Chronic Maxillary Sinusitis of Dental Origin: Is External Surgical Approach Mandatory?
Objective: The study evaluated a minimally invasive endoscopic shaver-assisted technique for treatment of chronic maxillary sinusitis of dental origin.
Study Design: A retrospective multicenter chart review was performed at two clinics of all patients who had a diagnosis of chronic maxillary sinusitis of dental origin and were treated using the technique.
Methods: The patients were divided into two main groups: patients with and without chronic oral antral fistula. Data from the patients were collected and analyzed.
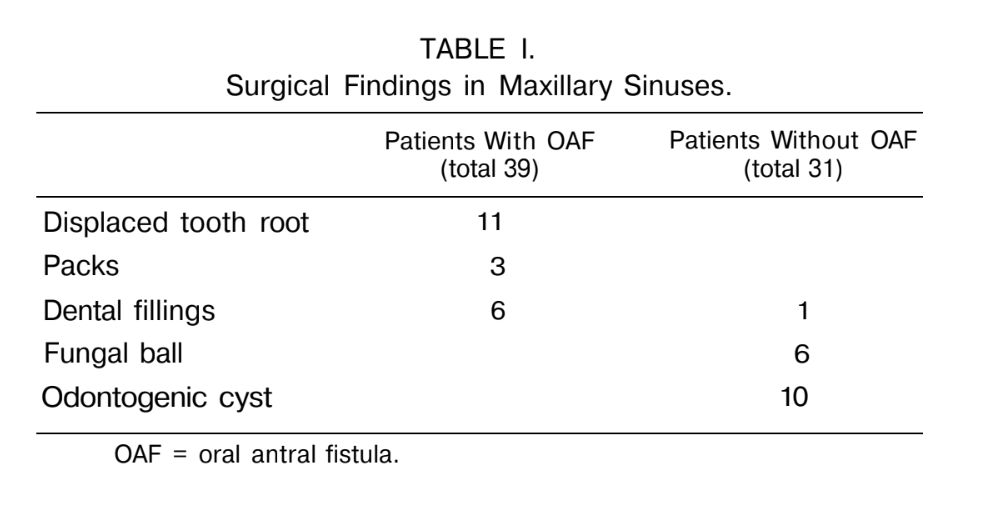
Results: Seventy patients aged 16 to 62 years had surgery using the endoscopic technique. Thirty-nine patients presented with oral antral fistula of different locations, the most common being third molar fistula (26 cases). Foreign bodies were found in 21 sinuses, among them teeth roots (in 11), dental fillings (in 7), and packs (in 3). Fungal ball was found in six sinuses. The surgical technique included retrograde resection of the uncinate process, enlargement of the natural maxillary ostium posteriorly, and removal of the polyps and foreign bodies from the sinus through the middle meatal antrostomy window. Approach through the oral antral fistula facilitated additional access to the alveolar recess. Removal of polyps from the alveolar recess was performed using the microdebrider, which was introduced through the fistula under endoscopic control through the nasoantral window. The fistula was closed in two layers. Good results were obtained in all but four patients in terms up to 3 years. No complications occurred. Overall recovery rate after primary surgery was 94.7%.
Conclusion: Endoscopic approach to chronic maxillary sinusitis of dental origin is a new, reliable method associated with less morbidity and lower incidence of complications.
Introduction
Chronic maxillary sinusitis of dental origin (CMSDO) is a common disease, but its prevalence has often been underestimated. There were studies reporting that chronic inflammation in the maxillary had dental origin in 14% to 24% of cases. Chronic maxillary sinusitis of dental origin may be caused by the following: chronic oral antral fistula (OAF), foreign bodies (dental fillings, teeth roots, parts of broken instruments, or packing materials) pushed through the root canal or OAF into the sinus, periapical granulomas or small inflammatory cysts of the molars and bicuspids, or large odontogenic cysts occupying total or subtotal space of the maxillary sinus.
Despite development of new, effective modalities in medical and surgical therapy of chronic sinusitis and markedly improved endoscopic visualization for sinus surgery since the early 1980s, results of CMSDO treatment have not always been satisfactory. External approach and extensive exploration of the diseased sinus are widely employed in treatment of CMSDO, although these methods are traumatic and carry a risk of postoperative com- plications, such as trigeminal neuralgia. Need for revision because of persistent inflammation and recurrent fistula even after that extensive surgery is approximately 9% to 15%, and in chronic OAF the success rate drops sometimes to 60% to 70% depending on the technique. The current study was aimed at evaluation of efficacy of a less invasive endoscopic approach in the treatment of CMSDO.
Patients and methods
Patients
Charts from all patients diagnosed with CMSDO in whom endoscopic sinus surgery (ESS) had been used were collected from the two medical centers (Presidential Medical Center in Moscow and Novosibirsk State Medical Academy) and analyzed. Between January 1997 and June 2000, endoscopic surgery of the maxillary sinus was performed in 70 patients diagnosed with CMSDO (age range, 16 — 62 y). A similar surgical technique was being used in the two centers during that period time.
Apart from routine methods of rhinological and dental examination, x-rays of the diseased teeth (pantomography) and sinuses, computed tomography (CT) scan of paranasal sinuses in a coronal plane, and nasal endoscopy were used for precise diagnosis of location and extent of disease. Thirty-nine patients from the present series presented with chronic OAF of different locations, the most common being third molar fistula (26 cases); 7 of all study patients had previously had Caldwell-Luc operation. The surgery was usually performed with the patient under general anesthesia. Local anesthesia was used only for cases of maxillary sinus foreign bodies without OAF.
Surgical Technique
The technique of ESS started with careful medial traction of the middle turbinate and retrograde resection of the posteroinferior part of the uncinate process using back-biting forceps. As usual, multiple small polyps were found in the infundibulum as a result of chronic inflammation. Under control of a rigid 30°, 4.0 mm endoscope, the polyps were removed and the uncinate cut edges trimmed with a microdebrider (Hummer-2, Stryker Endoscopy, Santa Clara, СA) with a 3.5-mm straight aggressive cutter blade to the extent that the natural maxillary sinus ostium was identified. Ethmoidal bulla, usually containing polyps, was removed in all cases.
Transection of the posterior fontanel in a horizontal plane was performed using a sickle knife, and the natural ostium was enlarged posteriorly while removing the cut edges with the microdebrider. To prevent postoperative circular stenosis, we always tried to preserve the anterior half of the ostium edge and to leave it untouched. In cases of concomitant purulent inflammation or polyposis in the ethmoid, opening of the diseased anterior and, if necessary, posterior cells was performed.
Endoscopic endonasal approach using 30° and 70° endoscopes allows for perfect visualization of the posteroinferior and upper walls of the sinus, as well as its zygomatic recess. Thus, removal of pathological content and polyps from the posterior, lateral, and upper parts of the antrum using 80° curved double-spoon Binner forceps and/or the microdebrider with 20° and 40° curved aggressive cutting blades can be easily performed. However, there is no need for meticulous stripping of as much mucosa as possible. Only true polyps and cysts have to be removed. Swollen mucous membrane, even in the case of CMSDO, has a strong tendency to healing after restoration of ventilation and drainage of the diseased sinus.
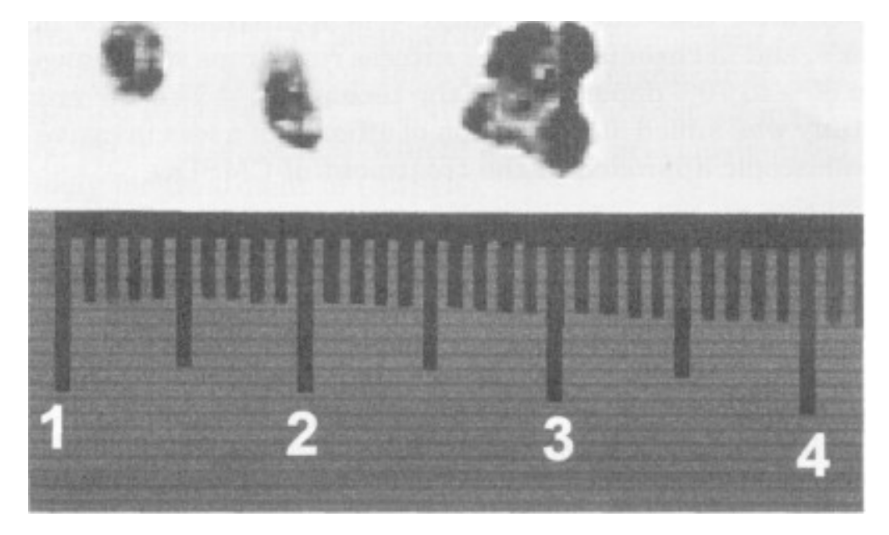
Foreign bodies and fungal balls were removed with a curved suction tip through the enlarged maxillary ostium (Fig. 1). To address the alveolar recess, additional puncture through the fossa canina was performed in some patients without OAF in 1997, when this surgical technique was being developed.
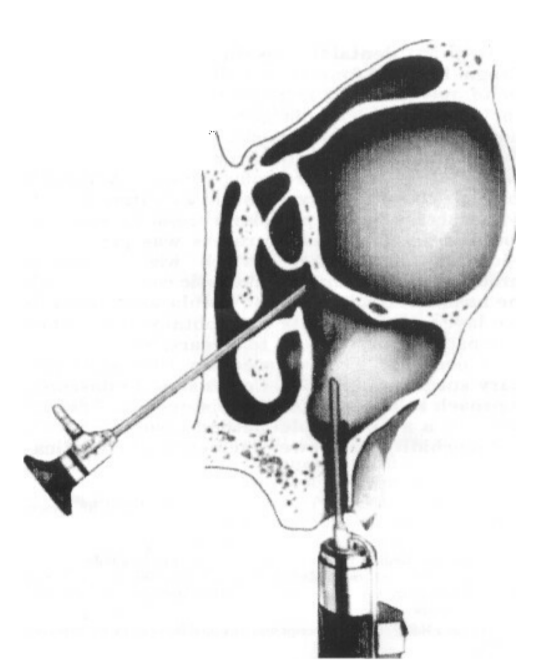
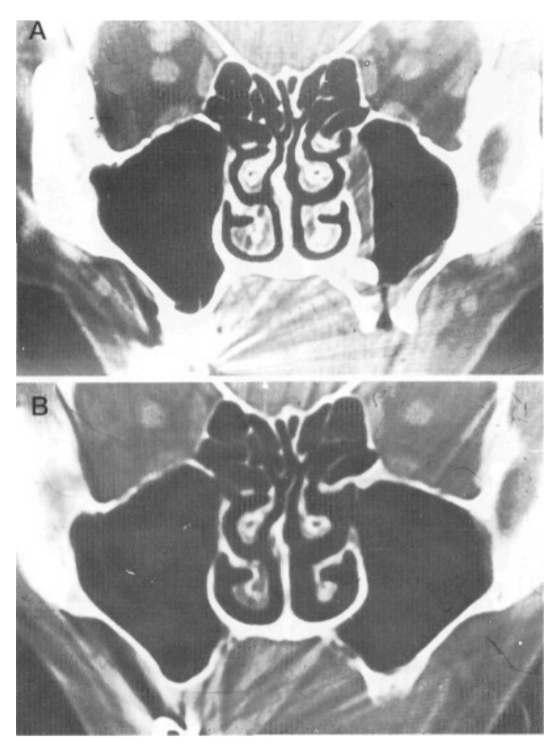
In the presence of OAF, meticulous revision of the alveolar recess and the fistula itself is crucial, and it was performed through the OAF canal. Removal of polyps and granulations from the alveolar recess was carried out by means of the straight, 3.5 mm aggressive microdebrider blade introduced through the fistula. Manipulations of the blade inside the maxillary sinus cavity were visually controlled through the supraturbinate window using a 30° endoscope (Fig. 2). In the same way, we scraped the epithelial layer of the fistulous tract, preparing the latter for plastic closure.
The fistula was closed in two layers. In all cases of OAF, we did not sacrifice soft tissues of the OAF canal but used them for plastic closure. Circular incision around the orifice of the fistula enabled creation of two small de-epithelialized flaps. Inversion and suturing of these flaps provided the first layer of closure. A typical mucoperiosteal advancement flap from the vestibular surface of the alveolar process constituted the second layer in 34 patients. A palatal rotating flap was used in the other five patients; all of them had had previous external surgery and severe deformity of the mucobuccal fold.
Results
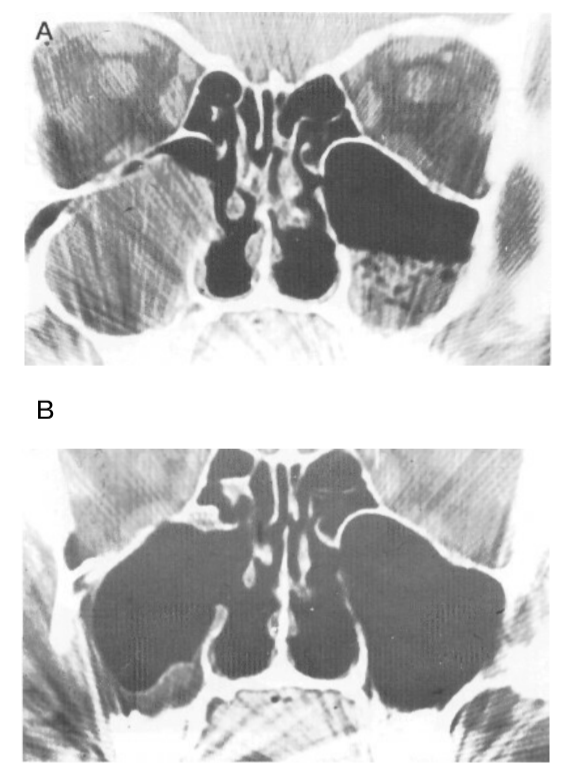
At the time of surgery, foreign bodies were found in 21 sinuses, among them teeth roots (in 11), dental fillings (in 7), and packs (in 3). The latter were of iatrogenic origin, and they had been lost in the sinus by dentists during their attempts to pack the fistula after tooth extraction. All these foreign bodies, including packs, were extracted from the sinuses through the endonasal approach. Large fungal balls were removed from 6 sinuses and odontogenic cysts from 10 (Table I). In all cases but one, a minimally invasive endoscopic approach was sufficient and allowed for complete removal of pathological material from the diseased sinus. Wide opening through the anterior wall and complete removal of the antral mucosa were used in only one case of large ossified odontogenic cyst, which had partially destroyed bony walls. Even in this particular case, instead of creating an infraturbinal window, an endoscopic approach through the middle meatus was used to address the stenotic natural maxillary ostium (Fig. 3).
The combined approach using an endoscopic shaver-assisted technique allowed for minimal trauma to the diseased sinus and provided a smooth postoperative period and faster healing. Cheek edema and nasal obstruction were less severe and regressed much faster than after the Caldwell-Luc procedure, which we had used for treatment of CMSDO previously. No case of postoperative trigeminal neuralgia occurred.
We considered distant results as "good" if the patient was free of symptoms such as nasal discharge and facial pain or headache and if the fistula healed completely. In terms of follow-up from 1 to 3 years, good distant results (Fig. 4) were obtained in all but four patients. Thus, the overall success rate after primary intervention was 94.3%. Oral antral fistula recurred in three patents; in two of them we performed surgery after previous Caldwell-Luc surgery. In one of the first patients from the current series, who had no OAF, recurrence of chronic maxillary sinusitis occurred because of stenosis of the sinus ostium. He had middle meatal antrostomy revision and no further recurrence. Two patients with recurrent OAF underwent second attempts of the fistula closure, which were also successful. One patient refused further therapy and was lost to follow-up. Thus, the recurrence rate for OAF after the first attempt was 7.7% (3 of 39 cases), and there was no recurrent fistula after the second attempt.
Discussion
Chronic maxillary sinusitis of dental origin and chronic OAF have often been considered rare entities, but it seems they are not uncommon, particularly in Russia and the former Union of Soviet Socialist Republics. Quite high prevalence of this disease has been confirmed by the current study. We were able to collect 70 cases (39 cases of OAF among them) from two departments during 3.5 years, and those were only the cases in which an endoscopic surgical technique was used.
That CMSDO, especially associated with OAF, requires an external approach and extensive exploration of the diseased sinus, apart from closure of the OAF itself, is a general opinion of otorhinolaryngological and maxillofacial surgeons. Typically, classic Caldwell-Luc surgery with removal of the innocent anterior wall and all sinus mucosa and creation of an infraturbinate window is used. Disadvantages of this approach have been discussed many times elsewhere in the relevant literature. An alternative approach could be curettage of the antrum through the existing OAF, but the fistula must be sufficiently enlarged to facilitate adequate exposure. The latter technique does not allow an approach to the maxillary ostium and the key area of the ostiomeatal complex.
Today, indications for ESS are not limited by chronic sinusitis and nasal polyposis. Surprisingly, the list of advanced indications for ESS does not include CMSDO. Few studies have dealt with an endoscopic approach to this disease. This stimulated us to attempt an endoscopic shaver-assisted technique for solution of this challenging problem.
Obviously, an endoscopic approach presents a less traumatic modality compared with the Caldwell-Luc operation: The anterior bony wall of the sinus can be spared, and infraturbinal antrostomy avoided. Only irreversibly diseased mucosa has to be removed under endoscopic control. In experienced hands, ESS allows for precise manipulations in any part of the maxillary sinus but not in its anteromedial part and the alveolar recess. The latter area can be easily approached with the microdebrider through OAF. This minimally invasive technique is not associated with a serious risk of postoperative trigeminal neuralgia. The rate of recurrence of the OAF is not higher than that reported in literature and is less than that after radical external approach which we had previously used widely for treatment of CMSDO.
An endonasal approach is justified by the need for revision (and widening) of the natural maxillary ostium, which cannot be addressed in any other way. In 25 cases from the current series, a blocked maxillary ostium and anatomical abnormalities (concha bullosa, deviated uncinate process, large ethmoidal bulla) were revealed. We think that restoration of the ostium patency and the natural sinus clearance mechanism decreases bacterial contamination of the sinus and facilitates faster healing of the OAF.
Indications for removal of foreign bodies from the maxillary sinus need further discussion. Clearly, teeth roots, parts of instruments, and packs must be removed immediately while they sustain purulent inflammation and initiate necrosis of the mucosa and underlying bone, as well as polyp formation. Dental fillings, even if they do not result in any complaints, should also be removed because they cause fungal ball growth. In this case, however, immediate actions are not necessary. Under normal conditions, the mucociliary clearance mechanism is strong enough to transport even big particles of the filling to the maxillary ostium and then to the nasal cavity. The small size of the ostium prevents evacuation of the fillings, and this justifies a delicate endoscopic intervention in the middle meatus, which solves the problem. Our experience shows that dental fillings encapsulated under the sinus mucosa need no removal because they cause neither fungal growth nor clinical symptoms.
Conclusion
An endoscopic shaver-assisted approach to CMSDO is a reliable, minimally invasive method associated with less morbidity and lower incidence of complications. In the current series, the recovery rate was 94.3% after primary surgery and there were no recurrences after the second attempt. These results are better than after the Caldwell-Luc technique that we used previously.
Authors: Andrey S. Lopatin, Svyatoslav P. Sysolyatin, Pavel G. Sysolyatin, Mikhail N. Melnikov
Bibliography:
- Uvarov VM. Odontogennye haimority [Odontogenic Maxillary Sinusitis]. Leningrad: Medgiz, 1962:34-39.
- Shargorodsky AG. Vospalitelnye zabolevania chelustno-litsevoy oblasti i shei [Inflammatory Diseases of the Maxillofacial Region and the Neck]. Moscow: Medgiz, 1985: 15-24.
- Gluckman JL. Oroantral fistula. In: Donald PJ, Gluckman JL, Rice DH, eds. The Sinuses. New York: Raven, 1995: 599-606.
- Yih WY, Merril R, Howerton D. Secondary closure of oroantral and oronasal fistulas. J Oral Maxillofac Surg 1988;46: 357-364.
- Setliff RC. Minimally invasive sinus surgery: the rationale and the technique. Otolaryngol Clin North Am 1996;29: 115-129.
- Loscalzo LJ. Management of dental disease and oral antral fistula. In: Blitzer A, Lawson W, Friedman WH, eds. Surgery of the Paranasal Sinuses. Philadelphia: WB Saunders, 1991:289-296.
- Romo T, Goldberg J. Functional endoscopic sinus surgery to manage chronic oral antral fistula. Operative Techn Otolaryngol Head Neck Surg 1991;2:247-256.
- Balabantsev AG, Bogdanov W, Gontcharuk VP, Krasnikov VA, Logosyuk AV. Differentsirovanniy podhod k lecheniyu lits s odontogennym haimoritom [Different approaches to the treatment of patients with odontogenic maxillary sinusitis]. Zh Ushnyh Nosovyh Gorlovyh Hvoryb (Kiev) 2000; 2:121-124.
- Stammberger H. Functional Endoscopic Sinus Surgery: The Messerklinger Technique. Philadelphia: BC Decker, 1991: 398-427.
- Stammberger H. Functional Endoscopic Sinus Surgery: The Messerklinger Technique. Philadelphia: BC Decker, 1991: 247.
