Management of peri-implant soft tissues in post-extraction implant placement with digitally customized healing abutments. A clinical case.
Machine translation
Original article is written in IT language (link to read it) .
The conditioning of peri-implant tissues in post-extraction cases is very important. Purpose: it is to describe the conditioning of soft tissues achievable with digitally customized healing screws obtained from CAD/CAM technology. This case report describes the procedure to digitally customize healing screws in order to speed up and improve clinical practice. Materials and methods: a 36-year-old non-smoking patient, ASA 1, rehabilitated on 1.5 with implant-supported prosthesis. Before the extraction, an intraoral scan of the tooth and surrounding areas was performed, and a digitally customized healing screw was placed. After three months, the definitive prosthesis was executed. After one year, the affected area was scanned to compare the volumetric changes of the peri-implant tissues. Results: clinically, after one year, the method with digitally customized healing screws proves to be an effective method and in this case has ensured healthy peri-implant tissues. Conclusions: the procedure has proven to be very accurate and makes the digital workflow fast and comfortable for both the patient and the clinician.
Introduction
It is widely described in the literature that there are dimensional changes in the bone after an extraction. The dimensional changes vary depending on the sites and occur mainly in the first 6 months. The flapless insertion of an implant drastically reduces this phenomenon of resorption of the alveolar bone. Tarnow et al. investigated through a retrospective study how the horizontal volume of the alveolar bone could vary after the placement of a post-extraction implant. The transverse bone resorption was evaluated in 4 common clinical situations of post-extraction implants: with simultaneous bone grafting with and without a provisional and in the absence of bone grafting with and without a provisional. The best results were obtained by inserting a graft and stabilizing it with a healing screw or with a customized provisional. This case report aims to describe a method for stabilizing the graft after the insertion of a post-extraction implant using a customized healing screw obtained through a complete digital workflow. The possible advantages range from speeding up and simplifying the technical-clinical procedures to greater dimensional accuracy of the healing screw itself.
Case Presentation
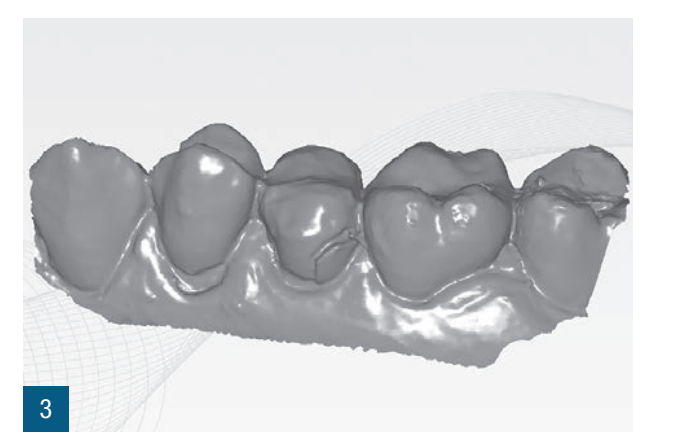
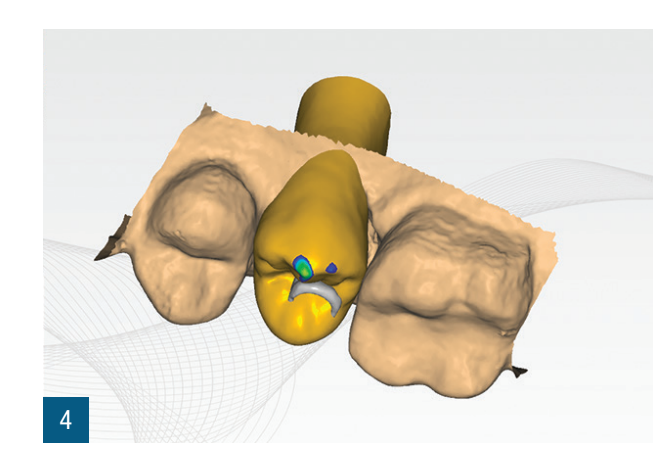
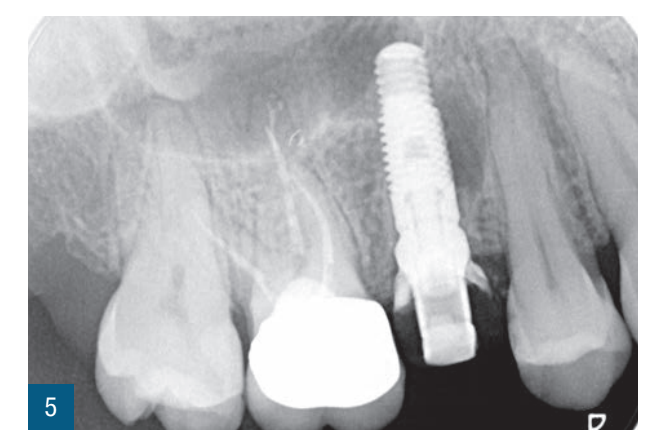
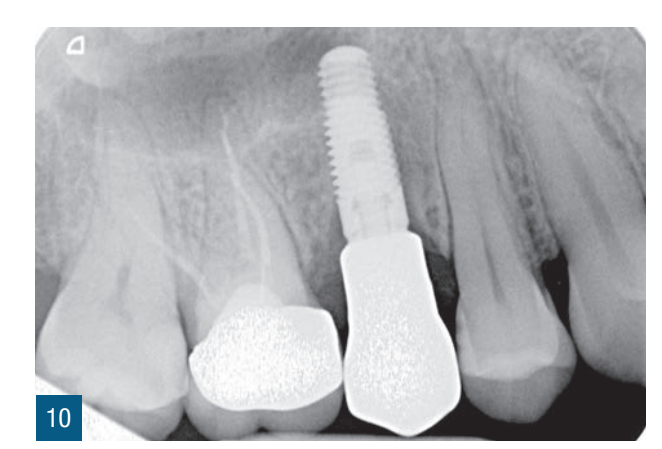
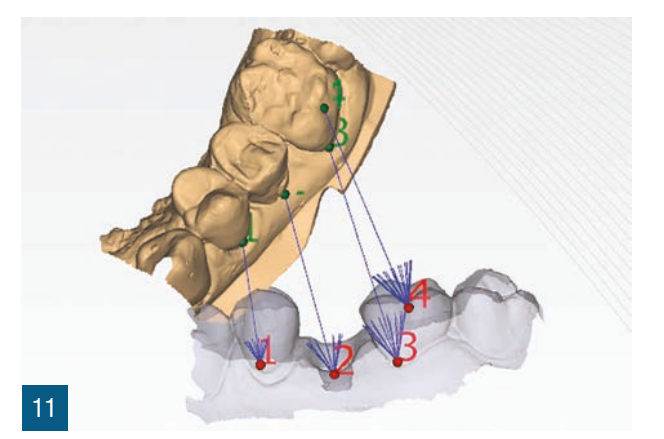
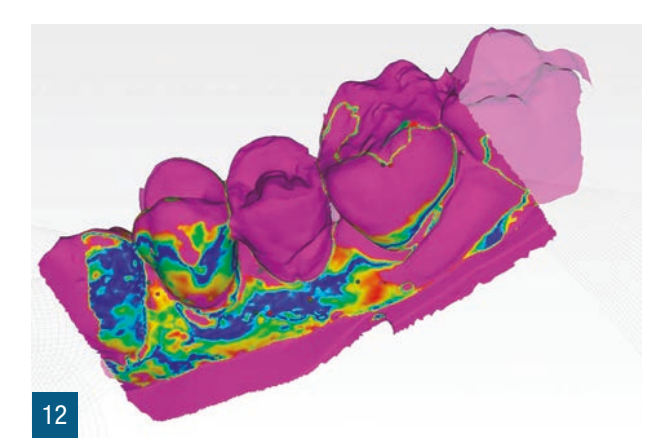
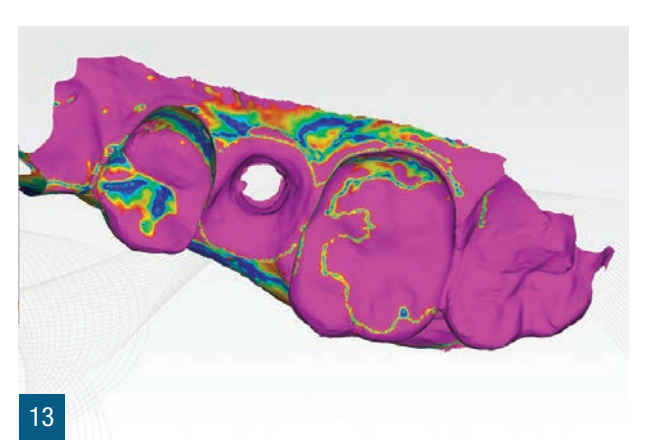
A 36-year-old female patient presented to our attention for a partial fracture of the crown of the right second premolar (1.5). After confirming the impossibility of conservative restorative recovery, an immediate post-extraction implant-prosthetic treatment was planned for the replacement of the compromised element (Figs. 1,2). The patient, a non-smoker, was classified as ASA 1. A localized CBCT was then performed in the area of interest to verify the presence and morphology of the vestibular bone side at the element to be extracted from the alveolar process. Before extracting 1.5, an intraoral digital impression (iTero Flex, Align Technology) of the dental element and surrounding areas was taken (Fig. 3). After administering local anesthesia, the extraction was performed, limiting trauma to the periodontal tissues by separating the roots and using mini levers and periotomes to preserve the vestibular bone plate. After assessing the alveolar integrity and favorable anatomical conditions, an implant of appropriate dimensions was placed to ensure adequate primary stability (4.1 x 11.5 TSVH ZimmerBiomet). The implant was positioned in a palatal proximal position according to the literature guidelines (Figs. 6,7), filling the gap between the implant and the vestibular cortical bone with an allograft (Copioss Zimmer-Biomet). The mounting device was shaped as if it were an abutment, and after being screwed onto the implant, it was scanned. From the intraoral digital scan, the CAD design of the healing screw was executed (Fig. 4). Both the pre-extraction scan and the scan with the mounting device transformed into an abutment will be used in the design to reproduce the healing screw as faithfully as possible. The morphology of the healing screw will replicate the existing tissue conditions at the time of surgery and will help avoid aesthetic issues concerning the pink aesthetics. Once the digital design was completed, a 3D print in resin (Lab2 Formlab) of the customized healing screw was performed. After printing, the healing screw obtained with Nextdent resin was cemented with auto and light-curing resin cement (Relix Unicem, 3M) to the abutment obtained from the mounting device and then screwed onto the implant (Figs. 5,6). Radiographic checks were performed three months and one year later (Figs. 7,8). After 3 months, the definitive crown was made through a digital workflow using the same scanner and dedicated scan bodies (Gentek, Zfx) that allow for the identification of the exact spatial position of the implant. One week later, the definitive monolithic zirconia crown was delivered, screwed onto the ti-base (Figs. 9,10). After one year, an additional scan was performed to evaluate any volumetric changes in the peri-implant tissues over time. The scans performed in the pre-extraction phase and at one year were processed with dedicated software (meshlab) to assess dimensional changes (Figs.11-13).






Discussion
In relation to the clinical objectives described by Tarnow et al., this clinical case highlights how the simultaneous stabilization of the bone site and the filling of the existing gap with heterologous material allows for the maintenance of the horizontal and vertical volumes of the post-extraction site. The speed and ease of performing a customized healing screw with this method improves the seal of the transmucosal pathway and maintains the pre-extraction morphological and volumetric characteristics. If non-anatomical healing screws of a larger diameter were used, we would certainly have a better seal compared to standard commercial healing screws, but they would not allow for an exact reproduction of the boundaries of the post-extraction site like a customized healing screw obtained with analog and/or digital methods. Digitalization allows for a substantial reduction in execution times and greater customization of the obtained artifact. The faithful reproduction of the existing situation can likely guarantee the implant a lower number of maintenance interventions, such as screwing and unscrewing, during the trial phases. This case report suggests that the stabilization of peri-implant tissues can ensure optimal healing and maturation of the tissues, simplifying the final prosthetic phases. This may help avoid further interventions to manage peri-implant tissues such as second surgeries, grafts, and the use of temporaries. The CAD phase allows for the faithful reproduction of the emergence profile by copying the shape of the cervical third of the tooth. Furthermore, it should be noted that the analog creation of the healing screw requires downtime that can be used for other purposes, thus speeding up the workflow and achieving the final result during intraoperative management. The use of pre- and post-surgical digital scans has allowed for the comparison of peri-implant tissue volumes, overlaying the pre- and post-surgical scans at three months and one year to highlight volumetric changes. This is a useful tool for potential clinical evaluations, but also as communication with the patient.
Conclusions
This case report was the first in a series of cases that led to a new aesthetic workflow. Considering the limitations of a single clinical case, the digital approach to the workflow for creating a customized digital screw proves to be reliable and accurate, moreover speeding up and improving the comfort of both the patient and the clinician.
Maurizio De Francesco, Grazieli Dalmaschio, Giuseppe Marano, Filippo Tomarelli, Piero Venezia, Riccardo Scaringi
References:
- Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005 Feb;32(2):212-8.
- Fickl S, Zuhr O, Wachtel H, Stappert CFJ, Stein JM, Hürzeler MB. Dimensional changes of the alveolar ridge contour after different socket preservation techniques. J Clin Periodontol. 2008 Oct;35(10):906-13.
- Iasella JM, Greenwell H, Miller RL, Hill M, Drisko C, Bohra AA, Scheetz JP. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003 Jul;74(7):990-9.
- Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003 Aug;23(4):313-23.
- Tarnow DP, Chu SJ, Salama MA, Stappert CFJ, Salama H, Garber DA, Sarnachiaro GO, Sarnachiaro E, Gotta SL, Saito H. Flapless postextraction socket implant placement in the esthetic zone: part
- The effect of bone grafting and/or provisional restoration on facial-palatal ridge dimensional change-a retrospective cohort study. Int J Periodontics Restorative Dent. May-Jun 2014;34(3):323-31.
- Bäumer D, Zuhr O, Rebele S, Hürzeler M. Socket Shield Technique for immediate implant placement - clinical, radiographic and volumetric data after 5 years. Clin Oral Implants Res. 2017 Nov;28(11):1450-1458.
- Brownfield LA, Weltman RL. Ridge preservation with or without an osteoinductive allograft: a clinical, radiographic, micro-computed tomography, and histologic study evaluating dimensional changes and new bone formation of the alveolar ridge. J Periodontol. 2012 May;83(5):581-9.
- Patzelt SBM, Emmanouilidi A, Stampf S, Strub JR, Att W. Accuracy of full-arch scans using intraoral scanners. Clin Oral Investig. 2014 Jul;18(6):1687-94.
- Yuzbasioglu E, Kurt H, Turunc R, Bilir H. Comparison of digital and conventional impression techniques: evaluation of patients’ perception, treatment comfort, effectiveness and clinical outcomes. BMC Oral Health. 2014 Jan 30;14:10.
- Giménez B, Özcan M, Martínez-Rus F, Pradíes G. Accuracy of a digital impression system based on active wavefront sampling technology for implants considering operator experience, implant angulation, and depth. Clin Implant Dent Relat Res. 2015 Jan;17 Suppl 1:e54-64.
- Nayyar N, Yilmaz B, McGlumphy E. Using digitally coded healing abutments and an intraoral scanner to fabricate implant-supported, cement-retained restorations. J Prosthet Dent. 2013 Apr;109(4):210-5.
- Camargo PM, Lekovic V, Carnio J, Kenney EB. Alveolar bone preservation following tooth extraction: a perspective of clinical trials utilizing osseous grafting and guided bone regeneration. Oral Maxillofac Surg Clin North Am. 2004 Feb;16(1):9-18, v.
- Sarnachiaro GO, Chu SJ, Sarnachiaro E, Gotta SL, Tarnow DP. Immediate Implant Placement into Extraction Sockets with Labial Plate Dehiscence Defects: A Clinical Case Series. Clin Implant Dent Relat Res. 2016 Aug;18(4):821-9.
- Abrahamsson I, Berglundh T, Lindhe J. The mucosal barrier following abutment dis/reconnection. An experimental study in dogs. J Clin Periodontol. 1997 Aug;24(8):568-72.

