Ridge Augmentation and Delayed Extraction Implant in a Central Incisor: Proper Management of Hard and Soft Tissues to Achieve Ideal Aesthetics
Machine translation
Original article is written in IT language (link to read it) .
Introduction
The implant rehabilitation of the anterior areas of the mouth represents one of the most complex implant-prosthetic procedures.
The anatomical characteristics of the area (upper incisors) with the presence of extremely thin cortical bone, bundle bone less than 1 mm in 87% of cases, the buccopalatal dimensions often below 9 mm, and the inclination of the dental root axis not aligned with the future implant axis, make it a critical area. At the same time, the upper incisor sector is the area with the highest aesthetic value, requiring extreme precision in the reconstruction of hard and soft tissues to create perfect symmetry with the adjacent natural teeth and allow for an aesthetically impeccable smile.
The indications for deciding whether to manage cases with extraction and immediate placement are strict and limit this procedure in aesthetic areas to a very limited number of cases. Much more common is the management in multiple phases (type 2 and 3) in which the extraction of the dental element must always be accompanied by an alveolar preservation technique or a ridge augmentation technique.
The Socket Preservation is indicated (Consensus Conference IAO 2020) in intact extraction sockets where, for anatomical reasons, primary stability of the implant, or aesthetic considerations, the placement of the implant must be postponed to 16/20 weeks.
In some clinical situations with a well-defined deficit of the alveolar ridge, at the time of extraction, it is possible to perform a contextual GBR using the Ridge Augmentation technique to allow for bone reconstruction and make the placement of the implant at 5/6 months easier and less invasive.
Some heterologous materials currently available have been shown to compensate for physiological ridge resorption in extraction sites and indeed in these regenerative procedures can represent the gold standard.
Materials and methods
Case report
The patient M.S., 45 years old, presents to our observation complaining of swelling at the level of the upper right central incisor 1.1. She reports a trauma in adolescence on this tooth with loss of vitality and the need for root canal therapy, and in 2004, following the onset of an apical granuloma, she underwent apicoectomy there (Fig. 1).

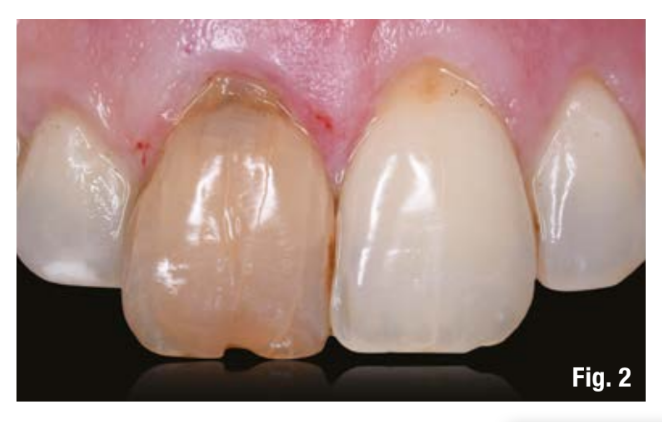
At the general objective examination, the patient presents a Class 2 malocclusion with multiple recessions in the frontal and lateral-posterior sectors, a gummy smile, and a thin and festooned gingival phenotype with triangular-shaped teeth. Locally, tooth 1.1 appears strongly discolored with an apical fistula, recession of the soft tissues of both 1.1 and 2.1 of about 3 mm with cervical erosion (Fig. 2). An initial two-dimensional radiographic investigation (periapical endoral x-ray) highlights an incongruous root canal treatment and apical radiolucency on 1.1. A three-dimensional CBCT examination reveals a discontinuity of the vestibular cortex identified as Class 4 according to Tarnow, as a result of the apical infection, but there remains a crestal bone bridge that will be essential for the reconstruction of hard and soft tissues (Fig. 3).

After a complete photographic session, the analysis of aesthetic, clinical, and radiographic risk factors identified the need to proceed with the extraction of 1.1 and its replacement with an implant-prosthetic rehabilitation according to a timing and a type 3 post-extraction protocol: extraction, management of bone and gingival volumes, and after 4/5 months, implant placement.
The goal of the first therapeutic phase (extraction therapy) was to use a highly predictable technique that would allow us to reconstruct the missing buccal bone wall (apical portion of the wall) and to maintain gingival volumes, allowing for the reconstruction of soft tissues, increasing their height and enabling, in the subsequent implant and prosthetic phase, the correct management of the interdental papilla.
After a plexus anesthesia with articaine 1:100,000, without incising the mesial and distal papillae, 1.1 is gently extracted with piezoelectric instruments preserving the existing buccal cortex (essential for managing the surgery); after a careful surgical cleaning of the site, a Ridge Augmentation with Socket Seal was performed.
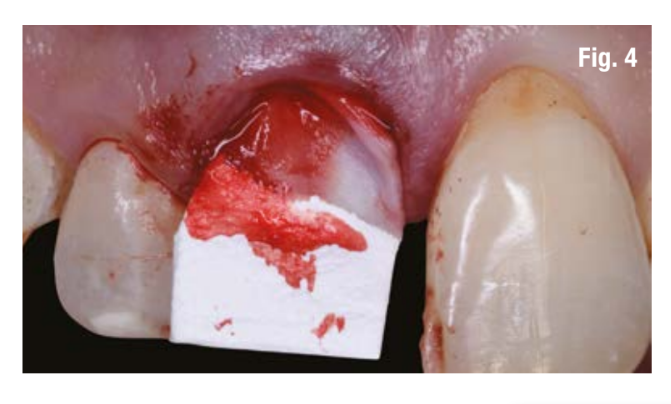
An intrasulcular vestibular incision was then made at the site without touching the papillae, sliding the blade along the crestal bone plane, and in the most apical portion where there was a discontinuity of the cortical bone, the blade was moved mesially and distally and further apically until the bone plane was found according to the CBCT indications; it was thus possible to insert a Geistlich Bio-Gide (Geistlich Pharma) porcine collagen membrane appropriately shaped to have support on the bone planes (Fig. 4); inside the alveolus, Geistlich Bio-Oss Collagen (Geistlich Pharma) was placed, deproteinized bovine bone with the addition of 10% porcine collagen, an osteoconductive material that, in addition to being a space maintainer and scaffold for bone regeneration, also serves as support for the overlying soft tissue (Fig. 5).

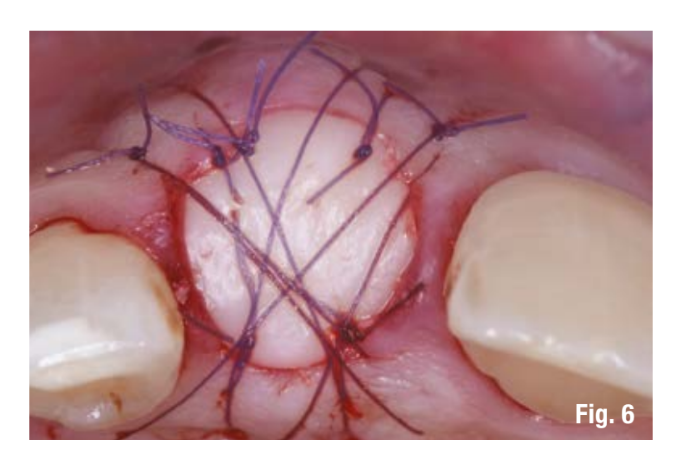
After palatal anesthesia, a circular punch biopsy of connective epithelial tissue was taken with a shape and size similar to the socket of 1.1 to be sealed; after the epithelialization of the margins of the socket, the punch was sutured above the bone substitute with Vicril 6-0 sutures (Johnson & Johnson) with detached stitches at the four corners and a compressive crossed mattress suture (Fig. 6). At this stage, the patient was rehabilitated with a Maryland bridge made of composite cemented adhesively.
The patient was discharged with supportive pharmacological therapy and two weeks later, the removal of the resorbable sutures was performed, with clinical checks carried out at 1 month, 3 months, and 5 months.
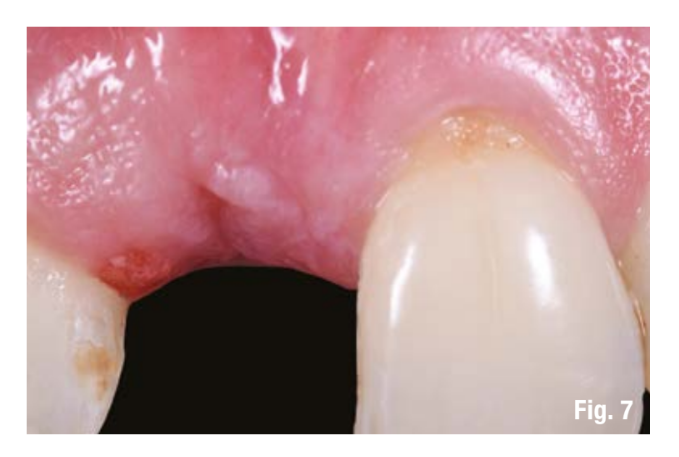
At the end of the tissue maturation phase (5 months) (Fig. 7), it was highlighted that from a clinical point of view, the volumes on the vertical plane were maintained (even more coronal by about 2 mm compared to the contralateral central 2.1) and on the transverse vestibulo-palatal plane, and furthermore, the new CBCT examination showed the reconstruction of the vestibular bone wall (Fig. 8).

The CBCT examination was integrated with digital impressions of the two arches using the Carestream 3600 optical scanner (Carestream Dental), and the Dicom and STL files along with the digital diagnostic wax-up were uploaded into a surgical planning software (3 Diemme) where the positioning of the implant on 1.1 was designed, Imax implant 3.3 x 13 (Ires Group), to be inserted via guided surgery with a dental-supported surgical template.
The computer analysis allowed for highlighting the correct implant positioning in three-dimensional space and, in the implant-centric representation, the presence of bone at 360°; it was also possible to seek primary implant stability that, along with a correct prosthetic emergence axis (palatal under the cingulum), would allow for managing an immediate load with a screwed provisional.
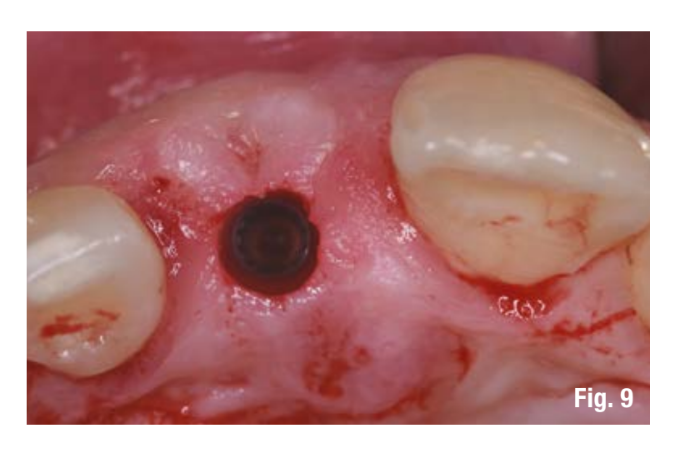
At the time of the implant surgery, with appropriate supportive antibiotic therapy (2 g of amoxicillin and clavulanic acid 1 hour before the procedure) and after a plexus anesthesia with articaine 1:100,000, the surgical template was positioned and the implant site was prepared with the dedicated surgical kit, using a sub-preparation technique, and then the programmed Imax implant "3.3 x 13" (Ires Group) was positioned; the insertion torque was greater than 70 Ncm and the resonance frequency measured with Osstel was 75 ISQ, thus confirming the possibility of performing immediate loading (Fig. 9).
The examination of the patient's smile highlighted the need to slightly correct the transverse plane of the root convexity of 1.1 in order to simulate the root draft and simultaneously correct the recession on element 2.1 which was causing an unevenness of the gingival margins and the harmony of the smile.
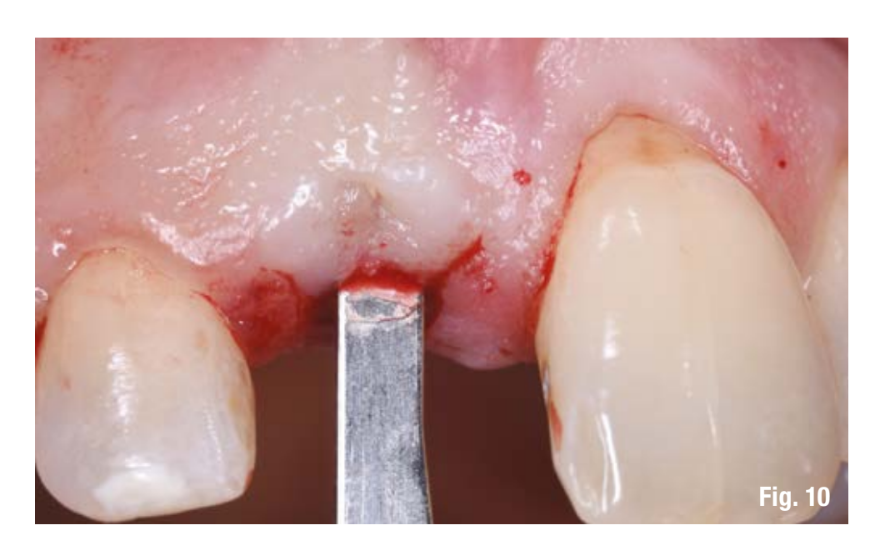
To minimize the invasiveness of the surgery and limit the management of the flap, a tunnel technique with an intrasulcular incision was performed (Fig. 10) that from the gingival margin of the implant preparation site 1.1, with a partial thickness incision, creates a vestibular pocket and then connects with the intrasulcular margin of 2.1 where, also with partial thickness, an incision was made beyond the mucogingival junction to allow for the mobilization of the flap and its movement in a coronal direction for root coverage.
To cover the recession on the natural tooth 2.1, after careful root planing and conditioning with EDTA (Prefgel Straumann), a palatal graft was taken through a rectangular incision of connective epithelium with a thickness of 1.5 mm, a height of about 4 mm, and a length equal to the area to be treated, about 10 mm (Fig. 11). Once the donor site was sutured, the epithelium of the graft was removed, allowing for a connective graft of 1 mm thickness and 4 mm height to be obtained, which was positioned and sutured with Vicril 7-0 suture (Johnson & Johnson) on the recession of 2.1. The flap was then repositioned coronally and secured in this position with a 4-0 Eptfe suture (Omnia) anchored to the vestibular surface of the crown of 2.1.

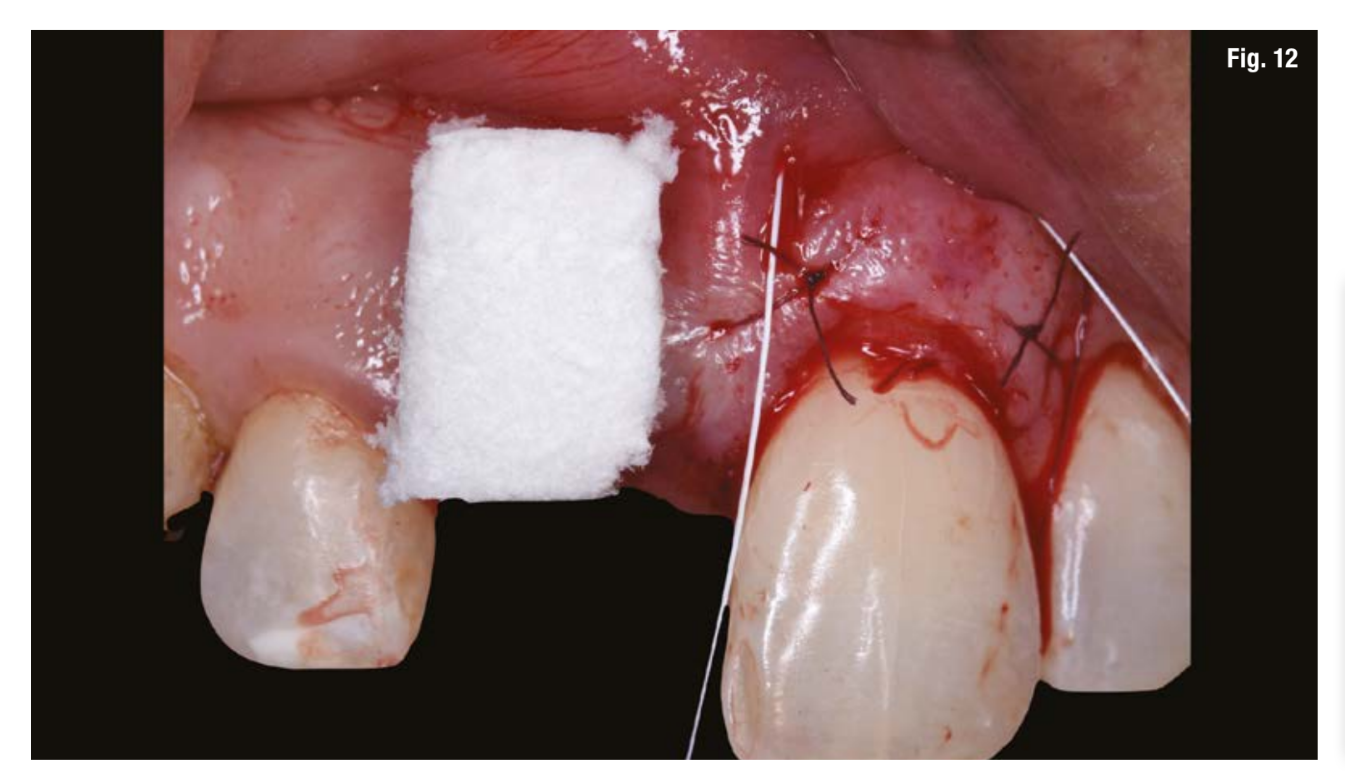
At the implant level 1.1, a volumetrically stable heterologous matrix of porcine origin Geistlich Fibro-Gide (Geistlich Pharma) (Fig. 12) was inserted in a pouch stabilized with a resorbable suture Vicril 6-0 (Johnson & Johnson) which, thanks to its excellent integration and stability over time, will allow for the reconstruction of the root bump and achieve an ideal volume of soft tissues around the implant.
The procedure was completed with a digital impression of the soft tissue path and the position of the implant with scan body, and the file was sent to the laboratory for the finalization of the temporary.
The laboratory that had already performed the digital diagnostic wax-up optimized the creation of the screw-retained provisional crown with the new profile of the corrected soft tissues. It is essential at this stage to properly manage the subgingival profile of the provisional (beak wings), keeping it concave without creating compression on the grafted tissues and allowing for proper maturation, and only later possibly increasing the convexity with flow composite. The mesial and distal contact points were managed according to the indications of Tarnow and Coll. to achieve complete reformation of the interdental papillae and a correct gingival parabola.
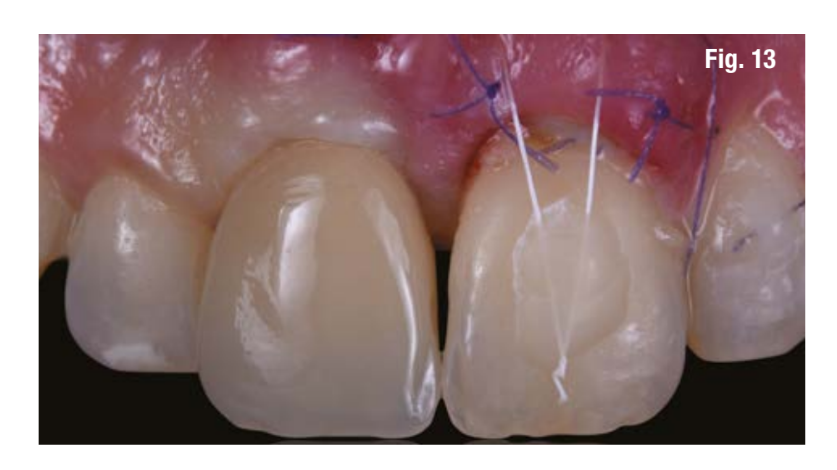
24 hours after the surgery, the provisional was placed with no vestibular compression for a non-functional immediate load, naturally freeing it in the contacts of centric, protrusive, and lateral movements (Fig. 13). A few hours after the procedure, perfect tissues are evident, with an ideal volume created by the matrix, which will now be supported in the healing phase by the presence of the provisional crown shaped this way (Fig. 14).

The patient was discharged with supportive pharmacological therapy and was re-evaluated with clinical and joint checks at 2 weeks (suture removal), and then at 4, 8, 12, and 16 weeks, observing the maturation of the soft tissues and radiographic bone healing.
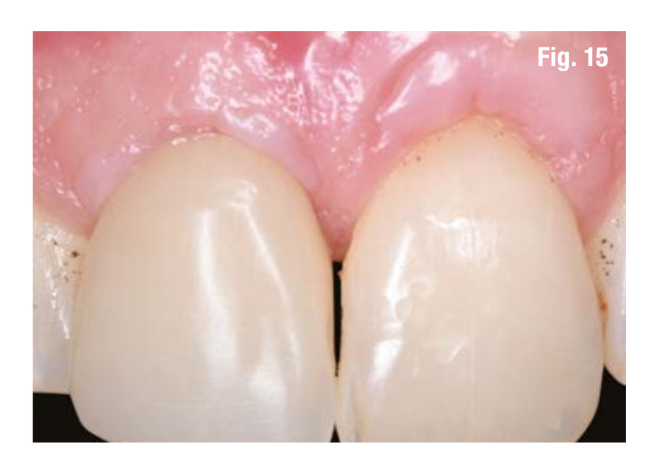
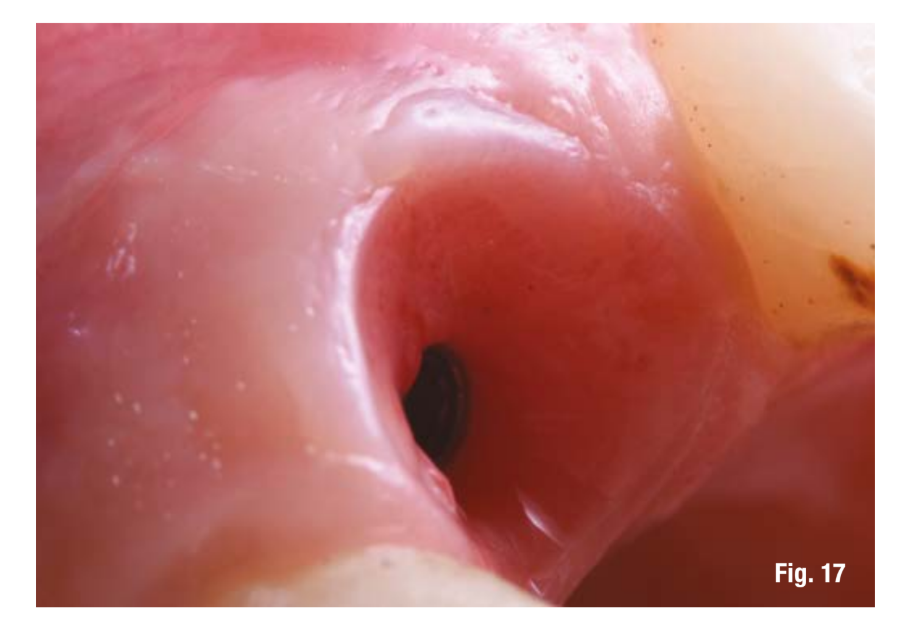
Four months after implant surgery, we achieved excellent leveling of the gingival contours in the frontal plane with the restoration of a correct and ideal anatomy of both the gingival margins of 1.1 and 2.1 and the mesial and distal interproximal papillae to the crown on the implant of 1.1 (Fig. 15), while the removal of the screwed provisional allowed us to highlight in the transverse plane the conditioning of the soft tissues, the perfect integration of the Fibro-Gide matrix (Geistlich), and the vascularization of the site with circumferential fibers restoring the correct ideal anatomy around a crown on an implant from the center to the periphery with connective tissue, junctional epithelium, and sulcular epithelium (Figs. 16, 17); the new resonance frequency level rose to 81 ISQ.

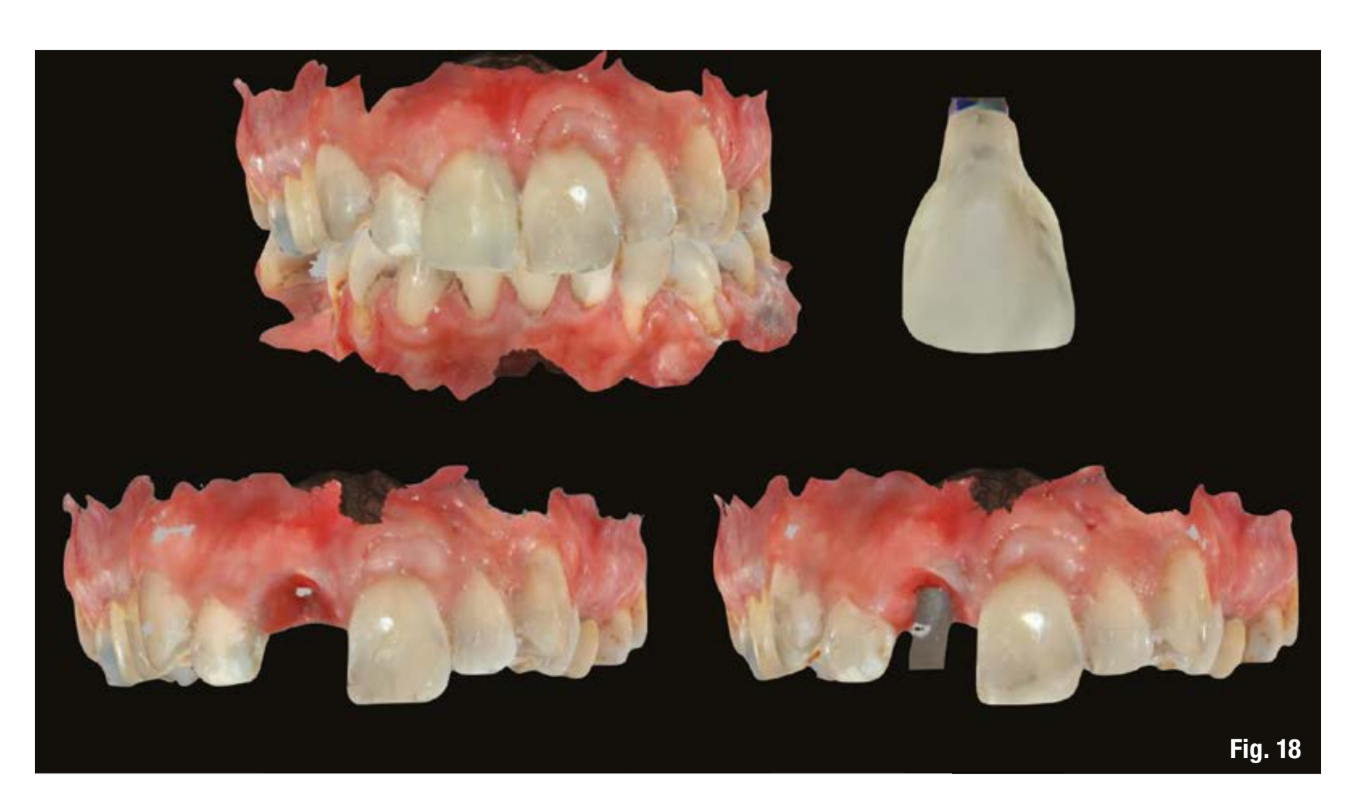
The case finalization involved the use of a digital scanning protocol with optical impression of the dental arch with the provisional in situ, the provisional outside the mouth, the conditioning of the soft tissues (transmucosal pathway), and the implant position recorded with the scan body, in addition to the antagonist impression and the occlusal registration check (Fig. 18): all of this allows for reading the conditioning of the obtained soft tissues and the profile of the provisional (corrected during the healing phase) that determined it and recreating a definitive crown that "rests" perfectly in the tissues thus obtained.
The laboratory phases, also carried out with a nearly completely digital process (the need to have a working model in polyurethane for the layering of the ceramic), involved the creation of a layered zirconia ceramic crown screwed with a concave subgingival emergence profile that respects the conditioning of the soft tissues obtained from the grafts (epithelial connective punch from the extraction phase and heterologous matrix in the implant phase) and their prosthetic modeling during immediate loading.
After an aesthetic test of color and surface texture, and a two-dimensional radiographic check, the case was finalized by positioning the screw-retained ceramic restoration, which was tightened with a torque of 25 Ncm (Fig. 19).
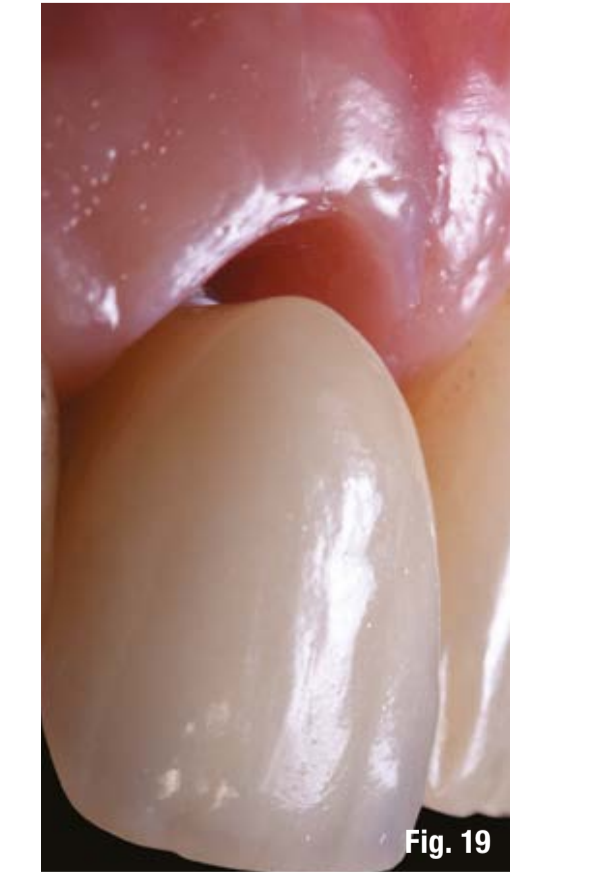
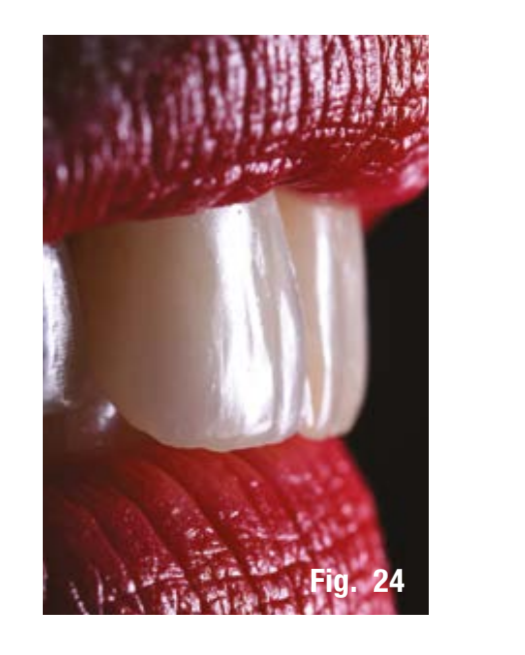
An ideal and completely natural camouflage was achieved both regarding the white component of the restoration (ceramic) and the pink component (profile, thickness, and anatomy of the soft tissues), resulting in excellent aesthetics (Figs. 20-24).




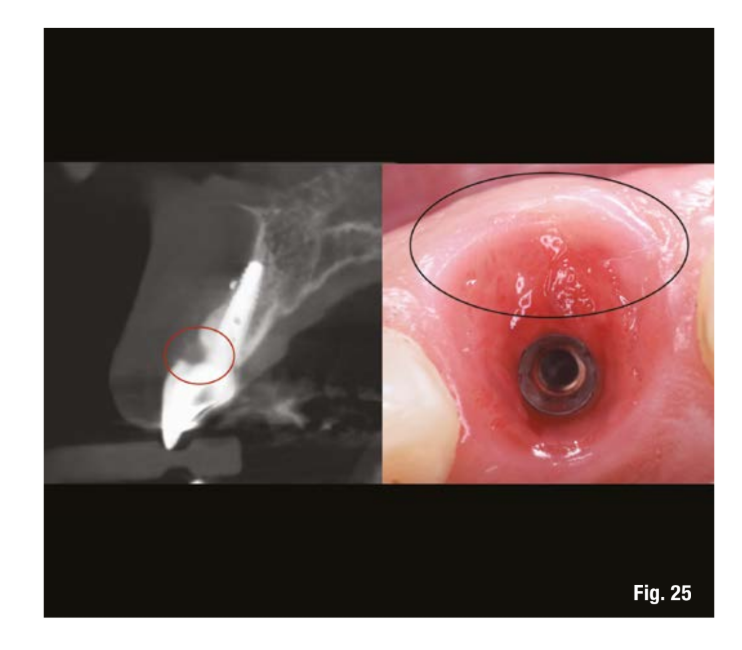
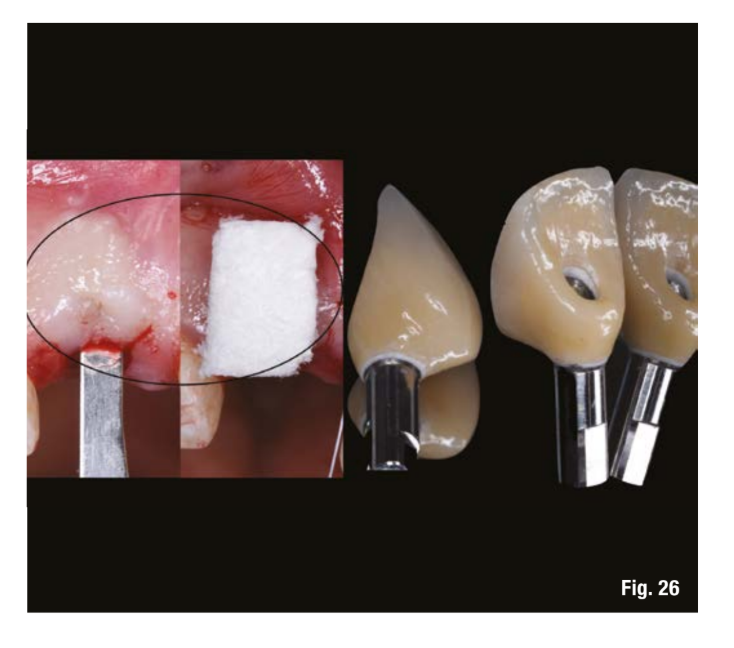
The clinical and three-dimensional radiographic control after 2 months highlighted the perfect integration of the prosthetic crown, and the radial images from the CBCT show both the presence of well-maintained cortical bone that respects the 2 mm required by the indications of the Scientific Literature (ITI Treatment Guide Vol. 1-6), as well as the radiolucent crestal vestibular space occupied by the soft tissue obtained through the heterologous matrix graft and the appropriate morphology of the subgingival profile of the prosthetic crown (Figs. 25, 26).
Discussion
The clinical case described highlights how the management of a case with high aesthetic value requires a strict and scientifically validated protocol from the clinician, as well as autogenous or xenogenic materials that provide predictability and stability over time.
The success of an implant rehabilitation in the aesthetic zone relies on the correct management according to a 4D protocol, where the implant positioning, more palatal and apical, the implant design, reduced implant diameter and platform switching, the prosthetic design, abutments and crowns with a concave profile, and the correct volumes of hard and soft tissues are fundamental.
A systematic review of the literature by Jung highlights that 5 years after the implant-prosthetic rehabilitation of a frontal sector, aesthetic complications can reach up to 13.6%. This poses the risk, as described by Chen and Buser, that the onset of soft tissue recession of up to 2 mm, exposure of the prosthetic abutment, gingival margin leveling, and the lack of a proper interdental papilla can compromise the aesthetic outcome of our procedures.
In the approach to post-extraction implantology cases, the 2019 Consensus Report outlines a decision-making pathway for treating aesthetic cases with different modalities (type 1, 2, 3), focusing on the presence of infection, the possibility of achieving primary implant stability, the presence of intact or resorbed sockets, the type of periodontal phenotype, aesthetic requests, and any systemic diseases that may be present.
Immediate post-extraction procedures in the frontal area are therefore limited to well-selected cases to avoid the previously described aesthetic complications.
As in the described clinical case, it is more common to have to extract the dental element and proceed with a delayed implant placement at 16/20 weeks.
At the time of extraction, however, we have a sequence of events well described in the literature that leads to resorption of the bundle bone and thus the vestibular cortex of the ridge, with an average reduction in thickness of 3.79 mm in the horizontal plane and 2.3 mm in the vertical plane. All of this is accompanied by an apical and horizontal shift of the soft tissues.
Since the vestibular cortical bone at the level of the maxillary central incisors has an average thickness of 1.08 mm (range 0.45-1.75 mm), it is clear how the simple extraction of an incisor without additional procedures leads to significant alveolar remodeling that will then require important horizontal and vertical bone regeneration at the time of implant placement.
The placement of Geistlich Bio-Oss Collagen at the time of extraction does not prevent the resorption of the bundle bone, but tends to predictably preserve the volume of the ridge: it will result in a compensation of the vestibular marginal bone contraction with bone regeneration within the extraction socket. Therefore, we are not talking about true preservation of the socket but rather about preservation of the ridge volume, with a compensatory mechanism involving internal regeneration.
The Ridge Augmentation technique allows, as in the described clinical case, for guided bone regeneration within the extraction site concurrent with extraction in a situation of mild to moderate bone defect. The placement of a resorbable collagen membrane on the vestibular bone defect and the management of the extraction socket with an osteoconductive biomaterial optimizes the healing of the extraction site, limiting the extent of regenerative procedures at the time of subsequent implant placement.
The Ridge Augmentation procedure is completed and achieves a better clinical result when it is also associated with a Socket Seal technique: the closure of the extraction socket with a connective graft helps to partially compensate for the vertical resorption of the soft tissues and results in an increase in the volume of the tissues at the base of the future papilla, allowing for its correct reformation according to the indications expressed by Tarnow and Roccuzzo.
Since 2012, the use of a porcine collagen xenogenic matrix, Geistlich Mucograft (Geistlich Pharma), taking advantage of its excellent integration into the tissues at 30 days and its complete integration at 6 weeks, has shown that it can be used in the closure of the extraction socket with predictable results comparable to the classic epithelial connective graft, eliminating the need for access to a second surgical site (donor site) and thus significantly reducing morbidity for the patient.
The restoration of the correct peri-implant phenotype to achieve stability of hard and soft tissues over time also requires creating a quantity of keratinized gingiva greater than 2 mm, a thickness of soft tissues at the crest level greater than 2.5 mm, and a height of the soft tissue above the crest greater than 3 mm.
It is therefore important to manage the soft tissues on a horizontal plane, modifying the thickness of the vestibular connective tissue to provide long-term stability to our implant-prosthetic restorations. Soft tissue grafting procedures, essential in patients with a thin and scalloped phenotype, can be performed during the Ridge Augmentation phase, implant placement, or at the uncovering of the implant itself. The gold standard is represented by connective tissue grafting harvested from the palatal mucosa or the tuberosity, but currently, the use of a new volumetrically stable porcine collagen heterologous matrix (Geistlich Fibro-Gide) has shown comparable results in terms of tissue thickness increase with clinical, radiographic, and profilometric analysis, with stable results over time with a 3-year follow-up.
A recent systematic review of the literature with meta-analysis compared connective grafts and heterologous collagen matrices in increasing mucosal thickness and changes in the quantity of keratinized mucosa, as well as secondary effects related to the patient and the surgical procedure. The results, despite the limitations of the number of available randomized clinical studies, 7 with 218 implant sites, led to equivalent results for the increase of perimplant soft tissues between collagen matrices and connective tissue grafts.
As for the secondary aspects, the advantages of matrices, both those used for closing extraction sockets and those for increasing volume and keratinized tissue, are certainly represented by a lower operative morbidity, greater comfort for the patient, a reduction in discomfort and postoperative pain, as well as a reduction in chair time.
Conclusions
The implant replacement of upper incisors represents a challenge for the clinician in which every surgical and prosthetic step is dictated by scientific principles aimed at restoring the structural unit: bone, soft tissues, implant, prosthetic crown with the reconstruction of an ideal implant phenotype. The heterologous materials currently available both as bone substitutes and soft tissue substitutes allow for reduced invasiveness of implant surgery and achieve stable predictive results over time.
Author: Filippo Tomarelli, Maurizio De Francesco
