for Animal Health registered with number 026618. The study design and organization respected the ARRIVE guidelines (Kilkenny et al., 2010).
Study population and sample
Relevant preclinical TMJ studies have been conducted in sheep (Ishimaru and Goss, 1992; Matsuura et al., 2006; Miyamoto et al., 1999; Ogi et al., 1996; Takaishi et al., 2007), and to decrease biological variability in TEMPOJIMS results, a specific purebred Black Merino sheep strain was used (Ângelo DF et., 2017). In 2016, our group performed an anatomic, biomechanical and histologic study of Black Merino sheep TMJ highlighting the potential of this animal to conduct preclinical trials in the TMJ domain (Angelo et al., 2016). The following eligibility criteria were used: certified Black Merino sheep, adult (aged between 2 and 5 years), female, and in good health condition (evaluation was performed by veterinaries, also confirming normal dentition).
Randomization
The randomization process was performed by a statistical group, not enrolled in the outcome assessments. Ten sheep were randomly allocated to the intervention group: bilateral sham surgery (n = 3), bilateral discectomy (n = 3), bilateral discopexy (n = 3), and backup group (n = 1). One backup sheep was planned to be used if death occurred due to anaesthesia, or other complication not related to surgical intervention. The allocation to each randomized group was performed preoperatively by sealed envelope.
Procedures
Ten eligible sheep were selected and baseline body weight was measured at days 11, 10, and 9 before surgery. Transportation to surgical facilities was performed 5 days before surgery to avoid animal stress and allow familiarization to the temporary accommodation. Head CT-scan was performed on the day of surgery taking advantage of pre-anaesthesia sedation (supplementary material doc 1). The surgical team was not blinded to treatment allocation given the type of intervention; however surgical team members were not involved in outcome assessment. Serious adverse events were defined as events that were fatal or life-threatening or persistent disability, or that resulted in death, over 10% weight loss per week, or clinically significant hazard or harm to the animal.
Intervention phase
Anaesthesia protocol
Fasting and water restriction were required 24 h before surgery. Sedation was performed with diazepam (0.5 mg/kg i.v.), followed by anaesthesia induction with ketamine (5 mg/kg i.v.). Oral intubation was performed and anaesthesia was maintained with isoflurane (1.5e2%). To guarantee animal analgesia, meloxicam (0.5 mg/kg i.v, bid) was administered on the day of surgery up until 4 days post-operatively. Antibiotic prophylaxis with amoxicillin and clavulanic acid (50 mg/kg i.v. bid) was used for 5 days, after surgeries.
Surgical intervention
In all animals, the surgical site was shaved, the skin prepared with povidone iodine solution, and isolated with sterile drapes according to standard surgical procedures. With a 15-scalpel blade a 6 cm long pre-auricular skin incision was performed followed by blunt dissection of the soft tissue covering the joint, to expose the articular capsule. Tissue retractors were used to maintain exposure of the surgical field. In the sham group (n = 3) TMJ articular capsule was not incised, and the wound was closed in 3 layers (muscular, subcutaneous and skin) with Vicryl 3/0. In the remaining animals, the joint capsule was incised and the disc and its attachments were identified. In the discectomy group (n = 3), the disc was exposed and using iris scissors the lateral, anterior and posterior attachments were dissected, allowing exposure and transection of the medial attachment and removal of the intact disc. In the discopexy group (n = 3), the lateral and posterior disc attachments were sharply detached using an iris scissor. A 4-mm triangular segment of the retrodiscal tissue was removed and then sutured with PDS 3/0. The wound, including joint capsule, was closed in 4 layers (joint capsule, muscular, subcutaneous and skin) with Vicryl 3/0.
Follow-up assessments
Ten days after surgery, animals were transported to TEMPOJIMS facilities (Ângelo et al., 2017). From the 19th to 21st day after surgery, follow-up secondary outcomes were recorded, which were repeated every 30 days for 6 months (T1 to T6, respectively). Data from T0-T6 were calculated on a mean of the 3-day measurements of each month. Six months after the intervention, immediately after euthanasia, all animals had a second CT scan and the TMJ block was removed to histology.
Outcomes
Histologic analysis: Intact TMJ was removed using a necropsy bone oscillatory saw according to the following anatomic references: cranial e cranial aspect of coronoid process in the union region of the zygomatic process; caudal e external to acoustic meatus; dorsal e the squamous temporal bone; and ventral - 2 cm below the acoustic meatus in the zone of stylo-hyoid angle. The joints were fixed in 10% buffered formalin for 24 h and stored in 70% ethanol. Decalcification was obtained by immersion in 10% formic acid in 5% formalin for 20 days with solution changed every 2 days, after which the articulations were cut sagittally through the whole condyle. TMJ articulations were then immersed in three graded methyl salicylate/paraffin mixtures, embedded in paraffin and sectioned through to the central part of TMJ. Four micron sections were mounted on glass slides, heated for 1 h at 65ºC, de-waxed with 3 cycles of 5 min with xylene, and stained with toluidine blue and fast green as previously described (Little et al., 2010). Slides identified by a number code were randomized and shipped to the Raymond Purves Labs for scoring by 2 blinded independent assessors experienced in evaluating sheep joint histopathology (CBL, MMS).
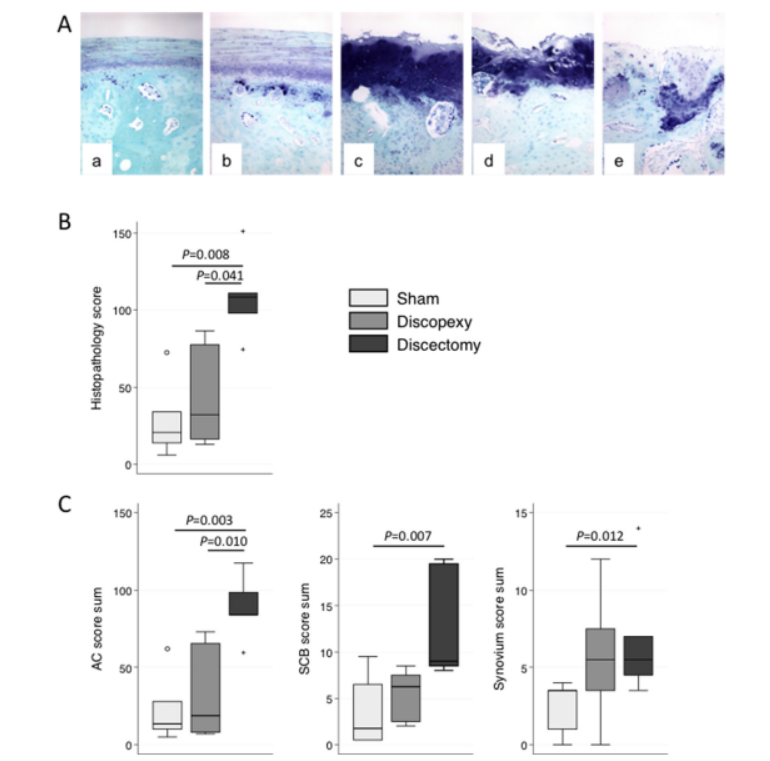
As the normal histomorphology of the TMJ is quite distinct from cartilage in appendicular synovial joints (Murphy et al., 2013) (Fig. 1Aa), a modification of a published scoring system specific for the TMJ was used (Li et al., 2014) (supplementary material doc2). Briefly, the mandibular and temporal cartilage (structure, cell number, shape and cloning, and proteoglycan content and distribution), tidemark, cement line, and subchondral bone (structure, osteocyte number, osteoblast activation, vascular invasion, and calcified cartilage islands) were separately scored from 0 (normal) to 3 (>70% abnormal). Additionally, the temporal and retrodiscal synovial hyperplasia, fibrosis and inflammatory cell infiltration were also scored from 0 to 3. The summed cartilage (possible maximum score 60 in each condyle), subchondral bone (possible maximum score 15 in each condyle), synovial (possible maximum score 9 in each site), and total (possible maximum score 168) histopathology scores were calculated.
Imaging analysis: Imaging evaluation was performed and classified independently by 2 experienced radiologists (RS, LN) who were blinded to the intervention using the outlined criteria (supplementary material doc 3).
Body mass assessment: Sheep were weighed immediately after eating 150-gr of dry pellets. Body mass assessments were performed by 2 trained evaluators who were not affiliated with the intervention.
Statistical analysis
Statistical analyses were performed using either the Statistical Package for Social Sciences (IBM SPSS, version 22.0) or Statistics/ data Analysis (STATA-corporation version 14.2). The histopathology scores for each parameter in each section of the 2 evaluators were averaged, and following un-blinding the median scores (and score summations) for each treatment group were calculated. Differences between treatments were analysed by mixed ordinal logistic regression.
A one-way Analysis of Variance (ANOVA) was performed for cross-sectional analysis, to compare the outcome variables in the three levels of the independent variable before and after the random treatment group assignment. For longitudinal analysis, a one-way ANOVA with repeated measures was performed taking as within-subjects effects observations after surgery (T1-T6) for all conditions. Primary analysis tested the effects of the surgical intervention using series pre-test and post-test. Body mass and imaging score were used as dependent variables for degenerative process. Body mass was measured 3 times in the pre-test for supporting invariance concerning the outcome measures before the clinical intervention. The secondary analysis (post-test) assessed the outcomes measuring 3 times, in 6 time-points, one per month at the same place, date and hour as in pre-test (Ângelo et al., 2017). To analyse imaging results, non-parametric tests were performed attending to the sample size and the non-normality of the distribution for most variables in each group, ShapiroeWilk test ≤ .82, p ≤ .091. KruskaleWallis tests were performed for group comparisons, with Bonferroni test for post-hoc multiple comparisons. Partial eta squared (η2p) and Cohen's d were used for effect size calculations. Cohen's categories were used to evaluate the magnitude of these effect sizes (small if 0 ≤ |d|≤ 0.5, medium if 0.5 < |d|≤ 0.8, and large if |d| > 0.8).
Results
At baseline, no differences between groups were observed in body mass (sham group: 55.1 ± 2.7 kg, discopexy group: 62.3 ± 6.0 kg, discectomy group: 67.3 ± 10.2, p > .10).
Histologic results
The morphological appearance of the cartilage and bone in sham operated joints was consistent with that previously described as normal TMJ (Murphy et al., 2013; Li et al., 2015) (Fig. 1Aa). The superficial half of the cartilage depth had a distinct laminar appearance, with sparse flattened cells and limited proteoglycan staining more intense with depth. Beneath this, there was a layer densely populated with cells that had a mesenchymal appearance, and more intense diffuse matrix proteoglycan staining. The deepest cartilage layer contained mature and/or hypertrophic chondrocytes often surrounded by a proteoglycan rich peri-cellular matrix but little or no inter-territorial proteoglycan. A tidemark separating the upper two layers from the deepest cartilage layers could be observed in some sections, suggesting the lower zone was calcified. An indistinct cement line demarcated the subchondral bone which contained evenly distributed osteocytes in lacunae, and completely separated the cartilage from sparse marrow spaces lined by osteoblasts in the deeper bone. The synovium in sham-operated TMJ was similar to that in the knee joint in sheep (Smith et al., 2008) with a single lining layer of synoviocytes overlying a loose connective tissue with adipocytes and sparse fibroblasts and collagen.
A variety of pathological changes of varying severity were noted in discopexy and discectomy joints (Fig. 1Abee). The mildest changes included cartilage thickening, slightly increased matrix and peri-cellular proteoglycan staining, increased cell density, vascular activation and invasion of the sub-chondral bone and calcified cartilage layer, with both the tidemark and cement line being more distinct (Fig. 1Ab). Intermediate cartilage pathology was characterized by surface roughening/fibrillation, loss of typical laminar structure, a marked increase in inter-territorial proteoglycan staining in all layers, cell cloning particularly in the upper zones, and further deep zone vascular invasion (Fig. 1Ac). Further advancement of pathology was evident with erosion and loss of surface zone cartilage, decreased cell density in the mid zone but cloning in all layers, vascular invasion into the mid zone (Fig. 1Ad), and ultimately complete loss of cartilage integrity and marked subchondral bone remodelling (Fig. 1Ae). Accompanying the osteochondral changes, there was synovitis with hyperplasia of surface cells, sub-synovial fibrosis with loss of adipocytes and both peri-vascular and diffuse inflammatory cell infiltration (not shown). Blinded scoring demonstrated a significant increase in total median histopathology score in discectomy compared with the other groups (Fig. 1B). This was driven by a significant increase in pathology in cartilage, bone and synovium in discectomy compared with sham-operated joints (Fig. 1C). Discopexy joints displayed some evidence of cartilage and synovial pathology, but this was quite variable and did not reach statistical significance.
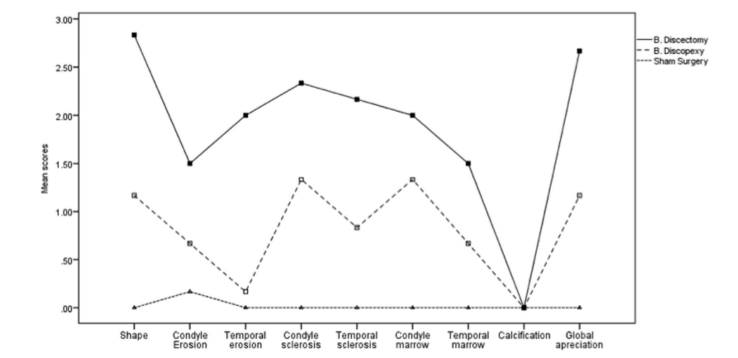
Imaging results
The authors compared the outcomes of all surgery conditions (Table 1). In general, differences were very high (η2p corresponding to 90.8%, statistical power > .999) for all outcomes, excluding calcification. Considering each outcome, differences were higher for shape, followed by condyle sclerosis, temporal sclerosis, condyle marrow, temporal erosion, condyle erosion, and temporal marrow. The effect size of the differences ranged from 43.4% to 90.8%. Fig. 2 is a representative CT imaging of sham surgery group (Fig. 2A), discopexy group (Fig. 2B) and discectomy (Fig. 2C).
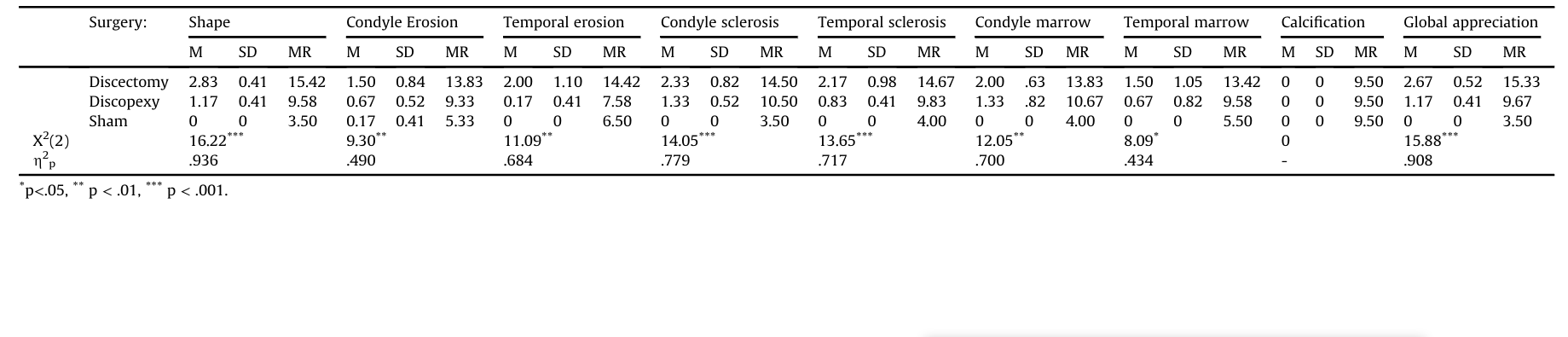
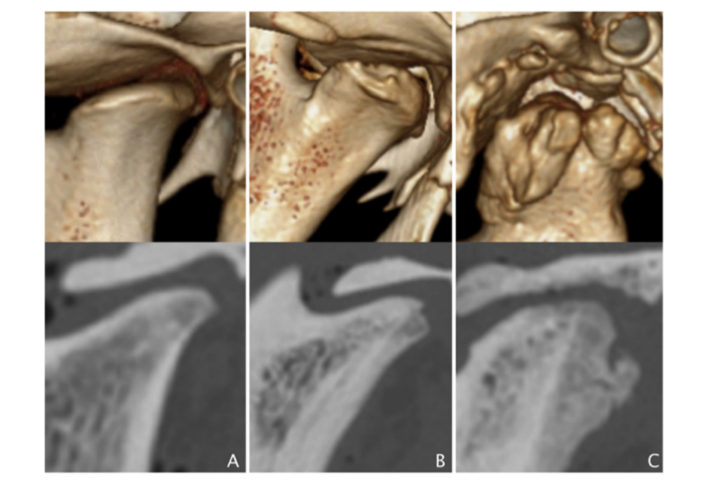
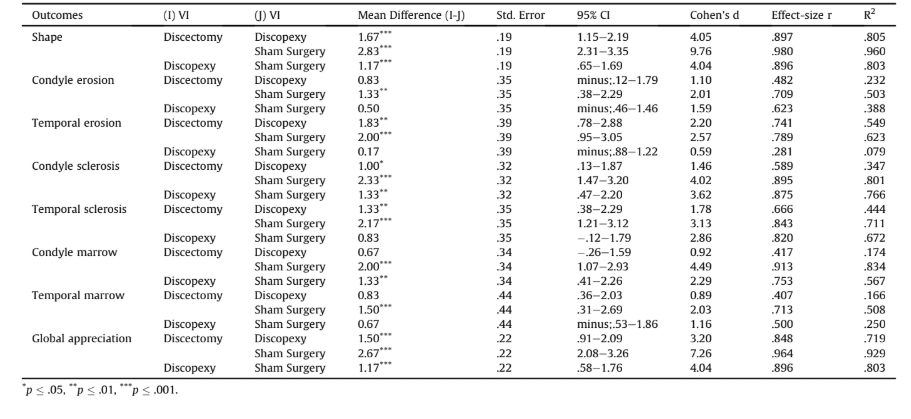
Excluding the difference between discopexy and sham surgery for temporal erosion (d = 0.59), all the other differences were classified as large (d > 0.80). The larger differences were between discectomy and sham surgery (R2 corresponding to 92.9% of degeneration in global appreciation), mainly due to shape (R2 = 96.0%), condyle marrow (R2 = 83.4%), and condyle sclerosis (R2 = 80.1%). Condyle erosion and temporal marrow were the least affected, despite an effect size of R2 of 50.3% and 50.8%, respectively. Temporal sclerosis and temporal erosion showed R2 effect sizes of 71.1% and 62.3%, respectively. Discopexy also differed from sham surgery (R2 corresponding to 80.3% of deterioration in global appreciation), although with lower effect sizes in comparison to the differences between discectomy and sham surgery, and only for shape (R2 = 80.3%), condyle sclerosis (R2 = 76.6%), and condyle marrow (R2 = 56.7%) (Table 2 and Fig. 3).
Body mass results
Cross-sectional analysis.
Statistical differences were not found in body mass in the pre-test (T0) and in all times for the post-test (p > .10, Table 3).
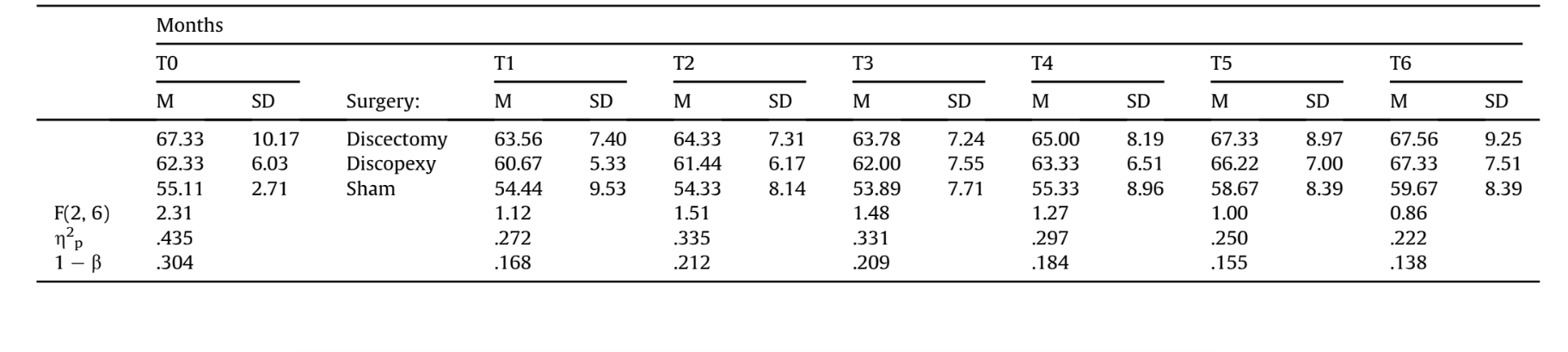
In Fig. 4 can be seen that in the discectomy condition sheep lost weight from month 1 to month 4 and recovered their weight during months 5 and 6 after surgery.
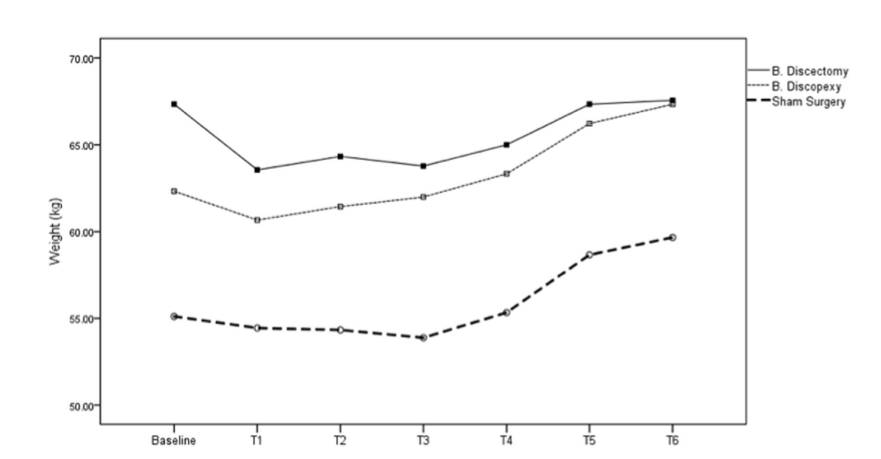
Longitudinal analysis.
A one-way ANOVA with repeated measures was performed taking as within-subjects effects months after surgery (T1-T6) for discectomy, discopexy, and sham surgery. Statistically significant differences were found, F(5, 10) = 9.69, 27.35 and 8.07, p < .01, η2p = .829, .932, and .801, (1 – β) = .992, 1.00, and .977 for discectomy, discopexy, and sham surgery respectively, showing that sheep recovered weight from T1 to T6. The tests of within-subjects contrasts identified that the increase happened from T4 to T5 both in discectomy (p = .04), discopexy (p = .01), and sham surgery (p = .01). Despite this increase, only those in the discopexy and sham groups increased their weight over the pre-test in T5 and T6, t(2) = —5.34 and —5.00, p < .04. In discectomy and sham surgery conditions sheep did not exceed their weight at baseline.
Discussion
This is the first temporomandibular preclinical study using a randomized, blinded design respecting ARRIVE guidelines. Using the suitable Black Merino sheep with age and gender selection, sham control group and bilateral approach, the authors aimed to reduce possible bias on results. In humans, TMJ cartilage is different from appendicular synovial joints (Murphy et al., 2013), with the distinctly laminar fibrocartilage with sparse proteoglycan reminiscent of meniscus and annulus fibrosus of the intervertebral disc (Melrose et al., 2017; Shu et al., 2017). In sham-operated joints of Black Merino sheep the TMJ cartilage was histologically very like humans, supporting sheep as a good animal model. Rat (Zhang et al., 2016) and goat (Li et al, 2015) also have a typical TMJ fibro-cartilage appearance with the distinct organized layers, while in the mouse (Cohen et al., 2014; Xu et al., 2009) and rabbit (Wu et al., 2015) the laminar structure is less apparent.
The histopathology changes obtained in the sheep TMJ after bilateral discectomy were consistent with other investigations using various species, including mice (Cohen et al., 2014), rats (Zhanget al., 2016), rabbits (Embree et al., 2015) and goats (Li et al., 2015). The authors noticed an increase in proteoglycan and rounded cells and thickening of the cartilage after discectomy. These changes in Black Merino sheep are similar to reports in other animals (e.g. mouse (Cohen et al., 2014; Matías et al., 2016; Xu et al., 2009) and rat (Zhang et al., 2016)). They are consistent with a chondroid metaplasia, which is potentially associated with the loss of the disc and increased direct loading in the TMJ cartilage. However, when this first protective phase fails under continued abnormal loading, the joint undergoes degeneration with cell death and cloning, surface erosion, subchondral bone changes and degeneration. This latter phase is well described and similar to that in the sheep knee joint following meniscectomy (Cake et al., 2013; Little et al., 2010). In the discopexy intervention group, the TMJ capsule and the intra-articular environment was preserved. The result, as expected, had less severe histopathologic changes, because the disc remained interposed between the bony surfaces, dissipating loading and protecting the TMJ cartilage. It is noteworthy that we also found more severe synovitis in discectomy compared with discopexy, indicating that the inflammation is not just a reaction to the arthrotomy, but part of the OA process in the joint. The histopathological appearance of the synovitis in the TMJ was the same as that in sheep knee joints with OA (Smith et al., 2008). Still, given the underlying anatomical differences in cartilage, future studies should explore the molecular mechanisms that underlie TMJ OA pathology, to determine their similarities and differences with appendicular joints such as the knee (Young et al., 2005). Such studies could lead to progress in defining the pathophysiology and the management of TMJ degenerative disorders.
Radiographic morphologic changes caused by discectomy were first reported by Boman in 1947, describing “flattening off the articular surface” (Boman, 1947). In 1985, similar conclusions were obtained with condylar flattening and sclerosis after unilateral discectomy, where no osteophytes but severe damage were described (Eriksson and Westesson, 1985). Concomitantly, condyle flattening and sclerosis were the most common radiographic findings in a 33.8 years post discectomy investigation (Tolvanen et al., 1988). In the present study, these outcomes are reinforced with severe morphological changes observed after bilateral discectomy. Most statistical differences were noted in shape and condyle sclerosis, corresponding to other authors' clinical findings (Eriksson and Westesson, 1985; Takaku et al., 2000). While the human condyle is convex and tends to flatten after discectomy, the sheep condyle is normally flat and tend to a more convex form after discectomy (Fig. 2C). Nevertheless, condyle sclerosis in all joints after bilateral discectomy (R2 = 80.1%) and change in underlying trabecular bone (condyle bone marrow) were also detected. Cortical breakdown characterized by an initial destructive phase was reported by Agerber and Lundberg in the first 6 months post- discectomy (Agerberg and Lundberg, 1971). Some authors suggest that these changes can occur if loading is not controlled during those 6 months (Hall, 1985). Other authors raised the question of whether the lytic condylar process is precipitated by discectomy or overloading, since the contralateral nonoperated joint has similar morphologic changes (Agerberg and Lundberg, 1971; Eriksson and Westesson, 1985; Takaku and Toyoda, 1994; Wilkes, 1991). Yaillen, in 1979 described bony ankylosis between the condyle and temporal bone 1 year after unilateral discectomy in Macaca fascicularis (Yaillen et al., 1979). Later, Bjornland found fibrous ankylosis 6 months after unilateral discectomy (Bjornland and Larheim, 2003). In TEMPOJIMS, 6 months after bilateral discectomy no intra-articular calcification was found, and while fibrous ankylosis cannot be excluded with CT, this was not evident histologically. Significant osteophyte formation is also reported, rarely described in previous studies, which may be due to imaging limitations of radiography and arthrography compared with CT.
To the best of our knowledge, there are no clinical or preclinical studies assessing imaging after discopexy. Results showed that TMJ open surgery is not innocuous, resulting in mild to moderate changes in global remodelling. The condyle is more affected than the temporal bone and only for shape (R2 = 80.3%), condyle scle- rosis (R2 = 76.6%), and condyle marrow (R2 = 56.7%).
In other diseases like rheumatoid arthritis (England et al., 2017), cancer (Lynch et al., 2017), HIV (Malvy et al., 2001) and surgical interventions like gastric sleeve (Casillas et al., 2017), body mass has been used as a valuable outcome to evaluate progress of disease and intervention success. However, for TMJ disorders this outcome has rarely been used. A 4% decrease of body mass in 60% of the animals, 3 months after unilateral discectomy with condyle and temporal surfaces removal, has been reported (Miyamoto et al.,1999). In a study in mice, after partial discectomy no significant losses or gains in the body weight of the experimental or control mice were seen (Xu et al., 2009). In this study, after bilateral dis- cectomy there was 5.2% body mass loss (all occurring in the first month) but with full recovery at 6 months follow-up. In contrast, the discopexy and sham surgery sheep increased body weight (mostly in T4-T6), finishing the study 8% and 8.2% above the baseline, respectively. It is consistent with the limited TMJ pathology. The evaluation of body mass was also a welfare control measure related to healthy and well fed, respecting the 3 Rs principle (replacement, reduction, or refinement) (Richmond, 2002).
Conclusion
This pilot study design demonstrates it is feasible to conduct surgical TMJ preclinical trials in Black Merino sheep. In this study, the authors observed: (1) bilateral discopexy in a healthy TMJ is not an innocuous intervention, resulting in variable cartilage and synovial pathology along with imaging changes; (2) bilateral discectomy induced severe TMJ changes detected with both imaging and histopathologic analysis; (3) no fibrous or bony ankylosis was detected over the 6-month period after bilateral discectomy and discopexy. And (4) beyond expected cartilage and bone changes, synovitis was shown to be part of the osteoarthritis process, providing a new outcome measure and therapeutic target.
This study has reinforced that: (1) TMJ cartilage is different from appendicular synovial joints, and as such may require unique therapeutic approaches; (2) future investigations are needed to study an effective interposal material to substitute the TMJ disc and (3) future investigations are needed to explore the molecular mechanisms that underlie TMJ cartilage degeneration.
Authors: David Faustino Ângelo, Pedro Morouço, Florencio Monje Gil, Lisete Mónico, Raúl González-Gárcia, Rita Sousa, Lia Neto, Inês Caldeira, Margaret Smith, Susan Smith, David Sanz, Fábio Abade dos Santos, Mário Pinho, Belmira Carrapiço, Sandra Cavaco, Carla Moura, Nuno Alves, Francisco Salvado, Christopher Little
References:
- Agerberg G, Lundberg M: Changes in the temporomandibular joint after surgical treatment. A radiologic follow-up study. Oral Surg Oral Med Oral Pathol 32(6): 865e875, 1971
- Angelo DF, Morouço P, Alves N, Viana T, Santos F, González R, et al: Choosing sheep (Ovis aries) as animal model for temporomandibular joint research: morphological, histological and biomechanical characterization of the joint disc. Morphologie 100(331): 223e233, 2016
- Ângelo DF, Gil FM, González-Garcia R, Mo´nico L, Sousa R, Neto L, et al: Effects of bilateral discectomy and bilateral discopexy on black Merino sheep rumination kinematics: TEMPOJIMS - phase 1-pilot blinded, randomized preclinical study. J Craniomaxillofac Surg, 2017a S1010e5182(17)30415-8
- Ângelo DF, Monje FG, Gonzalez-Garcia R, Little CB, Monico L, Pinho M, et al: Bioengineered temporomandibular joint disk implants: study protocol for a two-phase exploratory randomized preclinical pilot trial in 18 black Merino sheep (TEMPOJIMS). JMIR Res Protoc 6(3): e37, 2017b
- Bjornland T, Larheim TA: Discectomy of the temporomandibular joint: 3-year follow-up as a predictor of the 10-year outcome. J Oral Maxillofac Surg 61(1): 55e60, 2003
- Block MS, Bouvier M: Adaptive remodeling of the rabbit temporomandibular joint following discectomy and dietary variations. J Oral Maxillofac Surg 48(5): 482e486, 1990
- Boman K: Temporomandibular joint arthrosis and its treatment by extirpation of the disc: a clinical study. Follow-up examination. Acta Chir Scand 95(192), 1947
- Cake MA, Read RA, Corfield G, et al: Comparison of gait and pathology outcomes of three meniscal procedures for induction of knee osteoarthritis in sheep. Osteoarthr Cartil 21(1): 226e236, 2013
- Casillas RA, Kim B, Fisher H, Zelada JL, Um SS, Coleman KJ: Comparative effectiveness of sleeve gastrectomy versus Roux-en-Y gastric bypass for weight loss and safety outcomes in older adults. Surg Obes Relat Dis 13(9): 1476e1483, 2017
- Choukas NC, Toto PD, Schoen JE: Gross and histologic changes in the jaws of the Macaca rhesus monkey following surgery. Oral Surg Oral Med Oral Pathol 27(6): 795e805, 1969
- Cohen WA, Servais JM, Polur I, Li Y, Xu L: Articular cartilage degeneration in the contralateral non-surgical temporomandibular joint in mice with a unilateral partial discectomy. J Oral Pathol Med 43(2): 162e165, 2014
- Cordeiro PC, Guimaraes JP, de Souza VA, Dias IM, Silva JN, Devito KL, et al: Temporomandibular joint involvement in rheumatoid arthritis patients: association between clinical and tomographic data. Acta Odontol Latinoam 29(3): 123e129, 2016
- Dimitroulis G: The role of surgery in the management of disorders of the temporomandibular joint: a critical review of the literature. Part 2. Int J Oral Maxillofac Surg 34(3): 231e237, 2005
- Dimitroulis G: A new surgical classification for temporomandibular joint disorders. Int J Oral Maxillofac Surg 42: 218e222, 2013
- Embree MC, Iwaoka GM, Kong D, Martin BN, Patel RK, Lee AH, et al: Soft tissue ossification and condylar cartilage degeneration following TMJ disc perforation in a rabbit pilot study. Osteoarthr Cartil 23(4): 629e639, 2015
- England BR, Baker JF, Sayles H, Michaud K, Caplan L, Davis LA: Body mass index, weight loss, and cause-specific mortality in rheumatoid arthritis. Arthritis Care Res, Apr 20. 2017
- Eriksson L, Westesson PL: Long-term evaluation of meniscectomy of the temporomandibular joint. J Oral Maxillofac Surg 43(4): 263e269, 1985
- Eriksson L, Westesson P-L: Discectomy as an effective treatment for painful temporomandibular joint internal derangement: a 5-year clinical and radio- graphic follow-up. J Oral Maxillofac Surg 59(7): 750e758, 2001
- Hagandora CK, Almarza AJ: TMJ disc removal: comparison between pre-clinical studies and clinical findings. J Dent Res 91(8): 745e752, 2012
- Hall HD: Meniscectomy for damaged disks of the temporomandibular joint. South Med J 78(5): 569e572, 1985
- Ishimaru J, Goss AN: A model for osteoarthritis of the temporomandibular joint. J Oral Maxillofac Surg 50(11): 1191e1195, 1992
- Kiehn CL, Desprez JD: Meniscectomy for internal derangement of temporomandibular joint. Br J Plast Surg 15: 199e204, 1962
- Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG: Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol 8(6): e1000412, 2010
- Laurell KA, Tootle R, Cunningham R, Beltran J, Simon D: Magnetic resonance imaging of the temporomandibular joint. Part II: comparison with laminographic, autopsy, and histologic findings. J Prosthet Dent 58(2): 211e218, 1987
- Li L, Wang L, Sun Y, Yang C, He D: Establishment and histological evaluation of a goat traumatic temporomandibular joint model. J Oral Maxillofac Surg 73(5): 943e950, 2015
- Little CB, Smith MM, Cake MA, Read RA, Murphy MJ, Barry FP: The OARSI histopathology initiative e recommendations for histological assessments of osteoarthritis in sheep and goats. Osteoarthr Cartil 18(Suppl 3): S80eS92, 2010
- Lynch SM, Stricker CT, Brown JC, Berardi JM, Vaughn D, Domchek S, et al: Evaluation of a web-based weight loss intervention in overweight cancer survivors aged 50 years and younger. Obes Sci Pract 3(1): 83e94, 2017
- Macher DJ, Westesson PL, Brooks SL, Hicks DG, Tallents RH: Temporomandibular joint: surgically created disk displacement causes arthrosis in the rabbit. Oral Surg Oral Med Oral Pathol 73(6): 645e649, 1992
- Malvy E, Thie´baut R, Marimoutou C, Dabis F, Groupe d'Epidemiologie Clinique du Sida en Aquitaine: Weight loss and body mass index as predictors of HIV disease progression to AIDS in adults. Aquitaine cohort, France, 1985-1997. J Am Coll Nutr 20(6): 609e615, 2001
- Matías EM, Mecham DK, Black CS, Graf JW, Steel SD, Wilhelm SK, et al: Malocclusion model of temporomandibular joint osteoarthritis in mice with and without receptor for advanced glycation end products. Arch Oral Biol 69: 47e62, 2016
- Matsuura H, Miyamoto H, Kurita K, Goss AN: The effect of autogenous costochondral grafts on temporomandibular joint fibrous and bony ankylosis: a preliminary experimental study. J Oral Maxillofac Surg 64(10): 1517e1525, 2006
- Melrose J, Fuller ES, Little CB: The biology of meniscal pathology in osteoarthritis and its contribution to joint disease: beyond simple mechanics. Connect Tissue Res 58(3e4): 282e294, 2017
- Miyamoto H, Kurita K, Ishimaru J, Goss AN: A sheep model for temporomandibular joint ankylosis. J Oral Maxillofac Surg 57(7): 812e817, 1999
- Murphy MK, MacBarb RF, Wong ME, Athanasiou KA: Temporomandibular disorders: a review of etiology, clinical management, and tissue engineering strategies. Int J Oral Maxillofac Implant 28(6): e393e414, 2013
- Ogi N, Kurita K, Handa Y, Goss AN: The short-term effect of discectomy on the osteoarthrotic temporomandibular joint in sheep. Int J Oral Maxillofac Surg 25(4): 319e324, 1996
- Reston JT, Turkelson CM: Meta-analysis of surgical treatments for temporomandibular articular disorders. J Oral Maxillofac Surg 61(1), 2003 3e10-2
- Richmond J: Refinement, reduction, and replacement of animal use for regulatory testing: future improvements and implementation within the regulatory framework. ILAR J 43(Suppl): S63eS68, 2002
- Shu CC, Smith MM, Smith SM, Dart AJ, Little CB, Melrose J: A histopathological scheme for the quantitative scoring of intervertebral disc degeneration and the therapeutic utility of adult mesenchymal stem cells for intervertebral disc regeneration. Int J Mol Sci 18(5), 2017
- Silver CM: Long-term results of meniscectomy of the temporomandibular joint. Cranio 3(1): 46e57, 1984
- Smith MM, Cake MA, Ghosh P, Schiavinato A, Read RA, Little CB: Significant synovial pathology in a meniscectomy model of osteoarthritis: modification by intra-articular hyaluronan therapy. Rheumatology (Oxford) 47(8): 1172e1178, 2008
- Souza RF, Lovato da Silva CH, Nasser M, Fedorowicz Z, Al-Muharraqi MA: Interventions for the management of temporomandibular joint osteoarthritis. In: de Souza RF (ed.), Cochrane database of systematic reviews; 2012, 2012
- Takaishi M, Kurita K, Matsuura H, Goss AN: Effect of auricular cartilage graft in the surgical treatment of temporomandibular joint ankylosis: an animal study using sheep. J Oral Maxillofac Surg 65(2): 198e204, 2007
- Takaku S, Toyoda T: Long-term evaluation of discectomy of the temporomandibular joint. J Oral Maxillofac Surg 52(7), 1994 722e726-8
- Takaku S, Sano T, Yoshida M: Long-term magnetic resonance imaging after temporomandibular joint discectomy without replacement. J Oral Maxillofac Surg 58(7): 739e745, 2000
- Tolvanen M, Oikarinen VJ, Wolf JA: 30-year follow-up study of temporomandibular joint meniscectomies: a report on five patients. Br J Oral Maxillofac Surg 26(4): 311e316, 1988
- Trumpy IG, Lyberg T: Surgical treatment of internal derangement of the temporomandibular joint: long-term evaluation of three techniques. J Oral Maxillofac Surg 53(7), 1995 740e746-7
- Wilkes CH: Surgical treatment of internal derangements of the temporomandibular joint. A long-term study. Arch Otolaryngol Head Neck Surg 117(1): 64e72, 1991
- Wu G, Zhu S, Sun X, Hu J: Subchondral bone changes and chondrogenic capacity of progenitor cells from subchondral bone in the collagenase-induced temporomandibular joints osteoarthritis rabbit model. Int J Clin Exp Pathol 8(9): 9782e9789, 2015
- Xu L, Polur I, Lim C, Servais JM, Dobeck J, Li Y, et al: Early-onset osteoarthritis of mouse temporomandibular joint induced by partial discectomy. Osteoarthr Cartil 17(7): 917e922, 2009
- Yaillen DM, Shapiro PA, Luschei ES, Feldman GR: Temporomandibular joint meniscectomyeeffects on joint structure and masticatory function in macaca fascicularis. J Maxillofac Surg 7(4): 255e264, 1979
- Young AA, Smith MM, Smith SM, Cake MA, Ghosh P, Read RA, et al: Regional assessment of articular cartilage gene expression and small proteoglycan metabolism in an animal model of osteoarthritis. Arthritis Res Ther 7(4): 852e861, 2005
- Zhang M, Wang H, Zhang J, Zhang H, Yang H, Wan X, et al: Unilateral anterior crossbite induces aberrant mineral deposition in degenerative temporomandibular cartilage in rats. Osteoarthr Cartil 24(5): 921e931, 2016
