Flat-Oval Root Canal Preparation with Self-Adjusting File Instrument: A Micro–Computed Tomography Study
Abstract
Introduction: The aim of this study was to evaluate the root canal preparation in flat-oval canals treated with either rotary or self-adjusting file (SAF) by using micro-tomography analysis.
Methods: Forty mandibular incisors were scanned before and after root canal instrumentation with rotary instruments (n = 20) or SAF (n = 20). Changes in canal volume, surface area, and cross-sectional geometry were compared with preoperative values. Data were compared by independent sample t test and χ2 test between groups and paired sample t test within the group (α = 0.05).
Results: Overall, area, perimeter, roundness, and major and minor diameters revealed no statistical difference between groups (P > .05). In the coronal third, percentage of prepared root canal walls and mean increases of volume and area were significantly higher with SAF (92.0%, 1.44 ± 0.49 mm3, 0.40 ± 0.14 mm2, respectively) than rotary instrumentation (62.0%, 0.81 ± 0.45 mm3, 0.23 ± 0.15 mm2, respectively) (P < .05). SAF removed dentin layer from all around the canal, whereas rotary instrumentation showed substantial untouched areas.
Conclusions: In the coronal third, mean increases of area and volume of the canal as well as the percentage of prepared walls were significantly higher with SAF than with rotary instrumentation. By using SAF instruments, flat-oval canals were homogenously and circumferentially prepared. The size of the SAF preparation in the apical third of the canal was equivalent to those prepared with #40 rotary file with a 0.02 taper. (J Endod 2011;37:1002–1007)
The ultimate goal of chemomechanical preparation is to remove the inner layer of the dentin, while allowing the irrigant to reach the entire length of the root canal, eradicating bacterial populations or at least reducing them to levels that are compatible with periradicular tissue healing. Although many technical advances have been made in endodontics, canal preparation is still adversely influenced by the highly variable anatomy, especially in oval, flat, or curved root canals. In flat-oval canals, rotary files have failed to perform adequate cleaning and shaping, leaving untouched fins or recesses on the buccal and/or lingual aspects of the central canal area prepared by the instrument.
The self-adjusting file (SAF) (ReDent-Nova, Ra’anana, Israel) has been devised with the purpose of sidestepping some of the limitations of nickel-titanium (NiTi) rotary instruments. During its operation, the file is designed to adapt itself three-dimensionally to the shape of the root canal. Rather than machining a central portion of the root canal into a round cross section, the SAF is claimed to maintain a flat canal as a flat canal with slightly larger dimensions. Hence, SAF system has the potential to be particularly advantageous in promoting cleaning and shaping of flat-oval–shaped canals The development of x-ray micro–computed tomography (μCT) has gained increasing significance in the study of hard tissues. μCT offers a noninvasive reproducible technique for three-dimensional assessment of the root canal system and can be applied quantitatively as well as qualitatively. Recent ex vivo μCT studies showed that the percentage of root canal area affected by the SAF method is larger than that affected by popular rotary instrumentation systems in different teeth. To date, root canal preparation with SAF has been quantitatively and qualitatively described in different teeth, but not in mandibular incisors. Thus, the purpose of this study was to evaluate the root canal preparation in flat-oval root canals of mandibular incisors treated with either rotary or SAF by using three-dimensional μCT analysis.
Materials and Methods
Selection of Teeth
After ethics committee approval, 40 single-rooted freshly extracted human mandibular incisor teeth with fully formed apices were selected and stored in 9◦C aqueous 0.1% thymol solution until further use. Each root was radiographed in buccolingual and mesiodistal projections to categorize them and to detect any possible obstruction. When the buccolingual diameter was 4 or more times larger than that of the mesiodistal diameter, the canals were classified as flat-oval. All teeth presenting isthmus, lateral, accessory, apical curvature, or 2 canals were excluded from the study.
After being washed in running water for 24 hours, each tooth was dried, mounted on a custom attachment, and scanned in a desktop x-ray microfocus CT scanner (SkyScan 1174v2; SkyScan N.V., Kontich, Belgium) at an isotropic resolution of 19.7 mm. The system consisted of a sealed air-cooled x-ray tube, 20–50 kV/40W/800 mA, with a precision object manipulator with 2 translations and 1 rotation direction. The system also included a 14-bit charge-coupled device (CCD) camera based on a 1.3 megapixel (1304 × 1024 pixels) CCD sensor.
Teeth were accessed by using high-speed diamond burs, and patency of the coronal canal was confirmed. Coronal flaring was accomplished with #2 and #3 Gates Glidden burs (Dentsply Maillefer, Ballaigues, Switzerland), in a low-speed contra-angle handpiece, placed to 2–4 mm below the cementoenamel junction. Flaring was followed by irrigation with 5 mL of 2.5% NaOCl delivered in a syringe with a 27-gauge needle (Endo Eze; Ultradent Products Inc, South Jordan, UT). Subsequently, apical patency was determined by inserting a size 10 K-file into the root canal until its tip was visible at the apical foramen; working length (WL) was set 0.5 mm shorter of this measurement. A glide path was confirmed at least to a size #20 K-file. Specimens were then randomly assigned to 2 experimental groups (n = 20) according to the instrumentation technique: SAF (group A) and rotary (group B). Canals in group A were shaped by a general practitioner who had been specifically trained with the SAF instrument and in group B by a specialist (M.A.V.) with 12 years of clinical experience with rotary instruments.
Root Canal Preparation with SAF
A 1.5-mm diameter SAF (ReDent-Nova) was operated for 4 minutes by using a trans-line (in-and-out) vibrating handpiece (Gentle-Power Lux 20LP; KaVo, Biberach, Germany) adapted with a RDT3 head (ReDent-Nova) at a frequency of 83.3 Hz (5000 rpm) and amplitude of 0.4 mm. The instrument was used with a manual in-and-out motion to the WL. Continuous irrigation with 2.5% NaOCl was applied throughout the procedure at 5 mL/min by using a special irrigation apparatus (VATEA; ReDent-Nova).
Root Canal Preparation with Rotary Instruments
The coronal and middle thirds were serially enlarged with NiTi rotary instruments sizes #25, 0.12 taper, #25, 0.10 taper, and #25, 0.08 taper (K3; SybronEndo, West Collins, CA) in a crown-down manner by using gentle in-and-out motion toward the apex. Then, instruments of sizes #25, 0.02 taper, #25, 0.04 taper, #30, 0.02 taper, #30, 0.04 taper, #35, 0.02 taper, #35, 0.04 taper, and #40, 0.02 taper were used to the WL. To avoid fracture, 5 canals were instrumented with 1 set of instruments at the WL, which were driven by a torque-controlled motor (X-Smart; Dentsply Maillefer) set to 300 rpm. The instruments were withdrawn when resistance was felt and changed for the next instrument. Passive ultrasonic irrigation was performed between each instrument by using a size #20 K-file mounted on a piezoelectric handpiece (JetSonic Four; Gnatus, Ribeirão Preto, SP, Brazil) at a power setting of 3, which was activated for 10 seconds at the WL. Each canal was irrigated with a total of 20 mL of 2.5% NaOCl.
In all groups after root canal preparation, a final rinse with 5 mL of normal saline solution was performed, the root canals were dried with paper points, and teeth were resubmitted to a postoperative μCT scan by applying the initial parameter settings.
Evaluation of the Root Canal Preparation
Images were reconstructed from the apex to the level of the cementoenamel junction (NRecon v1.6.1.5; SkyScan), providing axial cross sections of the inner structure of the samples. For each tooth, evaluation was done for the full canal length in approximately 400 slices per specimen.
CTAn v1.10.1.0 software (Skyscan) was used for two- and three-dimensional volumetric analysis and measurements of area, perimeter, roundness, major diameter, minor diameter, volume, and surface area. The cross-sectional appearance, round or more ribbon-shaped, was expressed as roundness. This index varies from 0 (parallel plates) to 1 (perfect ball). Mean increase (△) of each analyzed parameter was calculated by subtracting the scores for the treated canals from those recorded for the untreated counterparts. The percentage of increase of each parameter (%△) was calculated by using the scores measured before (B) and after (A) root canal preparation, according to the formula:
%△ = (A * 100/B) – 100
CTVol software (Skyscan) was used for three-dimensional visualization and qualitative evaluation of the preinstrumented and postinstrumented canals. Color-coded root canal models (green indicates preoperative, red postoperative canal surfaces) enabled qualitative comparison of the matched root canals before and after shaping.
OnDemand 3D software (Cybermed Inc, Irvine, CA) was used for the analysis of the 15 superimposed cross-sectional images of each specimen (n = 300 per group) regarding the percentage of instrumented and noninstrumented walls. The root canal preparation was classified into 2 categories: (1) cross section in which the whole perimeter or almost all the perimeter was treated (80% or more of the perimeter treated) and (2) cross section in which most of the perimeter was untreated (20% or less of the perimeter treated).
Statistical Analysis
The results were statistically analyzed with independent sample t test and χ2 test (with Yates correction) between groups and paired sample t test within the group, with the null hypothesis set as 5%, by using SPSS v17.0 for Windows (SPSS Inc, Chicago, IL).
Results
Quantitative Evaluation
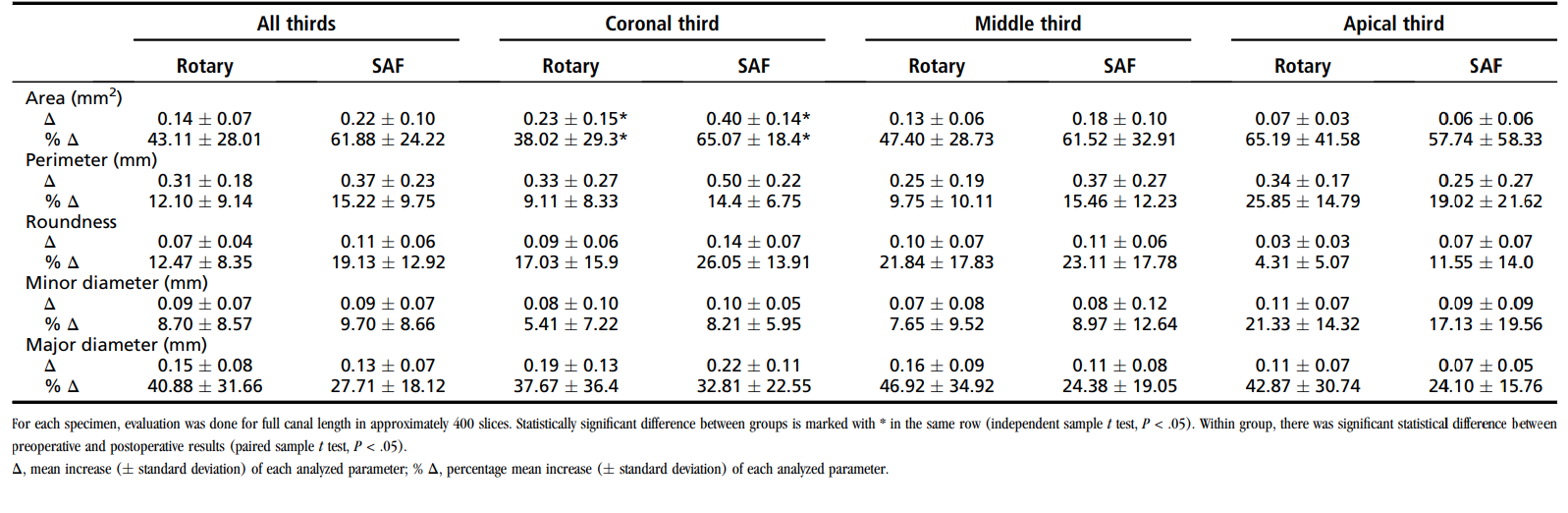
Two-Dimensional Analysis. The results of two-dimensional analysis are detailed in Table 1. Overall, area, perimeter, roundness, and major and minor diameters revealed no statistically significant difference between SAF and rotary preparation (P > .05). However, percentage mean increase of the root canal area in the coronal third was significantly higher with SAF (65.07% 18.4%) than with rotary instrumentation (38.02% 29.3%) (P = .03). Despite differences between groups in the postoperative results in relation to roundness (P = .02) and minor diameter (P = .01), no difference was observed in the preoperative and postoperative increase of these parameters (P >.05). No statistical difference was observed regarding the analyzed parameters in the middle and apical thirds (P > .05). Within group, there was a significant statistical difference between preoperative and postoperative results (P < .05).
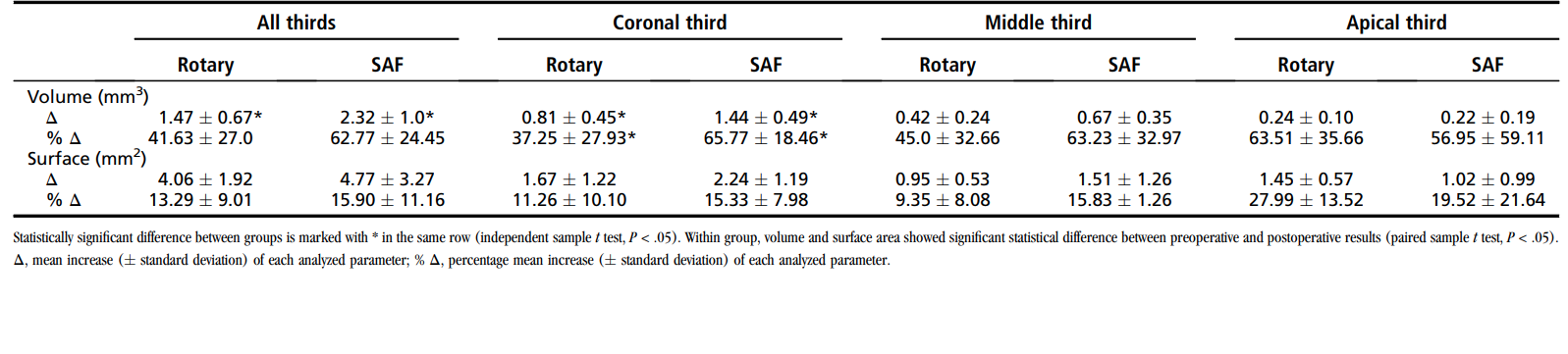
Three-Dimensional Analysis. The results of three-dimensional analysis are detailed in Table 2. No statistical difference in volume or surface area was observed in the middle or apical thirds between the groups (P > .05). Despite that the mean increase of the canal volume in the coronal third was significantly higher with SAF (1.44 ± 0.49 mm3) than with rotary instrumentation (0.81 ± 0.45 mm3) (P = .01), the same was not observed with the surface area (P > .05). Within group, volume and surface area showed a significant statistical difference between preoperative and postoperative results (P < .05).
Qualitative Evaluation
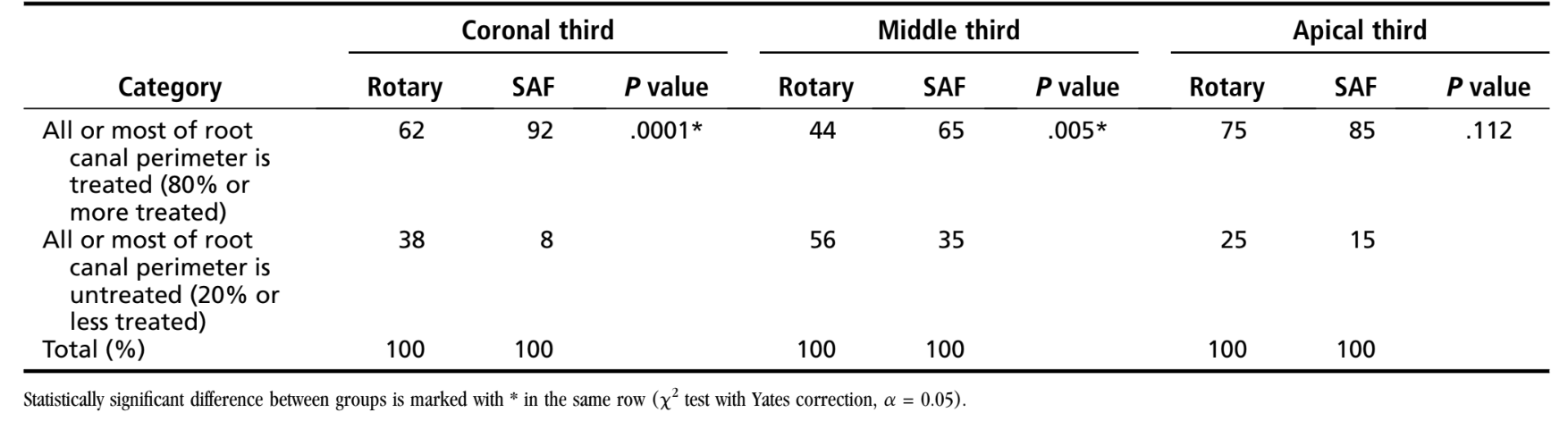
Preoperatively, root canal cross sections presented significantly flatter in the mesiodistal view than in the buccolingual aspect. Its geometry was changed after root canal preparation with both instruments. Superimposed μCT reconstructions in all thirds demonstrated that the use of SAF resulted in a more uniform dentin removal along the perimeter of the canals than with rotary instrumentation. The latter showed substantial untouched areas mainly on the lingual side of the canal. The number of samples in which all or most of the root canal perimeter was untreated, considering the coronal, middle, and apical thirds, was 58 (19.3%) for SAF group and 119 (39.7%) for rotary group. There was a statistically significant difference between the instrumented and the noninstrumented walls between groups at coronal and middle thirds (Table 3). Cross sections and tridimensional analysis showed that the use of SAF resulted in a more homogenous preparation of the root canal walls compared with rotary instruments (Figs. 1 and 2).
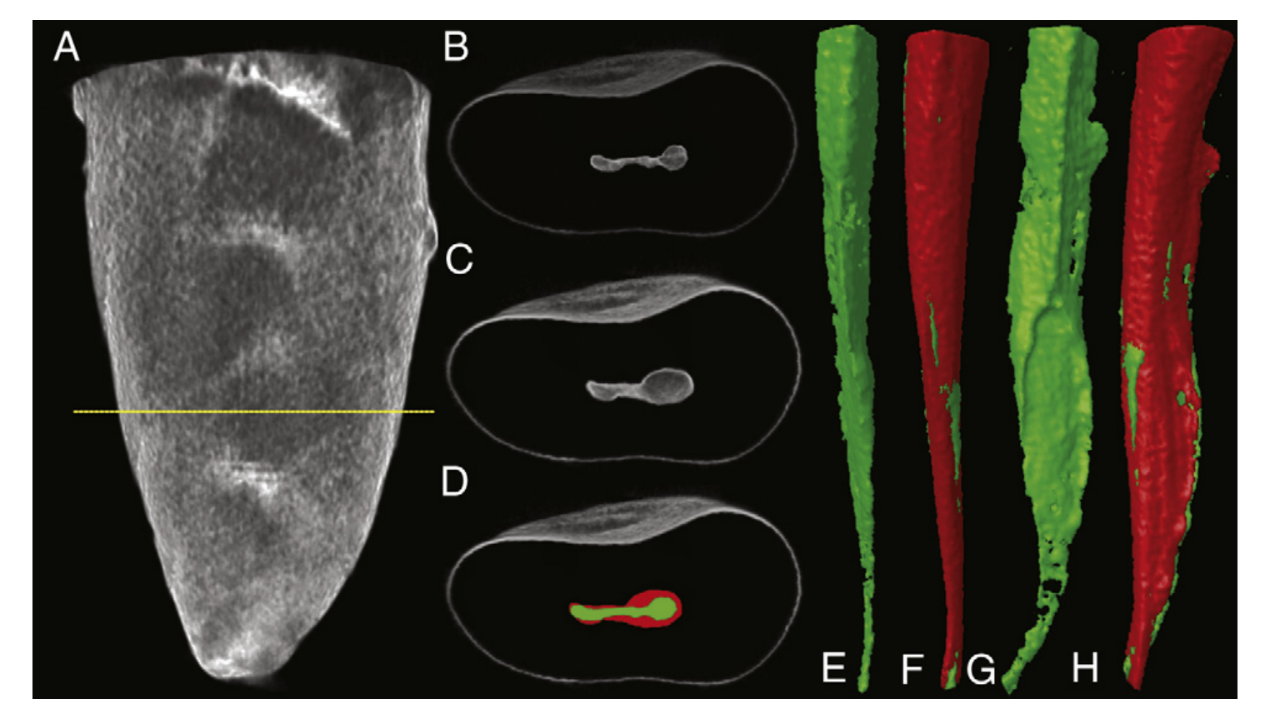
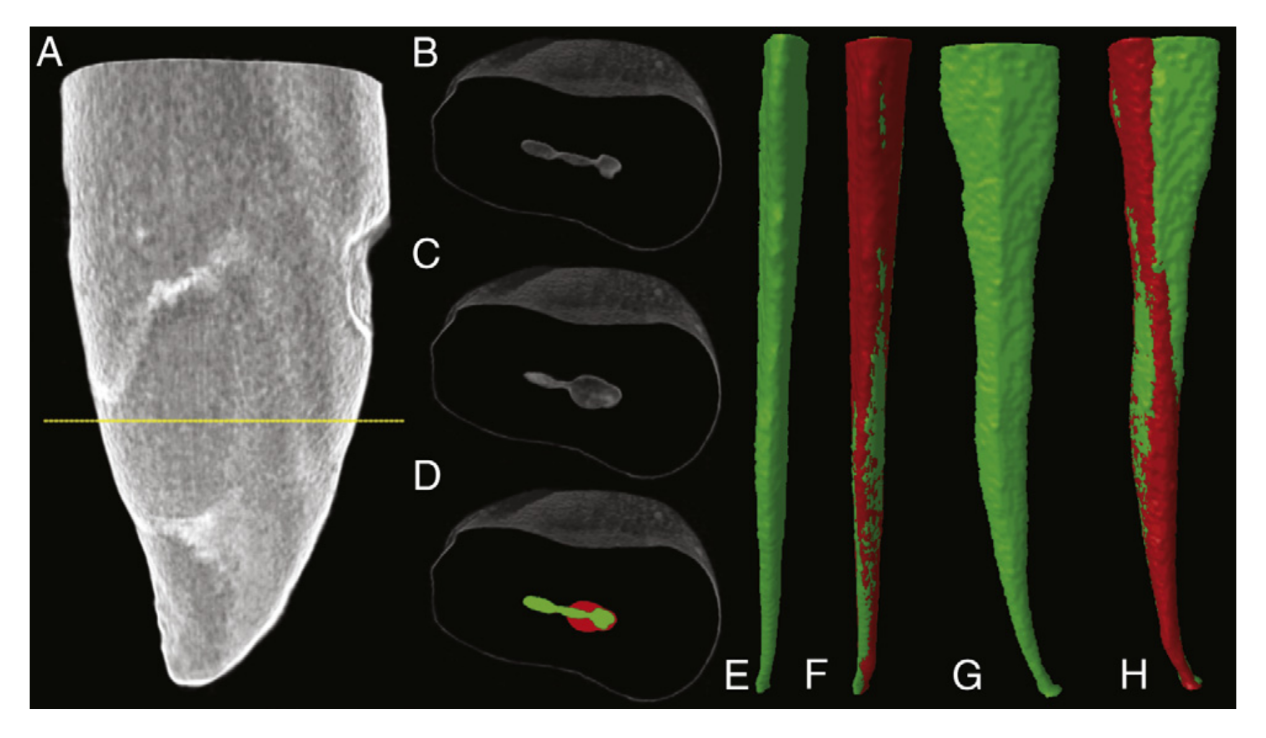
aration in buccal (E) and distal views (G). The superimposed μCT reconstructions in buccal (F) and distal (H) views demonstrate substantial untouched areas afterroot canal preparation with rotary instruments.
Discussion
Variations in canal geometry before shaping and cleaning procedures seem to have more influence on the changes that occurred during preparation than the instrumentation techniques themselves. Therefore, in the present study care was taken to ensure that the sample was balanced in terms of preoperative morphologic parameters between groups. The root canals in both groups were preflared and a #20 K-file was used for apical sizing because this procedure reflects clinical conditions under which root canal treatment is performed, as recommended by SAF’s manufacturer. Because the operator tactile skills have been considered more important than the technique in the thoroughness of canal debridement, root canal preparations were carried out by dentists with expertise in each of the tested techniques. Nonetheless, as previously pointed out, a potential limitation of this study could also be a result from the relatively small sample size of 20 teeth per group; however, it is similar to recent μCT studies.
When compared with rotary NiTi instrumentation, it has been reported that SAF leaves less unprepared areas and was significantly more effective in disinfecting long oval root canals in vitro. In the present study, SAF presented a higher increase of area (two-dimensional analysis) and volume (three-dimensional analysis) than the rotary group only at the coronal third. It might be explained as the relative softness of dentin near the pulp chamber as a result of the higher dentinal diameter and density, compared with the other canal regions. Besides, preflaring with Gates Glidden burs facilitated endodontic instrumentation and allowed SAF to act freely at this portion, promoting more dentin removal than with rotary instruments.
At middle third, although no differences have been observed regarding area or volume between groups, SAF system presented significantly higher percentage of prepared root canal walls (65%) than rotary instrumentation (44%). It might be inferred that this result would be due mainly to the anatomic feature of the flat-oval–shaped canal of mandibular incisor.
The preparation of the most apical canal section remains a challenge. At this region, previous studies on root canal preparation with SAF have left uninstrumented areas ranging from 28.8%–47.4% in maxillary molar root canals. Although there is disagreement among endodontic specialists about the maximal enlargement at WL, in the present study the final apical preparation with size #40, taper 0.02 in the rotary group was used as previously recommended for mandibular incisors. Despite the differences in file design, it should be noted that the final apical preparation was identical to both groups, considering either two-dimensional or three-dimensional analyzed quantitative parameters. As a consequence, no statistical difference was also found in the percentage of unprepared root canal walls by using SAF (15%) or rotary (25%) instruments. It might be explained as root canals of lower incisors tend toward a rounder cross section at this region, favoring the action of rotary instruments. This result demonstrates the action of SAF at the apical region and confirms the statement that the resulting apical size with SAF is usually at least equivalent to size #40 file.
Although the overall quantitative analysis of middle and apical thirds showed no difference between groups, the results clearly showed that instrumentation groups differed from each other in the qualitative analysis. As previously demonstrated, the present results suggest that rotary NiTi instrument alone was unable to adequately prepare the root canal, and SAF does indeed result in homogenous preparation and circumferential removal of a layer of hard tissue, favoring root canal disinfection and the accommodation of the root canal filling.
Further studies should be performed to compare the cleaning efficacy of the SAF system with a combination of rotary files with passive ultrasonic irrigation method in the flat-oval–shaped canals.
Conclusions
Within the limitations of this ex vivo study, it can be concluded that in the coronal third, mean increases of area and volume of the root canal, as well as the percentage of prepared walls, were significantly higher with SAF than with rotary instrumentation. By using SAF instrument, flat-oval–shaped canals of mandibular incisors were homogenously and circumferentially prepared. The size of the SAF preparation in the apical third of the canal was equivalent to those prepared with #40 rotary file with 0.02 taper.
Authors: Marco Aurélio Versiani, MS, Jesus Djalma Pécora, PhD, and Manoel Damião de Sousa-Neto
References:
- Metzger Z, Teperovich E, Zary R, Cohen R, Hof R. The self-adjusting file (SAF): part 1—respecting the root canal anatomy: a new concept of endodontic files and its implementation. J Endod 2010;36:679–90.
- Siqueira JF Jr, Roc¸as IN. Clinical implications and microbiology of bacterial persistence after treatment procedures. J Endod 2008;34:1291–301.
- Paqué F, Ganahl D, Peters OA. Effects of root canal preparation on apical geometry assessed by micro-computed tomography. J Endod 2009;35:1056–9.
- Peters OA. Current challenges and concepts in the preparation of root canal systems: a review. J Endod 2004;30:559–67.
- Barbizam JV, Fariniuk LF, Marchesan MA, Pécora JD, Sousa-Neto MD. Effectiveness of manual and rotary instrumentation techniques for cleaning flattened root canals. J Endod 2002;28:365–6.
- Fornari VJ, Silva-Sousa YT, Vanni JR, Pécora JD, Versiani MA, Sousa-Neto MD. Histological evaluation of the effectiveness of increased apical enlargement for cleaning the apical third of curved canals. Int Endod J 2010;43:988–94.
- Nadalin MR, Perez DE, Vansan LP, Paschoala C, Sousa-Neto MD, Saquy PC. Effectiveness of different final irrigation protocols in removing debris in flattened root canals. Braz Dent J 2009;20:211–4.
- Sasaki EW, Versiani MA, Perez DE, Sousa-Neto MD, Silva-Sousa YT, Silva RG. Ex vivo analysis of the debris remaining in flattened root canals of vital and nonvital teeth after biomechanical preparation with Ni-Ti rotary instruments. Braz Dent J 2006;17: 233–6.
- Taha NA, Ozawa T, Messer HH. Comparison of three techniques for preparing oval-shaped root canals. J Endod 2010;36:532–5.
- Peters OA, Paqué F. Root canal preparation of maxillary molars with the self-adjusting file: a micro-computed tomography study. J Endod 2011;37:517–21.
- Hof R, Perevalov V, Eltanani M, Zary R, Metzger Z. The self-adjusting file (SAF): part 2—mechanical analysis. J Endod 2010;36:691–6.
- Metzger Z, Teperovich E, Cohen R, Zary R, Paqué F, Hülsmann M. The self-adjusting file (SAF): part 3—removal of debris and smear layer: a scanning electron microscope study. J Endod 2010;36:697–702.
- Peters OA, Boessler C, Paqué F. Root canal preparation with a novel nickel-titanium instrument evaluated with micro-computed tomography: canal surface preparation over time. J Endod 2010;36:1068–72.
- Siqueira JF Jr, Alves FR, Almeida BM, de Oliveira JC, Roças IN. Ability of chemome- chanical preparation with either rotary instruments or self-adjusting file to disinfect oval-shaped root canals. J Endod 2010;36:1860–5.
- Somma F, Leoni D, Plotino G, Grande NM, Plasschaert A. Root canal morphology of the mesiobuccal root of maxillary first molars: a micro-computed tomographic analysis. Int Endod J 2009;42:165–74.
- Metzger Z, Zary R, Cohen R, Teperovich E, Paqué F. The quality of root canal preparation and root canal obturation in canals treated with rotary versus self-adjusting files: a three-dimensional micro-computed tomographic study. J Endod 2010;36: 1569–73.
- Hülsmann M, Peters OA, Dummer PMH. Mechanical preparation of root canals: shaping goals, techniques and means. Endod Topics 2005;10:30–76.
- Pashley D, Okabe A, Parham P. The relationship between dentin microhardness and tubule density. Endod Dent Traumatol 1985;1:176–9.
- Mauger MJ, Schindler WG, Walker WA 3rd. An evaluation of canal morphology at different levels of root resection in mandibular incisors. J Endod 1998;24:607–9.
- Wu MK, R’Oris A, Barkis D, Wesselink PR. Prevalence and extent of long oval canals in the apical third. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:739–43.
- Jou YT, Karabucak B, Levin J, Liu D. Endodontic working width: current concepts and techniques. Dent Clin North Am 2004;48:323–35.
- Schäfer E, Schlingemann R. Efficiency of rotary nickel-titanium K3 instruments compared with stainless steel hand K-Flexofile: part 2—cleaning effectiveness and shaping ability in severely curved root canals of extracted teeth. Int Endod J 2003;36:208–17.
