The role of curvilinear distraction system in pediatric obstructive sleep apnea: A case report
Abstract
Objective: The authors present a case of obstructive sleep apnea associated with severe mandibular micrognathia treated by mandibular bone distraction with curvilinear system planned under computer assistance.
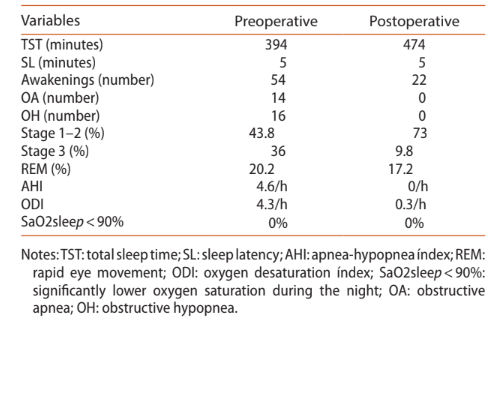
Clinical Presentation: A 15-year-old child with limited compliance to continuous positive airway therapy was referred to the authors’ department. Observation revealed severe mandibular micrognathia as the major cause for obstructive sleep apnea syndrome. The first polysomnography study revealed 14 obstructive apneas, 16 obstructive hypopneas, and 4.6/h apnea-hypopnea index.
Conclusion: Mandibular distraction osteogenesis can be a successful technique in alleviating upper airway obstruction secondary to micrognathia, while also improving the patient’s appearance. Surgical planning under computer assistance is a useful tool to predict bone movements, and curvilinear distraction could be considered valuable in mandibular distraction.
Introduction
Obstructive sleep apnea syndrome (OSAS) in children is defined as a disorder of breathing during sleep, characterized by prolonged partial upper airway obstruction and/or intermittent complete obstruction (obstructive apnea) that disrupts ventilation during sleep and fragments sleep patterns. Of the general pediatric population, 1.2–5.7% exhibits OSAS. Adenotonsillar hypertrophy is the most common etiology of OSAS in children. Other causes are obesity, facial or skeletal malformations, and neuromuscular, respiratory, or metabolic diseases. Children born with congenital craniofacial abnormalities such as Pierre Robin sequence or Treacher Collins syndrome are faced with complex airway management issues. They often exhibit mandibular micrognathia and glossoptosis, resulting in airway obstruction. The sequelae of OSAS include neuropsychological and cognitive impairment, systemic and pulmonary hypertension, and endothelial dysfunction. Continuous positive airway pressure (CPAP) remains a non-surgical treatment alternative for pediatric OSAS; however, limited compliance to this mode of therapy remains a realistic limitation in children. Mandibular distraction osteogenesis (MDO) has shown to improve upper airway obstruction and other functional outcomes in selected patients with craniofacial abnormalities. The authors present a case of obstructive sleep apnea associated with severe mandibular micrognathia treated by mandibular bone distraction planned with computer assistance.
Case report
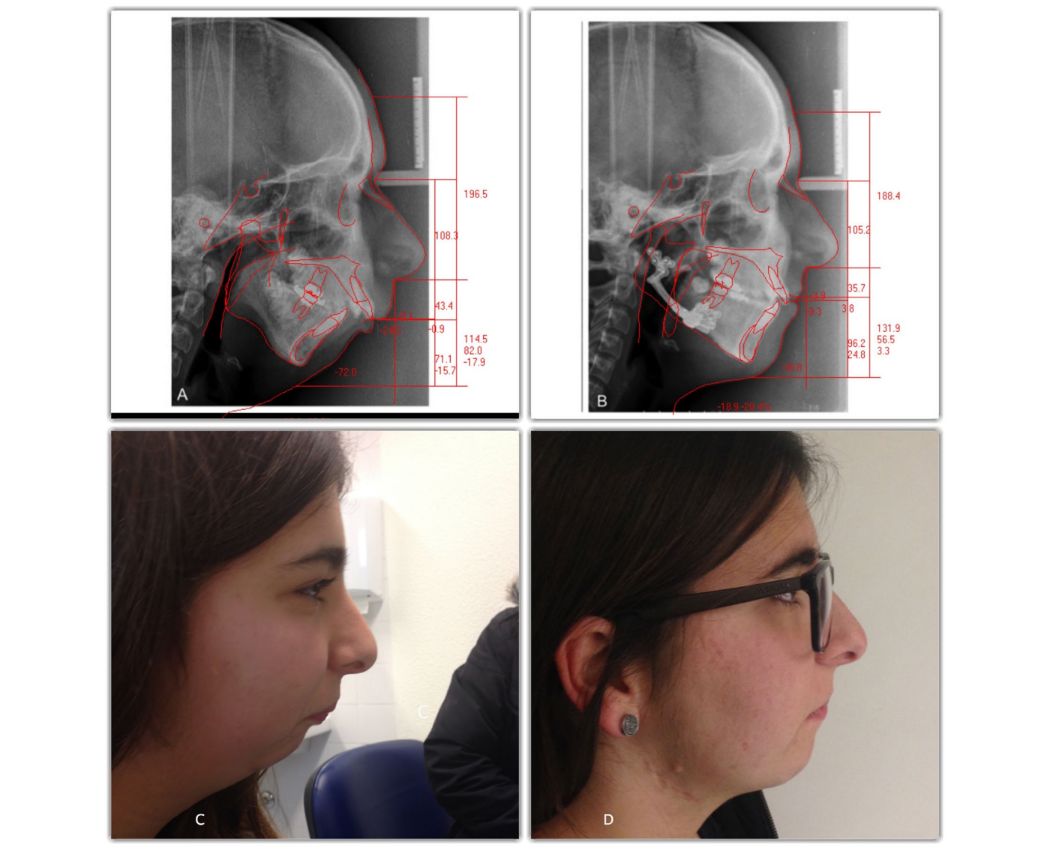
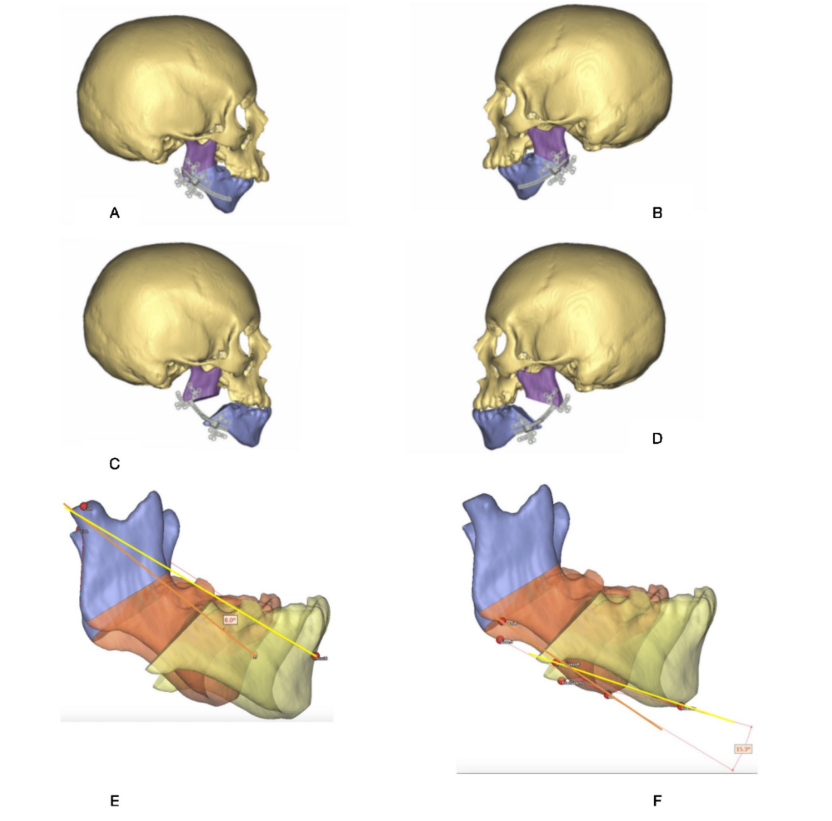
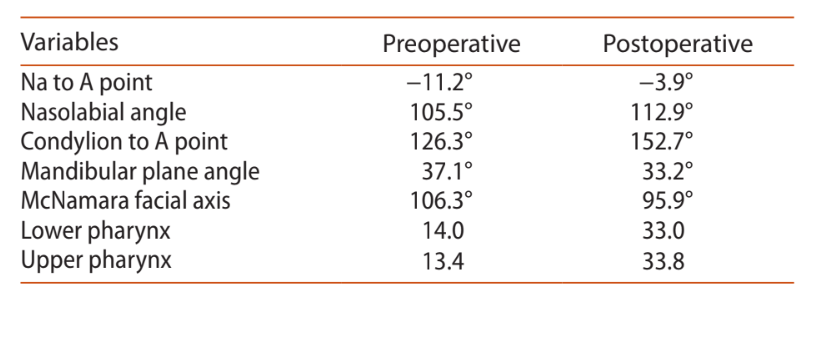
A 15-year-old child was referred to the author’s department for consultation after limited compliance to CPAP therapy and general cognitive complaints. General facial observation revealed a severe mandibular micrognathia as a major cause for OSAS (Figure 1(C)). Polysomnography revealed 14 obstructive apneas, 16 obstructive hypopneas and 4.6/h apnea-hypopnea index (Table 1). The cephalometric tracing (Figure 1(A)) confirmed mandibular micrognathia and a small upper airway (Table 2). To plan the mandibular advancement, a three-dimensional (3D) computerized tomographic (CT) was performed, and 3D virtual planning was executed (Figure 2). Permission was obtained from the patient’s parents.
Management and outcome
The surgical team planned to use an internal Curvilinear Distraction System from DePuySynthes® (DePuy Sythes CMF, West Chester, PA, US) to use two planes simultaneously: horizontal and vertical (Figure 2(E), (F)). Synthes ProPlan CMF® (computer-aided surgical planning service) was used to plan this case. In phase 1, the approximate site of the osteotomy (Figure 2(A), (B)) was marked. Then the distal segment of the mandible was moved to the desired post-distraction position (Figure 2(C)–(D)).
The authors used an intraoral surgical approach to perform the osteotomy and to fit the distractor as planned. The distractor was fitted to the mandible correctly. Then, a percutaneous activation port was created in the soft tissue through which the extension arm exited. Before performing the osteotomy, the position of the distractor was marked by drilling and inserting the screws through each footplate. Then, the distractor was unscrewed and removed to perform the corticotomy on the buccal side of the mandible, extending into the superior and inferior borders. This allowed stability of the bone segments during reattachment of the distractor. The distractor was reattached by aligning the footplates with the holes made previously, and the osteotomy was completed on the lingual aspect of the mandible, using an osteotome. At the end, the activation instrument was used to engage the activation hex of the extension arm. It was rotated counter clockwise, in the direction marked on the instrument handle to confirm device stability and verify movement of the mandible, and the distractor returned to its original position. The patient began active distraction five days after surgery, 1.0 mm per day (half turn twice a day), to prevent premature consolidation. After 27 days, she started the consolidation period for 10 weeks. In this phase, extension arms were removed. After that period, the surgical team removed the distractor using an extraoral approach. This approach was not planned, but the team was not able to remove the distractor intraorally. The postoperative polysomnography presented with zero apnea and zero apnea-hypopnea index (Table 1). The final result (Figure 1(D)) was satisfactory.
Discussion
Micrognathia is usually a congenital condition characterized by a small and retrusive mandible and has a direct impact on the surrounding soft tissues of the upper airway, restricting airflow. This situation tends to occur with posterior tongue displacement (glossoptosis), which can lead to physical obstruction of the oropharyngeal and hypopharyngeal airways during inspiration and can result in apnea/hypopnea. This condition, characterized by apneic and/or hypopneic episodes during sleep, can be accompanied by severe secondary problems. It is important to mention that where possible, conservative treatment should always be tried first before surgical intervention is considered. However, the esthetic improvement and self-image can be very important, especially for females at 15 years of age. Considering the esthetic improvement, surgical option has great value.
When considering MDO in any infant or child, the risks vs. benefits of surgery must always be considered.
Numerous surgical options have been described for the management of pediatric OSAS, secondary to hypoplastic mandible. MDO is currently an accepted method of treatment for patients requiring reconstruction of hypoplastic mandibles. MDO relieves the airway obstruction by lengthening the mandible. This stretches the tongue attachments to the mandible (genioglossus muscle), which positions the tongue more anteriorly, relieving the glossoptosis. Although MDO is very effective at relieving airway distress secondary to micrognathia, the optimum age for surgery is yet to be determined. When comparing the results of those younger than 2 months, 2–6 months, 6–18 months, and 18 months of age at the time of MDO, there was no significant difference in failure rate. Unfortunately, this patient was referred for consultation at 15 years of age, and the authors believe that surgical intervention should have been performed earlier. Surgical complications such as facial scarring, facial nerve palsy, neurosensory disturbances of the inferior alveolar nerve, occlusal abnormalities such as an anterior open bite, and dental damage can occur from MDO. Planning surgical intervention with 3D software has several advantages and can reduce surgical complications. 3D CT allows precise and spatial orientation of the deformed bone, which can be measured and evaluated in all dimensions. This allows precise surgical planning. This surgical instrument with the Curvilinear Distraction System from DePuySynthes® could be considered valuable in mandibular distraction, taking into consideration the use of reproducible landmarks and regions for the osteotomies on each side of the mandible and the possible identification of bony/dental interferences along the path of movement.
Conclusion
In conclusion, MDO can be a successful technique in alleviating upper airway obstruction secondary to micrognathia, while also improving the patient’s appearance. Surgical planning under computer assistance seems to be a useful tool to predict bone movements, and curvilinear distraction could be considered valuable in mandibular distraction.
Authors: David Serrano Faustino Ângelo, Bruno Rosa, Rogério Santos & Carlos Diogo Matos
References:
- Rosen CL. Obstructive sleep apnea syndrome (OSAS) in children: diagnostic challenges. Sleep. 1996;19:S274–7.
- Li AM, So HK, Au CT, et al. Epidemiology of obstructive sleep apnea syndrome in Chinese children: a two-phase community study. Thorax. 2010;65:991–997.
- Bixler EO, Vgontzas AN, Lin H-M, et al. Sleep disordered breathing in children in a general population sample: prevalence and risk factors. Sleep. 2009;32:731–736.
- Beydon N, Aubertin G. Diagnostic criteria for obstructive sleep apnea syndrome. Arch Pédiatrie Organe Off La Sociéte Fr Pédiatrie [Pediatr Arch French Pediatr Soc]. 2016;23:432–436. French.
- Gozal D, Serpero LD, Sans Capdevila O, et al. Systemic inflammation in non-obese children with obstructive sleep apnea. Sleep Med. 2008;9:254–259.
- Miman MC, Kirazli T, Ozyurek R. Doppler echocardiography in adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol. 2000;54:21–26.
- Atkeson A, Yeh SY, Malhotra A, et al. Endothelial function in obstructive sleep apnea. Prog Cardiovasc Dis. 2009;51:351–362.
- King MS, Xanthopoulos MS, Marcus CL. Improving positive airway pressure adherence in children. Sleep Med Clin. 2014;9:219–234.
- Marcus CL, Beck SE, Traylor J, et al. Randomized, double-blind clinical trial of two different modes of positive airway pressure therapy on adherence and efficacy in children. J Clin Sleep Med. 2012;8(1):37–42, Feb 15.
- Hong P. A clinical narrative review of mandibular distraction osteogenesis in neonates with Pierre Robin sequence. Int J Pediatr Otorhinolaryngol. 2011;75:985– 991.
- Ow ATC, Cheung LK. Meta-analysis of mandibular distraction osteogenesis: clinical applications and functional outcomes. Plast Reconstr Surg. 2008;121:54e– 69e.
- Hong P, McNeil M, Kearns DB, et al. Mandibular distraction osteogenesis in children with Pierre Robin sequence: Impact on health-related quality of life. Int J Pediatr Otorhinolaryngol. 2012;76:1159–1163.
- Kaban B, Seldin E, Kikins R, et al. Clinical application of curvilinear distraction osteogenesis for correction of mandibular deformities. J Oral Maxillofac Surg. 2009;67:996–1008.
- Manikandhan R, Lakshminarayana G, Sneha P, et al. Impact of mandibular distraction osteogenesis on the oropharyngeal airway in adult patients with obstructive sleep apnea secondary to retroglossal airway obstruction. J Maxillofac Oral Surg. 2014;13:92–98.
- Breik O, Tivey D, Umapathysivam K, et al. Mandibular distraction osteogenesis for the management of upper airway obstruction in children with micrognathia: a systematic review. Int J Oral Maxillofac Surg. 2016;45:769–782.
- Kolstad CK, Senders CW, Rubinstein BK, et al. Mandibular distraction osteogenesis: at what age to proceed. Int J Pediatr Otorhinolaryngol. 2011;75:1380–1384.
- Verlinden CRA, van de Vijfeijken SECM, Jansma EP, et al. Complications of mandibular distraction osteogenesis for congenital deformities: a systematic review of the literature and proposal of a new classification for complications. Int J Oral Maxillofac Surg. 2015;44:37–43.
