Digital Workflow: Provisionalization on Implants
Machine translation
Original article is written in ES language (link to read it) .
Introduction
Currently, implant therapy is considered an effective treatment for the functional and aesthetic rehabilitation of lost teeth, as evidenced by long-term studies with different implant systems. Despite these high success rates, osseointegrated implants are susceptible to changes in the level of crestal bone and soft tissues, through physiological remodeling or pathological processes, such as peri-implantitis. It is currently believed that early bone loss could be a risk factor for the onset of peri-implantitis. Therefore, there is a greater interest in maintaining peri-implant bone levels, mainly buccal bone due to the possible aesthetic implications that may lead to recessions of the vestibular soft tissue. On the other hand, good support in terms of the volume of attached soft tissue around the implant can help maintain the implant both in terms of bone stability and oral hygiene by the patient.
Hence, the realization of provisional restorations on implants in order to improve or increase the perimplant soft tissue is a tool that should never be underestimated. The digital workflow for creating an aesthetic/functional provisional on an implant must respect certain biological factors that do not differ much from a conventional protocol. It could be said that with the implementation of digital technology, we can create prosthetic elements that achieve good trueness and precision, as well as shorten time in the clinic and improve the flow of information with the laboratory. Additionally, these are easily replicable elements, without having to take measurements from the patient again.
The key factors are summarized in 6 points: Volume of soft tissue; Level of soft tissues in relation to adjacent teeth; Bone substrate; Position of the implant in relation to the available soft tissue; Conversion of the gingival biotype; and Design of the prosthetic abutment.
Soft Tissue Volume
Lindhe highlighted that 85% of people have a thick biotype and 15% have a thin biotype. Kan et al. have suggested that tissue is thick if the thickness is >1 mm; in contrast, tissue is thin if the thickness is <1 mm.
The thickness of the tissue has a direct impact on the influence of recession. Kan et al. found that 35 implants after 90 months had an average recession of 1 mm. When only the thick biotype was considered, the average recession was <0.5 mm; with the thin biotype, the average recession was 1.5 mm. Additionally, prominent roots cause greater thinning of the buccal tissues, with a higher risk of recession. Recent research has placed a lot of emphasis on measuring soft tissue to truly establish the amount of tissue the patient has and whether it is sufficient for proper implant positioning.
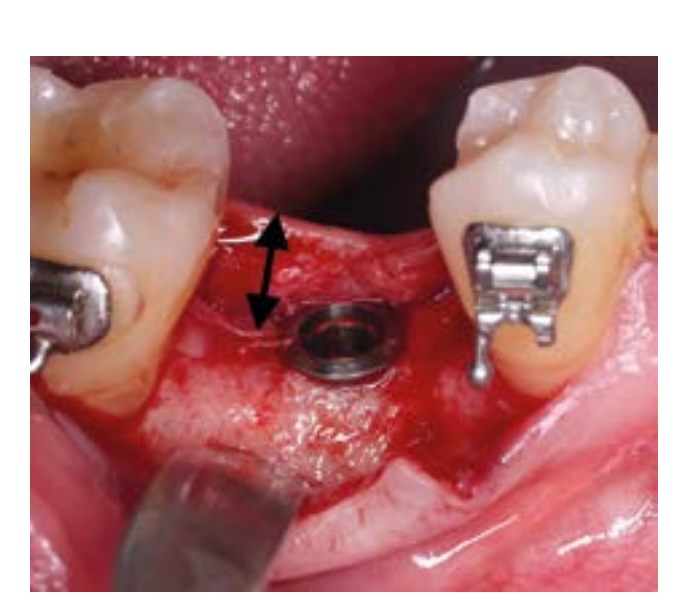
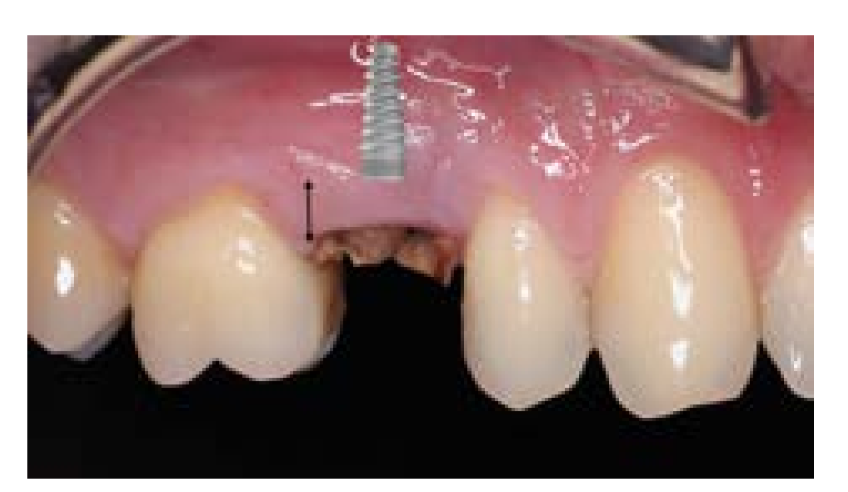
The correct measurement of soft tissue includes: the horizontal width of keratinized tissue, the amount of attached gingiva vestibular, and the height of the crestal soft tissue (vertical thickness of gingiva). (Fig. 1-1).

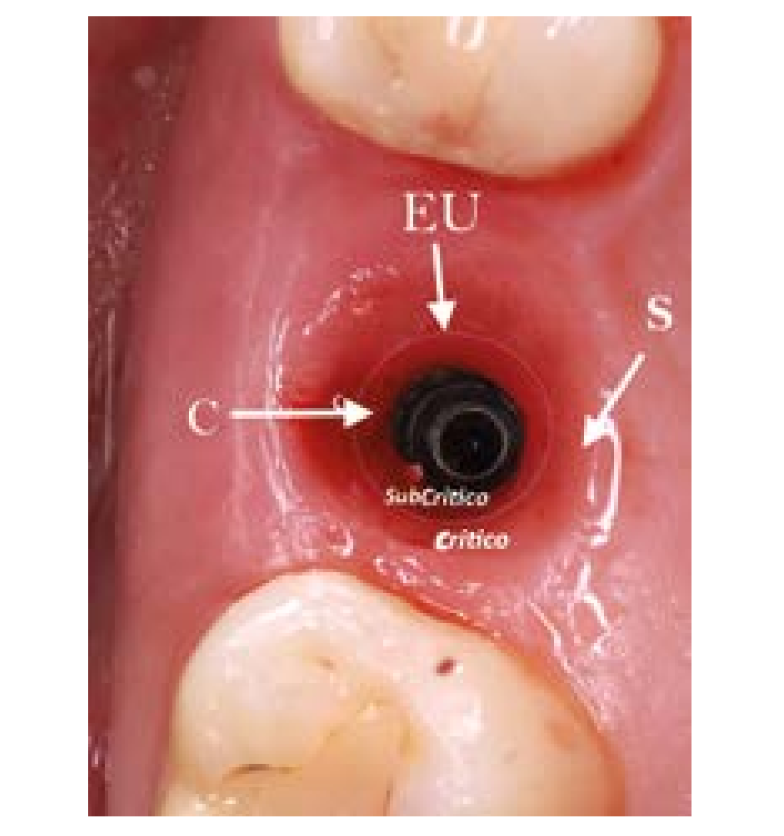
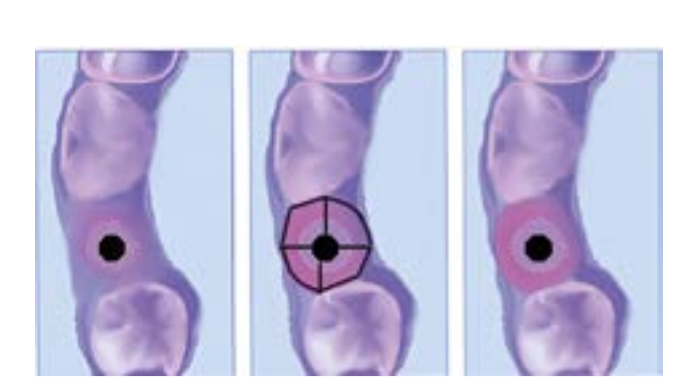
The future peri-implant environment consists of circular collagen fibers that embrace the prosthetic portion of the implant, delineating a critical and subcritical contour (connective zone and epithelial adhesion zone). (Fig. 1-2).
The formation of the biological width and the maturation of the barrier function around transmucosal implants requires 6 to 8 weeks of healing. For the proper fabrication of a provisional on an implant, the presence of good attached keratinized gingiva in both width and height is important so that the provisional can create a perimplantary environment of sufficient thickness that allows for perimplantary bone stability and thus create a good emergence profile.
Soft Tissue Level
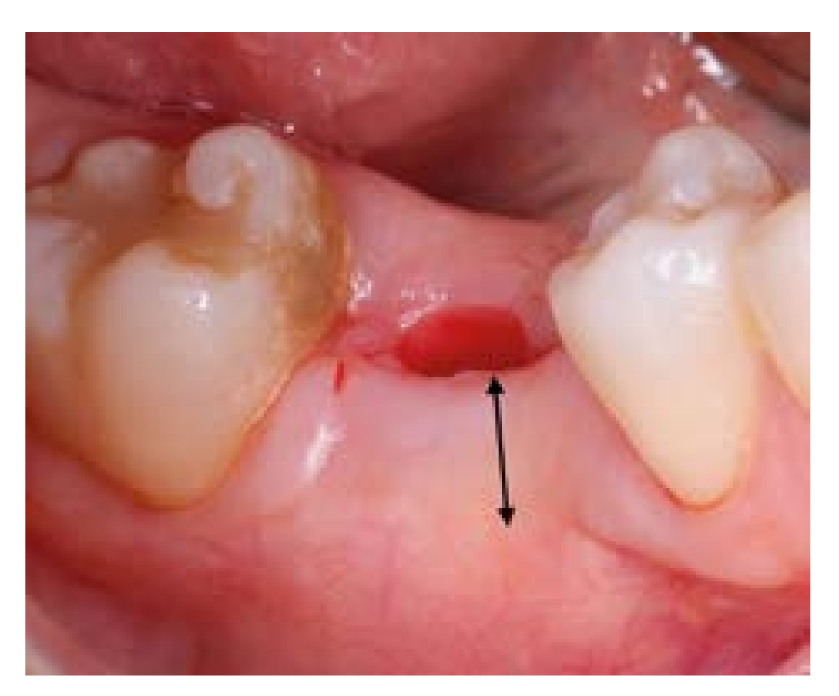
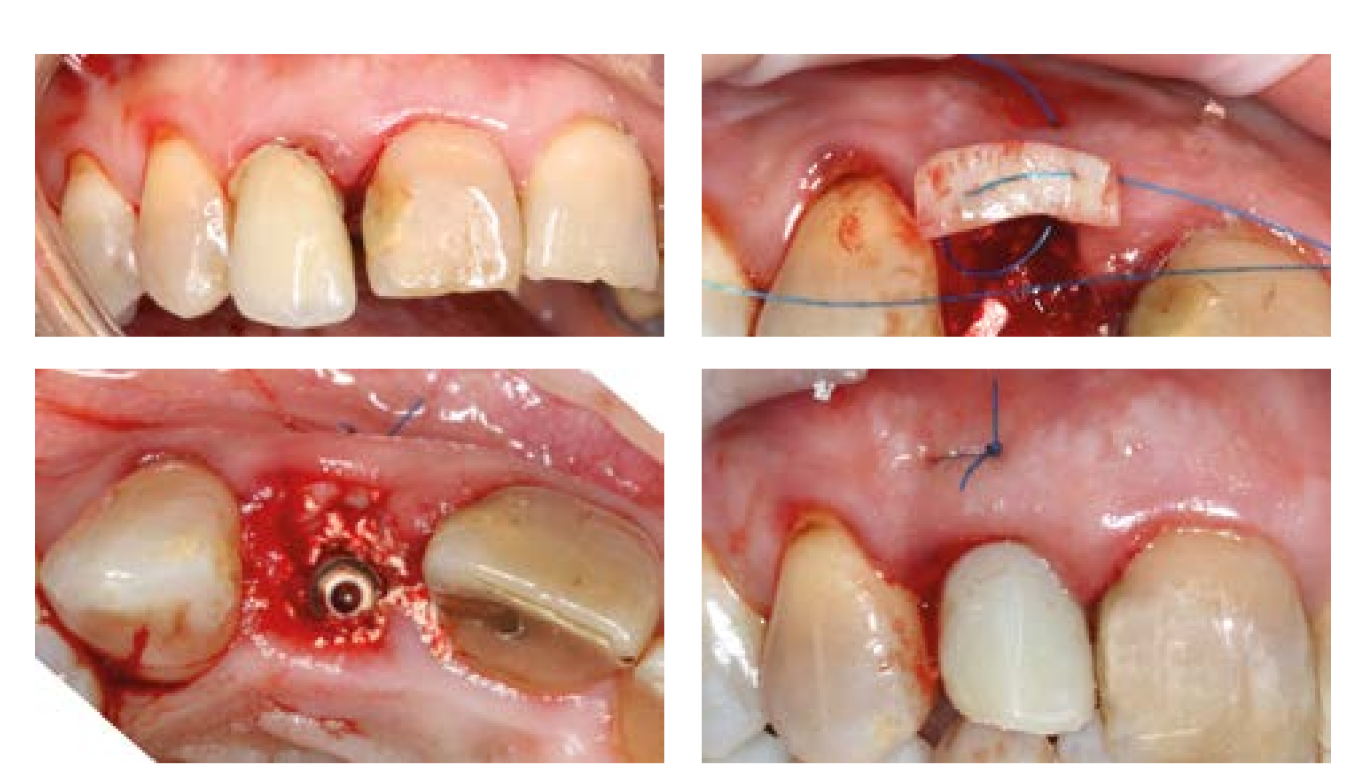
Of utmost importance is the location of the gingival margin in relation to the adjacent teeth. We can find ourselves in three situations: a more apical gingival margin, at the level, or more coronal than the margin of the adjacent tooth. (Fig. 2-1) The latter is more favorable due to the possible loss of soft tissue that may occur after extraction.

In the rest of the cases, it is necessary to act in such a way that the risks of recession are minimized using, for example, soft tissue/bone grafts, orthodontic extrusion, etc., before prosthetic rehabilitation. The level of the smile also influences aesthetics; a high smile is the least favorable in aesthetic terms.
Bone substrate
The gingival margin of our future prosthesis is conditioned not only by the peri-implant soft tissues but also by the present bone substrate.
It is important to identify: Situation, height, position of the bone insertion at its most coronal point in the pieces (or implants) adjacent to the defect.
The bone framework and its relationship with the implant environment is a conditioning factor for pink aesthetics.
Tarnow in 2000 identified that 100% formation of the interproximal papilla is achieved only when the distance between the crest/bone peak and the contact point is below 5 mm. (Fig. 2-2).
Implant Position in Relation to Soft Tissue
According to the latest research, the correct position of an implant must take into account, on one hand, the correct three-dimensional position in the bone and on the other, the relationship with the available soft tissue. In a post-extraction socket, a correct position is 4-5 mm below the gingival margin (Fig. 2-3), while in an edentulous ridge it is important to measure 4 mm of vertical gingival height, calculated after the first cut to raise the vestibular flap (if the tissue is insufficient, an appropriate implant must be chosen for subcrestal placement or soft tissue augmentation must be performed, as from this keratinized gum the perimplant biological space will be formed in the future). (Fig. 1-1a).
Conversion of the gingival biotype
The performance of a connective tissue graft in the surgical phase or in the second phase can convert a thin biotype into a thick biotype and thus increase the stability of the peri-implant tissues over time. Elian et al in 2007 recommend a trimodal approach for immediate implants with immediate provisionalization: Connective tissue graft, bone graft, and immediate provisional. (Fig. 2-4).

Kan et al. in 2011 demonstrated that after an average follow-up period of 4 years (range, 2 to 8.2 years), the overall mean change in the vestibular gingival level (–1.13 mm) was significantly greater than that observed at the 1-year follow-up (–0.55 mm), suggesting that vestibular gingival tissue recession is a dynamic process and may continue more than 12 months after implant surgery.
Design of the prosthetic abutment
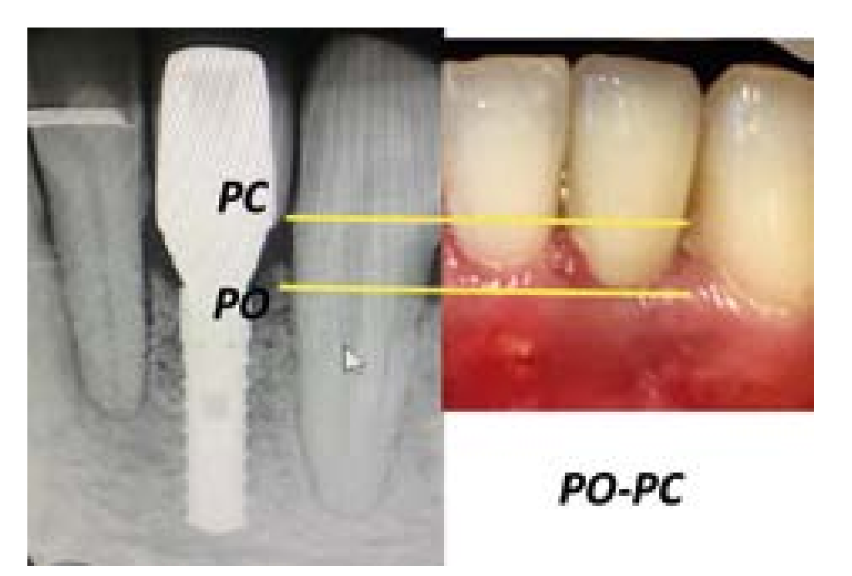
The design of the prosthetic abutment must respect the gingival environment in both height and width. The height of the abutment is the point where our emergence profile will begin. Therefore, it is advisable to use a Ti-base that has a height of 1 mm if the implant is at the crest level and 2-3 mm if the implant is subcrestal to avoid compressing the "bone tunnel" created during drilling.
In contrast to the standard shape of the abutment, the transmucosal design of the abutment, when possible, should be concave rather than convex. (Fig. 2-5). Technicians are accustomed to shaping the abutment without considering the biology of the soft tissue. Generally, they shape the abutment by modifying it through subtraction, but a convex abutment causes compression of the soft tissues and, therefore, ischemia with possible associated recession. The concave abutment shape can help preserve the crestal bone by creating a kind of connective-epithelial junction with the perimplant soft tissue, functioning as a barrier at the bone-implant interface and thus preventing bacterial infiltration. This way, preservation is favored, keeping the tissue more stable over time. The soft tissue will appear very healthy with a light pink color and sometimes with a characteristic similar to the stippling of an orange peel like that surrounding natural teeth.

Complications Related to the Emergence Profile
In some cases, the incorrect choice of prosthetic components can create serious complications. To avoid bone resorption, the height and angulation of the abutments must be carefully selected. If the implants are placed subcrestally and a screw-retained prosthesis is chosen, the healing caps and their future prosthetic abutment must be sufficiently tall to allow the initiation of the supracrestal restoration and as straight as possible to avoid compression regarding the tunnel created by the milling; thus, we avoid bone resorption and consequent gingival recession. If a cemented prosthesis is chosen, the abutment follows the same rules, but additionally, the margin line of the cementation should not exceed 1 mm subgingival (in areas with high aesthetic demand) to be able to remove cement remnants (when possible, opt for cement/screw-retained prostheses that allow extraoral polishing). In posterior areas where there is no high aesthetic demand, the cementation should be supragingival.
Another important complication is the choice of material, the incorrect study of the gingival margin, or the incorrect manufacturing of the prosthesis can lead to the exposure of the implant prosthesis margin. By following the previous guidelines, these errors can be avoided. (Fig. 2-6).



Digital workflow: creation of provisional prostheses on implants.
When choosing the appropriate protocol for creating a provisional on implants, all the previously described factors must be taken into account and an attempt should be made to reveal the maximum amount of information to avoid errors and achieve success with each project.
The current procedures for manufacturing a provisional with digital workflow present 4 steps “E-D-F-A”:
- Intraoral digital scanning using a scanbody or with conventional impression taking of the implant and its subsequent digitization through scanning the master model.
- Design of the digital provisional (CAD Phase): We can design an individual abutment or use a prefabricated abutment (e.g., PMMA blocks) depending on the 3D position of the implant. It is created from library files (implant abutment) and the temporary restoration is designed with the chosen material; the file of the created individual abutment (original CAD drawing) is saved (as STL files) in a specific folder labeled “abutment design,” ready to be retrieved in the following phases.
- Milling of the abutment or use of a prefabricated abutment and milling of the temporary crown (CAM Phase); If a cemented prosthesis is chosen, it will be manufactured and subsequently cemented onto the abutment we have designed.
- Clinical application: Placement of the abutment in the mouth. (Fig. 3-1).



The process begins with an intraoral scan of the working arch and the antagonist, recording the occlusion and subsequently placing one or several scan bodies (which can be customized in the mouth with adjustments using burs to fit the emergence profile) and their subsequent scanning. We can also perform a conventional impression taking and scanning of the master model. If we use an intraoral scanner, we must pay attention to the areas of contact points with adjacent teeth and occlusal areas to increase the accuracy of the scanning, as overlaps often occur in this area. At this step, a first quality validation is performed.
The intraoral scanning must be carried out rigorously and attempting to proceed in a linear manner (using a scanning protocol with the fewest possible interruptions) to avoid creating overlaps that could generate margins of error in the creation of the STL file, ready to be imported into CAD.
Once the scans are imported into the CAD software (Exocad DentalCAD®, Exocad, Darmstadt, Germany), the scanbody of the implant scan is replaced by the corresponding library file, and the different abutment bases (e.g. Ti-base) are selected. The digital design of the provisional (CAD) must achieve the purpose of stabilizing the peri-implant tissues and ensuring good aesthetics. For this reason, the focus should be on creating a correct emergence profile.
Within the CAD software, it is therefore possible to choose the abutment that best fits the context and draw the top of a customized abutment on it; in this way, a conventional PMMA provisional or a customized hybrid abutment can be prepared, made of a Ti-Base (lower portion) and zirconia/PMMA (upper portion). The lower portion corresponds to the chosen abutment base, which will be the area of connection to the connective portion of the peri-implant tissue, a preformed component supplied by the implant manufacturer, coupled to the implant (to avoid zirconia chipping); the upper portion corresponds to the individual portion, which will be the area of epithelial adhesion that will be formed, being modeled and then milled in zirconia/PMMA based on the emergence profile we want to create. Several provisionals can be made that will be changed to gradually modify the emergence profile (for example, in anterior areas with high aesthetic requirements where strict control of the margin level is necessary).
After careful control of the occlusal adaptation and checking the congruence of the contact points, polishing and characterization must be performed to verify the occlusion. To check the quality of the contact points, dental floss is used, which should pass with slight effort. It is advised, for biological reasons, to leave the provisional restoration for a period of time, 2 months, to promote the adaptation of the soft tissues and the use on several occasions of various provisionals.
Kokat and Akca in 2013, to achieve a correct design of the gingival margin, developed a protocol where they use an overlay of the implant scan with a virtual design of an ideal emergence profile.
The precision of the emergence profile of the provisionals allows for an ideal healing of the soft tissues and determines a gingival conditioning that, if properly guided, results in a natural appearance of the transition between the gum and the tooth, which also allows the patient to perform oral hygiene operations easily and effectively.
The provisional is manufactured according to the chosen material: VITA, ENAMIC, PMMA, PROCERA, others.
It is of utmost importance to create a design of the convex emergence profile without steps or with an extra polish, to allow for the migration and consequent creation of stable peri-implant tissues.
If a cemented provisional is chosen, the cementation between the abutment and the provisional crown can be carried out with opaque dual cements (Ivoclar Vivadent Multilink Hyutter Abutment or similar), and the surface of the prosthetic abutment should avoid being previously treated with aluminum oxide sandblasting because it decreases its retention.
Conclusion
The use of a provisional in implantology is a useful and often essential tool to enhance the function and dental aesthetics of the soft tissues.
There have been significant technological advancements that are being applied in modern dentistry to facilitate or expand the range of options available to the professional for their clinical work.
Currently, it is feasible to create a “virtual patient” in 3D using a combined use of CBCT, facial scanner, and intraoral scanner for better diagnosis, planning, and treatment; in addition to improving communication with the laboratory to make it more effective.
Bibliography
- Buser, D, Janner, S, Wittneben, J, Bragger, U, Ramseier C, Salvi G. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res. 2012: 14, 839-51.
- Gotfredsen, K. 2012. A 10-year prospective study of single tooth implants placed in the anterior maxilla. Clin Implant Dent Relat. 2012; 14: 80-7.
- Ostman, P, Hellman, M, Sennerby, L. Ten years later. Results from a prospective single-centre clinical study on 121 oxidized (TiUnite) Branemark implants in 46 patients. Clin Implant Dent Relat Res. 2012; 14: 852-60.
- Laurell L, Lundgren, D. Marginal bone level changes at dental implants after 5 years in function: a meta-analysis. Clin Implant Dent Relat Res. 2011; 13:19-28.
- Schwarz, F, Sahm N, Becker J. Impact of the outcome of guided bone regeneration in dehiscence-type defects on the long-term stability of peri-implant health: clinical observations at 4 years. Clin Oral Implants Res. 2012; 23: 191-6.
- Merheb, J., Quirynen, M., Teughels, W. Critical buccal bone dimensions along implants. Periodontol. 2014; 66: 97-105.
- Spray, J. R., Black, C. G., Morris, H. F., Ochi, S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000; 5: 119-28.
- Tordiglione L, De Franco M B. The prosthetic Workflow in the Digital Era. Int J Dent. 2016; 2: 118.
- Renne W, Ludlow M, Fryml J, et al. Evaluation of the accuracy of 7 digital scanners: An in vitro analysis based on 3-dimensional comparisons. J Prosthet Dent. 2017;118(1):3642.
- Goracci C, Franchi L., Vichi A. FM. Accuracy, reliability, and efficiency of intraoral scanners for full-arch impressions: A systematic review of the clinical evidence. Eur J Orthod 2016;38422–428. 2016;(38):422–8.
- Mangano F., Gandolfi A., Luongo G. LS. Intraoral scanners in dentistry: A review of the current literature. BMC Oral Heal. 2017;17:149.
- Inãki Gamborena, Jaebum Lee, Tiago Fiorini, Brent A. Wenzel, Peter Schüpbach, Ulf M. E. Wikesjö CS, 20. Effect of Platform Shift/Switch and Concave Abutments on Crestal Bone Levels and Mucosal Profile following Flap and Flapless Implant. Clin Implant Dent Relat Res. 2015;Oct 17(5):908–16.
- Salama H, Salama M, Garber D AP. The interproximal height of bone: a guidepost to predictable aesthetic strategies and soft tissue contours in anterior tooth replacement. Pract Periodontics Aesthetic Dent. 1998;10:1131–41.
- Kan JY, Morimoto T, Rungcharassaeng K, Roe P SD. Gingival biotype assessment in the esthetic zone: visual versus direct measurement. Int J periodontics Restor Dent. 2010;(30):237–43.
- Saadoun AP, LeGall M TB. Selection and ideal tridimensional implant position for soft tissue aesthetics. Pract Periodontics Aesthetic Dent. 1999;11:1063–72.
- Grunder U, Gracis S CM. Influence of 3-D bone-to-implant relationship on esthetics. International. J Periodontics Restor Dent. 2005;25:113–9.
- Linkevicius, T., Puisys, A., Steigmann, M., Vindasiute, E. and Linkeviciene L. Influence of Vertical Soft Tissue Thickness on Crestal Bone Changes Around Implants with Platform Switching: A Comparative Clinical Study. Clin Implant Dent Relat Res. 2015;17:1228–36.
- Su H, Gonzalez-Martin O, Weisgold A, Lee E. Considerations of implant abutment and crown contour: critical contour and subcritical contour. Int J Periodontics Restorative Dent. 2010;30(4):335343.
- Thoma DS, Mühlemann S, Jung RE. Critical soft-tissue dimensions with dental implants and treatment concepts. Periodontol 2000. 2014;66(1):106118.
- Wennström JL, Derks J. Is there a need for keratinized mucosa around implants to maintain health and tissue stability?. Clin Oral Implants Res. 2012;23 Suppl 6:136146. doi:10.1111/j.1600-0501.2012.02540.x
- Redemagni, Marco & Cremonesi, Sergio & Garlini, Giuliano & Maiorana C. Soft tissue stability with immediate implants and concave abutments. Eur J Esthet Dent Off J Eur Acad Esthet Dent. 2009;4:328–37.
- Sculean A, Gruber R, Bosshardt DD. Soft tissue wound healing around teeth and dental implants. J Clin Periodontol. 2014;41 Suppl 15:S6S22. doi:10.1111/ jcpe.12206
- Souza CA, Pinho RCM, de Siqueira RAC, et al. Factors Influencing the Presence of Papilla between Adjacent Implants and between a Tooth and an Implant. Acta Stomatol Croat. 2019;53(4):337346. doi:10.15644/asc53/4/4
- Tarnow DP CS. Human histologic verification of osseointegration of an immediate implant placed into a fresh extraction socket with excessive gap distance without primary flap closure, graft, or membrane: a case report. Int J Periodontics Restor Dent. 2011;31:515–21.
- Monje A, Chan HL, Galindo-Moreno P, et al. Alveolar Bone Architecture: A Systematic Review and Meta-Analysis. J Periodontol. 2015;86(11):12311248. doi:10.1902/jop.2015.150263
- Testori T, Weinstein T, Scutellà F, Wang HL, Zucchelli G. Implant placement in the esthetic area: criteria for positioning single and multiple implants. Periodontol 2000. 2018;77(1):176196. doi:10.1111/prd.12211
- Elian N, Cho SC, Froum S, Smith RB, Tarnow DP. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99106.
- Kan JY, Rungcharassaeng K, Lozada JL ZG. Facial Gingival Tissue Stability Following Immediate Placement and Provisionalization of Maxillary Anterior Single Implants: A 2-to 8-Year Follow-up. Int J Oral Maxillofac Implant. 2011;(26):179–87.
- López-López PJ, Mareque-Bueno J, Boquete-Castro A, Aguilar-Salvatierra Raya A, Martínez-González JM, Calvo-Guirado JL. The effects of healing abutments of different size and anatomic shape placed immediately in extraction sockets on peri-implant hard and soft tissues. A pilot study in foxhound dogs. Clin Oral Implants Res. 2016;27(1):9096.
- Souza AB, Alshihri A, Kämmerer PW, Araújo MG, Gallucci GO. Histological and micro-CT analysis of peri-implant soft and hard tissue healing on implants with different healing abutments configurations. Clin Oral Implants Res. 2018;29(10):10071015.
- Cabello G, Rioboo M, Fábrega JG. Immediate placement and restoration of implants in the aesthetic zone with a trimodal approach: soft tissue alterations and its relation to gingival biotype. Clin Oral Implants Res. 2013;24(10):10941100. doi:10.1111/ j.1600-0501.2012.02516.x
- Thoma DS, Naenni N, Figuero E, et al. Effects of soft tissue augmentation procedures on peri-implant health or disease: A systematic review and meta-analysis. Clin Oral Implants Res. 2018;29 Suppl 15:3249. doi:10.1111/clr.13114
- Giannobile WV, Jung RE, Schwarz F; Groups of the 2nd Osteology Foundation Consensus Meeting. Evidence-based knowledge on the aesthetics and maintenance of peri-implant soft tissues: Osteology Foundation Consensus Report Part 1-Effects of soft tissue augmentation procedures on the maintenance of peri-implant soft tissue health. Clin Oral Implants Res. 2018;29 Suppl 15:710. doi:10.1111/clr.13110
- Ivanovski S, Lee R. Comparison of peri-implant and periodontal marginal soft tissues in health and disease. Periodontol 2000. 2018;76(1):116130. doi:10.1111/prd.12150
- Giannobile WV, Jung RE, Schwarz F; Groups of the 2nd Osteology Foundation Consensus Meeting. Evidence-based knowledge on the aesthetics and maintenance of peri-implant soft tissues: Osteology Foundation Consensus Report Part 1-Effects of soft tissue augmentation procedures on the maintenance of peri-implant soft tissue health. Clin Oral Implants Res. 2018;29 Suppl 15:710. doi:10.1111/clr.13110
- Linkevicius T, Vindasiute E, Puisys A, Peciuliene V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin Oral Implants Res. 2011;22(12):13791384. doi:10.1111/j.1600-0501.2010.02119.x
- Fretwurst T, Nelson K, Tarnow DP, Wang HL, Giannobile WV. Is Metal Particle Release Associated with Peri-implant Bone Destruction? An Emerging Concept. J Dent Res. 2018;97(3):259265. doi:10.1177/0022034517740560
- ManganoF, Margiani B AO. A Novel Full-Digital Protocol (SCAN-PLAN-MAKE-DONE®) for the Design and Fabrication of Implant-Supported Monolithic Translucent Zirconia Crowns Cemented on Customized Hybrid Abutments: A Retrospective Clinical Study on 25 Patients. Int J Env Res Public Heal. 2019;16(3):317.
- Ferrari M, Keeling A, Mandelli F, Lo Giudice, Garcia Godoy F JT. The ability of marginal detection using different intraoral scanning systems: A pilot randomized controlled trial. Am J dent. 2018;Oct 31(5):272–6.
- Papadiochou S, Pissiotis AL. Marginal adaptation and CAD-CAM technology: A systematic review of restorative material and fabrication techniques. J Prosthet Dent. 2018;119(4):545551.
- Pjetursson BE, Valente NA, Strasding M, Zwahlen M, Liu S, Sailer I. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic single crowns. Clin Oral Implants Res. 2018;29 Suppl 16:199214. doi:10.1111/clr.13306
- Flügge T, van der Meer WJ, Gonzalez BG, Vach K, Wismeijer D, Wang P. The accuracy of different dental impression techniques for implant-supported dental prostheses: A systematic review and meta-analysis. Clin Oral Implants Res. 2018;29 Suppl 16:374392. doi:10.1111/clr.13273
- Ghodsi S, Zeighami S, Meisami Azad M. Comparing Retention and Internal Adaptation of Different Implant-Supported, Metal-Free Frameworks. Int J Prosthodont. 2018;31(5):475477. doi:10.11607/ ijp.5800
- Kökat AM, Akça K. Fabrication of a screw-retained fixed provisional prosthesis supported by dental implants. J Prosthet Dent. 2004;91(3):293297.
- Howe MS. Implant maintenance treatment and peri-implant health. Evid Based Dent. 2017;18(1):810. doi:10.1038/sj.ebd.6401216
- Konstantinidis I., Trikka D., Gasparatos S. MME. Clinical Outcomes of Monolithic Zirconia Crowns with CAD/CAM Technology. A 1-Year Follow-Up Prospective Clinical Study of 65 Patients. Int J Environ Res Public Heal. 2018;15:2523.
- Linkevicius T, Caplikas A, Dumbryte I, Linkeviciene L, Svediene O. Retention of zirconia copings over smooth and airborne-particle-abraded titanium bases with different resin cements. J Prosthet Dent. 2019;121(6):949954.
- Naudi KB, Benramadan R, Brocklebank L, Ju X, Khambay B, Ayoub A. The virtual human face: superimposing the simultaneously captured 3D photo-realistic skin surface of the face on the untextured skin image of the CBCT scan. Int J Oral Maxillofac Surg. 2013;42(3):393400.
