CAD Evaluation of Dimensional Changes After Using Volumetrically Stable Collagen Matrices in Vestibular Horizontal Defects Concurrent with Implant Placement. A Pilot Study
Machine translation
Original article is written in IT language (link to read it) .
Objective
CAD evaluation of dimensional changes after the use of volumetrically stable porcine collagen matrices in the management of horizontal defects in implant-prosthetic rehabilitations.
Methods
Intraoral scans were performed using the iTero scanner before tooth extraction (S0), at time S1, 3 months after implant surgery, during which a volumetrically stable collagen matrix was simultaneously inserted (S1), and at 1 year (S2). The obtained scans were processed with exocad and the STL files analyzed with the same software for the analysis of volumetric variations: in this part of the study, colorimetric analysis was evaluated with a range between 0 and 2 mm.
Conclusions
The use of a volumetrically stable collagen matrix as a tissue substitute at the time of implant insertion allowed for an increase in soft tissues around the implants, avoiding an autologous graft site, and achieving a stable result at 1 year in accordance with the currently available literature data.
Introduction
In recent years, the demand from patients for implant-prosthetic rehabilitations has seen a significant increase.
To meet this growing demand, there has also been an increased need from clinicians for high and stable aesthetic results over time. In particular, the relationship between the pink and white components of the peri-implant structures must allow for total biomimicry of the rehabilitations.
Furhauser et al. in 2005 provided parameters to evaluate and respect regarding pink aesthetics to consider the results obtained a success. Thoma et al. in 2014 described how the increase of soft tissues was an integral part of implant surgery in order to achieve lasting results over time, especially in cases where the soft tissues belonged to thin biotypes.
Over time, the approach has increasingly focused on the management of soft tissues, aiming to compensate for the volumetric deficits that are sometimes present. The gold standard currently described in the literature for soft tissue augmentation is still considered to be connective tissue grafting.
The harvesting from the palate, however, requires specific surgical knowledge, and involving a second surgical access can sometimes be a disadvantage in the patient's decision to proceed with the treatment plan.
For this reason, in recent years, collagen matrices have been developed that, if inserted and stabilized correctly, allow for valid results with increases not inferior to autologous grafts.
This study is a pilot evaluation, using CAD/3D software, of the volumetric changes at one year, in cases of implant placement and simultaneous use of volumetrically stable collagen matrices inserted in the vestibular position.
Materials and methods
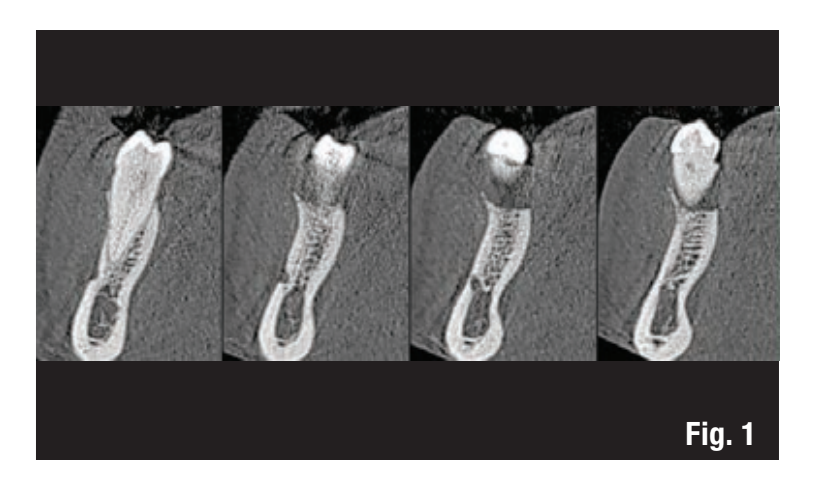
Ten ASA 2 patients without systemic diseases were selected, requiring rehabilitation in areas 44-45 or 34-35 through extraction and implant placement, who presented adequate bone volume without the need for GBR but with the possibility of increasing the soft tissues to harmonize the peri-implant volume for aesthetic purposes and to maintain long-term success (Fig. 1).
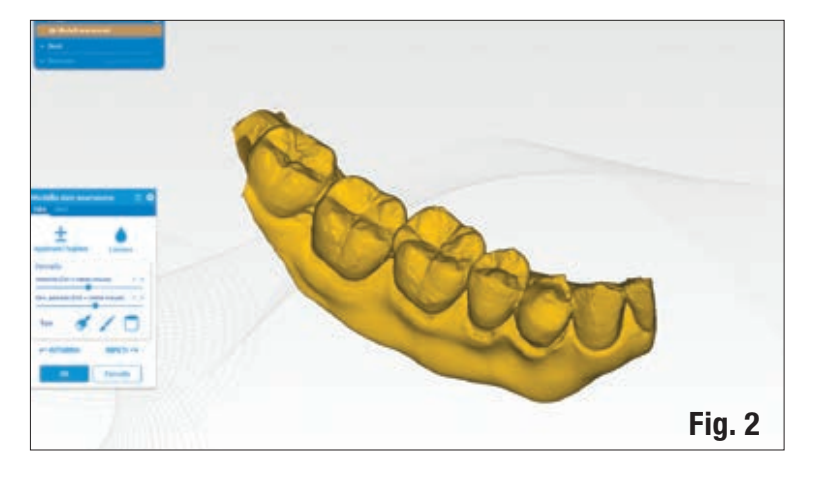
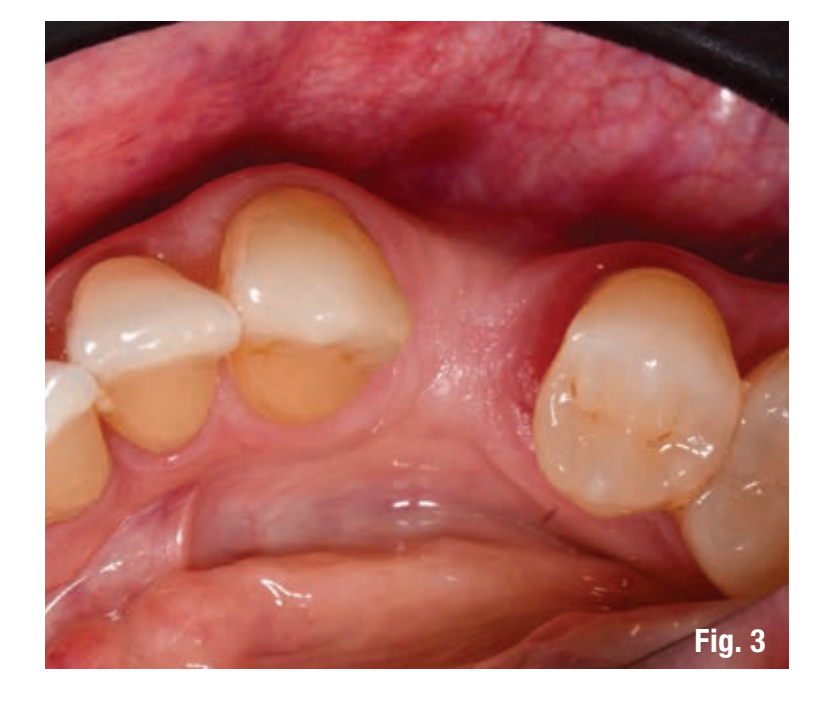
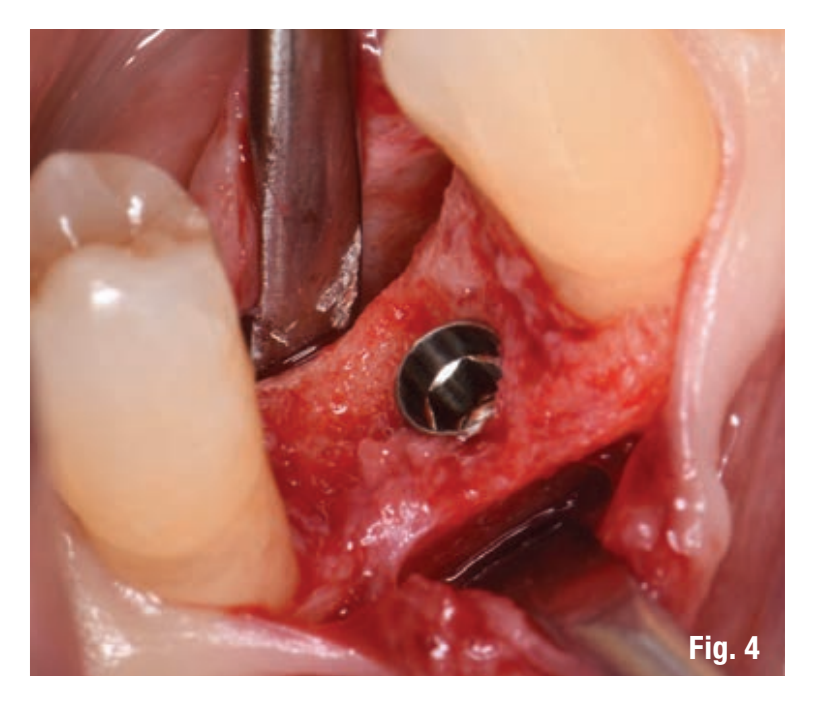
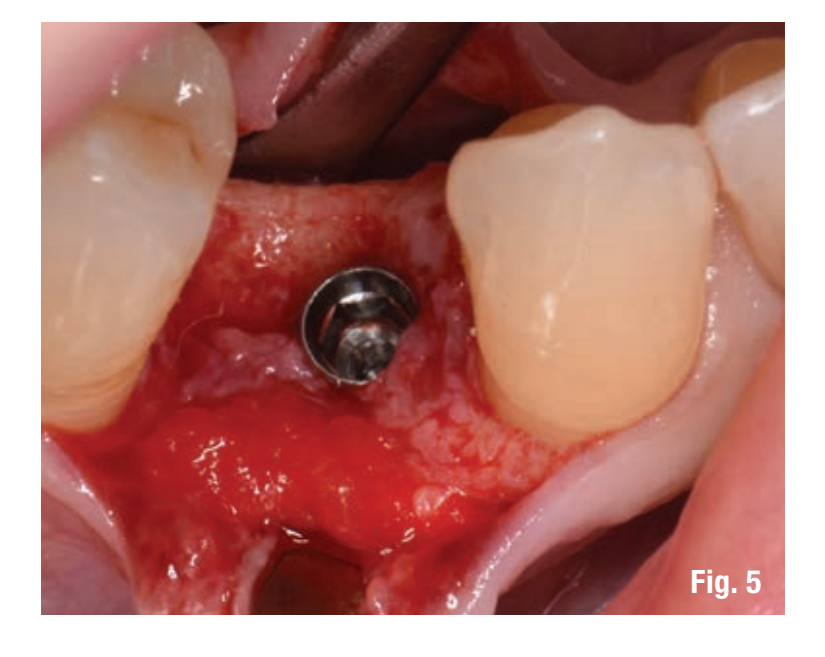
Before the extraction (S0), an intraoral scan was performed on each patient using the iTero scanner (Align Technology) (Fig. 2), and the scans were archived. Two months after the extraction, a full-thickness vestibular flap was created, the implant was inserted into the site (Figs. 3, 4), and the volumetrically stable porcine collagen matrix Geistlich Fibro-Gide (Geistlich Pharma) was placed, stabilizing it to the periosteum with two internal absorbable sutures (Fig. 5). The flap was then sutured with non-absorbable sutures and suspended stitches to ensure primary closure and keep the matrix submerged but not compressed (Fig. 6).

Patients were managed pre-surgically with 1 tablet of 1 g. of Augmentin antibiotic, therapy maintained for a total of 6 days with one tablet every 12 hours and 0.2% chlorhexidine rinses.
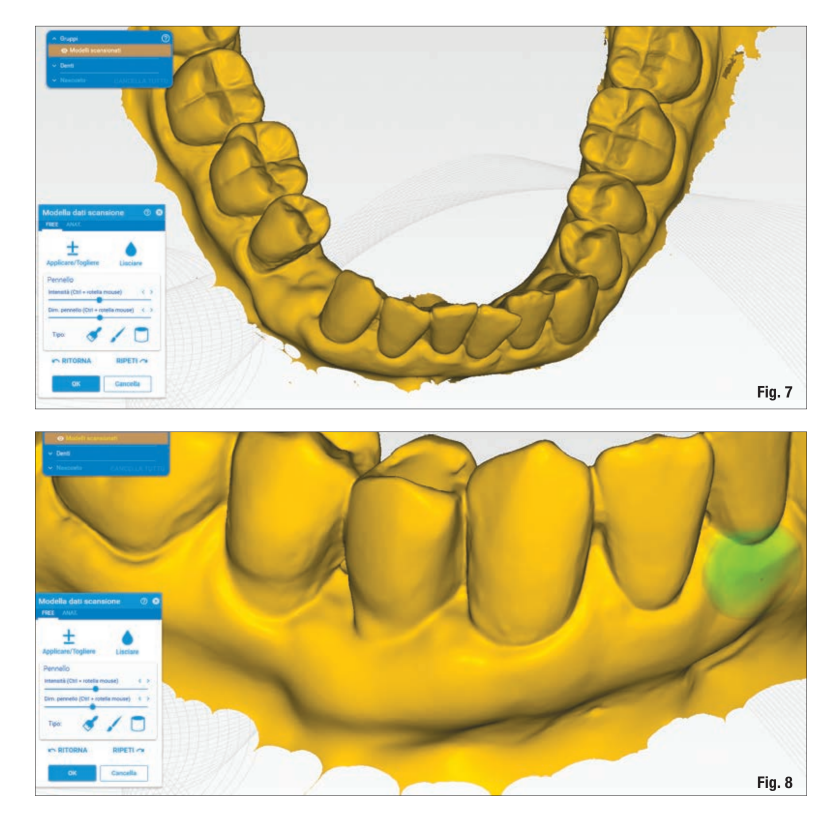
After 15 days, the sutures were removed and after 3 months from the insertion of the implant and the collagen matrix (S1), a second scan was performed (Fig. 7). After one year (S2), the last scan was performed (Figs. 8-10).

Each scan group for each patient was processed using exocad and analyzed by comparing S0 with S1 (three-month evaluation) and S0 with S2 (one-year evaluation) (Figs. 11, 12).
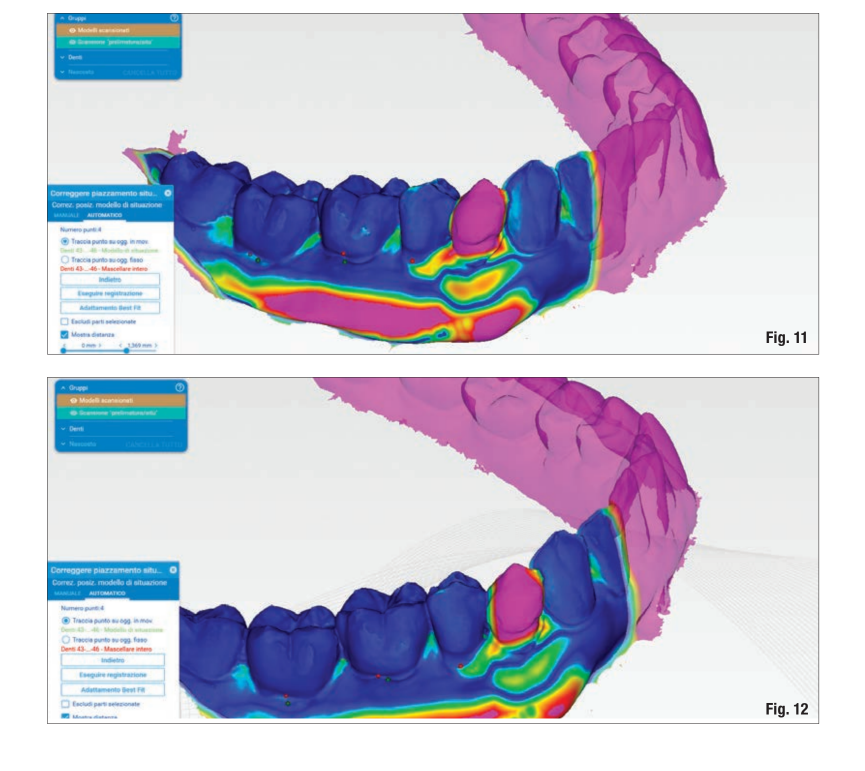
The evaluation of the area of interest concerns a trapezoidal zone located in the grafted part that expands from a hypothetical line connecting the margins of adjacent teeth and extends to the mucogingival line and laterally to the interproximal areas.
Through colorimetric visual analysis, it was possible to evaluate the volumetric increase at different time points: the STL obtained were analyzed with Rhinocerus software for the analysis of vestibular numerical-volumetric variations.
The data is still under analysis, and in this part of the study, only the colorimetric analysis in a range between 0 and 2 mm has been considered.
Results
The comparison group S0 with S1 (Fig. 11) shows a linear increase that settles in the range between 0 and 2 mm with areas within the region of interest colored green-orange-red. This result is present in all 10 analyzed cases.
In the comparison group S0 with S2 after one year (Fig. 12), there is a remodeling of the grafted area but with an increase compared to the baseline (S0) ranging between 0 and 1.5 mm, that is, with areas within the regions of interest colored blue-light blue-green. This result is present in all 10 analyzed cases.
The analysis of the results was based on the color scale with a range from 0 to 1.885 mm respectively with a color scale from blue to red (Fig. 12).
Discussion
This pilot study, within the limits of colorimetric analysis, allows for an effective and immediate evaluation of how, one year after the insertion of the volumetrically stable porcine collagen matrix Geistlich Fibro-Gide, there has been an increase in the grafted area with a consequent greater thickness of the peri-implant soft tissues. These results are aligned with those found by Huber et al. and Thoma et al. which demonstrate how collagen substitutes can, if properly stabilized, not only increase the area of interest but also remain stable over time.
It is interesting to analyze how in the first three months there is a significant volumetric increase that then tends to remodel and become stable after one year.
The evaluation of the S0-S1 group indeed highlights how there is a greater increase in the area of interest reaching peaks of red coloration (about 2 mm).
Analyzing the same scans, in the S0-S2 comparison group, there is a slight decrease that stabilizes at 1 year in a range that has led to a good average increase of around 1.00 - 1.50 mm.
Thoma et al. demonstrate how beneficial it is, to protect the peri-implant bone, to graft soft tissue to reduce marginal bone loss and to create a zone of keratinized tissue often capable of protecting the implant-prosthetic connection area. The grafting of soft tissues requires, in addition to knowledge of mucogingival surgery, the use of a donor site which can be a limitation for the patient's acceptance of the treatment plan.
Volumetrically stable collagen substitutes such as the Geistlich Fibro-Gide matrix used in the correct indications allow for not using the donor site from the palate, also enabling a faster and less painful healing period for the patient.
As evident from the data present in the literature and discussed above, we can consider the Geistlich Fibro-Gide matrix reliable for the augmentation of peri-implant soft tissues in order to harmonize the aesthetic result and to protect the entire implant-prosthetic system in the long term.
Conclusions
Within the limits of this pilot study, it can be stated that the use of the volumetrically stable porcine collagen matrix Geistlich Fibro-Gide allows, after one year, an increase in soft tissues in the vestibular graft area, without the need for a donor site. Further studies are needed to evaluate the long-term stability and quantify the actual extent of the increase.
Authors: M. De Francesco, E. Lorenzelli, S. Salucci, G. Dalmaschio, F. Grisolia, F. Tomarelli
References:
- Thoma, D. S., Villar, C. C., Cochran, D. L., Hammerle, C. H. and Jung, R. E. (2012) Tissue integration of collagen-based matrices: an experimental study in mice. Clinical Oral Implants Research 23, 1333–1339.
- Furhauser, R., Florescu, D., Benesch, T., Haas, R., Mailath, G. and Watzek, G. (2005) Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clinical Oral Implants Research 16, 639–644.
- Thoma, D. S., Buranawat, B., Hämmerle, C. H., Held, U., Jung, R. E. (2014) Efficacy of soft tissue augmentation around dental implants and in partially edentulous areas: a systematic review. Journal of Clinical Periodontology 41, S77-S91.
- Thoma, D. S., Benic, G. I., Zwahlen, M., Hammerle, C. H. and Jung, R. E. (2009) A systematic review assessing soft tissue augmentation techniques. Clinical Oral Implants Research 20 (Suppl. 4), 146–165.
- G. Zucchelli, L. Tavelli, M. K. Mcguire, G. Rasperini, S. E. Feinberg, H. Lay Wang, W. V. Giannobile. (2020) Autogenous soft tissue grafting for periodontal and peri-implant plastic surgical reconstruction. Journal of Periodontology 91(1), 9-16.
- Thoma, D.S., Zeltner, M., Hilbe, M., Hämmerle, C.H., Hüsler, J., Jung RE. (2016) Randomized controlled clinical study evaluating effectiveness and safety of a volume-stable collagen matrix compared to autogenous connective tissue grafts for soft tissue augmentation at implant sites. Periodontology 43(10), 874-885.
- Schneider, D., Grunder, U., Ender, A., Hammerle, C. H., Jung, R. E. (2011). Volume gain and stability of peri-implant tissue following bone and soft tissue augmentation: 1-year results from a prospective cohort study. Clinical Oral Implants Research 22, 28–37.
- Chappuis, V., Shahim, K., Buser, R., Koller, E., Joda, T., Reyes, M., Buser, D. (2018). Novel Collagen Matrix to Increase Tissue Thickness Simultaneous with Guided Bone Regeneration and Implant Placement in Esthetic Implant Sites: A Feasibility Study. Int J Periodontics Restorative Dentistry 38, 575-582.
- Huber, S., Zeltner, M., Hammerle, C.H., Jung, R. E., Thoma, D.S. (2012). Non-interventional 1-year follow-up study of peri-implant soft tissues following previous soft tissue augmentation and crown insertion in single tooth gaps. Journal of Clinical Periodontology 8, 1-9.
- Thoma, D.S., Naenni, N., E, F., Hämmerle, C.H., Schwarz, F., Jung, R., and Sanz-Sanchez, I. (2017). Effects of soft tissue augmentation procedures on peri-implant health or disease – A systematic review and meta-analysis. Clinical Oral Implants Research 29, 32-49.
- Thoma, D.S., Gasser, T.J.W., Jung, R.E., Hämmerle, C.H. (2020). Randomized controlled clinical trial comparing implant sites augmented with a volume-stable collagen matrix or an autogenous connective tissue graft: 3-year data after insertion of reconstructions. Journal of Clinical Periodontology 47(5), 630-639.
