Patient experience and satisfaction with different temporomandibular joint treatments: A retrospective study
Abstract
This retrospective study aimed to evaluate patient satisfaction with different temporomandibular joint (TMJ) treatments. Patients were included in the study according to the following inclusion criteria: 1) arthrogenous and/or myogenous temporomandibular disorders (TMD); 2) Dimitroulis classification category between 1-4; 3) conservative treatment without any improvement at least for 3 months; 4) indication for one of the following TMD treatments: injection of botulinum toxin; arthrocentesis; arthroscopy, and open surgery without alloplastic material; and 5) age ≥16 years. An independent satisfaction questionnaire with 11 queries was applied via phone call to all patients, which included 6 questions using a 10-point Likert scale and 5 yes-or-no questions. The principal outcome was the overall satisfaction with the clinical result of the treatment, and the secondary outcomes were specific satisfaction with the following: 1) pain reduction; 2) range of mouth opening; 3) chewing ability; 4) post-operative recovery; 5) the fulfillment of expectations; 6) treatment choice; 7) treatment recommendation to a friend; and 8) the need for another intervention. Anxiety and depression were also included as variables. Data were analyzed using descriptive statistics, non-parametric Kruskal-Wallis and Spearman rank correlation coefficient tests. A total of 120 patients (mean age 41.20 ± 17.78 years) were enrolled, comprising 109 women (90%) and 11 men (10%). The overall clinical satisfaction of all patients was 8.24 ± 2.23 (mean ± SD), and 97 patients (80.8%) stated that they would repeat the treatment. Patients submitted to TMJ arthrocentesis and arthroscopy had higher overall clinical satisfaction (9.09 ± 0.971 and 9.03 ± 1.13, p = 0.021) followed by open surgery (8.38 ± 1.84). The authors observed three statistically significant correlations: 1) overall clinical satisfaction and patient expectations (r = 0.803; p < 0.0001); 2) overall clinical satisfaction and post-treatment pain (r = -0.299; p = 0.003); and (3) the presence of depression and the need for further TMJ treatment (r = 0.186; p = 0.043). Within the limitations of the study it seems that patient expectations should be addressed ad initium, and the presence of a diagnosis of depression with concomitant TMD must alert the clinical team and patient for the possible need of additional treatment.
Introduction
Temporomandibular disorders (TMD) are a group of arthrogenous and/or myogenous problems associated with morphological and functional deformities (Murphy et al., 2013; Yap et al., 2021). TMD is the most common cause of orofacial pain of nondental origin (Soni, 2019). The estimated prevalence among adults ranges between 5% and 15% (Liu and Steinkeler, 2013; Ahmad and Schiffman, 2016; Li and Leung, 2021; Yap et al., 2021), yet TMD-related symptoms may be present in up to 50% of adults (Li and Leung, 2021).
The main goal of TMD treatment is pain reduction and function improvement, and increasing patients’ quality of life (Liu and Steinkeler, 2013; Al-Moraissi et al., 2021). Historically, treatment strategies for arthrogenous TMD have involved a sequential approach (Al-Moraissi et al., 2020). In a first attempt, the literature highlights the role of reversible strategies. Second, minimally invasive, non-reversible procedures should be attempted: (1) intra-articular injection (IAI) of different drugs (hyaluronic acid, platelet-rich plasma); (2) temporomandibular joint (TMJ) arthrocentesis; or
(3) TMJ arthroscopy (alone or in combination with IAI) (Dimitroulis, 2018; Al-Moraissi et al., 2020).
Among the available reversible approaches, botulinum toxin (BTX) injections have demonstrated interesting therapeutic effects in the treatment of myofascial pain (Schwartz and Freund, 2002; Song et al., 2007; Awan et al., 2019). Some studies report that BTX injections into the masticatory muscles are a considerable treatment method to address TMD pain, reducing its intensity (Sipahi Calis et al., 2019; Machado et al., 2020) and improving quality of life (Villa et al., 2019). In addition, it is a simple procedure with a good risk-to-benefit ratio (Sunil Dutt et al., 2015; Sipahi Calis et al., 2019). Minimally invasive techniques such as TMJ arthrocentesis and arthroscopy are now among the most widely used techniques in the treatment of internal derangements. Open joint surgeries are recommended for more severe arthrogenous TMD (Krug et al., 2004; Doucet and Morrison, 2011, Ângelo et al., 2022).
The majority of the studies evaluate clinical outcomes to define surgical success: TMJ pain in VAS scale and maximum mouth opening (MMO, mm) (Eriksson and Westesson, 2001; Bas et al., 2019; Insel et al., 2020). However, few studies evaluate patient perspective on clinical outcomes. The non-evaluation of patient perspective may be associated with a distortion between clinical and patient interpretation of the results. Therefore patient- centered studies may present an advantage in evaluating the effectiveness of each treatment taking into account the patient's perspective. Thus, the authors formulated the following hypothe- ses: 1) minimally invasive treatments are associated with higher clinical satisfaction compared to open surgery? 2) botulinum toxin injections in myogenous TMD are associated with high satisfaction? 3) mental disorders (eg, depression, anxiety) have a relation to patients' clinical satisfaction?
The main purpose of this study was to evaluate patients’ clinical satisfaction with different TMJ treatments: BTX injections, TMJ arthrocentesis, arthroscopy, and open joint surgery without alloplastic material.
Materials and methods
Study design
A cross-sectional retrospective study was performed that included patients treated for TMD from April of 2017 to April of 2021. The study was approved by the institutional ethics commit- tee. All enrolled patients gave their informed consent in writing, following current legislation.
The inclusion criteria were as follows: 1) arthrogenous and/or myogenous TMD; 2) Dimitroulis classification category between 1-4; 3) conservative treatment without any improvement at least for 3 months; 4) indication for one of the following TMD treatments: injection of botulinum toxin; TMJ arthrocentesis; TMJ arthroscopy; TMJ open surgery without alloplastic material; and 5) age ≥16 years. An age over 16 years was considered as an inclusion criterion for the following reasons: 1) it is accepted in the literature that 99% of facial bone growth is complete (Weaver et al., 1998); and 2) a young adult is able to understand the application of the questionnaire and to answer it autonomously (Hargreaves et al., 2018). Exclusion criteria were as follows: 1) previous TMJ surgical intervention; 2) impaired cognitive capacity; 3) age <16 years; and 4) current pregnancy or breastfeeding.
Prior to treatment, all patients were examined and treated by the same TMJ surgeon (D.A.). TMJ pain was assessed with a visual analog scale (VAS; 0e10, with 0 being no pain and 10 having maximum insupportable pain) and MMO (mm) using a certified ruler between the incisor teeth. Arthralgia was diagnosed through positive history for both of the following criteria: 1) pain in the jaw, temple, ear, or in front of the ear and 2) pain modified with jaw movement, function, or parafunction. Positive examination for arthralgia was reported if pain location in TMJ area was observed and pain was experienced on palpation of the lateral pole; or pain on maximum unassisted or assisted mouth opening, right or left lateral movements, or protrusive movements. The final arthrogenous diagnosis was confirmed with magnetic resonance imaging (MRI). Myogenous disease, including myalgia, was diagnosed according to a clinical history positive for the following: 1) in the past 30 days, pain in the jaw, temple, in front of the ear, or in the ear, with clinical confirmation of pain location in the temporalis or masseter muscle; and 2) pain modified with jaw movement, function or parafunction, and a positive clinical evaluation for palpation pressure (5 s/1 kg pressure) in masseter and/or temporalis muscles, as defined in DC/TMD (Schiffman et al., 2014). Myalgia was graded in accordingly with pain intensity in each muscle: 0 = no pain/pressure only; 1 = mild pain; 2 = moderate pain; 3 = severe pain (Goiato et al., 2017).
Postoperative pain was assessed at each patient's last follow-up visit before the application of the questionnaire.
The decision regarding which treatment to apply was based on the Dimitroulis classification (Dimitroulis, 2013), as follows: Category 1: patients without joint noises, no history of locking or disc dislocation, with TMJ pain associated with myofascial pain. These patients were treated with botulinum toxin injections. Category 2: patients with intermittent pain, joint clicking, diagnosis of DDwR or indication of joint inflammation with normal condyles. These patients were treated with TMJ arthrocentesis. Category 3: patients with long-standing closed lock (>2 months), painful recurrent dislocation of the TMJ with diagnosis of DDwoR, absence of clicks, TMJ internal derangement or synovial chondromatosis. These cases were treated with TMJ arthroscopy. Category 4: patients with radiological signs of changes in condylar morphology such as osteophytes, small subcondral cysts and with loss or thinning of cartilage layer, severe displaced and deformed articular discs, including disc perforation. When the disc was salvageable, the patients were treated with discopexy; if the disc was unsalvageable, discectomy was performed (Ângelo et al., 2022).
Treatment protocol
BTX injections
One session of BTX injections was used for patients with muscle tenderness without an arthrogenous disorder. For muscular tenderness grade 1-2 and 3, 155 U and 195 U of incobotulinum toxin A, respectively, was injected equally distributed in the right and left temporal and masseter muscles. The authors used Xeomin® (Merz).
TMJ arthrocentesis
Local anesthesia was done with lidocaine and epinephrine (1:80.000), blocking the auriculotemporal nerve. The first puncture point was performed with a careful palpation of the lateral rim of the glenoid fossa. A 5-cc syringe was prepared with 3-cc of Ringer's lactate and 1.8-cc of lidocaine with epinephrine 1:80.000. A 21-G needle coupled with a 5-cc syringe was gently inserted into the joint, and when the tip of the needle made contact with the posterior slope of the eminence of the upper joint compartment, the surgeon verticalized the needle to access the upper compartment. The first validation was performed with a successful pumping action with inflow and outflow of fluids in the joint space. If the surgeon was not able to achieve a positive pumping, the arthrocentesis was aborted. After this step, the second portal was easily completed with a 21-G needle, promoting a successful outflow fluid. After completing an effective circuit, a joint washing was performed with 60-80 ml of Ringer's lactate solution. Supplemental injection was performed with hyaluronic acid (1.5 ml) or hyaluronic acid and platelet-rich plasma (PRP) in patients with osteoarthritis (OA).
TMJ arthroscopy
TMJ arthroscopy was performed with a 1.9-mm arthroscope including a video system (Stryker, San Jose, CA, USA), with a 2.8-mm outer protective cannula. Additional equipment has been previously described (Ângelo et al., 2021). Briefly, for TMJ arthroscopy level 1, the authors used the classic puncture with an entry point 10 mm anterior and 2 mm below the HolmlundeHellsing (HeH) line. The arthroscope was inserted into the superior joint space. A second puncture with a 21-G needle was performed 30 mm anterior and 7 mm below the HeH line to wash the joint with 250e300 ml Ringer's solution. After washing the joint, 1.5-2-cc of hyaluronic acid was injected into it. For arthroscopy level 2, the second puncture was substituted by a 2.8-mm outer protective cannula with a sharp trocar until the joint was reached. The 2.8-mm cannula was used for an instrumental passage way for: 1) a ReFlex Ultra 45 Plasma Wand system for intra-articular coblation and/or 2) intra-synovial medication through a 22-G long spinal needle. Antibiotic protocol (amoxicillin/clavulanic-acid or clarithromycin) and non-steroidal anti-inflammatory drugs (ibuprofen) were routinely prescribed following surgery. No bandage was applied or special care performed after the surgery. No hair washing restrictions were recommended. All patients were hospitalized for less than 24 h.
TMJ open surgery
A classic preauricular incision or a root of helix inter tragus notch incision (RHITNI) was used in most cases, as previously described (Ângelo, 2020). Discectomy or discopexy with mitek mini-anchors was performed, depending on whether the TMJ disc was salvageable or not. Condilectomy or condiloplasty was also performed for condyle hyperplasia or severe osteoarthritic changes, respectively. No bandage or special care was performed after the surgery. No hair washing restrictions were recommended. All patients were hospitalized for 24 h.
All patients were instructed to follow a soft diet for 3 days after intervention and to have 5 physiotherapy and 3 speech therapy sessions starting 1-3 days after the intervention.
Design and application of patient satisfaction questionnaire
Patients who met criteria to be included in the study were contacted via phone call, and all patients were asked if they wished to participate in the questionnaire, and had the freedom of choice to decline participation. The survey consisted of 11 questions, 6 using a 10-point Likert scale (0 = very dissatisfied and 10 = very satisfied) (questions 1-6) and 5 yes-or-no questions (questions 7-11) (Table S1). Three of the questions had the possibility to explain the given answer and thus to allow an open response (Table S1).
The questions were written in Portuguese in the most neutral form to reduce response bias, specifically wording bias. Binary response questions (yes-or-no) were included, with those that offered a range of options, to require the patient to think about the answer. Open-ended questions were also included, because this allows the patient the opportunity to reflect on possible dissatisfaction factors that should be actively investigated by the researcher.
The questionnaire was developed based on surgical surveys evaluating patient satisfaction related with clinical outcomes (Mahomed et al., 2011) (Posnick and Wallace, 2008). The principal outcome was the overall satisfaction with the clinical result of the treatment (question 4) and the secondary outcomes were specific satisfaction with the following: pain reduction (question 1); range of mouth opening (question 2); chewing ability (question 3); postoperative recovery (question 5); the fulfillment of expectations (question 6); treatment choice (question 7); treatment recommendation to a friend (question 8); and the need for another intervention (question 11). Questions 1 to 5 were based on the work of Mahomed et al. (2011) and Posnick and Wallace (2008). Questions 1 to 3 and 5 were included as patient-related outcome measures of treatment satisfaction. Question 6, regarding the fulfilment of expectations, was based on the idea that satisfaction may actually represent the fulfilment of an expectation rather than only satisfaction with the outcome (Graham et al., 2015; Graham, 2016). The patients were also asked if they would undergo the same treatment again (question 7) and if they would recommend it to friends (question 8), since these are indirect measures of satisfaction (Espeland et al., 2008; Rauck et al., 2020). Finally, patients were also asked whether, in the present or recent past, they had had a diagnosis, performed by a psychiatrist or family physician, of anxiety (question 9) or depression (question 10) (Table S1). The authors decided to include these questions, given the burden that anxiety and depression represent in TMD and also based on the work of Rauck et al. (2020), who hypothesized that patients with worse preoperative mental and physical health would be less satisfied. Patients were also asked about the need for further TMJ treatment (question 11), since we believe that the need for further TMJ treatment may reduce the level of overall clinical satisfaction. The level of education was also assessed, since it may have an impact on the patient perception of post-intervention outcome (Chow et al., 2009; Kahlenberg et al., 2018; Rauck et al., 2020).
Statistical analysis
Variables are expressed as the mean (± standard deviation [SD]). The normality analysis was performed with the Shapiro—Wilk test. A normality assumption was not fulfilled. For comparison between groups, the Kruskal—Wallis test with multiple comparison with Dunn correction was performed. Correlations between the study
variables were performed with the Spearman rank correlation coefficient. p-values < 0.05 were considered statistically significant. These data analyses were obtained using SPSS (v26) and GraphPad Prism (v9).
Results
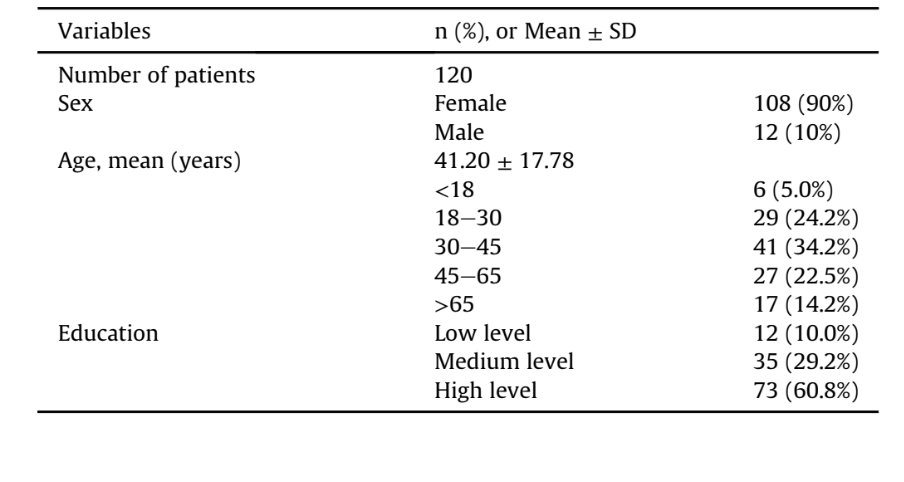
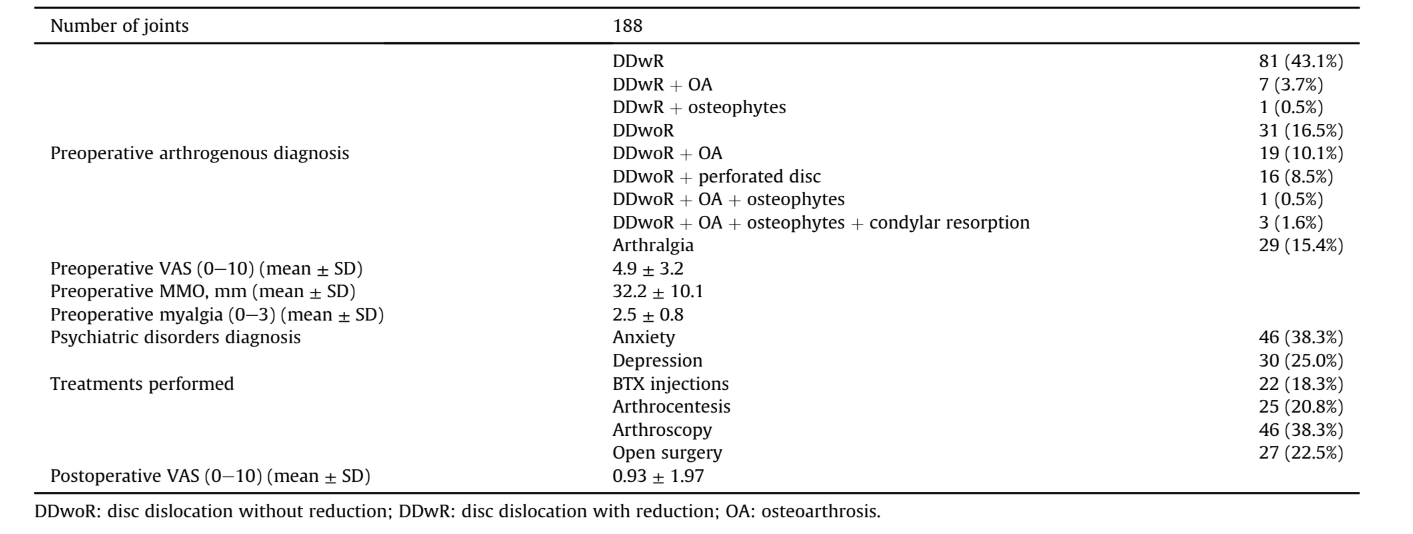
A total of 158 patients were assessed for study eligibility. Of these, 30 could not be reached with the contact details provided, 6 refused to participate, and 2 died. Thus, 120 patients (108 female and 12 male) were included in the present study (Table 1). The mean age was 41.20 ± 17.78 years (ranging from 14 to 89 years) (Table 1). Regarding education, 12 patients (10.0%) had completed primary and/or middle school; 35 patients (29.2%) had completed secondary school, and 73 patients (60.8%) had a college degree (Bachelor's, Master's, and/or doctorate degrees) (Table 1). A total of 188 joints were diagnosed with arthrogenous TMD (Table 2). The mean preoperative pain was 4.9 ± 3.2 (mean ± SD), MMO was 32.2 ± 10.1 mm (mean ± SD), and degree of myalgia was 2.5 ± 0.8 (mean ± SD) (Table 2). Considering the TMJ treatments, 22 patients undergone BTX injections, 25 TMJ arthrocentesis, 46 TMJ arthroscopy, and 27 TMJ open surgery (Table 2). Through questions 9 and 10, it was verified that almost two-thirds of the group (63.3%) reported a clinical history of anxiety (38.3%, 46 patients) or depression (25.0%, 30 patients) (Table 2).
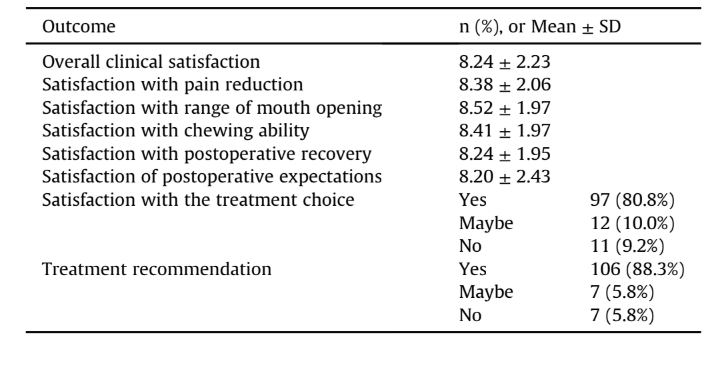
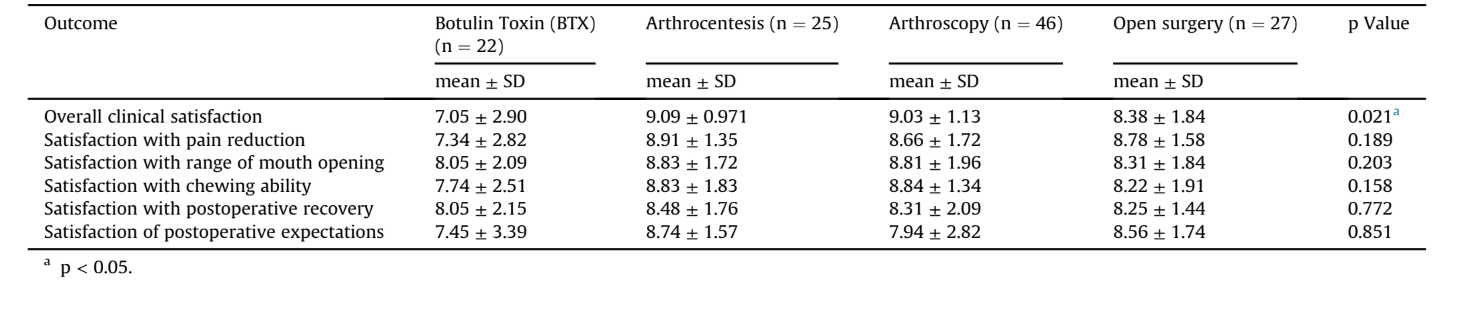
The overall clinical satisfaction (question 4) of all four treatments included in this study was 8.24 ± 2.23. A total of 97 patients (80.8%) reported that they would repeat the procedure performed (question 7) (Table 3). Furthermore, 106 patients (88.3%) would recommend the treatment (question 8) (Table 3). Pain reduction, range of mouth opening, and chewing ability evaluation were included in the study as patient-related outcome measures of treatment satisfaction. The mean subjective in pain reduction (question 1), range of mouth opening (question 2), and chewing ability (question 3) was 8.38 ± 2.06, 8.52 ± 1.97, and 8.41 ± 1.97, respectively. Patients also rated their satisfaction regarding expectations in 8.20 ± 2.43 (question 6). The mean satisfaction with postoperative recovery (question 5) was 8.24 ± 1.95 (Table 3).
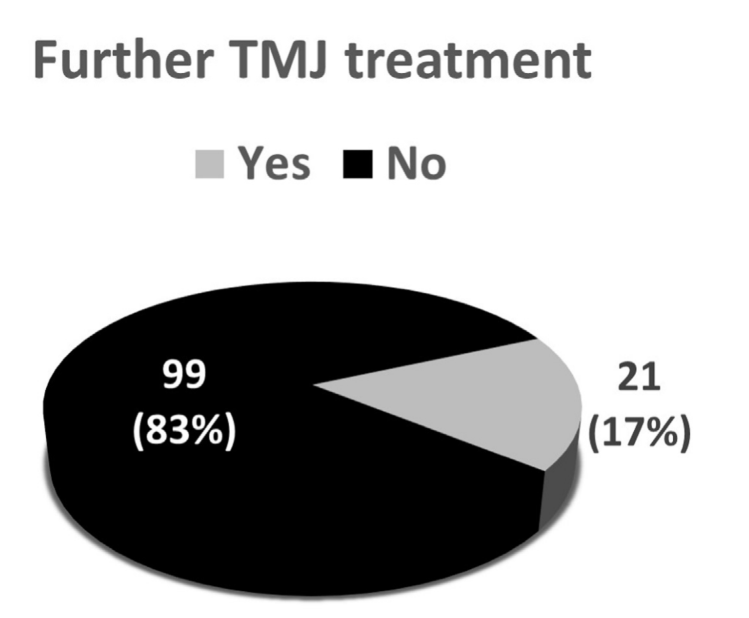
Of the study patients, 99 (83%) required no other TMJ intervention, and the remaining 21 patients (17%) needed further TMJ treatment: either BTX injections (4 patients); arthrocentesis (13 patients); and open surgery (4 patients) (Fig. 1).
The degree of satisfaction with each surgical intervention was analyzed. The overall clinical satisfaction was higher with TMJ arthrocentesis, 9.09 ± 0.971, followed by TMJ arthroscopy,
9.03 ± 1.13, and TMJ open surgery, 8.38 ± 1.84 (Table 4). The treatment that provided less overall clinical satisfaction to patients was the BTX injections (7.05 ± 2.90) comparative to arthrocentesis (p = 0.029) and arthroscopy (p = 0.013) (Table 4, p = 0.021). Regarding the analysis of other satisfaction parameters, no statistically significant differences were found.
To assess possible controlling factors in satisfaction, the authors used the Spearman rank correlation coefficient (Table 5). It was shown that the overall clinical satisfaction (question 4) and the fulfillment of expectations (question 6) were strongly correlated (r = 0.803) and statistically significant (p < 0.0001). This is relevant, because it demonstrates that the individual's satisfaction rating is dependent on the degree of the patient expectations (Graham, 2016). Preoperative pain, DDwoR or DDwR diagnosis, Dimitroulis classification, anxiety and depression diagnosis were not found to be correlated with the degree of satisfaction (Table 5). Instead, the degree of satisfaction was inversely correlated with the post-operative pain recorded in consultation (r = —0.299, p = 0.003).
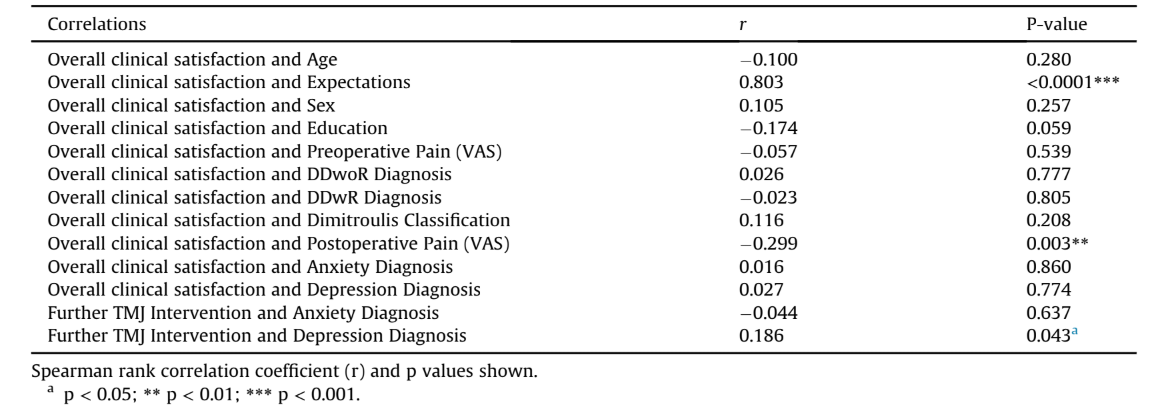
The presence of depression in the present or recent past (question 10) and the need for further TMJ treatment (question 11) were positively correlated (r = 0.186, p = 0.043).
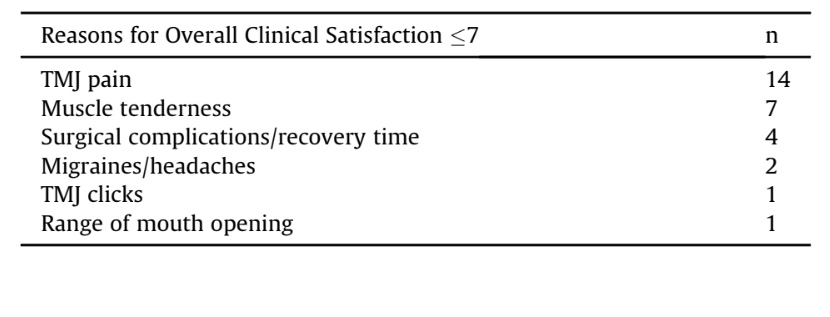
The main reasons given by patients for having a lower-than-average level of satisfaction (satisfaction ≤7) included TMJ pain (n = 14), muscle tenderness (n = 7), surgical complications (speech difficulty, tinnitus)/recovery time (n = 4), migraines/headaches (n = 2), TMJ clicks (n = 1), and range of mouth opening (n = 1) (Table 6).
Discussion
In this work, all of the studied treatments achieved a high level of overall patient satisfaction. According to the literature, it is reported that 80% of patients with signs and symptoms of TMD have some form of internal derangement (Paesani et al., 1992). In this study, 188 joints had a preoperative diagnosis of an arthrogenous TMD, mainly disc displacement with or without reduction, 47 of them with other additional TMD diagnoses (OA, osteophytes, condylar resorption, perforated disc). Because of the different types of TMD typology, it was decided to sub-classify all patients according to the Dimitroulis classification (Dimitroulis, 2013). The Dimitroulis classification includes a broader spectrum of TMD subtypes and also suggests suitable medical treatment for each grade (Dimitroulis, 2013).
Treatment with BTX injections is a highly reviewed topic, and studies seem to indicate that it has therapeutic value (Thomas and Aronovich, 2017; Villa et al., 2019). However, it still remains off-label treatment for TMD. The literature presents multiple evidence supporting the use of BTX injections alone or in combination with other treatments to address TMD, asserting its improvement of pain and quality of life (Thomas and Aronovich, 2017; Villa et al., 2019). The lack of a validated protocol regarding the type of BTX, length of the follow-up period, and outcomes studied makes it difficult to interpret the existing results in the literature. Within our study group, BTX injections had a lower level of overall clinical satisfaction (7.05 ± 2.90, p = 0.021) compared to arthrocentesis and arthroscopy. Moreover, this group of patients had the highest standard deviations across all parameters evaluated, which is in agreement with the answers collected, with some patients reporting full satisfaction and complete improvement in quality of life and others reporting some positive change but not as much as they had expected. This is an important evidence, reinforcing that BTX has efficacy but that perhaps not all patients respond the same way. Another reason that may explain the BTX results is the transient effect and cost. Six patients in our study stated that BTX injections were too expensive for the result to last less than a year. The cost has been referred to be a disadvantage in other studies (Yurttutan et al., 2019; Thambar et al., 2020). Finally, in this group of patients, there was a greater need for some patients to engage more in the physiotherapy sessions and to acquire some muscle relaxation techniques to use in their daily life. This need for greater patient compliance and the potential risk to not fully follow the recommendations could help explain the level of satisfaction achieved. We believe that the results obtained were very satisfactory, especially considering the low risk of the BTX treatment, and therefore it seems to be a viable option that surgeons should consider.
TMJ arthrocentesis was the treatment with the best results, 9.09 ± 0.971. This treatment is described as a simple, less invasive, less expensive, and highly effective procedure with a minimum number of complications and significant clinical benefits (Al-Moraissi, 2015; Laskin, 2018; Soni, 2019). According to Al-Moraissi and colleagues, there may be a current paradigm shift in the treatment of arthrogenous TMD, supporting the initiation of minimally invasive procedures, particularly in combination with platelet-rich plasma or HA sooner in the treatment course, since they seem to be more effective than conservative treatments for pain reduction and MMO improvement. Nevertheless, the success rate of this treatment varies significantly within the available literature. The review performed by Soni in 2019 evaluated seven studies, with a success rate for arthrocentesis ranging from 70% to 95%, and it was recognized that arthrocentesis could re-establish normal mouth opening and reduce pain and functional disorder (Soni, 2019).
With a small difference in regard to arthrocentesis, the overall clinical satisfaction obtained with TMJ arthroscopy was 9.03 ± 1.13. According to Laskin, the effectiveness of both arthrocentesis and arthroscopy is comparable (Laskin, 2018). However, arthrocentesis is less invasive, less expensive, and is associated with less post-operative morbidity and possible complications (Laskin, 2018). In addition, unlike arthrocentesis, arthroscopy is performed under general anesthesia, which may lead to a greater potential for complications and also contribute to a longer recovery period. Nevertheless, the arthroscopy group of patients still presented with high levels of satisfaction regarding postoperative recovery. Instead, TMJ arthroscopy allows the surgeon to see the joint during the procedure, thus having a diagnostic and therapeutic role (Sidebottom and Murakami, 2017) that cannot be equaled by arthrocentesis. Moreover, arthroscopy has shown to be superior to arthrocentesis in terms of improvement of mouth opening (Al-Moraissi et al., 2020). However, in this work, patients who undergone arthrocentesis and arthroscopy had equal satisfaction levels regarding the ability to open the mouth and to chew.
Open surgery without alloplastic material is used only in more advanced cases of TMD (Li and Leung, 2021) and sometimes as a last attempt to prevent the need for a replacement joint. Al-Moraissi and colleagues concluded that there are not enough data available to draw meaningful conclusions as to the efficacy of open surgery versus minimally invasive procedures (Al-Moraissi et al., 2020). Open surgery should be the last resort to treat progressive stages of arthrogenous disease when conservative approaches fail. Even though our study participants still reported high levels of satisfaction (8.38 ± 1.84), three of them also described side effects that had implications for their quality of life: facial hypoesthesia, tinnitus, and maxillary deviation. The greater risk of complications, in combination with the fact that it is a more invasive treatment with a longer postoperative recovery, may explain the lower levels of satisfaction achieved (8.25 ± 1.44), althought without statistically significant differences.
The analysis of satisfaction with pain resolution, mouth opening, and chewing ability were included as patient-related outcome measures. No statistical differences were found between the different types of treatment. Because of the complexity of the disease, it may be a combination of indirect measurements and factors that can contribute to overall clinical satisfaction with treatment. Although, not the target of analysis in this manuscript, the authors believe that patient experience with the treatment may also influence answers to the questionnaire.
TMD have been related to emotional distress, disturbed sleep, and impaired oral health—related quality of life (Lei et al., 2021). Depression, anxiety, and stress usually coexist in patients with TMD and they appear to be interconnected (Lei et al., 2015). Patients in our study also reported the exacerbation of the symptoms in periods of greater stress and anxiety, which is in accordance with the review by Li and Leung (2021), who reported that symptoms may be exacerbated during times of stressful events in TMD patients. This is an important fact, since some studies suggest that parafunctional oral habits could be a risk factor for myofascial pain and disc derangement (Michelotti et al., 2010). This is in accordance with our work, in which 46 patients (38.3%) were diagnosed with anxiety and 30 patients (25.0%) with depression in the present or recent past. There was also a statistically significant correlation between the need for further TMJ intervention and the presence of a depression diagnostic (r = 0.186; p = 0.043). It is well established that depression and pain intensity have complex interactions (Goesling et al., 2013). Severe depression and higher levels of somatization are associated with TMD of arthrogenous and myogenous origins (Yap et al., 2002). On the contrary, no statistically significant correlation was identified between the need for further TMJ treatment and anxiety diagnosis, which corroborates the work of Reiter and colleagues, who suggested a less significant role of anxiety in TMD (Reiter et al., 2015).
In this study, it was found the correlation between overall clinical satisfaction and the fulfillment of patients' expectations (r = 0.803, p < 0.0001). It is clear that, when the outcome of treatment fails to meet patients’ expectations, they will express more dissatisfaction with the outcome (Graham, 2016). Therefore, and as pointed out by our patients during the survey, surgeons must explain, prior to treatment, what would be a reasonable outcome, how long it might take to achieve it, how long it would last, and possible risks and complications. The fulfillment of these premises will help the patient not to feel disappointed in relation to prior expectations. Instead, higher preoperative levels of pain, or DDwR and DDwoR diagnoses and severity of the disease (Dimitroulis classification), have not been shown to correlate with lower levels of satisfaction. This result showed that the degree of satisfaction was not correlated with the type of diagnosis and the severity of the disease. The main reason for lower degrees of satisfaction were related to the presence of pain after treatment (Table 6). This fact was corroborated by the inverse correlation of the degree of satisfaction with post-treatment pain (VAS) recorded by the clinician (p = 0.003) (Table 5).
The main limitations of this study were: 1) the postoperative period was different between patients; long periods can contribute to recall bias, and with short periods it is possible that maximum satisfaction was not yet achieved; 2) the small number of patients with different diagnosis; 3) the authors assessed the presence of an anxiety or depression diagnosis only in the present or recent past but did not take into account how many years mean “recent past”; 4) this study included a non-validated questionnaire; and 5) a sample size calculation was not performed.
Conclusion
Within the limitations of the study it seems that patient expectations should be addressed ad initium, and the presence of a diagnosis of depression with concomitant TMD must alert the clinical team and patient for the possible need of additional treatment.
Authors: Ana Lúcia Pereira Rodrigues, Henrique José Cardoso, David Faustino Ângelo
References:
- Ahmad, M., Schiffman, E.L., 2016. Temporomandibular joint disorders and orofacial pain. Dent. Clin. 60, 105-124.
- Al-Moraissi, E.A., 2015. Arthroscopy versus arthrocentesis in the management of internal derangement of the temporomandibular joint: a systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 44, 104-112.
- Al-Moraissi, E.A., Conti, P.C.R., Alyahya, A., Alkebsi, K., Elsharkawy, A., Christidis, N., 2021. The hierarchy of different treatments for myogenous temporomandibular disorders: a systematic review and network meta-analysis of randomized clinical trials. Oral Maxillofac. Surg. https://doi.org/10.1007/s10006-021-01009-y.
- Al-Moraissi, E.A., Wolford, L.M., Ellis, E., Neff, A., 2020. The hierarchy of different treatments for arthrogenous temporomandibular disorders: a network meta-analysis of randomized clinical trials. J. Cranio-Maxillofacial Surg. 48, 9-23.
- Ângelo, D.F., 2020. A letter to the editor on "Root of helix inter tragus notch incision (RHITNI) for temporomandibular open surgery. Int. J. Surg. 83, 233-234.
- Ângelo, D.F., Araújo, R.A.D., Sanz, D., 2021. Surgical complications related to temporomandibular joint arthroscopy: a prospective analysis of 39 single-portal versus 43 double-portal procedures. Int. J. Oral Maxillofac. Surg. 50, 1089-1094.
- Ângelo, D.F., Sanz, D., Cardoso, H.J., 2022. Unilateral temporomandibular joint discectomy without interposal material in patients with disc perforation or fragmentation: a prospective study. J. Oral Maxillofacial Surg. Med. Pathol. 34, 375-380.
- Awan, K.H., Patil, S., Alamir, A.W.H., Maddur, N., Arakeri, G., Carrozzo, M., Brennan, P.A., 2019. Botulinum toxin in the management of myofascial pain associated with temporomandibular dysfunction. J. Oral Pathol. Med. 48, 192-200.
- Bas, B., Yuceer, E., Kazan, D., Gurbanov, V., Kutuk, N., 2019. Clinical and intra-operative factors affecting the outcome of arthrocentesis in disc displacement without reduction: a retrospective study. J. Oral Rehabil. 46, 699-703.
- Chow, A., Mayer, E.K., Darzi, A.W., Athanasiou, T., 2009. Patient-reported outcome measures: the importance of patient satisfaction in surgery. Surgery 146, 435-443.
- Dimitroulis, G., 2013. A new surgical classification for temporomandibular joint disorders. Int. J. Oral Maxillofac. Surg. 42, 218-222.
- Dimitroulis, G., 2018. Management of temporomandibular joint disorders: a surgeon's perspective. Aust. Dent. J. 63 (Suppl. 1), S79-S90.
- Doucet, J.C., Morrison, A.D., 2011. Bilateral mandibular condylysis from systemic sclerosis: case report of surgical correction with bilateral total temporomandibular joint replacement. Craniomaxillofacial Trauma Reconstr. 4, 11-18.
- Eriksson, L., Westesson, P.-L., 2001. Discectomy as an effective treatment for painful temporomandibular joint internal derangement: a 5-year clinical and radiographic follow-up. J. Oral Maxillofac. Surg. 59, 750-758.
- Espeland, L., Høgevold, H.E., Stenvik, A., 2008. A 3-year patient-centred follow-up of 516 consecutively treated orthognathic surgery patients. Eur. J. Orthod. 30, 24e30.
- Goesling, J., Clauw, D.J., Hassett, A.L., 2013. Pain and depression: an integrative review of neurobiological and psychological factors. Curr. Psychiatr. Rep. 15, 421. Goiato, M.C., Zuim, P.R.J., Moreno, A., Dos Santos, D.M., da Silva, E.V.F., de Caxias, F.P., Turcio, K.H.L., 2017. Does pain in the masseter and anterior temporal muscles influence maximal bite force? Arch. Oral Biol. 83, 1-6.
- Graham, B., 2016. Defining and measuring patient satisfaction. J. Hand. Surg. Am. 41, 929-931.
- Graham, B., Green, A., James, M., Katz, J., Swiontkowski, M., 2015. Measuring patient satisfaction in orthopaedic surgery. J. Bone Joint Surg. Am. 97, 80-84.
- Hargreaves, D.S., Sizmur, S., Pitchforth, J., Tallett, A., Toomey, S.L., Hopwood, B., Schuster, M.A., Viner, R.M., 2018. Children and young people's versus parents' responses in an English national inpatient survey. Arch. Dis. Child. 103, 486-491.
- Insel, O., Glickman, A., Reeve, G., Kahan, B., Tran, T., Israel, H., 2020. New criteria demonstrate successful outcomes following temporomandibular joint (TMJ) arthroscopy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 130, e20-e21.
- Kahlenberg, C.A., Nwachukwu, B.U., McLawhorn, A.S., Cross, M.B., Cornell, C.N., Padgett, D.E., 2018. Patient satisfaction after total knee replacement: a systematic review. HSS J. 14, 192-201.
- Krug, J., Jirousek, Z., Suchmová, H., Cermáková, E., 2004. Influence of discoplasty and discectomy of the temporomandibular joint on elimination of pain and restricted mouth opening. Acta Med. 47, 47-53.
- Laskin, D.M., 2018. Arthroscopy versus arthrocentesis for treating internal derangements of the temporomandibular joint. Oral Maxillofac. Surg. Clin. 30, 325-328.
- Lei, J., Liu, M.Q., Yap, A.U., Fu, K.Y., 2015. Sleep disturbance and psychologic distress: prevalence and risk indicators for temporomandibular disorders in a Chinese population. J Oral Facial Pain Headache 29, 24-30.
- Lei, J., Yap, A.U., Zhang, M., Fu, K.-Y., 2021. Temporomandibular disorder subtypes, emotional distress, impaired sleep, and oral health-related quality of life in Asian patients. Community Dent. Oral Epidemiol. 49, 543-549.
- Li, D.T.S., Leung, Y.Y., 2021. Temporomandibular disorders: current concepts and controversies in diagnosis and management. Diagnostics 11, 459.
- Liu, F., Steinkeler, A., 2013. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent. Clin. 57, 465e479.
- Machado, D., Martimbianco, A.L.C., Bussadori, S.K., Pacheco, R.L., Riera, R., Santos, E.M., 2020. Botulinum toxin type A for painful temporomandibular disorders: systematic review and meta-analysis. J. Pain 21, 281-293.
- Mahomed, N., Gandhi, R., Daltroy, L., Katz, J.N., 2011. The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis, 591253, 2011.
- Michelotti, A., Cioffi, I., Festa, P., Scala, G., Farella, M., 2010. Oral parafunctions as risk factors for diagnostic TMD subgroups. J. Oral Rehabil. 37, 157e162.
- Murphy, M.K., MacBarb, R.F., Wong, M.E., Athanasiou, K.A., 2013. Temporomandibular disorders: a review of etiology, clinical management, and tissue engineering strategies. Int. J. Oral Maxillofac. Implants 28, e393-e414.
- Paesani, D., Westesson, P.-L., Hatala, M., Tallents, R.H., Kurita, K., 1992. Prevalence of temporomandibular joint internal derangement in patients with craniomandibular disorders. Am. J. Orthod. Dentofacial Orthop. 101, 41-47.
- Posnick, J.C., Wallace, J., 2008. Complex orthognathic surgery: assessment of patient satisfaction. J. Oral Maxillofac. Surg. 66, 934-942.
- Rauck, R.C., Ruzbarsky, J.J., Swarup, I., Gruskay, J., Dines, J.S., Warren, R.F., Dines, D.M., Gulotta, L.V., 2020. Predictors of patient satisfaction after reverse shoulder arthroplasty. J. Shoulder Elbow Surg. 29, e67-e74.
- Reiter, S., Emodi-Perlman, A., Goldsmith, C., Friedman-Rubin, P., Winocur, E., 2015. Comorbidity between depression and anxiety in patients with temporomandibular disorders according to the research diagnostic criteria for temporo-mandibular disorders. J Oral Facial Pain Headache 29, 135-143.
- Schiffman, E., Ohrbach, R., Truelove, E., Look, J., Anderson, G., Goulet, J.P., List, T., Svensson, P., Gonzalez, Y., Lobbezoo, F., Michelotti, A., Brooks, S.L., Ceusters, W., Drangsholt, M., Ettlin, D., Gaul, C., Goldberg, L.J., Haythornthwaite, J.A., Hollender, L., Jensen, R., John, M.T., De Laat, A., de Leeuw, R., Maixner, W., van der Meulen, M., Murray, G.M., Nixdorf, D.R., Palla, S., Petersson, A., Pionchon, P., Smith, B., Visscher, C.M., Zakrzewska, J., Dworkin, S.F., 2014. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain Headache 28, 6-27.
- Schwartz, M., Freund, B., 2002. Treatment of temporomandibular disorders with botulinum toxin. Clin. J. Pain 18, S198-S203.
- Sidebottom, A., Murakami, K., 2017. 96 - arthrocentesis and arthroscopic management of the temporomandibular joint. In: Brennan, P.A., Schliephake, H., Ghali, G.E., Cascarini, L. (Eds.), Maxillofacial Surgery, third ed. Churchill Livingstone, pp. 1473-1479. https://doi.org/10.1016/B978-0-7020-6056-4.00096-4.
- Sipahi Calis, A., Colakoglu, Z., Gunbay, S., 2019. The use of botulinum toxin-A in the treatment of muscular temporomandibular joint disorders. J. Stomatol. Oral Maxillofac. Surg. 120, 322-325.
- Song, P., Schwartz, J., Blitzer, A., 2007. The emerging role of botulinum toxin in the treatment of temporomandibular disorders. Oral Dis. 13, 253-260.
- Soni, A., 2019. Arthrocentesis of temporomandibular jointebridging the gap between non-surgical and surgical treatment. Annal. Maxillofac. Surg. 9, 158-167. Sunil Dutt, C., Ramnani, P., Thakur, D., Pandit, M., 2015. Botulinum toxin in the treatment of muscle specific oro-facial pain: a literature review. J. Maxillofac. Oral Surg. 14, 171-175.
- Thambar, S., Kulkarni, S., Armstrong, S., Nikolarakos, D., 2020. Botulinum toxin in the management of temporomandibular disorders: a systematic review. Br. J. Oral Maxillofac. Surg. 58, 508-519.
- Thomas, N.J., Aronovich, S., 2017. Does adjunctive botulinum toxin A reduce pain scores when combined with temporomandibular joint arthroscopy for the treatment of concomitant temporomandibular joint arthralgia and myofascial pain? J. Oral Maxillofac. Surg. 75, 2521-2528.
- Villa, S., Raoul, G., Machuron, F., Ferri, J., Nicot, R., 2019. Improvement in quality of life after botulinum toxin injection for temporomandibular disorder. J. Stomatol. Oral Maxillofac. Surg. 120, 2-6.
- Weaver, N., Glover, K., Major, P., Varnhagen, C., Grace, M., 1998. Age limitation on provision of orthopedic therapy and orthognathic surgery. Am. J. Orthod. Dentofacial Orthop. 113, 156-164.
- Yap, A.U., Cao, Y., Zhang, M.-J., Lei, J., Fu, K.-Y., 2021. Comparison of emotional disturbance, sleep, and life quality in adult patients with painful temporomandibular disorders of different origins. Clin. Oral Invest. 25, 4097-4105.
- Yap, A.U.J., Tan, K.B.C., Prosthodont, C., Chua, E.K., Tan, H.H., 2002. Depression and somatization in patients with temporomandibular disorders. J. Prosthet. Dent 88, 479e484.
- Yurttutan, M.E., Tütüncüler Sancak, K., Tüzüner, A.M., 2019. Which treatment is effective for bruxism: occlusal splints or botulinum toxin? J. Oral Maxillofac. Surg. 77, 2431-2438.
