Surgical complications related to temporomandibular joint arthroscopy: a prospective analysis of 39 single-portal versus 43 double-portal procedures
Abstract
Temporomandibular joint (TMJ) arthroscopy is a minimally invasive surgical procedure proposed for diverse TMJ intra-articular disorders. A prospective study was designed with the aim of investigating intraoperative and postoperative surgical complications for single and double-portal TMJ arthroscopy. All interventions were performed by one surgeon with the same surgical protocol. A total of 55 patients were enrolled, resulting in 82 TMJ arthroscopies (28 unilateral and 27 bilateral). A total of 39 single portal (47.57%) and 43 double-portal (52.43%) arthroscopies were performed. No severe and irreversible complications were observed. Most complications were resolved after 4 weeks. Double-portal was associated with more complications (n = 23) compared with single-portal TMJ arthroscopy (n = 14), with a statistically significant difference found between single and double-portal TMJ arthroscopy in two intraoperative complications: intra-articular bleeding (P = 0.044) and oedema of the preauricular area (P = 0.042). This study confirms the safety of TMJ arthroscopy for single and double-portal procedures, with the authors suggesting a multicentre study, in an effort to minimize any possible bias.
Temporomandibular joint(TMJ) arthroscopy is a minimally invasive surgical procedure proposed for diverse TMJ intra-articular disorders. This technique is considered safe by most authors, however, intraoperative and postoperative complications have been reported. The comparisons of surgical complications in TMJ arthroscopy between different authors can be associated with bias due to the use of different protocols. In Europe, most TMJ surgeons perform arthroscopy under gener al anaesthesia, whereas in Asia others have performed the same intervention under local anaesthesia. The majority of surgeons use a 30◦ arthroscope, while others prefer to use a 0◦ arthroscope, changing the intra-articular perspective. The arthroscope diameter used is also different amongst TMJ surgeons, usually varying from 1.9 mm to 2.3 mm. The posterior and anterior entry point, the lavage solution, pressure and the supplementation substance also vary between authors. The armamentarium is also different worldwide, with some surgeons having designed specific instruments for TMJ arthroscopy. The authors suggest that these changes in TMJ arthroscopic approach can contribute to different intraoperative and postoperative complications. The most common surgical complications are: (1) bleeding; (2) oedema of the pre-auricular area; (3) pharyngeal oedema; (4) instrument fracture; (5) laceration of the external auditory canal; (6) lesion of the facial nerve; (7) lesion of the trigeminal nerve; (8) alteration of visualaccuracy. This prospective study aims to compare TMJ arthroscopic complications using single versus double-portal procedure in a strict surgical protocol.
Material and Methods
Study Design
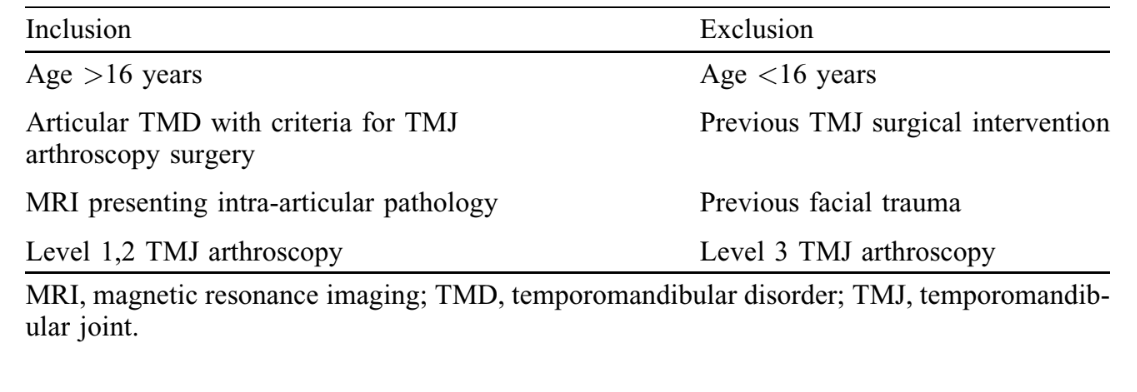
This prospective study was conducted at Instituto Português da Face, Lisboa, Portugal from 1 January 2017 to 31 December 2019. The study protocol was approved by the ethics committee of Centro Academico de Medicina de Lisboa. All the enrolled participants gave their informed, clarified and free term of consent in writing and in accordance with current legislation. Participant data was scrubbed of any personal identifying parameters, and all participants received a random ID number. Criteria for study inclusion and exclusion are represented in Table 1. Bilateral arthroscopies were analysed as isolated unilateral arthroscopies. No distinction was made between left and right sides.
Data Collection
A database was created to register patient intraoperative and postoperative complications: (1) extra-articular bleeding posterior puncture; (2) extra-articular bleeding anterior puncture; (3) intra-articular bleeding; (4) oedema of the preauricular area; (5) pharyngeal oedema; (6) instrument fracture; (7) laceration of the external auditory canal; (8) VII frontal branch nerve damage; (9) VII zygomatic branch nerve damage; (10) auriculotemporal nerve damage; (11) inferior alveolar nerve damage; (12) alteration of visual accuracy. The outcomes were registered in a dichotomic model of ‘yes’ or ‘no’. A detailed outcomes assessment is described in Supplementary Table S1.
Surgical Protocol
Before surgery, the patients rinsed their mouths three times with a chlorohexidine mouthwash solution, for 2 min. All patients underwent the same surgical protocol under general anaesthesia with nasoendotracheal intubation. Before draping, surgical skin preparation was made with betadine solution. The external auditory canal was packed with half of a fat gauze.
Single portal
A 1.9-mm arthroscope including a video system, with a 2.8-mm outer protective cannula (Stryker, San Jose, CA, USA), was used for level 1 TMJ arthroscopy. Additional equipment included a surgical scalpel (#11 blade), infusion tube, three- way pipe, 21-G needle and Ringer solution as part of the armamentarium. For single-portal TMJ arthroscopy, the authors used the classic puncture with the entry point 10 mm anterior and 2 mm below the Holmlund–Hellsing (H-H) line to insert a 21-G needle with 5 cc of Ringer Lactate to perform superior joint space distension. The arthroscope was inserted in a forward and upward direction (15º and 45º, respectively) into the superior joint space. An anterior puncture with a 21-G needle was performed 30 mm anterior and 7 mm below the H-H line to wash the joint with 250–300 ml Ringer solution with manual pressure, controlled by the assistant surgeon. All the aforementioned steps were performed with the patient in middle mouth opening and medium protrusion. After washing the joint with 250-300 ml Ringer solution, and a rigorous inspection of the superior joint space, 1.8–2.0 cc of hyaluronic acid (Synvisc) was injected into the joint using the 2.8-mm outer protective cannula irrigation pipe. After removal of the needle and arthroscope, surgical glue was used to close the skin. If unusual bleeding was noticed in the surgical entry points, a haemostatic suture was performed with nylon 4/0.
Double portal
For level 2 TMJ arthroscopy, the arthroscope was positioned in a more anterior position to the eminence slope. The anterior puncture was substituted by a 2.8-mm outer protective cannula with a shape trocar. If this puncture did not succeed after three attempts, the second point of entry was changed to 40 mm anterior and 12 mm below the H-H. When the surgical triangulation was performed, different techniques were used: intrasynovial medication, tissue coblation with ReFlex Ultra 45 Plasma Wand system or myotomy.
Antibiotics, non-steroidal anti-inflammatory drugs and corticoids were routinely prescribed after surgery and the patient was discharged on the same day. Patients were instructed to follow a soft diet for 3 days after surgery and physiotherapy exercise sessions started 5 days after intervention.
Statistical Analysis
All statistical analyses were performed using IBM SPSS Statistics for Windows, version 26 (IBM Corp, Armonk, NY, USA). A comparison of outcomes between single-portal (L1) and double-portal (L2) TMJ arthroscopies was performed for all 12 studied surgical complications. A parametric test, namely a paired Student’s t-test between L1 and L2 was determined for each variable.
Results
A total of 55 patients were enrolled; 45 (81.8%) were female and 10 (18.2%) were male, and their mean age was 39.40 ± 16.78 years (range 16–79 years). Of the 55 patients, 27 underwent bilateral arthroscopy and 28 patients had unilateral arthroscopy. A total of 39 (47.57%) single-portal and 43 (52.43%) double-ortal arthroscopies were performed. Patient characteristics are summarized in Supplementary Table S2.
In single-portal arthroscopy, the authors only observed complications for: (1) pre-auricular oedema (23.1%); (2) auriculo-temporal nerve damage (7.7%); and (3) extra-articular bleeding posterior puncture (5.1%). Oedema and bleeding were not severe in any of the cases, not being considered a real complication as the patient suffered no disturbance from it. The auriculotemporal nerve damage with paraesthesia of the ear territory was not permanent and returned to normal nerve function in 4 weeks.
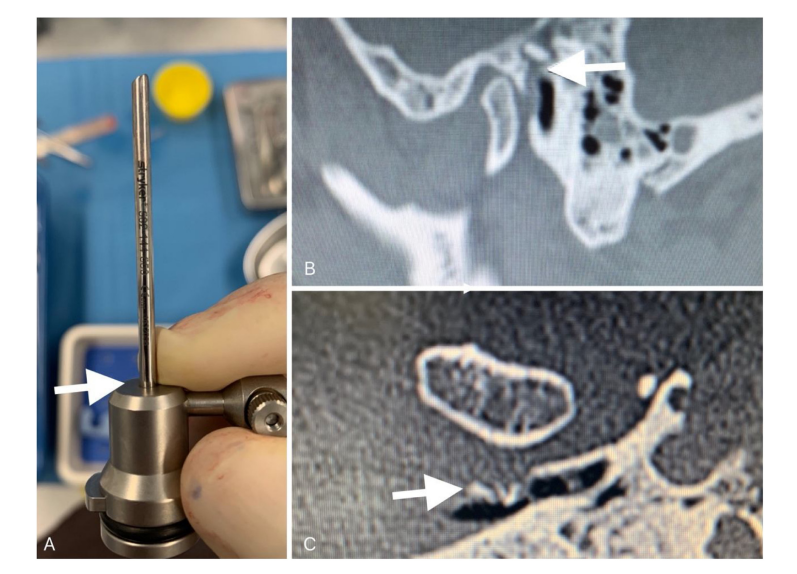
Regarding double-portal arthroscopy, the authors observed complications for: (1) intra-articular bleeding (9.3%); (2) auriculotemporal nerve damage (9.3%); (3) instrument fracture (7%); (4) VII frontal branch nerve damage (7%); (5) oedema of the preauricular area (7%); (6) extra-articular bleeding posterior puncture (7%); (7) laceration of the external auditory canal (4.7%); and (8) VII zygomatic branch nerve damage (2.3%) (Table 2). All these complications were observed during or immediately after the surgery, exception for the two cases with laceration of the external auditory canal. The intra-articular bleeding was not severe in any of the cases, and was controlled by increasing the flow speed inside the joint as a first measure, and if unsuccessful, coblation was performed as a second measure. The small Fogarty catheter to control intra-articular bleeding was not necessary in any of the cases. All cases with auriculotemporal nerve damage (n = 4) recovered after 4 weeks, except for one patient that needed 8 weeks to achieve a full recovery. Instrument fracture was observed in three interventions, and repeatedly on the connection of the 2.8-mm outer protective cannula from Stryker (reference 502144550), as observed in Fig. 1A. No surgical implications were associated, as the authors had a second instrument set and the broken instrument was replaced. The authors did not use excessive force or caused any damage that would justify the occurrence. A notification was sent to the manufacturer. The frontal branch nerve damage was observed in three patients, and was confirmed 1 day postoperatively. This paralysis was not permanent and normal function returned in 8 weeks. The zygomatic branch nerve damage was only observed in one patient with normal function achieved 8 weeks postoperative. As observed in the single portal technique, oedema of the preauricular area and the bleeding was not severe in any of the cases, and it was not considered as a real complication. The most delicate complications were the laceration of the external auditory canal noticed in two patients after TMJ arthroscopy level 2 (Fig. 1B, C). The management of those patients was made in collaboration with the otorhinolaryngologist using antibiotics in the main, without the need of surgical intervention.
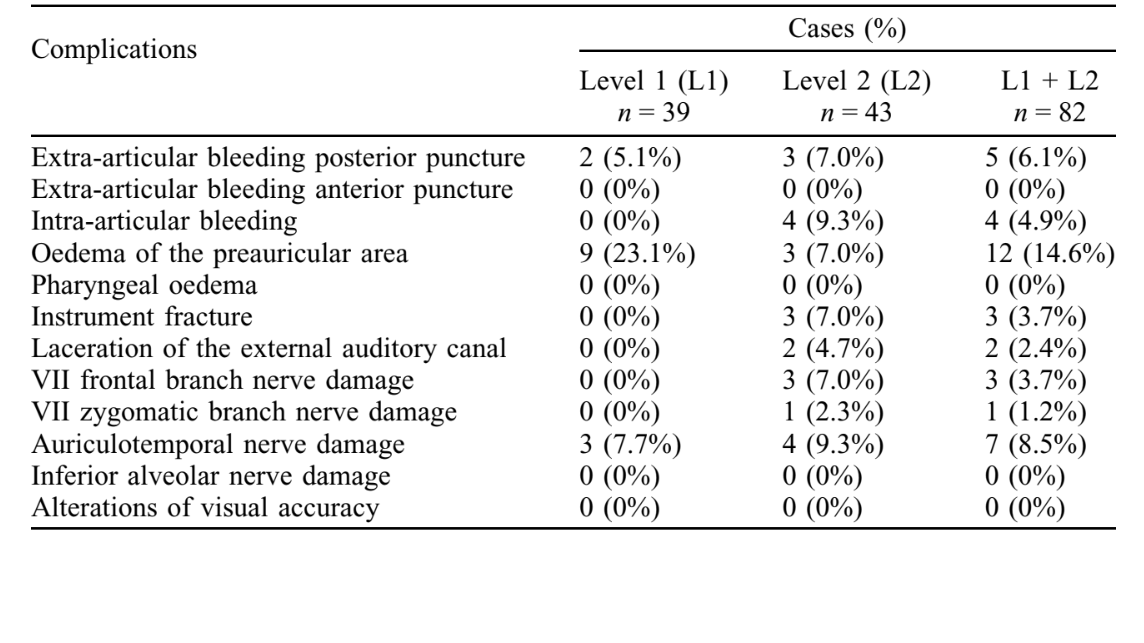
Regarding the statistical analysis, a paired Student’s t-test between arthroscopies level 1 (L1) and level 2 (L2) revealed a statistically significant difference (P < 0.05) for two intraoperative complications: intra-articular bleeding (P = 0.044) and oedema of the preauricular area (P = 0.042). These results can be seen highlighted in bold in Supplementary Table S3.
Discussion
TMJ arthroscopy is considered safe, but intraoperative and postoperative complications have been reported. Most studies do not specify in detail the surgical armamentarium and protocol and to our knowledge none has compared complications of single versus double portals in TMJ arthroscopy. In Table 3, available results are compared. In single- portal arthroscopy, the most common complication found was oedema in the preauricular area (n = 9, 23.1%). In the authors’ experience, multiple attempts to achieve a functional outflow and/or a non-effective outflow are the main reasons for a major solution extravasation. Previous studies have associated the sensory damage to be more likely related to fluid extravasation phenomena rather than from direct injury during penetration with the cannula. A non-effective outflow can, apart from preauricular oedema, result in a more severe complication: pharapharyngeal oedema which can lead to airway obstruction. However, in 2015, Karim et al. reported a case of parapharyngeal swelling after TMJ arthroscopy not associated with inefficient outflow. They managed the case by delaying extubation for 1 h. Special care must be taken by surgeon and anaesthesiologist, detecting possible parapharyngeal swelling, even with effective outflow. Using a double-portal, the authors observed less oedema in the pre-auricular area (n = 3, 7%) when compared with single-portal results. One possible explanation is due to the functional working cannula being more effective in the outflow, comparatively with the 21-G needle anterior puncture used in the single-portal technique. This could provide insight into understanding the data from Tsuyama et al. where the auriculotemporal nerve damage was the second most common complication in single-portal TMJ arthroscopy (n = 3, 7.7%). González et al., in 2006, reported a 0.15% rate for auriculotemporal nerve damage, but Weinberg et al. found auriculotemporal nerve injury in 29.6% of the cases. As reported in other studies, all nerve injury cases recovered completely in 6 weeks, and thus, the most appropriate medical term when describing this nerve damage should be secondary neuropraxia.
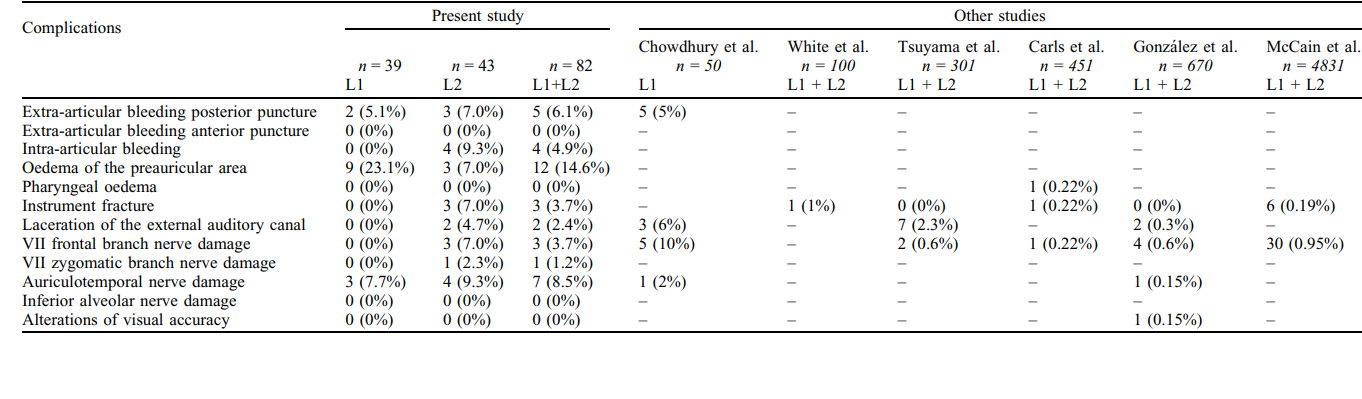
Extra-articular bleeding in the posterior puncture was not frequent (n = 2, 5.1%). Most studies did not evaluate this outcome. The puncture bleeding is most likely to be associated with temporal vessel injury. An anatomic study in 31 cadavers reported the traditional puncture site was located often adjacent to the temporal vessels, always anterior, however, the vessels were not damaged. McCain et al. reported that the temporal vessels can be avoided by the use of two techniques: (1) palpation of the vessels in order to avoid them; (2) using a lateral puncturing technique, in which the most posterior puncture into the superior joint space is 10 mm anterior to the midportion of the tragus on the tragus–canthus line. The authors used this technique; however, in two cases, temporal bleeding was noticed. For double puncture, no difference was seen, with three cases presenting bleeding in the posterior puncture, with all of them being easily controlled with gauze compression. In total (n = 82), the authors observed a posterior puncture bleeding rate of 6.1%, with bleeding not being severe in any of the cases. In single puncture, no intra-articular bleeding was observed, whereas in double puncture, a 9.3% (n = 4) intra-articular bleeding was noticed. This complication can lead to intraoperative difficulty in visualization and a consequent interruption of the procedure, as well as postoperative hemarthrosis with possible association with future trismus or intra-articular adhesions. Our data is similar to that of González et al., where it was reported that 8.5% of the bleeding was in the superior space, although not specifying whether it was for single or double punctures. The laceration of the external auditory canal was, to the authors, the most severe complication, causing discomfort and anxiety to the patient. González et al. reported a total of 0.3% incidence with single and double-portal procedures. Comparing our single and double-portal data, we reported a 2.4% incidence. However, no cases of laceration were observed in the single portal (0%), with all registered cases occurring with the double-portal technique (4.7%). Tsuyama et al. reported that 2.3% of cases had laceration of the external auditory canal in 309 double puncture arthroscopic surgeries.
The authors observed instrument fracture only for double-portal arthroscopy (n = 3, 7%), with McCain et al. reporting six broken instruments in a study of 4831 joint including single and double arthroscopies (0.12%), while others did not report instrument failure. The equipment failure was reported to the manufacturer. Interestingly, other manufactures have designed a new protective cannula, with a more robust connection, perhaps indicating that this was a known issue, even though it was not reported in the literature. The instrument fracture did not lead to any clinical consequence.
The VII frontal branch nerve damage was observed only in double-puncture patients (n = 3, 7%). In the study by González et al., a report of 0.6% (n = 4) was observed but included single and double puncture. In our study, for both single and double puncture, we report 3.7% (n = 3). Tsuyama et al. reported a 1.7% incidence, and in a study of 451 arthroscopies, Carls et al., reported that only one patient had frontal nerve damage. The VII zygomatic branch nerve damage was observed only for double puncture and in one patient (2.3%). This low percentage of cases seems to be in line with what was described by Tsuyama et al., that reported 0.6% incidence (n = 2) out of 301 cases.
This study has several limitations. First, the main surgeon was responsible for both the intervention and for registering the complications, which may have had an influence on the results. A second limitation was the limited sample size. As we know, surgeon experience plays an important role in the rate of surgical complications, and as such these results could be different in other centres.
This prospective study reinforced the safety of the TMJ arthroscopy for both single and double-portal techniques if the correct arthroscopic armamentarium is selected, and the puncture point landmarks are respected, therefore avoiding potentially dangerous zones.
Authors: D. F. Ângelo, R. A. D. Araújo, D. Sanz
References:
- González-García R, Rodríguez-Campo FJ, Escorial-Hernández V, Muñoz-Guerra MF, Sastre-Pérez J, Naval-Gías L, Gil-Díez Usandizaga JL. Complications of temporomandibular joint arthroscopy: a retrospective analytic study of 670 arthroscopic procedures. J Oral Maxillofac Surg 2006;64 (11):1587–91. http://dx.doi.org/10.1016/j.joms.2005.12.058.
- Fernández Sanromán J, Costas López A, Fernández Ferro M, de Sánchez AL, Stavaru B, Arenaz Bua J. Complications of temporomandibular joint arthroscopy using two-portal coblation technologies: a prospective study of 475 procedures. J Craniomaxillofac Surg 2016;44(9):1221–5. http://dx.doi.org/ 10.1016/j.jcms.2016.06.027.
- McCain JP, de la Rua H. Foreign body retrieval: a complication of TMJ arthroscopy. Report of a case. J Oral Maxillofac Surg 1989;47(11):1221–5.discussion 1228-1229.
- McCain JP. Complications of TMJ arthroscopy. J Oral Maxillofac Surg 1988;46 (4):256.
- Patel S, Jerjes W, Upile T, Hopper C. TMJ arthroscopy: rare neurological complications associated with breach of the skull base. Br J Oral Maxillofac Surg 2010;48(4):e18–20. http://dx.doi.org/10.1016/j.bjoms.2009.12.012.
- Carls FR, Engelke W, Locher MC, Sailer HF. Complications following arthroscopy of the temporomandibular joint: analysis covering a 10-year period (451 arthroscopies). J Craniomaxillofac Surg 1996;24(1):12–5. http:// dx.doi.org/10.1016/s1010-5182(96)80071-0.
- Sato FRL, Tavares RC. Abducens palsy after temporomandibular joint arthroscopy: a rare complication. Oral Maxillofac Surg 2016;20 (3):327–30. http://dx.doi.org/10.1007/s10006-016-0559-0.
- Kassam K, Cheong R, Cascarini L. Parapharangeal edema: an uncommon complication of TMJ arthroscopy. Clin Case Rep 2015;3(6):496–8. http://dx.doi.org/10.1002/ ccr3.189.
- Indresano AT. Arthroscopic surgery of the temporomandibular joint: report of 64 patients with long-term follow-up. J Oral Maxillofac Surg 1989;47(5):439–41. http://dx.doi.org/10.1016/0278-2391(89)90274-7.
- Holmlund A, Lund B, Weiner CK. Discectomy without replacement for the treatment of painful reciprocal clicking or catching and chronic closed lock of the temporomandibular joint: a clinical follow-up audit. Br J Oral Maxillofac Surg 2013;51(8):10–3. http://dx. doi.org/10.1016/j.bjoms.2012.12.006.
- Tsuyama M, Kondoh T, Seto K, Fukuda J. Complications of temporomandibular joint arthroscopy: a retrospective analysis of 301 lysis and lavage procedures performed using the triangulation technique. J Oral Maxillofac Surg 2000;58(5):500–5. http://dx.doi. org/10.1016/s0278-2391(00)90010-7.discussion 505-506.
- McCain JP, Sanders B, Koslin MG, Quinn JD, Peters PB, Indresano AT. Temporomandibular joint arthroscopy: a 6-year multicenter retrospective study of 4,831 joints. J Oral Maxillofac Surg 1992;50(9):926–30. http:// dx.doi.org/10.1016/0278-2391(92)90047-4.
- Boulox GF. Complications of Temporomandibular Joint Surgery. Cham: Springer International Publishing; 2017.
- Chowdhury SKR, Saxena V, Rajkumar K, Shadamarshan RA. Complications of Diagnostic TMJ Arthroscopy: an Institutional Study. J Maxillofac Oral Surg 2019;18(4):531–5. http://dx.doi.org/10.1007/ s12663-019-01202-3.
- White RD. Retrospective analysis of 100 consecutive surgical arthroscopies of the temporomandibular joint. J Oral Maxillofac Surg 1989;47(10):1014–21. http://dx.doi. org/10.1016/0278-2391(89)90171-7.
- Weinberg S, Kryshtalskyj B. Analysis of facial and trigeminal nerve function after arthroscopic surgery of the temporomandibular joint. J Oral Maxillofac Surg 1996;5 (1):40–3. http://dx.doi.org/10.1016/s0278-2391(96)90301-8. discussion 43-44.
- Westesson PL, Eriksson L, Liedberg J. The risk of damage to facial nerve, superficial temporal vessels, disk, and articular surfaces during arthroscopic examination of the temporomandibular joint. Oral Surg Oral Med Oral Pathol 1986;62(2):124–7. http:// dx.doi.org/10.1016/0030-4220(86)90028-9.
