Reconstruction of the jaws after facial trauma: implants, orthodontics, and maxillofacial surgery
Machine translation
Original article is written in ES language (link to read it) .
Introduction
The reconstruction of secondary deformities following facial trauma poses a significant challenge for maxillofacial surgeons. A surgeon with experience in orbitopalpebral surgery, rhinoplasty, and orthognathic surgery in combination with orthodontics, pre-prosthetic surgery, and implants is required. The management of avulsions of the alveolar process with implants is essential.
The combination of aesthetic and reconstructive surgical techniques produces the best results; however, in small deformities, the approach requires multiple surgeries due to its complexity. After panfacial fractures, sequelae are common, especially when orbitozygomatic and nasoethmoidal fractures are combined. In complex fractures with dental and alveolar process losses, achieving intermaxillary immobilization and perfect fracture reduction is challenging. If the sequelae of fractures are complex and affect multiple areas, the best results are obtained through an organized approach with exposure of the fracture areas, reduction after maxillary and orbital osteotomies, rigid fixation, and autologous bone grafts primarily taken from the calvaria. This is combined with pre-prosthetic surgery techniques, implants, and cosmetic surgery.
Clinical case
Post-traumatic. Complex facial reconstruction.
The 32-year-old female patient was referred for facial and maxillary reconstruction after suffering a traffic accident with panfacial fracture affecting both orbits, nasoethmoidal areas, and maxillae.
The patient had previously undergone surgery by non-maxillofacial surgeons and presented various sequelae (figures 1-5). The frontal view demonstrates significant orbital malposition with enophthalmos of the left orbit, vertical orbital dystopia, and telecanthus; the nose is deviated and laterally displaced to the left. The septum is deviated to the left with a C-shaped deformity, resulting in nasal respiratory insufficiency. The maxilla is retropositioned and displaced to the left with missing teeth, crown fractures, and left crossbite. In the profile view, the sinking of the nasal radix and the lack of support for the lip due to edentulism and maxillary fracture are prominent. The chin is retropositioned.

A series of objectives were established to try to return the patient to a premorbid state and even improve her aesthetics by taking advantage of successive surgeries. Due to the complexity of the sequelae, it was explained to the patient that she would require multiple surgeries in which aesthetic and reconstructive procedures on the soft and hard tissues of the face would be combined, fitting into a global reconstruction plan for the aesthetic units of the face. A very important part of the reconstruction would be in orthognathic surgery to subsequently place the nose and orbit in their proper position and perform implants in the prosthetically appropriate locations.
Objectives:
- Preoperative orthodontics.
- Maxillary reconstruction surgery through orthognathic surgery with autologous bone grafts to stabilize the osteotomies and subsequently place implants.
- Nasal reconstruction with rib grafts.
- Orbital reconstruction with external and internal cantopexy.
- Left orbital reconstruction with bone grafts.
- Genioplasty.
- Subepithelial connective tissue grafts.
- Osseointegrated implants.
- Mid and frontal third lift.
- Review of scars and fat grafts in the mid third and lip.
- Bridge over implants and reconstruction of crown fractures of fractured teeth.
Evidently, all these objectives required four surgical procedures.
Phase I: Upper jaw reconstruction (figures 6 and 7)
After a 12-month orthodontic process, a Lefort I osteotomy for advancement and centering was performed. The maxilla was moved as a block to the right and advanced.
The osteotomy was rigidly fixed with two miniplates, and grafts were taken from the cranial vault which were placed on the left maxilla and the alveolar process in onlay to subsequently place implants in the edentulous segments secondary to the avulsion of the alveolar process.
The procedure went without complications, continuing later with orthodontics.

Phase II: Nasal reconstruction and genioplasty (figures 8 and 9):
After creating a platform on the maxillae at 10 months, a procedure was planned mainly for aesthetic surgery.
Grafts were taken from the 6th rib and a centered and augmentation rhinoplasty was performed.
Septoplasty improved the axis of the nose and breathing. The rib was fixed with a Kirschner wire for 15 days. Genioplasty was performed by advancing the chin 6 mm, fixed with plates and screws of 1.6 mm, and the mentalis muscle and chin tuft were suspended.
The patient was discharged 24 hours later with the nasal packing removed.

Phase III: Orbital-Nasal Reconstruction:
This is undoubtedly the most complex phase of the reconstruction. Transnasal cantoplexy was performed with three wires to fix the inner canthus and telecanthus. The left orbit was reconstructed with calvarial grafts to support the eyeball and was fixed with 2 mm screws. Finally, external canthopexy was performed at the external orbital rim transosseously. A dermis graft was performed on the nose and osteotomies on the left nasal side. The improvement in facial aesthetics was considerable, and the bone reconstruction of the fractures was completed.
Phase IV: The final phase corresponds to the aesthetic reconstruction of soft tissues along with refinements of the previously performed procedures (figures 10-13).
Endoscopic lifting of the upper third was performed along with suspension of the middle third, improving the superolateral part of the orbit, adding more volume to the zygomatic area. Scars in the nasolabial area were reviewed, and fat grafts were placed in the nasolabial region and lip.
Osteointegrated implants were placed in the maxilla previously grafted with cranial bone. The grafts had undergone minimal resorption, achieving good primary stability. A subepithelial corrective tissue graft was taken from the palate. Three months later, the second phase of the implants was performed. Provisional restorations were placed to shape the gingival tissue and achieve papilla and adequate aesthetics.


Discussion
Patients who suffer from complex fractures often develop secondary deformities. Delays in treatment, avulsion of tissues, and iatrogenesis lead to severe aesthetic and functional alterations with significant disfigurement and misalignment of the orbit, nose, and jaws. The secondary deformities resulting from these sequelae must be individualized to reconstruct vision, nasal breathing, intermaxillary relationships, and the alveolar process. The patient must be informed of the need for multiple and complex surgeries as well as additional cosmetic and dental procedures.
Altered intermaxillary relationships are resolved with orthognathic surgery procedures that reconstruct a stable platform.
Autologous grafts are always used. Dental avulsions from the alveolar process are reconstructed with grafts and, subsequently, with osseointegrated implants once orthodontics is completed and considered stabilized.
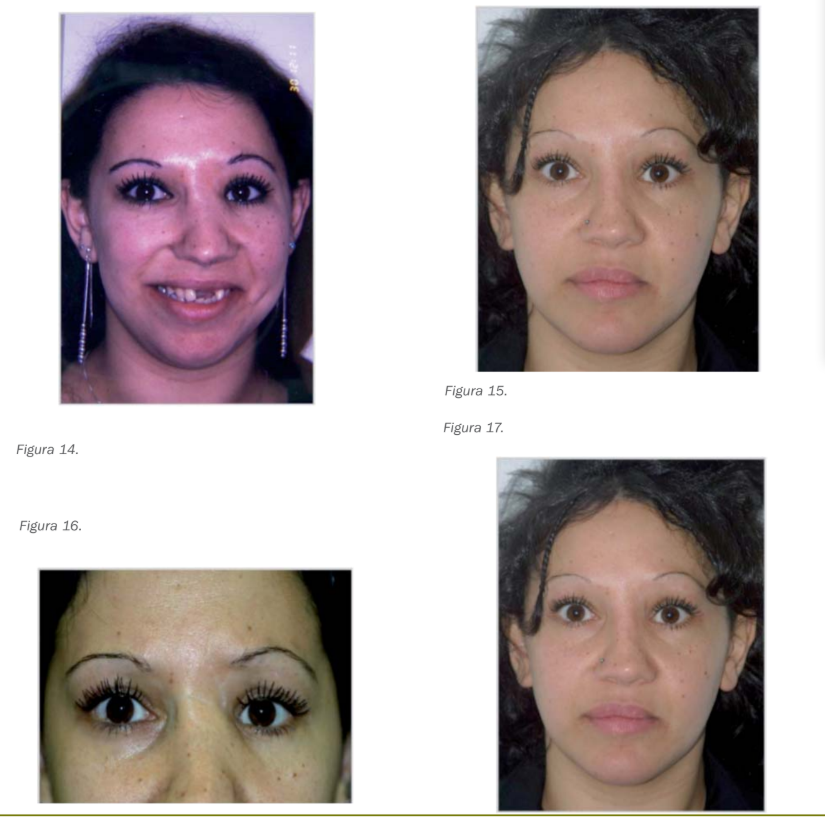
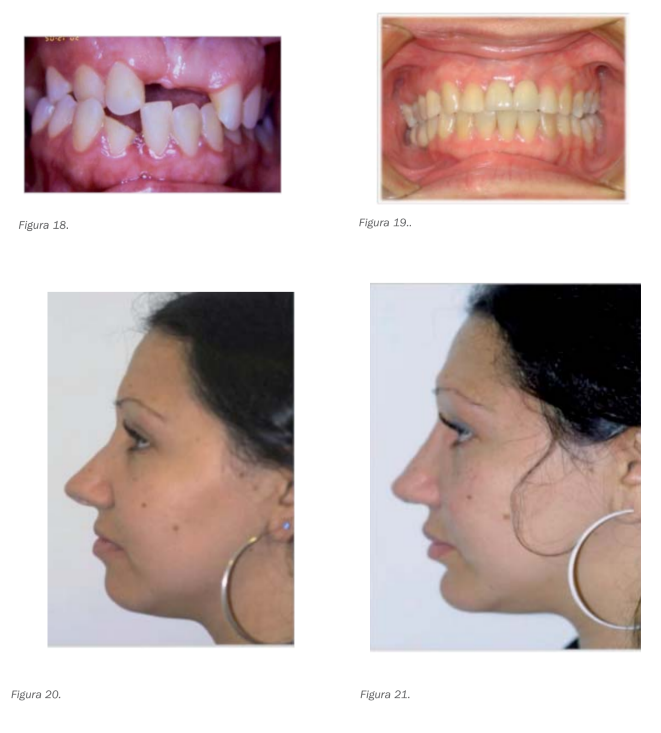
By following these principles, aesthetic and functional improvement is achieved, making these reconstructions one of the most satisfying and rewarding surgeries of the facial skeleton (figures 14-21).
Authors: César Colmenero, Marina Población Subiza, Silvia Rosón Gómez
Bibliography:
- Bussicres M, Tatum. Secondary craniofacial surgery for trauma facial plastic surgery vol 12: 2000, 135-152.
- De Souza M, Oeltjen J, Panthaki Z. Posttraumatic mandibular deformities. The journal of craniofacial surgery 17: 2007, 912-917.
- Clausen L, Galic M, Pagliero F. Posttraumatic enophthalmos. J. Craniofacial surgery 19: 2008, 351-359.
