Unilateral temporomandibular joint discectomy without interposal material in patients with disc perforation or fragmentation: A prospective study
Abstract
Objective: Temporomandibular joint (TMJ) discectomy is one of the most popular surgical techniques for patients with an unsalvageable disc. Previous studies have demonstrated predictable results of discectomy with optimal results in pain reduction and maximum mouth opening (MMO) improvement. However, those studies had most of the times wide-ranging inclusion criteria. This study was therefore conducted to assess the role of unilateral TMJ discectomy in a well defined diagnosis.
Methods: A 6-year prospective study was designed including patients treated with unilateral TMJ discectomy without interposal material, preserving condyle and temporal fibrocartilage, for two specific intra-articular diagnosis: disc perforation and disc fragmentation.
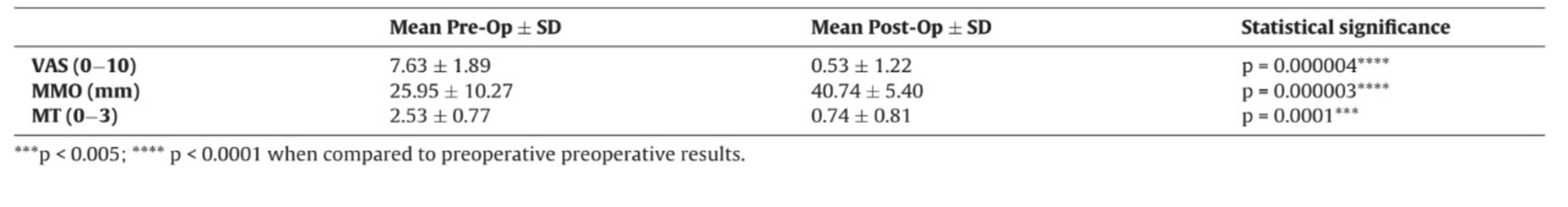
Results: A total of 19 patients were enrolled, with a mean age of 51.05 ± 13.71 (mean ± SD) years. Preoperative pain was 7.63 ± 1.89 (mean ± SD), MMO was 25.95 ± 10.27 mm (mean ± SD) and muscle tenderness (MT) was 2.53 ± 0.77 (mean ± SD). The most common diagnosis was disc perforation. After an average of 37.9 months of follow-up time (range from 10 to 71 months), a statistically significant improvement of pain (P < 0.0001), MMO (P < 0.0001) and MT (P = 0.00011) was observed. Postoperatively, 16 of 18 patients (89 %) showed a reduction in pain and improvement in MMO, fulfilling the criteria for a successful outcome of TMJ surgery. No second surgery was necessary.
Conclusion: Unilateral TMJ discectomy without interposal material in patients with disc perforation or fragmentation seems to be an adequate technique. However, we encourage rigorous long-term studies and new preclinical trials to pursuit a disc substitute, as relevant preclinical trials have demonstrated significant degenerative changes after TMJ discectomy.
Introduction
Temporomandibular disorders (TMD) are the most prevalent orofacial pain source of nondental origin. Those disorders can be due to a heterogeneous group of pathologies affecting the temporomandibular joint (TMJ), the jaw muscles, or both. TMD symptoms prevalence has been reported between 10–33% of the population. The most common signs and symptoms include pain, joint sounds, limitation of mandibular movement, facial deformities, condyle dislocation and recurrent headaches. These symptoms can negatively affect patients’ quality of life. Surgical treatments for TMD are reserved for specific cases, however with the popularization of mini-invasive surgical techniques such as TMJ arthroscopy, more patients have been eligible for these less invasive techniques, amplifying the scope of TMJ surgery. In diagnostics such as ankylosis, tumors and growth abnormalities, TMJ open surgery is strongly recommended; however, those diagnosisare relatively uncommon. TMJ internal derangement involving disc position/integrity and osteoarthrosis are more frequent, but the surgical indication is also more relative. From all the open surgery techniques, TMJ discectomy without interposal material is probably one of the most popular procedures. Recently, Ângelo et al. showed that bilateral discectomy, preserving condyle and temporal fibrocartilage can induce severe imaging and histopathologic TMJ changes in black Merino sheep. Besides, the degenerative changes in the condyle, functional masticatory changes were not observed. In a different preclinical study, disc and fibrocartilage removal resulted in traumatic TMJ ankylosis. It remains poorly understood the role of the condyle and temporal fibrocartilage in the joint, but it appears to be crucial, balancing the disc function. In humans, short-term studies on TMJ discectomy were associated with successful results. Michael Miloro et al. in a retrospective study described discectomy without replacement as an effective procedure improving the maximum mouth opening (MMO). In long-term evaluations, discectomy was effective relieving the pain and led to greater improvement in MMO (>35 mm). Despite the good clinical outcome, some studies have observed degenerative changes in imaging analysis, showing bone changes and remodeling of the mandibular condyle due to mechanical stress. Ellis et al. pointed that a lower improvement in MMO (<10 %) was associated with higher risk of poor outcome and the possible need of a TMJ total joint replacement. Together, clinical and preclinical results showed TMJ discectomy can be considered a suboptimal technique, and an effective disc substitute, acting as a cushion between the condyle and temporal fossa could, in theory, improve these results. Despite extensive research in the field of tissue engineering, currently no appropriate disc substitute has demonstrated safety and efficacy. In fact, the last guidelines do not recommend disc replacement because nonvalid option showed superiority over discectomy alone. While there is no effective disc substitute, discectomy is often used when the disc is partial or total damaged and cannot be salvageable and/or when other techniques fail to relieve the symptoms. Some previous studies have heterogenous inclusion criteria, retrospective data and non-randomization disclosing difficulty to draw clear conclusions about this technique. We designed a rigorous prospective study for patients with: 1) unilateral TMJ disc perforation or 2) unilateral TMJ disc fragmentation. Those patients were proposed to unilateral TMJ discectomy preserving condyle and temporal fibrocartilage.
Material and methods
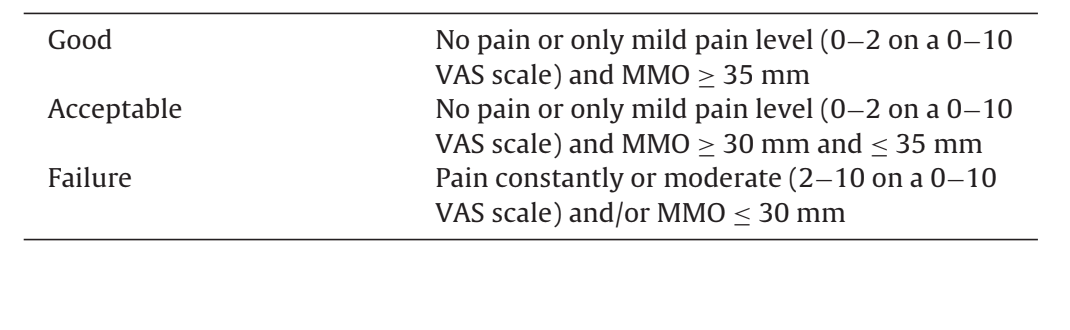
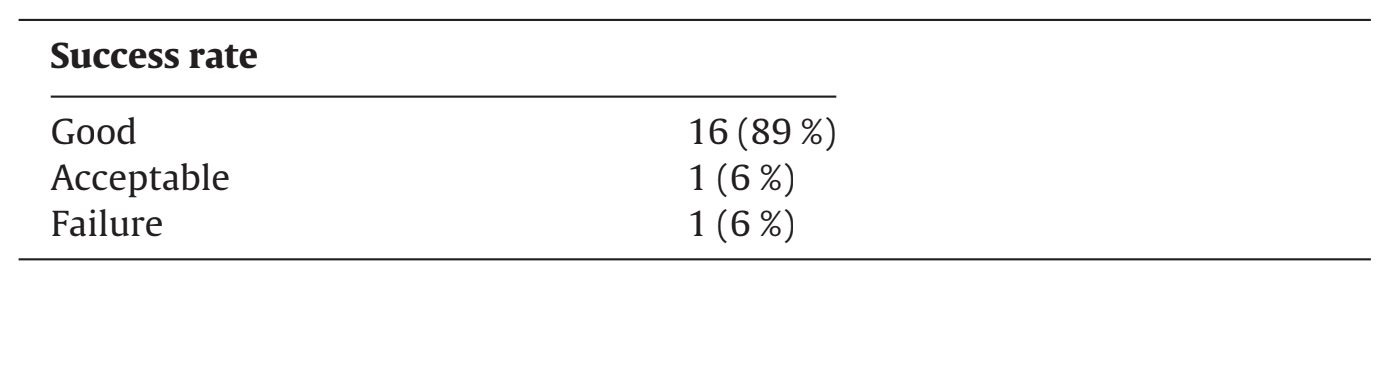
The variables measured throughout the study were TMJ pain, with a Visual Analog Scale (VAS, 0−10, with 0 being no pain and 10 having maximum insupportable pain), MMO (mm) using a certified ruler between the incisor’s teeth and muscle tenderness (MT) through palpation in masseter and temporalis muscle. For MT, the authors used a 0−3 classification as defined in TMD/RDC. This study is in form with the STROCSS guidelines. The study was registered in ClinicalTrials.Gov with the number: NCT04857294. The success rate of the surgery was graded as good, acceptable and failure in accordingly with Table 1 as described by Eriksson, Westesson.
Study design
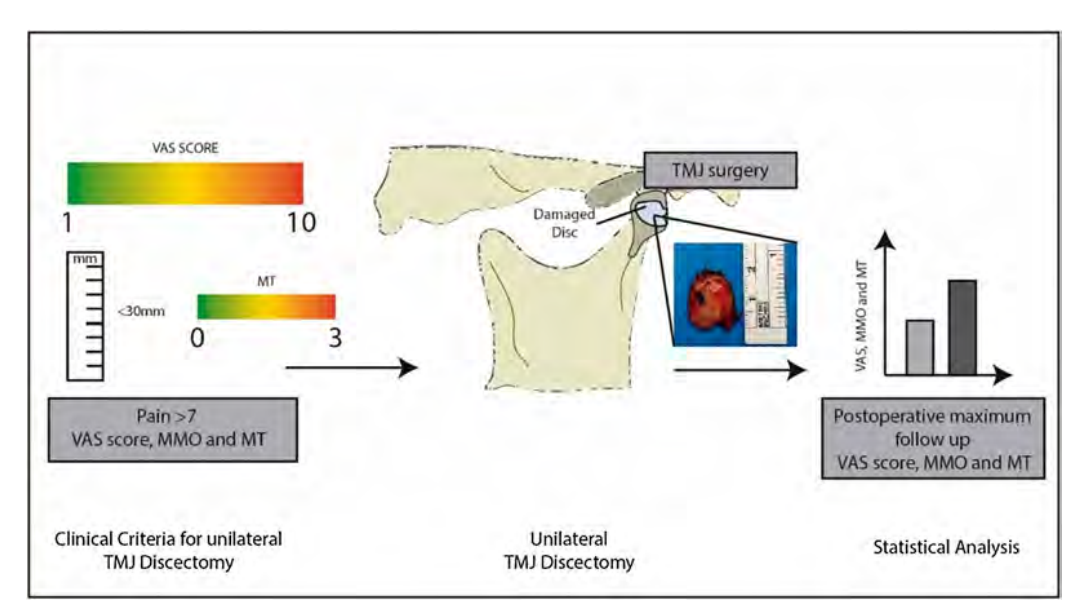
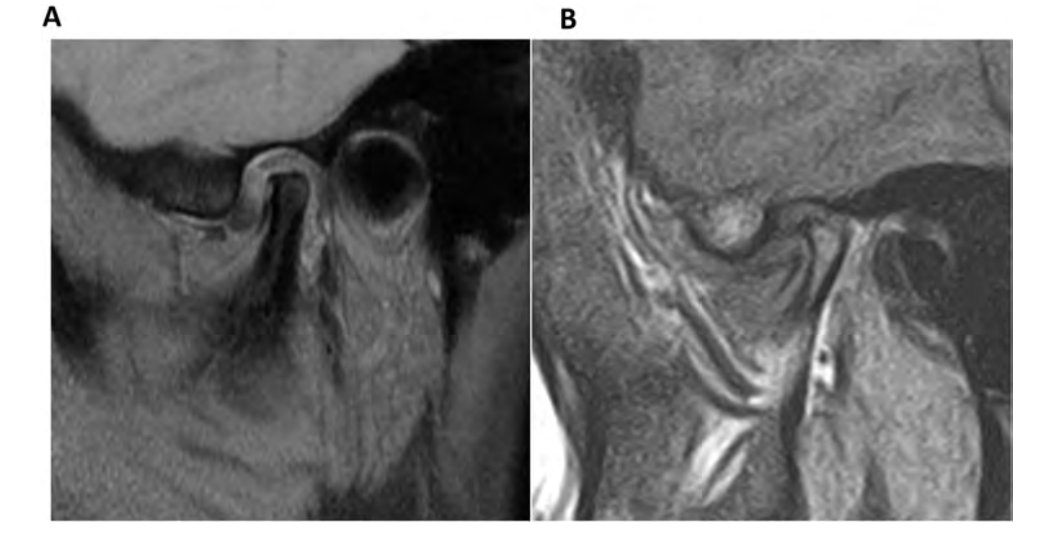
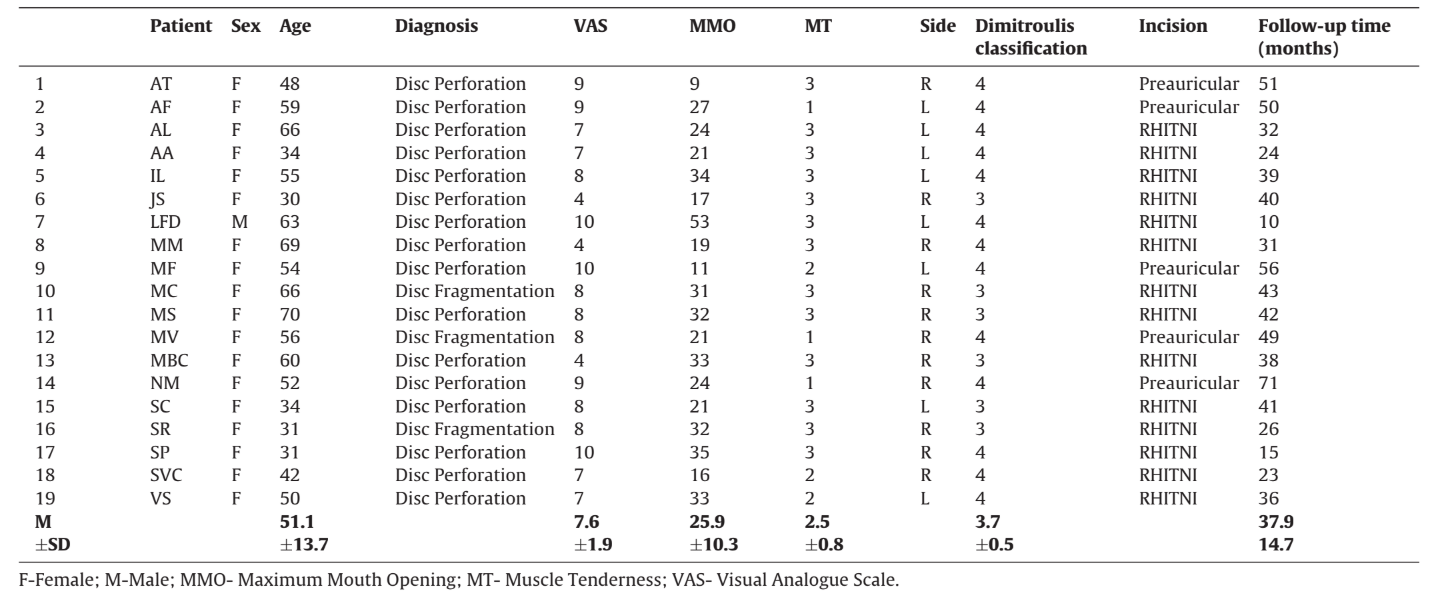
A 6-years prospective study was conducted in Portugal in a private institution from the 1st of January of 2015 to the 1st of October of 2021. The study was approved by the ethics review board. All enrolled patients gave their informed consent in writing, following current legislation. Patient data was scrubbed of any personal identifying parameters and given a random ID number. All surgeries were performed by the same surgeon (D.A.) with the same assistant surgeon (D.S.). The inclusion criteria were: 1) Age > 18 years old; 2) Unilateral TMJ pain >7 (0−10 VAS) and/or MMO < 30 mm (Fig. 1); 3) Magnetic Resonance Imaging (MRI) presenting unilateral disc perforation or disc fragmentation and confirmation of the definitive diagnosis during the surgery (Fig. 2); 4) Clinical and imaging examination with criteria for unilateral TMJ discectomy; 5) Dimitroulis classification in categories 3 and 4. Exclusion criteria: 1) Previous TMJ surgical intervention; 2) Concomitant contralateral surgery; 3) Age < 18 years old; 4) Degenerative changes of the condyle with or without osteophytes confirmed by MRI and intraoperatively. Patients’ VAS score, MMO and MT were registered preoperative and postoperative in the following timeline: T0 (preoperative – 2 weeks); and T1 (postoperative maximum follow-up) (Fig. 1).
Surgical protocol
Preoperative treatment included the use of a splint for more than 6 months and/or medication (NSAIDS and/or myorelaxant) for more than 1 month without symptomatic resolution. During operation, all patients underwent general anesthesia with nasotracheal intubation, managed in most cases with intravenous anesthesia protocol, usually with remifentanil infusion. Intraoperative steroids, usually dexamethasone, were administered primarily to minimize postoperative swelling. A classic preauricular incision or a root of helix inter tragus notch incision (RHITNI) was used. RHITNI is a modification of the classical endaural incision, marked from the inferior border of the root of the helix into the crux, performing a V shape following the inferior border of the tragus, to finish in the ear notch. This incision allows complete anatomic control during surgery, adequate surgical exposure, low risks in damaging nerve structures, reduced need for vessels ligature, and more satisfactory cosmetic results when compared to the classic preauricular or endaural approaches. The discectomy was performed preserving condyle and temporal fibrocartilage. No bandage or special care was performed after the surgery. No hair washing restrictions were recommended. rehabilitation program started 5 days after surgery with 9 sessions. Patients were seen on follow-up at 1-week, 15-days, 30-days, 90-days and then in 1-year intervals.
Statistical analysis
Data were analyzed using SPSS (v26) and GraphPad Prism (v9) software. The variables were expressed as the mean (± standard deviation (SD). The normality of data was verified for all tests. Student’s paired t-test was used for variables with normal distribution and Signed Ranks Test for variables without normal distribution. P < 0.05 was considered statistically significant.
Results
A total of 19 patients (between 30 and 70 years old), were included in this study (Table 2). Patients had a mean age of 51.05 ± 13.71 (mean ± SD) years, 18 of whom were female gender (95 %). Of the 19 patients, 11 were operated on the right TMJ and 8 on the left TMJ. All patients were classified as 3 or 4 in the Dimitroulis classification, corresponding to moderate or severe stages, respectively. The mean preoperative pain was 7.63 ± 1.89 (mean ± SD), MMO was 25.95 ± 10.27 mm (mean ± SD) and MT was 2.53 ± 0.77 (mean ± SD). The most common diagnosis was disc perforation. The mean follow-up time was 37.9 months (Table 2). There were no surgical or wound healing complications. The authors did not have to reoperate any joint after TMJ discectomy, however 2 patients reported contralateral pain (both with acute dislocated disc with reduction) and were treated with TMJ arthrocentesis. A comparison between preoperative and postoperative outcomes was performed. A normal distribution was found in the MMO data, contrary to the MT and VAS outcomes. After an average of 37.9 months of follow-up time, a statistically significant improvement of pain, MMO and MT was observed (Table 3). The proportion of the patients that showed a good and acceptable outcome was eighty and nine percent (89 %) and six percent (6 %), respectively. Six percent (6 %) was classified as failure (Table 4).
Discussion
This centenary technique, firstly described by Lanz in 1909, still be controversial. Until now, most of the studies are limited in short follow-up time. The patient behaviors after TMJ discectomy can contribute to different results across time and combined with preclinical trials results, can provide a distrustful mood of TMJ surgeons with a difficult decision regarding disc removal. The present prospective study with 19 patients, investigated the effect of unilateral TMJ discectomy preserving condyle and temporal fibrocartilage, on pain, MMO and MT strictly in patients with unilateral disc perforation or fragmentation. In the last years, different reports have studied the role of TMJ discectomy. However, in most cases the inclusion criteria for these studies comprised dislocated disc with reduction or dislocated without reduction. Some studies have demonstrated dislocated disc with reduction or dislocated without reduction, have good results with mini-invasive techniques, such as TMJ arthrocentesis and TMJ arthroscopy, in agreement with the authors clinical practice. However, when the disc is damaged, TMJ discectomy seems to be an accepted approach. A recent study observed significative histopathological changes in the TMJ discs in cases of disc fragmentation or perforation. Those changes were mainly: (1) pre-fibrous sclerosis with myxoid degeneration; (2) collagen deposits; (3) increase in fibro-hyaline and fibrous tissues; (4) loss of elasticity; (5) scattered calcifications, and (6) synovial inflammation This article reinforces the importance of performing discectomy in disc fragmentation and perforation cases, as these alterations seems to be irreversible.
In our study, the median age of patients was 51 years, superior to other studies (mean ∼32−37 years), yet our age range was 30–70 years. In our experience, we did not observe signs of perforation or fragmentation in patiens under 30 years. Most studies assigned a Wilkes stage classification to all patients and predominantly included Wilkes III, IV, and V stage disease. However, Wilkes classification is mostly based on 2 TMD sub-types (internal derangement and osteoarthrosis), not covering all the possible sub-classifications known these days. In our study, we used the Dimitroulis classification, a more recent classification that include more TMD sub-classifications. The mean Dimitroulis score was ∼4 corresponding to “severe TMJ changes” with indication for TMJ discectomy as the mainstay treatment. The authors believe Dimitroulis category 4 could be comparable to Wilkes stage IV.
Our study showed a statistically significant reduction in pain, measured with VAS score (Table 3). In the last years, different studies reported also reduction in pain postdiscectomy. Eriksson, Westesson described that 50 of 52 patients operated had no/reduced pain (0-19/100). Likewise, Takaku et al. in 35 operated joints observed the absence of pain in 32 joints, and 3 joints presented mild pain. Nyberg et al. in a 5-years retrospective study verified only a reduction in pain on chewing, while pain at rest was not significantly changed. Bjørnland, Larheim observed no pain in 20 of 29 patients (69 %) after 3-years, and similar observations were made 10 years post-operatively.
Discectomy also had a positive effect on MMO (Table 3). MMO changed from a mean preoperative MMO of 25.95 mm (range 9–53 mm) to a postoperative of 40.74 mm (range 36−55 mm). Our results are similar to Miloro et al. and Bjørnland, Larheim.
We verified a significant improvement in MT postdiscectomy (Table 3). However, no data has been reported in the literature regarding this parameter after TMJ discectomy. High levels of MT in the masseter and temporalis muscles are correlated with TMD dysfunction and the evaluation of this parameter can be an important complement to determine the success of the surgery.
In this study, the global success rate of discectomy was 89 % (Table 4). This value is accordingly with other authors that obtained favourable results in 82–87 % of the patients.
Accordingly, to Bjørnland, Larheim, 3-years successful results after TMJ discectomy is a reliable predictor for a 10-year results, which can support the continuation of our results. Complications of TMJ surgery are uncommon but can have serious implications. In our study, we did not find surgical complications in the operated joint and the authors did not have to reoperate any patient. However, 2 patients reported contralateral pain during the follow-up period. Those patients were easily managed with TMJ arthrocentesis. In 2004, Nyberg et al., in a retrospective study, observed in 15 patients submitted to unilateral TMJ discectomy an 87 % success rate in 5 years follow-up and no contralateral changes. On the contrary, Eriksson, Westesson despite reporting a good outcome in 85 % of the 64 patients submitted to bilateral and unilateral TMJ discectomy, they reported a 5% reoperation rate, and in 8%, they operated the contralateral side. In the imaging analysis, they also observed that more than 90 % of the patients had condyle osteophytes/flattening or sclerosis without association with patients’ symptoms. We did not evaluate imaging changes in this study. In a preclinical trial conducted in black Merino sheep, the authors observed significant imaging and histologic changes after bilateral TMJ discectomy. Those results were obtained in previous healthy joints with preserved fibrocartilage. The authors did not find any functional changes, neither in rumination or mastication. Discussion can be made, rather bilateral discectomy can have worst outcome, compared to unilateral surgery. Also, the fibrocartilage condition, specially after discectomy, can probably be important to maintain the joint integrity. All these points remain poorly understood, and unfortunately this work is of little value to clarify these concerns.
From a clinical perspective, TMJ tissue engineering remains a great opportunity for investigators to join efforts to find an effective and safe TMJ disc substitute. That difficult path must be meticulous to avoid precipitated decisions that could compromise patient’s health. In fact, failures from the past, as the example of Proplast-Teflon interposal material have demonstrated, we need to be careful in decisions regarding TMJ disc substitution. It is expected that in the coming years, with the evolution of tissue engineering, the disc replacement may be a reality. However, in this moment, in the presence of a damaged disc, discectomy without interposal material seems to be superior to any interposal material in the joint. Some promising preclinical studies have demonstrated the possible role of a new interposal material to protect the condyle and fossa from degenerative changes after TMJ discectomy.
The results of this study should be a reminder for TMJ surgeons to make an effort to record patient data in the long-term and share those results to ensure a close understanding of the effect of surgical interventions. Future long-term research, that analyze joint sound, imaging, or specific questionnaires can give more robust data regarding this topic. We strongly recommend other surgeons to study more variables to increase knowledge. Moreover, it seems important in future studies to ensure an independent element to record the outcomes. A more significant sample size will also reinforce the results obtained in this article.
With this prospective study the authors conclude, currently, unilateral TMJ discectomy without interposal material, preserving the condyle and fossa fibrocartilage in patients with unilateral disc perforation or fragmentation seems to be an optimal technique.
Authors: David Faustino Ângelo, David Sanz, Henrique José Cardoso
References:
- Jivnani HM, Tripathi S, Shanker R, Singh BP, Agrawal KK, Singhal R. A study to determine the prevalence of temporomandibular disorders in a young adult population and its association with psychological and functional occlusal parameters. J Prosthodont 2019;28:e445–9.
- Janal MN, Raphael KG, Nayak S, Klausner J. Prevalence of myofascial temporomandibular disorder in US community women. J Oral Rehabil 2008;35:801–9.
- Bertoli FMP, Bruzamolin CD, Pizzatto E, Losso EM, Brancher JA, de Souza JF. Prevalence of diagnosed temporomandibular disorders: a cross-sectional study in Brazilian adolescents. PLoS One 2018;13:e0192254.
- Feteih RM. Signs and symptoms of temporomandibular disorders and oral parafunctions in urban Saudi Arabian adolescents: a research report. Head Face Med 2006;2, 25-25.
- Dimitroulis G. The role of surgery in the management of disorders of the temporomandibular joint: a critical review of the literature. Part 2. Int J Oral Maxillofac Surg 2005;34:231–7.
- Eriksson L, Westesson PL. Long-term evaluation of meniscectomy of the temporomandibular joint. J Oral Maxillofac Surg 1985;43:263–9.
- Ângelo DF, Morouc¸ o P, Monje Gil F, Mónico L, González-Gárcia R, Sousa R, et al. Preclinical randomized controlled trial of bilateral discectomy versus bilateral discopexy in Black Merino sheep temporomandibular joint: TEMPOJIMS - Phase 1- histologic, imaging and body weight results. J Craniomaxillofac Surg 2018;46:688–96.
- Ângelo DF, Gil FM, González-García R, Mónico L, Sousa R, Neto L, et al. Effects of bilateral discectomy and bilateral discopexy on black Merino sheep rumination kinematics: TEMPOJIMS - phase 1 - pilot blinded, randomized preclinical study. J Craniomaxillofac Surg 2018;46:346–55.
- Wang HL, Liu H, Shen J, Zhang PP, Liang SX, Yan YB. Removal of the articular fibrous layers with discectomy leads to temporomandibular joint ankylosis. Oral Surg Oral Med Oral Pathol Oral Radiol 2019;127:372–80.
- Widmark G, Gröndahl HG, Kahnberg KE, Haraldson T. Radiographic morphology in the temporomandibular joint after diskectomy. Cranio 1996;14:37–41.
- Holmlund A, Lund B, Weiner CK. Discectomy without replacement for the treatment of painful reciprocal clicking or catching and chronic closed lock of the temporomandibular joint: a clinical follow-up audit. Br J Oral Maxillofac Surg 2013;51:e211–214.
- Bjørnland T, Larheim TA. Discectomy of the temporomandibular joint: 3-year follow-up as a predictor of the 10-year outcome. J Oral Maxillofac Surg 2003;61:55–60.
- Miloro M, Henriksen B. Discectomy as the primary surgical option for internal derangement of the temporomandibular joint. J Oral Maxillofac Surg 2010;68:782–9.
- Miloro M, McKnight M, Han MD, Markiewicz MR. Discectomy without replacement improves function in patients with internal derangement of the temporomandibular joint. J Craniomaxillofac Surg 2017;45:1425–31.
- Takaku S, Toyoda T. Long-term evaluation of discectomy of the temporomandibular joint. J Oral Maxillofac Surg 1994;52:722–6.
- Silver CM. Long-term results of meniscectomy of the temporomandibular joint. CRANIO® 1985;3:46–57.
- Eriksson L, Westesson PL. Discectomy as an effective treatment for painful temporomandibular joint internal derangement: a 5-year clinical and radiographic follow-up. J Oral Maxillofac Surg 2001;59:750–8, discussion 758-759.
- Ellis OG, Tocaciu S, McKenzie DP, McCullough MJ. Dimitroulis G. Risk factors associated with poor outcomes following temporomandibular joint discectomy and fat graft. J Oral Maxillofac Surg 2021.
- Renapurkar SK. Discectomy versus disc preservation for internal derangement of the temporomandibular joint. Oral Maxillofac Surg Clin North Am 2018;30:329–33.
- Schiffman EL, Ohrbach R, Truelove EL, Tai F, Anderson GC, Pan W, et al. The Research Diagnostic Criteria for Temporomandibular Disorders. V: methods used to establish and validate revised Axis I diagnostic algorithms. J Orofac Pain 2010;24:63–78.
- Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet J-P, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache 2014;28:6–27.
- Agha R, Abdall-Razak A, Crossley E, Dowlut N, Iosifidis C, STROCSS Mathew G. Guideline: strengthening the reporting of cohort studies in surgery. Int J Surg 2019;2019(72):156–65.
- Ângelo DF. A letter to the editor on “Root of helix inter tragus notch incision (RHITNI) for temporomandibular open surgery”. Int J Surg 2020;83:233–4.
- Dimitroulis G. A new surgical classification for temporomandibular joint disorders. Int J Oral Maxillofac Surg 2013;42:218–22.
- Ângelo DF, Sousa R, Pinto I, Sanz D, Gil FM, Salvado F. Early magnetic resonance imaging control after temporomandibular joint arthrocentesis. Ann Maxillofac Surg 2015;5:255–7.
- Lanz W. Discitis mandibularis. Zentralbl Chir 1909;36:289–94.
- Garrigós-Pedrón M, Elizagaray-García I, Domínguez-Gordillo AA,
- Del-Castillo-Pardo-de-Vera JL, Gil-Martínez A. Temporomandibular disorders: improving outcomes using a multidisciplinary approach. J Multidiscip Healthc 2019;12:733–47.
- Nyberg J, Adell R, Svensson B. Temporomandibular joint discectomy for treatment of unilateral internal derangements–a 5 year follow-up evaluation. Int J Oral Maxillofac Surg 2004;33:8–12.
- Takaku S, Sano T, Yoshida M. Long-term magnetic resonance imaging after temporomandibular joint discectomy without replacement. J Oral Maxillofac Surg 2000;58:739–45.
- Carvajal WA, Laskin DM. Long-term evaluation of arthrocentesis for the treatment of internal derangements of the temporomandibular joint. J Oral Maxillofac Surg 2000;58:852–5.
- Nishimura M, Segami N, Kaneyama K, Suzuki T. Prognostic factors in arthrocentesis of the temporomandibular joint: Evaluation of 100 patients with internal derangement. J Oral Maxillofac Surg 2001;59:874–7.
- [32] Dimitroulis G, Dolwick MF, Martinez A. Temporomandibular joint arthrocentesis and lavage for the treatment of closed lock: a follow-up study. Br J Oral Maxillofac Surg 1995;33:23–7.
- [33] Murakami K. Current role of arthrocentesis, arthroscopy and open surgery for temporomandibular joint internal derangement with inflammatory/degenerative disease; -pitfalls and pearls. J Oral Maxillofac Surg Med Pathol 2021.
- Indresano AT. Surgical arthroscopy as the preferred treatment for internal derangements of the temporomandibular joint. J Oral Maxillofac Surg 2001;59:308–12.
- González-García R, Rodríguez-Campo FJ. Arthroscopic lysis and lavage versus operative arthroscopy in the outcome of temporomandibular joint internal derangement: a comparative study based on Wilkes stages. J Oral Maxillofac Surg 2011;69:2513–24.
- Breik O, Devrukhkar V, Dimitroulis G. Temporomandibular joint (TMJ) arthroscopic lysis and lavage: Outcomes and rate of progression to open surgery. J Craniomaxillofac Surg 2016;44:1988–95.
- Murakami K, Segami N, Okamoto M, Yamamura I, Takahashi K, Tsuboi Y. Outcome of arthroscopic surgery for internal derangement of the temporomandibular joint: long-term results covering 10 years. J Craniomaxillofac Surg 2000;28:264–71.
- Guarda Nardini L, Meneghini M, Guido M, Baciorri F, Manfredini D. Histopathology of the temporomandibular joint disc: findings in 30 samples from joints with degenerative disease. J Oral Rehabil 2021;48:1025–34.
- Wilkes CH. Internal derangements of the temporomandibular joint. Pathological variations. Arch Otolaryngol Head Neck Surg 1989;115:469–77.
- Silveira A, Gadotti IC, Armijo-Olivo S, Biasotto-Gonzalez DA, Magee D. Jaw dysfunction is associated with neck disability and muscle tenderness in subjects with and without chronic temporomandibular disorders. Biomed Res Int 2015;2015:512792.
- Estabrooks LN, Fairbanks CE, Collett RJ, Miller L. A retrospective evaluation of 301 TMJ Proplast-Teflon implants. Oral Surg Oral Med Oral Pathol 1990;70:381–6.
- Berarducci JP, Thompson DA, Scheffer RB. Perforation into middle cranial fossa as a sequel to use of a Proplast-Teflon implant for temporomandibular joint reconstruction. J Oral Maxillofac Surg 1990;48:496–8.
- Kulber DA, Davos I, Aronowitz JA. Severe cutaneous foreign body giant cell reaction after temporomandibular joint reconstruction with Proplast-Teflon. J Oral Maxillofac Surg 1995;53:719–22, discussion 722-713.
- Hartman LC, Bessette RW, Baier RE, Meyer AE, Wirth J. Silicone rubber temporomandibular joint (TMJ) meniscal replacements: postimplant histopathologic and material evaluation. J Biomed Mater Res 1988;22:475–84.
- Dimitroulis G. A critical review of interpositional grafts following temporomandibular joint discectomy with an overview of the dermis-fat graft. Int J Oral Maxillofac Surg 2011;40:561–8.
- Ângelo DF, Wang Y, Morouc¸ o P, Monje F, Mónico L, González-Garcia R, et al. A randomized controlled preclinical trial on 3 interposal temporomandibular joint disc implants: TEMPOJIMS-Phase 2. J Tissue Eng Regen Med 2021;15:852–68.
