Hearing changes after temporomandibular joint arthroscopy: a prospective study
Abstract
Temporomandibular Joint (TMJ) arthroscopy is considered an effective and safe minimally invasive surgical approach. While the long-term outcomes of arthroscopy tend to be positive and free of secondary effects, patients occasionally complain about their hearing following the treatment. The aim of this prospective study was to investigate possible hearing changes associated with TMJ arthroscopy. Pure-tone audiograms were performed in patients two weeks before TMJ arthroscopy and repeated six weeks after intervention. A total of 15 patients (mean age of 41.73 ± 16.36) were enrolled; 25 TMJ arthroscopies were performed (five unilateral and 10 bilateral). Statistically significant differences were found between preoperative and postoperative audiograms in the frequencies 256 Hz (P = 0.011) and 8 kHz (P = 0.058, borderline). For the frequency 256 Hz the difference was favourable, but not superior to 5 dB. For the frequency 8 kHz, in three patients the TMJ arthroscopy resulted in a decrease of 10 dB. However, no clinical hearing changes or complaints were observed in the involved patients. No differences in audiograms between level 1 or 2 arthroscopy were observed. The study reinforces the safety of the TMJ arthroscopy level 1 and 2 with the reported protocol. The authors recommend larger studies to validate the results, specially for frequency 8 kHz.
Temporomandibular disorders (TMD) are among the most common causes of orofacial pain. Many studies have reported an association between TMD and otological symptoms such as hypoacusis, hearing loss, tinnitus, earache, vertigo and ear fullness. Temporomandibular joint (TMJ) arthroscopy is a minimally invasive surgical option for intra-articular disorders with good long-term results and is considered a safe procedure. During 4 years of regular TMJ arthroscopic practice in our department, two patients reported subjective hearing changes following the procedure, which was a cause for concern. Available literature on the topic from 1989 did not report any changes in audiograms after TMJ arthroscopy. In the authors’ opinion, there are three potential causes for hearing changes after TMJ arthroscopy: (1) Acoustic trauma, caused by drilling during the operation, could occur if the sound level meter (SLM) exceeded 118 dBA (with variation being associated with drill speeds and different burr types). We were able to exclude this possibility because burrs are not used in TMJ arthroscopy operations carried out in our department, and the coblator ReFlex Ultra with plasma technology does not produce any significant sound or vibration. (2) Acoustic damage caused by the compression of major structures due to extravasation of fluid into surrounding tissues or high intra-articular pressure in arthroscopic surgery (14.883 kPa 0.860). We exclude this as a possible cause, because the noble structures of the ear are enclosed in the otic capsule, surrounded by solid bone. (3) Acoustic damage due to turbulence and vibration associated to fluid lavage. We have accepted this hypothesis, which is supported by the observation that continuous vibration can induce histological cochlear damage. In 2013, a computational TMJ fluid dynamics analysis demonstrated that during TMJ arthroscopy the fluid speed in the joint could fall in a range of 0.740 m/s ± 0.106, substantially higher than in arthrocentesis (0.063 m/s ± 0.020). The increased fluid speed during joint lavage could be associated with vortices, turbulence and vibration in the joint, leading to possible hearing damage. This would probably go unnoticed unless audiometry were performed.
This prospective study aims to evaluate the possible effect of TMJ arthroscopy on the ear, comparing pure-tone audiogram changes before and after surgery.
Materials and Methods
Study Design
This prospective study was conducted at the Instituto Portugueˆs da Face, Lisboa, Portugal from January 1, 2019 to December 31, 2019. The study was approved by the ethics com- mittee of Centro Academico de Medicina de Lisboa. All enrolled patients gave their informed consent in writing, in accordance with the current legislation. Patient data was scrubbed of any personal identifying parameters and each patient was given a random ID number. The criteria for study inclusion were: (1) age >18 years; (2) TMD fulfilling the criteria for TMJ arthroscopy; (3) magnetic resonance imaging (MRI) presenting intra-articular pathology. The exclusion criteria were the presence of previous: (1) TMJ surgical intervention; (2) facial trauma; (3) otologic pathology; (4) otologic surgical intervention. An audiology technician performed a pure-tone audiometry on two distinct timelines: 2 weeks preoperative and 6 weeks postoperative. All patients were tested for hearing bilaterally regardless of whether their arthroscopy was unilateral or bilateral. Bilateral arthroscopies were ana- lysed as isolated unilateral arthroscopies. No distinction was made between left and right sides. No other otological symptoms were accessed.
Surgical Protocol
All patients underwent general anaesthesia with nasotracheal intubation, managed in most cases using intravenous protocol, usually with remifentanil and tranexamic acid infusion. Intraoperative steroids, usually dexamethasone, were administered, primarily to minimize postoperative swelling. TMJ arthroscopy was performed with a 1.9-mm arthroscope including a video system (Stryker, San Jose, CA, USA), with a 2.8-mm outer protective cannula. Additional equipment included a surgical scalpel (#11 blade), an infusion tube, a three-way pipe and Ringer solution as part of the armamentarium. For TMJ arthroscopy level 1, the authors used the classic puncture with an entry point 10 mm anterior and 2 mm below the Holmlund–Hellsing (H-H) line. The arthroscope was inserted in a forward and upward direction (15–45◦) into the superior joint space. A second puncture with a 21-G needle was performed 30 mm anterior and 7 mm below the H-H line to wash
the joint with 250–300 ml Ringer solution. After washing the joint, 1.5–2 cc of hyaluronic acid was injected into it.
For level 2 TMJ arthroscopy, the second puncture was substituted by a 2.8-mm outer protective cannula with sharp trocar until the joint was reached. The 2.8-mm cannula was used for instrumental passageway for (1) a ReFlex Ultra 45 Plasma Wand system for intra-articular coblation and/or (2) intrasynovial medication through a 22-G long spinal needle. Antibiotic protocol (amoxicillin/clavulanic-acid or clarithromycin) and non-steroidal anti-inflammatory drugs (ibuprofen) were routinely prescribed following surgery and the patients were instructed to follow a soft diet for 3 days postoperatively. Mouth opening exercises were started 1 week after surgery.
Statistical Analysis
Numerical variables were expressed as the mean (± standard deviation) and analysed inferentially using statistical tests. The frequencies studied were: 128 Hz, 256 Hz, 512 Hz, 1 kHz, 2 kHz, 4 kHz and 8 kHz, along with air conduction (AC) and bone conduction (BC). Shapiro–Wilk test was used to determine normality of data. Non-parametric statistics were used given the absence of normality in the distributions under analysis. The Wilcoxon signed-rank test (data with non-normal distribution and symmetrical differences) was performed to compare the distribution of audiogram results before and after surgery, in the search for statistically significant differences between the two groups.
The nonparametric Mann–Whitney U-test was used to compare the distributions of audiogram results between levels 1 and 2 arthroscopies. The level of significance alpha was set at 5%. The statistical analyses were performed using R.
Results
A total of 15 patients aged between 21 and 70 years, mean age of 41.73 (± 16.36 years) were enrolled. Ten patients underwent bilateral arthroscopy and five patients received unilateral arthroscopy, resulting in a total of 25 operated joints. Preoperative audiograms were normal for all but two patients. Both of these had had a previous neurosensorial hypoacusis: the first patient was 70 years old (30 dB in right ear and 30 dB in left ear) and the second patient was 59 years old (31.25 dB right ear and 21.25 dB in left ear).
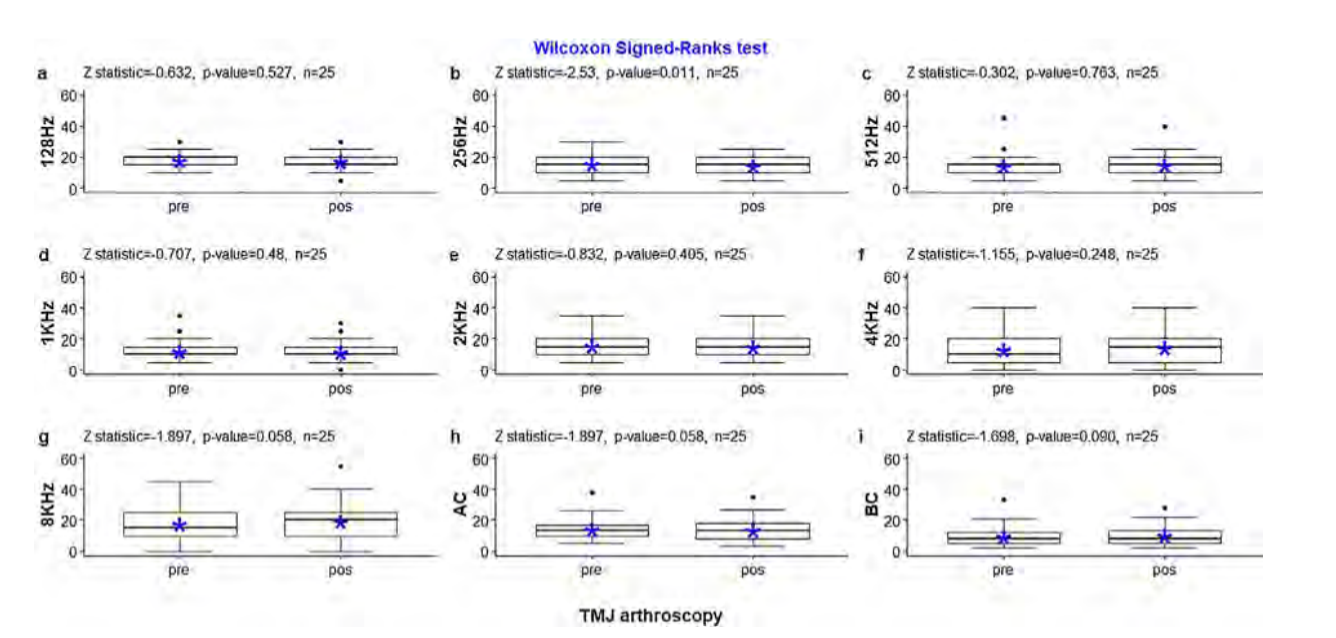
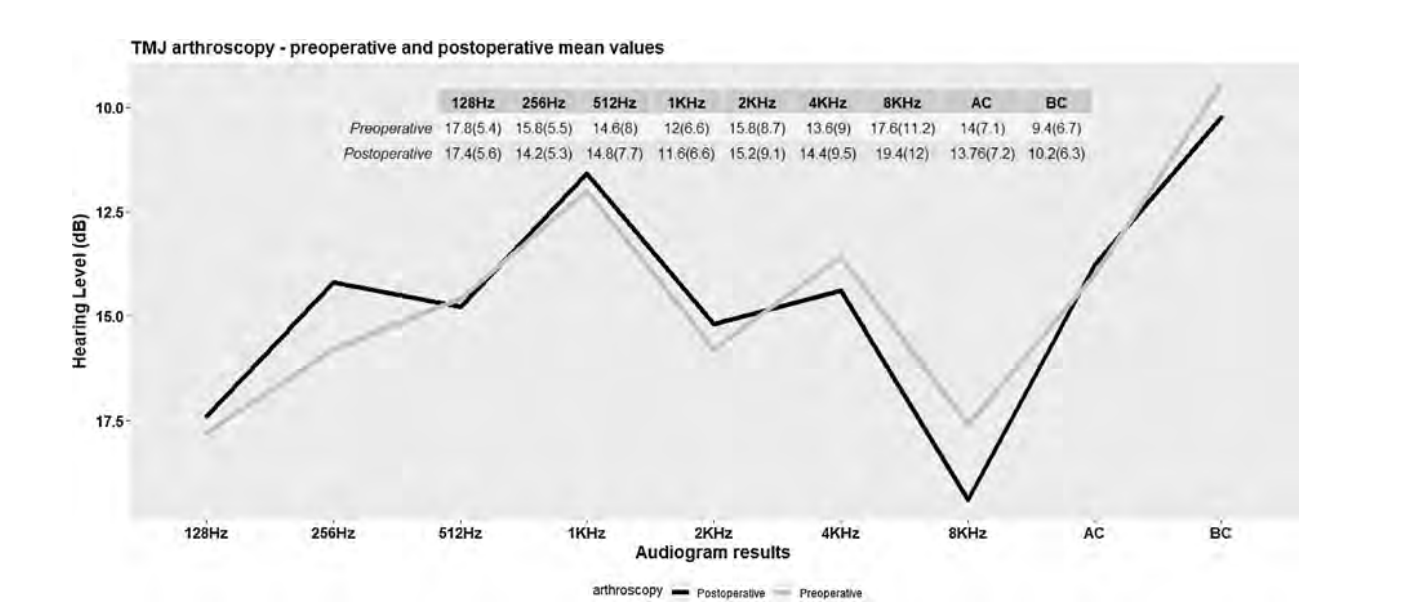
According to Wilcoxon’s test in the 15 patients, we observed statistically significant differences (P < 0.05) between pre-operative and postoperative audiograms in the frequencies 256 Hz (P = 0.011) and 8 kHz (P = 0.058, borderline). None of the patients reported clinical hearing complaints. Fig. 1 shows the detailed results of the Wilcoxon signed-rank test as well as the graphical representation of the percentiles, before and after the surgery. The representation of the mean values for each studied frequency can be seen in Fig. 2.
The nonparametric Mann–Whitney U- test concluded there were no statistically significant differences in the distribution of the audiograms results in relation to levels 1 and 2 of the arthroscopies (W = 3498, P = 0.11).
Discussion
Pure-tone audiometry consists of the study of the minimal auditive threshold for each frequency. Each threshold corresponds to the minimal intensity in which a sound is heard in at least 50% of the presented sequences for each tested frequency. This exam is a behavioural method to access hearing once it depends on the patient voluntary response when a sound is presented. In this regard, the pure-tone audiogram results do not correspond to an exact value; instead, this corresponds to an approximate estimate value around which the patient can hear the minimum auditive stimulus. Combining this definition with the modified Hugson–Westlake limits method, which is the acquisition technique used, means that hearing thresholds 5 dB should be considered as not different. In the present study, the statistical analysis of the audiograms presented significant differences between pre- and postoperative audiograms in the frequencies 256 Hz (P = 0.011) and 8 kHz (P = 0.058)
(Fig. 1). Nonetheless, the range of the differences in frequency 256 Hz was not superior to 5 dB and was an improvement in hearing. Regarding frequency 8 kHz, we observed differences superior to 5 dB in three patients. Those three patients had a deterioration of 10 dB in the pure-tone audiogram, however none of the patients reported any perceptible hearing impairment. This change in frequency 8 kHz could easily go unnoticed by the patient and/or surgeon. More than a hearing impairment, it could lead to tinnitus sensation, which was not observed.
McCain et al.10 and Jerry et al.18, reported no changes in hearing levels following TMJ arthroscopic surgery, however no inferentially statistical tests were used for the different frequencies. In the study by McCain et al.10 the postoperative evaluation was performed 4 weeks after intervention, in Jerry et al.18 after 48 h, while in our study it was performed 6 weeks after.
We did not observe any differences in audiograms between single or double puncture. Moreover, no data has been reported in the literature regarding this topic.
Concerning the possible non-surgical causes of hearing changes, most are outside the scope of TMJ surgeons, as they are generally related to epidural anesthesia or cardiopulmonary bypass surgery. However, prior to 2009, a total of 52 cases of hearing loss following non-otological surgery with general anaesthesia were reported. Rare cases were associated with maxillofacial procedures; however, we found one report related to hearing loss following bilateral TMJ arthroscopy. In this specific case, the anesthesia protocol included nitrous oxide, and the cause was attributed to this toxic gas. Nitrous oxide is 30 times more soluble in blood than nitrogen. Therefore, nitrous oxide penetrates the middle ear faster than nitrogen is expelled, resulting in increased middle ear pressure, which leads to barotrauma. One case of idiopathic hearing loss after a forehead lift was reported; this continues to be a difficult situation to manage, especially in cosmetic surgery. In 1991, four cases of sudden deafness following dental surgery were reported (one using general anaesthesia and three using local anaesthesia), but no explanation has been given to account for this deafness. The cause of hearing loss following general anaesthesia remains unknown. A variety of potential causes have been suggested, including changes in middle ear pressure, cerebro-spinal fluid pressure change, vascular disease, embolism, ototoxic drugs, and other miscellaneous issues.
While most studies consider TMJ arthroscopy a safe procedure, the majority are limited to the observation of intra- or immediate postoperative complications, and given the fact that hearing impairment is often subclinical, it can easily go unnoticed unless audiometry is performed. With this prospective study, the authors intended to clarify possible ear changes following TMJ arthroscopy.
The limitations of this study were: (1) the small sample size; (2) the 6-week follow-up audiogram – for future studies it may be helpful to observe changes in more timelines (the authors suggest 3 days, 2 weeks, 4 weeks and 6 weeks postoperatively); (3) the conventional pure-tone audiometry was performed analysing frequencies from 128 Hz to 8 kHz. An extended high-frequency audiometry which evaluates hearing thresholds at frequencies higher than 8 kHz (i.e. 10, 12, 14, 16, 18 and 20 kHz) could present new results; (4) the hypothesis that turbulence and vibration are associated with fluid velocity was not tested or confirmed; (5) no otoscopy was performed; (6) no other otological symptoms were accessed.
In summary, in this study the authors observed statistically significant differences for frequencies 256 Hz (hearing improvement) and 8 kHz (hearing impairment) between preoperative and postoperative audiograms, however no clinical changes were observed. No differences were found for level 1 and 2 TMJ arthroscopy (P = 0.11).
Larger studies are recommended (with other otological assessments, if possible) to allow for clinical hearing changes assessments. Regular audiometry tests for older patients could be adopted as a preventive measure, as those patients may be more likely to experience subclinical changes at higher frequencies (4 kHz and 8 kHz).
Authors: D.F. Ângelo, A. Moreira, D. Sanz, R. São João
References:
- Chang C-L, Wang D-H, Yang M-C, Hsu W- E, Hsu M-L. Functional disorders of the temporomandibular joints: Internal derangement of the temporomandibular joint. Kaohsiung J Med Sci 2018;34(4):223–30. http://dx.doi.org/10.1016/j.kjms.2018.01.004.
- Costen JB. A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. Ann Otol Rhinol Laryngol 1997;106(10):805–19. http://dx.doi.org/10.1177/000348949710601002.
- Effat KG. Otological symptoms and audiometric findings in patients with temporoman- dibular disorders: Costen’s syndrome revisited. J Laryngol Otol 2016;130 (12):1137–41. http://dx.doi.org/10.1017/S0022215116009300.
- Michiels S, van der Wal AC, Nieste E, Van de Heyning P, Braem M, Visscher C, et al. Conservative therapy for the treatment of patients with somatic tinnitus attributed to temporomandibular dysfunction: study protocol of a randomised controlled trial. Trials 2018;19(1):554. http://dx.doi.org/10.1186/s13063-018-2903-1.
- Pinto OF. A new structure related to the temporomandibular joint and middle ear. J Prosthet Dent 1962;12(1):95–103. http://dx.doi.org/10.1016/0022-3913(62)90014-8.
- Totta T, Santiago G, Gonçales ES, Saes S de O, Berretin-Felix G. Auditory characteristics of individuals with temporomandibular dysfunctions and dentofacial deformities. Dental Press J Orthod 2013;18(5):70–7. http://dx.doi.org/10.1590/S2176-94512013000500013.
- Miloro M, Gahli G, Larsen P, Waite P. Peterson’s Principles Of Oral & Maxillofacial Surgery, Third Edition. 3rd ed. 2011. Pmph USA.
- Carls FR, Engelke W, Locher MC, Sailer HF. Complications following arthroscopy of the temporomandibular joint: analysis covering a 10-year period (451 arthroscopies). J Cranio- maxillofac Surg 1996;24(1):12–5. http://dx.doi.org/10.1016/s1010-5182(96)80071-0.
- Fernández Sanromán J, Costas López A, Fernández Ferro M, de Sánchez AL, Stavaru B, Arenaz Bua J. Complications of tempo-romandibular joint arthroscopy using two-portal coblation technologies: A prospective study of 475 procedures. J Craniomaxillofac Surg 2016;44(9):1221–5. http://dx.doi.org/10.1016/j.jcms.2016.06.027.
- McCain JP, Goldberg HM, de la Rua H. Preoperative and postoperative audiologic measurements in patients undergoing ar- throscopy of the TMJ. J Oral Maxillofac Surg 1989;47(10):1026–7. http://dx.doi.org/10.1016/0278-2391(89)90173-0.
- Michaelides EM, Kartush JM. Implications of sound levels generated by otologic devices. Otolaryngol Neck Surg 2001;125(4):361–3. http://dx.doi.org/10.1067/mhn.2001.118956.
- Banakis Hartl RM, Mattingly JK, Greene NT, Farrell NF, Gubbels SP, Tollin DJ. Drill-in- duced cochlear injury during otologic surgery. Otol Neurotol 2017;38(7):938–47. http://dx.doi.org/10.1097/MAO.0000000000001474.
- Moussavi Najarkola SA, Khavanin A, Mirzaei R, Salehnia M, Muhammadnejad A. Cochlear damages caused by vibration exposure. Iran Red Crescent Med J 2013;15(9):771–4. http://dx.doi.org/10.5812/ircmj.5369.
- Hamernik RP, Henderson D, Coling D, Slepecky N. The interaction of whole body vibration and impulse noise. J Acoust Soc Am 1980;67 (3):928–34. http://dx.doi.org/10.1121/1.383942.
- Hamernik RP, Henderson D, Coling D, Salvi R. Influence of vibration on asymptotic threshold shift produced by impulse noise. Int J Audiol 1981;20(3):259–69. http://dx.doi.org/10.3109/00206098109072700.
- Xu Y, Lin H, Zhu P, Zhou W, Han Y, Zheng Y, et al. A comparative study between use of arthroscopic lavage and arthrocentesis of temporomandibular joint based on computa- tional fluid dynamics analysis. PLoS One 2013;8(11)e78953. http://dx.doi.org/10.1371/journal.pone.0078953.
- Cooper WA, Stokinger TE, Billings BL. Pure tone delayed auditory feedback: de- velopment of criteria of performance deterioration. J Am Audiol Soc 1976;1 (5):192–6.
- Jones JL, Horn KL. The effect of temporo- mandibular joint arthroscopy on ear func- tion. J Oral Maxillofac Surg 1989;47 (10):1022–5. http://dx.doi.org/10.1016/0278-2391(89)90172-9.
- Sato FRL, Tavares RC. Abducens palsy after temporomandibular joint arthroscopy: a rare complication. Oral Maxillofac Surg 2016;20 (3):327–30. http://dx.doi.org/10.1007/s10006-016-0559-0.
- Fog J, Wang LP, Sundberg A, Mucchiano C. Hearing loss after spinal anesthesia is related to needle size. Anesth Analg 1990;70 (5):517–22. http://dx.doi.org/10.1213/00000539-199005000-00009.
- Murad NJ, Patel C, Turner CR. Unilateral sensorineural hearing loss after general an- aesthesia. Anaesthesia 2008;63(5). http://dx.doi.org/10.1111/j.1365-2044.2008.05533.x.559–559.
- Punj J, Pandey R, Darlong V. Sensorineural hearing loss after general anaesthesia: 52 cases reported until now! Anaesthesia 2009;64(2). http://dx.doi.org/10.1111/j.1365-2044.2008.05846.x.226–226.
- Evan KE, Tavill MA, Goldberg AN, Silverstein H. Sudden sensorineural hearing loss after general anesthesia for nonotologic surgery. Laryngoscope 1997;107(6):747–52. http://dx.doi.org/10.1097/00005537-199706000-00008.
- Hsieh C-H, Tsai H-H, LiLiang P-C, Yeh M-C, Jeng S-F. Acute hearing loss following a forehead lift. Plast Reconstr Surg 2005;115(7). http://dx.doi.org/10.1097/01.PRS.0000164679.92423.58.115e-118e.
- Farrell RW, Pemberton MN, Parker AJ, Buf- fin JT. Sudden deafness after dental surgery. BMJ 1991;303(6809). http://dx.doi.org/10.1136/bmj.303.6809.1034.1034–1034.
- Sprung J, Bourke DL, Contreras MG, Warner ME, Findlay J. Perioperative hearing impairment. Anesthesiology 2003;98(1):241–57.
- Dreyer M, Migdal H. Transient medium- and deep-tone hearing disorders following spinal anesthesia. Reg Anaesth 1990;13(6):138–41.
