Middle mesial canals in mandibular first molars: A micro-CT study in different populations
Abstract
Objective: To describe the morphological aspects of middle mesial canals (MMC) in mandibular first molars using micro-CT.
Design: Mandibular first molars collected from the Brazilian (n = 136) and Turkish (n = 122) populations were scanned (voxel size: 9.9 µm) and mesial roots with MMC (n = 48) evaluated regarding several morphological aspects. The incidence of MMC in each population was statistically compared using Chi-square test (α = 0.05).
Results: Overall, the incidence of MMC was 18.6% (48 out of 258 molars) and was significantly higher in the Brazilian (n = 30; 22.1%) than in the Turkish (n = 18; 14.8%) population (p < 0.05). In both populations, confluent configuration of the MMC was the most frequent anatomy. Most of the specimens with MMC had 3 independent orifices (n = 26; 54.2%) and 3 apical foramina (n = 21; 43.8%). The mean minor diameter of the MMC orifice (0.16 mm) was 3 times less than the other orifices (~0.50 mm). In mesial roots with independent configuration (n = 3; 6.3%), the mean volumes (mm3) of the MMC, mesiobuccal (MBC) and mesiolingual (MLC) canals were 0.20 0.10, 0.75 0.28, and 0.88 0.19, respectively. In the specimens with canal confluence (n = 26; 54.2%), MMC merged to the MBC (n = 8; 16.7%), MLC (n = 4; 8.3%), or to both MBC and MLC (n = 14; 29.2%). Double mesial canal was observed in only 1 specimen. MMC with an independent foramen was observed mostly in Brazilian specimens.
Conclusions: Incidence of MMC was higher in the Brazilian molars. Confluent configuration was the most prevalent anatomic variation, while independent and fin configurations, as well as, double MMC, were found only in a few specimens.
Introduction
The main goal of endodontic therapy is to prevent or heal apical periodontitis. Unfortunately, cleaning and shaping procedures are adversely affected by the highly variable root canal anatomy. The presence of additional canals needs to be recognized in order to avoid incomplete instrumentation and the preservation of bacteria and their toxins, which can compromise the outcome of the root canal treatment. Therefore, the knowledge of the internal anatomy of teeth is a prerequisite for successful endodontic therapy (Vertucci, 1984).
The mesial root of mandibular molars commonly presents 1 mesiobuccal (MBC) and 1 mesiolingual (MLC) canals; however, other anatomical configurations have also been reported in the literature (de Pablo, Estevez, Peix Sanchez, Heilborn, & Cohenca, 2010). In 1974 , Barker, Parsons, Mills and Williams (1974) and Vertucci and Williams (1974) were the first authors to demonstrate the presence of an extra and independent canal in the mesial root of mandibular molars using the clearing technique. Later, Pomeranz, Eidelman, and Goldberg (1981) presented a comprehensive in vivo study describing its morphology and clinical management. Since then, several authors have reported this anatomical variation which has been termed intermediate canal (Fabra-Campos,1989), mesio-central canal (Navarro, Luzi, Garcia, & Garcia, 2007), third mesial canal (Holtzmann, 1997), accessory mesial canal (Karapinar-Kazandag, Basrani, & Friedman, 2010), and middle mesial canal (MMC) (Pomeranz et al., 1981; Azim, Deutsch, & Solomon, 2015; Baugh & Wallace, 2004; Bond, Hartwell, Donnelly, & Portell, 1988; Nosrat, Deschenes, Tordik, Hicks, & Fouad, 2015). In the literature, this anatomical variation has been found in a percentage frequency ranging from 0.26% (Kim, Kim, Woo, & Kim, 2013) to 46.15% (Azim et al., 2015).
In recent years, micro-computed tomographic imaging (micro-CT) has gained increasing significance in the study of hard tissues in endodontics as it offers a reproducible 3D technique for the assessment of the root canal anatomy (Leoni, Versiani, Pécora, & Sousa-Neto, 2014; Ordinola-Zapata et al., 2013). Using this technology, Harris, Bowles, Fok, and McClanahan, (2013) found the presence of more than 2 canals along any point of the mesial root in 8 out of 22 mandibular molars (36.3%). Currently, endodontic literature lacks a detailed morphological description of the anatomy of the MMC in mandibular molars. Thus, the aim of this study was to describe the morphological aspects of the MMC in mandibular first molars collected from the Brazilian and Turkish populations, using micro-CT imaging system.
Materials and methods
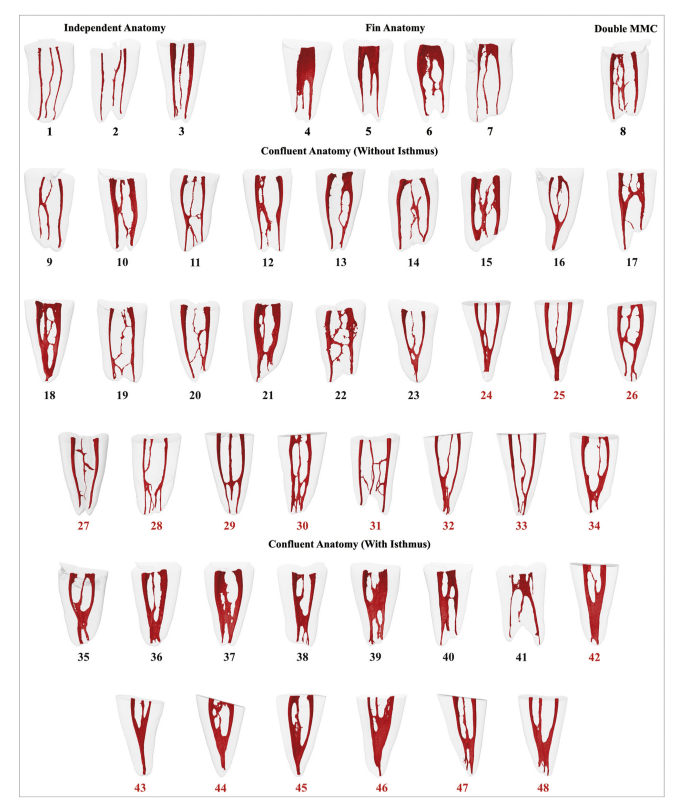
After ethics committee approval (protocol #2013/145), 258 two-rooted mandibular first molars, collected from Brazilian (n = 136) and Turkish (n = 122) populations, were selected and scanned in a micro-CT device (SkyScan 1172; Bruker-microCT, Kontich, Belgium), at 100 kV, 100 µA and an isotropic voxel size of 9.9 µm. The gender and age of the patients were unknown, and teeth were extracted for reasons not related to this study. Scanning procedure was performed through 180◦ rotation around the vertical axis, with a rotation step of 0.4◦, using a 0.5-mm-thick aluminium filter. After the reconstruction of the acquired projection images into cross-sections slices (NRecon v.1.6.9; Bruker-microCT), polygonal surface representations of the internal anatomy of mesial roots presenting MMC were obtained (Fig. 1) (CTAn v.1.14.4; Bruker-microCT) and classified according to Pomeranz et al. (1981) into:
- Independent: three independent canals extend from the pulp chamber to the apex;
- Fin: in the coronal third, MMC orifice is connect to the MBC and/ or MLC orifice(s) by a groove, but the mesial canals leave the root in 3 separate foramina;
- Confluent: MMC leaves the pulp chamber, separately or not to the other mesial canals, and joins the MBC and/or MLC by transverse anastamosis, intercanal connections or isthmus during its trajectory to the apical foramen.
The number and percentage frequency distribution of different root canal configurations was calculated. The incidence of MMC in each population was statistically compared using Chi-square test with a significance level set at 5% (SPSS v11.0 for Windows; SPSS Inc., Chicago, IL, USA). Additionally, the following analyses were performed using CTAn v.1.14.4 software (Bruker-microCT): (1) number, configuration (independent or confluent), and distance of the mesial canal orifices 1.5 mm coronal to the furcation; (2) length and depth (in mm) of the orifice confluence; (3) minor and major diameters (in mm) of the independent orifices; (4) width of dentin (in mm) toward the furcation side in relation to the MMC orifice; (5) distance (in mm) from the orifice level to the confluence of the MMC to the other mesial canals; (7) volume (in mm3) of the MMC, MBC and MLC in mesial roots with independent configuration; and (8) number of foramina.
Results
Table 1 summarizes the number and percentage frequency distribution of different root canal configurations in 48 mandibular first molars with MMC. Overall, the incidence of MMC was 18.6% (48 out of 258 mandibular first molars) and was significantly higher in the Brazilian (n = 30; 22.1%) than in the Turkish (n = 18; 14.8%) population (p < 0.05). Confluent anatomy was the most frequent anatomical variation comprising 73.3% (n = 22) and 100% (n = 18) of the Brazilian and Turkish molars with MMC, respectively. Among this group of teeth, isthmus was observed in 29.2% of the sample (n = 14). Independent (n = 3) and fin (n = 4) anatomies were observed only in the Brazilian specimens, as well as, a double MMC (n = 1).
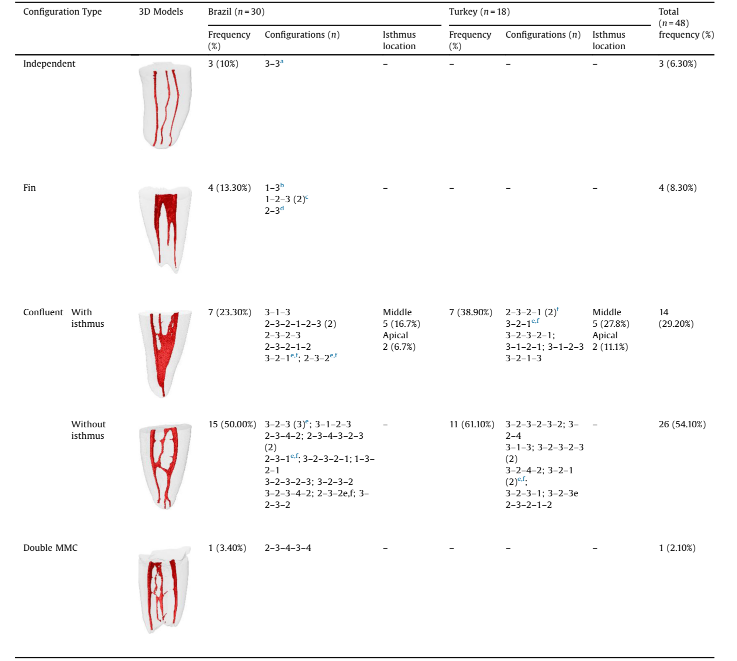
Table 2 shows some morphological aspects of the root canal system of mandibular first molars with MMC (n = 48). Overall, most of the specimens had 3 independent orifices (n = 26; 54.2%) and 3 apical foramina (n = 21; 43.8%). The presence of mesial grooves were more frequent in the Brazilian (n = 17; 56.6%) than in the Turkish (n = 5; 27.8%) molars. MMC orifice was confluent to MBC (n = 10; 20.8%), MLC (n = 8; 16.7%) and both MBC and MLC (n = 14; 8.3%) orifices in 22 out of 48 mesial roots. In specimens with 3 independent orifices (n = 26; 54.2%), the mean minor diameter of the MMC, MBC and MLC orifices were 0.16, 0.46 and 0.50 mm, respectively, while the major diameter were 0.40, 0.71 and 0.78 mm, respectively. Overall, the diameter of the MMC orifice was 2–3 times less than the other orifices. In the specimens with canal confluence (n = 26; 54.2%), MMC merged to the MBC (n = 8; 16.7%), MLC (n = 4; 8.3%), or to both MBC and MLC (n = 14; 29.2%) in its pathway within the root canal system. In mesial roots with independent configuration (n = 3; 6.3%), the mean volume of the MMC, MBC and MLC was 0.20 ± 0.10, 0.75 ± 0.28, and 0.88 ± 0.19 mm3, respectively.
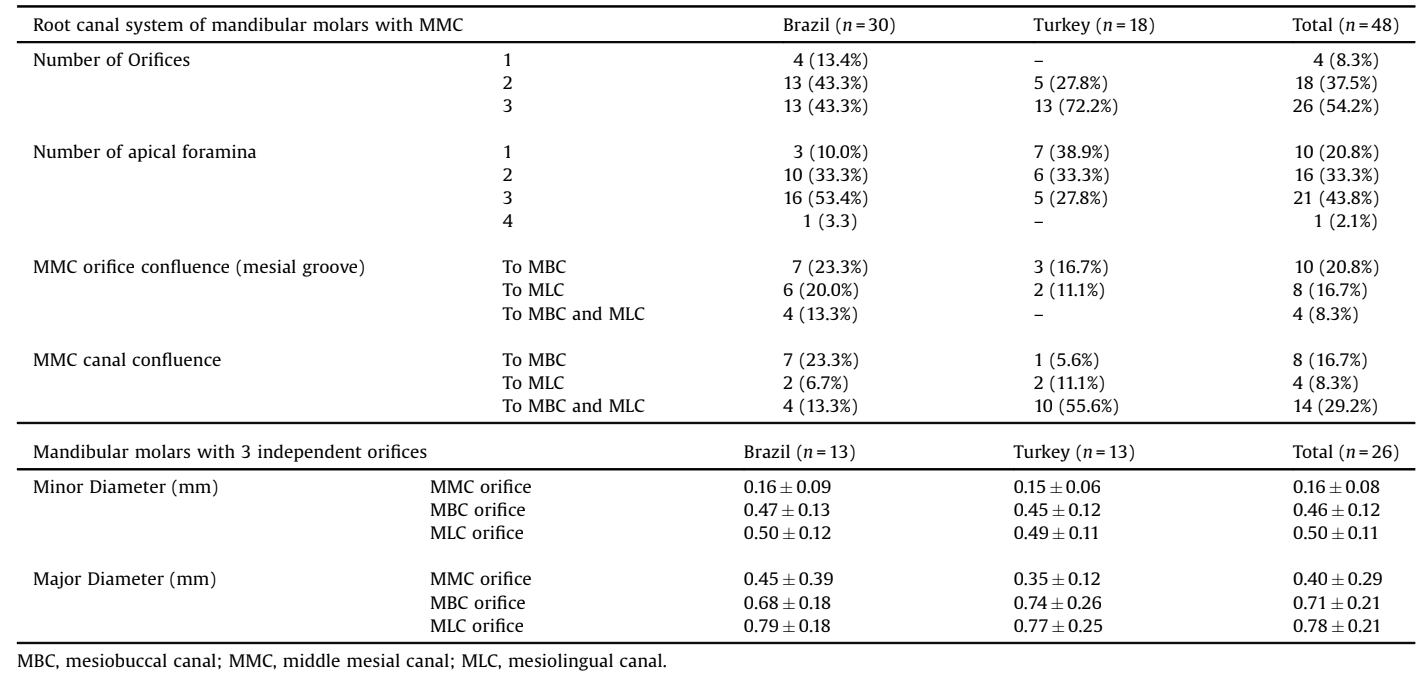
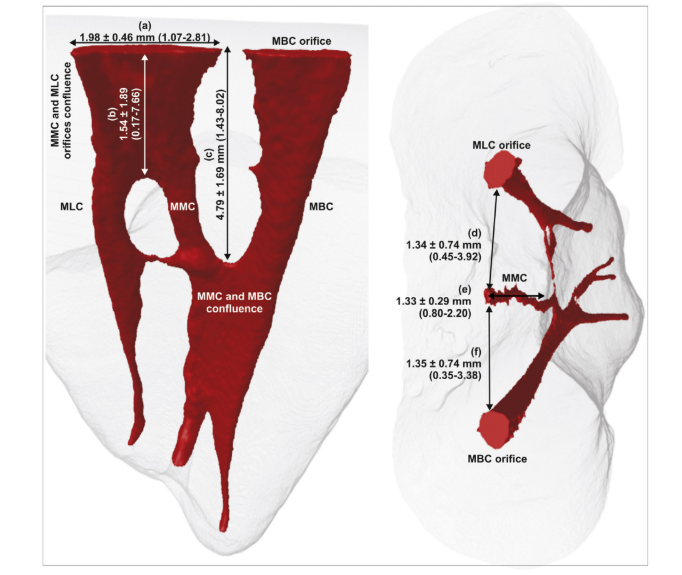
Fig. 2 illustrates the mean distances and range of values (in mm) between some anatomical landmarks and the MMC of mandibular first molars. In the teeth with orifice confluence (n = 22; 45,8%), mean length and depth of the mesial groove were 1.98 0.46 mm (range 1.07–2.81 mm) and 1.54 ± 1.89 mm (range 0.17–7.66), respectively. The distance (in mm) from the orifice to the canal confluence ranged from 1.43 to 8.02 mm. In the specimens with independent orifices (n = 26; 54.2%), MMC orifice was found at the same mean distance from the MBC and MLC orifices, while the width of dentin (in mm) toward the furcation side in relation to the MMC orifice was 1.33 ± 0.29 mm (range 0.80–2.20).
Discussion
The presence of a third canal in the mesial root of mandibular first molars, known as middle mesial canal (MMC) was identified in 20 ex vivo (Vertucci, 1984; Barker et al., 1974; Vertucci & Williams, 1974; Navarro et al., 2007; Karapinar-Kazandag et al., 2010; Harris et al., 2013; Ahmed, Abu-Bakr, Yahia, & Ibrahim, 2007; Shahi, Yavari, Rahimi, & Torkamani, 2008; Çalişkan, Pehlivan, Sepetçiog˘lu, Türkün, & Tuncer, 1995; de Carvalho & Zuolo, 2000; Gulabivala, Aung, Alavi, & Ng, 2001; Sert, Aslanalp, & Tanalp, 2004; Villegas, Yoshioka, Kobayashi, & Suda, 2004; Peiris, Pitakotuwage, Takaha- shi, Sasaki, & Kanazawa, 2008; Al-Qudah & Awawdeh, 2009; Chen, Yao, & Tong, 2009; Gu et al., 2010; Gulabivala, Opasanon, Ng, & Alavi, 2002; Wasti, Shearer, & Wilson, 2001) (Table 3) and 6 in vivo (Pomeranz et al., 1981; Fabra-Campos, 1989; Azim et al., 2015; Nosrat et al., 2015; Kim et al., 2013; Goel, Gill, & Taneja, 1991) (Table 4) studies, accounting for more than 5220 mesial roots. Clearing and radiographic techniques were used in most of these studies, and the reported incidence of MMC ranged from 0.82% to 37.5%. Undoubtedly, the conventional methodological approaches in these studies have been successfully used over many decades providing useful information to the clinicians about the internal anatomy of the teeth. However, inherent limitations repeatedly discussed in the endodontic literature regarding their lack of accuracy in detecting extra canals, encouraged the search for newer methodologies that could potentially surpass the anatomical challenges that the human dentition exhibits. Therefore, despite considerable amount of information regarding MMC has been published to date, very little information exists regarding its morphology using highly accurate contemporary non-destructive methodology such as the micro-CT imaging system used in the present study.
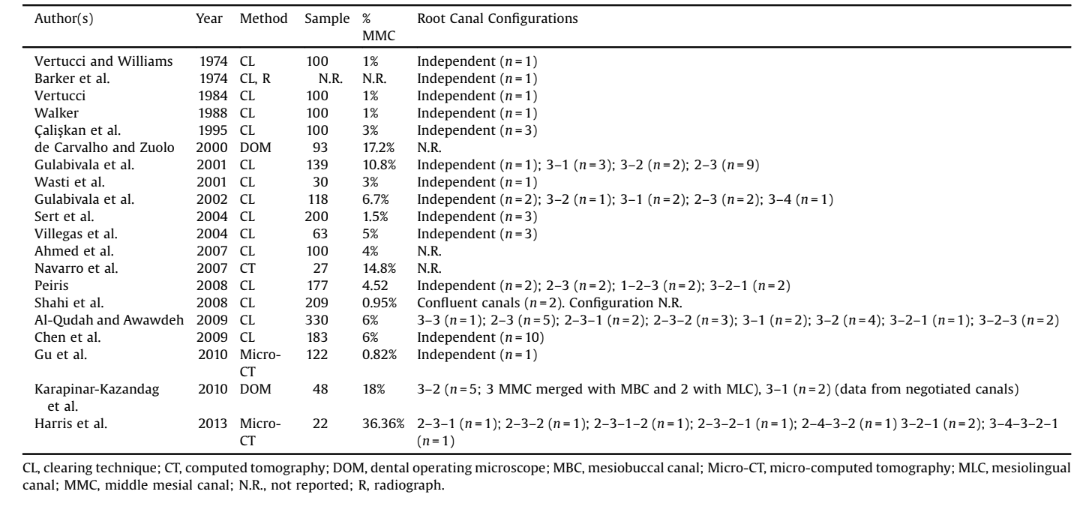
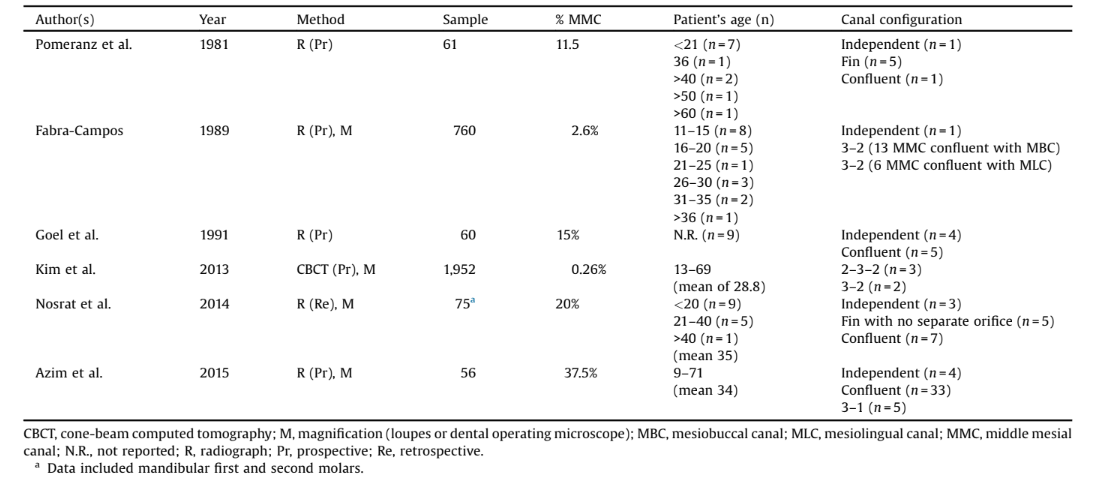
In this scenario, particular attention must be paid to the dissimilar incidences of MMC reported in the aforementioned studies (0.82–37.5%), which have been explained through diversity in sample size, study design, and/or racial factors (de Pablo et al., 2010; Nosrat et al., 2015; Kim et al., 2013; Walker, 1988; Sert et al., 2004; Al-Qudah & Awawdeh, 2009; Gu et al., 2010). Regarding the latter, studies concur that ethnicity is a predisposing factor for anatomical variations such as number of roots, but they failed to demonstrate any direct relationship between ethnicity and configuration of the root canal system (de Pablo et al., 2010). A recent study found a significant difference in the incidence of MMC between whites (12.2%) and nonwhites (29.4%) patients, but not regarding the ethnicity (Nosrat et al., 2015). In the present study, the significant difference in the incidence of MMC in the Brazilian (n = 30; 22.1%) and Turkish (n = 18; 14.8%) populations suggests that MMC in mandibular first molars may be race-related. It is worth to mention an importance aspect when evaluating less common anatomic variations (Al-Qudah & Awawdeh, 2009), which is the detailed morphological analysis of a large number of mandibular first molars with MMC (n = 48), when compared to previous anatomical investigations on this subject (Tables 3 and 4). However, Brazilian and Turkish populations may present a genetic variability because of the coexistence of multiple ethnicities. Therefore, these results must be taken with caution as larger populations of known ethnic backgrounds are needed to achieve an adequate statistical power for genetic association (Hong & Park, 2012).
Some authors support the view that MMC canals can be easily located in patients of a younger age group, but progressively decrease its incidence with age (Table 4) (Pomeranz et al., 1981; Fabra-Campos, 1989; Azim et al., 2015; Nosrat et al., 2015; Kim et al., 2013; Goel et al., 1991). It has been also postulated that, during the growth of the root, the connective pulp tissue is compressed by the accumulation of secondary dentin, which would form vertical dentinal partitions inside the root canal cavity, thus creating 3 mesial root canals (Pomeranz et al., 1981; Peiris et al., 2008). Though, considering that these hypotheses were not proven by an experiment, it is also possible that some of the anatomical variations found herein, such as the confluent anatomy without isthmus (Fig. 1), are not age-related changes, but instead they are natural canal configurations.
In the literature, 3 main morphological aspects of MMC regarding its relation to the other main root canals in the mesial root of mandibular molars have been described as independent, fin and confluent anatomies (Pomeranz et al., 1981). From a clinical standpoint, this classification system is very useful; however, it is of limited depth considering the huge amount of variations in the anatomy of the MMC (Fig. 1). In this way, in this study the confluent anatomy was subdivided into with or without isthmus. Unfortunately, the limitations of conventional tools in studying certain features of the root canal system are prone to a wide range of interpretation (Peiris et al., 2008). For instance, in clinical practice a thin and deep groove may be confounded with an extra root canal which help to explain the high incidence of MMC (37.5%) recently reported in an in vivo study using dental operating microscope (Azim et al., 2015). In this way, non-destructive micro-CT technology can allow the development of accurate 3D models of the internal anatomy and assist in obtaining quantitative morphometric data that are impossible to acquire using conventional methodologies such as clearing, radiography or sectioning techniques. Nevertheless, as any other methodological approach, micro-CT technology has also limitations: (i) scanning and reconstruction procedures take considerable time; (ii) the technique is not suitable for clinical use; (iii) the equipment is quite expensive; and (iv) the complexity of the technical procedures requires a high learning curve and an in-depth knowledge of dedicated software.
Improvements in the digital imaging systems have also enabled in vivo evaluation of the root canal anatomy using non-destructive methods, such as cone-beam computed-tomography (CBCT). CBCT has been proved to be a more accurate and precise imaging tool for detecting extra canals than conventional periapical radiograph. Kim et al. (2013) used this technology to evaluate 1952 mandibular first molars from 976 patients and found only 2 teeth with MMC (0.26%). This low incidence can be explained because CBCT systems hampered by insufficient spatial resolution and slice thickness for detecting more complex anatomical configurations in which fine ramifications are present. In contrast, micro-CT provides a better assessment of fine anatomical structures because of the possibility of using a higher exposure time and lower voxel sizes than CBCT during the scanning procedures. However, to date, only 2 ex vivo studies aimed to evaluate the incidence of MMC in mandibular molars using micro-CT technology. Gu et al. (2010) evaluated 122 mandibular molars from native Chinese population and found only 1 teeth (0.82%) with 3 independent root canals in the mesial root, while Harris et al. (2013) reported the presence of MMC in 36.36% of their sample, which was higher than in the present study (18.6%; 48 out of 258 mandibular first molars); however, the limited sample size (n = 22) of that study reduces the impact of the results (Harris et al., 2013).
MMC orifice is often hidden by a dentinal projection of the mesial aspect of pulp chamber walls making its detection challenging (Karapinar-Kazandag et al., 2010). In order to find MMC orifice, this dentin projection must be carefully removed under a better illumination and magnification (Karapinar-Kazandag et al., 2010; de Carvalho & Zuolo, 2000), using ultrasound tips (Kontakiotis & Tzanetakis, 2007) or long shank rounded burs (Nosrat et al., 2015). In the present study, MMC orifice was found to be in a developmental groove between the MBC and MLC in 22 specimens (45.8%). In contrast to the literature, in which MMC orifice was detected closer to the MLC (Karapinar-Kazandag et al., 2010), a higher incidence of confluence to the MBC in both populations (n = 10; 20.8%) was observed herein (Table 2). Clinically speaking, an extensive exploration of the grooves between mesial orifices has been a significant factor for accessing additional root canals (Karapinar-Kazandag et al., 2010; Azim et al., 2015). However, the length (1.07–2.81 mm) and depth (0.17– 7.66 mm) of this groove must be taken into consideration during its troughing because of the small dentin thickness toward the furcation side in relation to the MMC orifice (0.80–2.20 mm), which increases the risk of root perforation (Karapinar-Kazandag et al., 2010; Azim et al., 2015). Thus, it would be advisable that clinicians use less tapered instruments during MMC preparation in order to avoid excessive dentin removal (Azim et al., 2015).
In accordance with previous studies (Tables 3 and 4), the analysis of the pathway of the MMC showed that it merged to the other mesial canals in a high percentage of the sample (73.3% and 100% of the Brazilian and Turkish mandibular molars, respectively), in a distance from the orifice level that ranged from 1.43 to 8.02 mm. The variety of canal morphologies observed herein also included 1 molar with a double MMC among the Brazilian molars. To date, quite a few studies have reported this anatomical variation in the mesial root of mandibular molars (Goel et al., 1991; Kontakiotis & Tzanetakis, 2007).
In clinical practice, while preparation and disinfection of independent and fin anatomies are relatively easy, branched canal configurations and intercanal ramifications, such as in the confluent anatomy, may render complete debridement of canal system difficult. Because mechanical instrumentation of these areas is unfeasible, our efforts should concentrate on efficient delivery and activation of irrigants to achieve proper disinfection (de Pablo et al., 2010; Gulabivala et al., 2001) avoiding subsequent need for retreatment or surgical intervention. If surgery becomes necessary in roots with MMC, the natural anatomy is altered, and additional anatomic features such as undebrided isthmus, transverse anastomoses, lateral connections or multiple foramina need to be addressed (Leoni et al., 2014). In this way, surgical microscope (Karapinar-Kazandag et al., 2010; Azim et al., 2015; Nosrat et al., 2015; Kim et al., 2013; de Carvalho & Zuolo, 2000) and ultrasound (Reeh, 1998) would help clinicians to better visualize the apex, incorporating all canals and the isthmus into the root-end preparation to ensure complete debridement and sealing of the root canal system (Leoni et al., 2014).
Considering the limitations of the present study, the incidence of MMC was higher in the Brazilian molars. Confluent configuration was the most prevalent anatomic variation, while independent and fin configurations, as well as, double MMC, were found only in a few specimens.
Authors: Marco Aurélio Versiani, Ronald Ordinola-Zapata, Ali Keleş, Hatice Alcin, Clóvis Monteiro Bramante, Jesus Djalma Pécora, Manoel Damião Sousa-Neto
References:
- Çalişkan, M. K., Pehlivan, Y., Sepetçioğlu, F., Türkün, M., & Tuncer, S. S. (1995). Root canal morphology of human permanent teeth in a Turkish population. Journal of Endodontics, 21, 200–204.
- Ahmed, H. A., Abu-Bakr, N. H., Yahia, N. A., & Ibrahim, Y. E. (2007). Root and canal morphology of permanent mandibular molars in a Sudanese population. International Endodontic Journal, 40, 766–771.
- Al-Qudah, A. A., & Awawdeh, L. A. (2009). Root and canal morphology of mandibular first and second molar teeth in a Jordanian population. International Endodontic Journal, 42, 775–784.
- Azim, A. A., Deutsch, A. S., & Solomon, C. S. (2015). Prevalence of middle mesial canals in mandibular molars after guided troughing under high magnification: an in vivo investigation. Journal of Endodontics, 41, 164–168.
- Barker, B. C., Parsons, K. C., Mills, P. R., & Williams, G. L. (1974). Anatomy of root canals. III. Permanent mandibular molars. Australian Dental Journal, 19, 408–413.
- Baugh, D., & Wallace, J. (2004). Middle mesial canal of the mandibular first molar: a case report and literature review. Journal of Endodontics, 30, 185–186.
