Morphological evaluation of maxillary second molars with fused roots: a micro-CT study
Abstract
Aim: To evaluate the internal and external morphologies of fused-rooted maxillary second molars by means of micro-computed tomography (micro-CT) analysis.
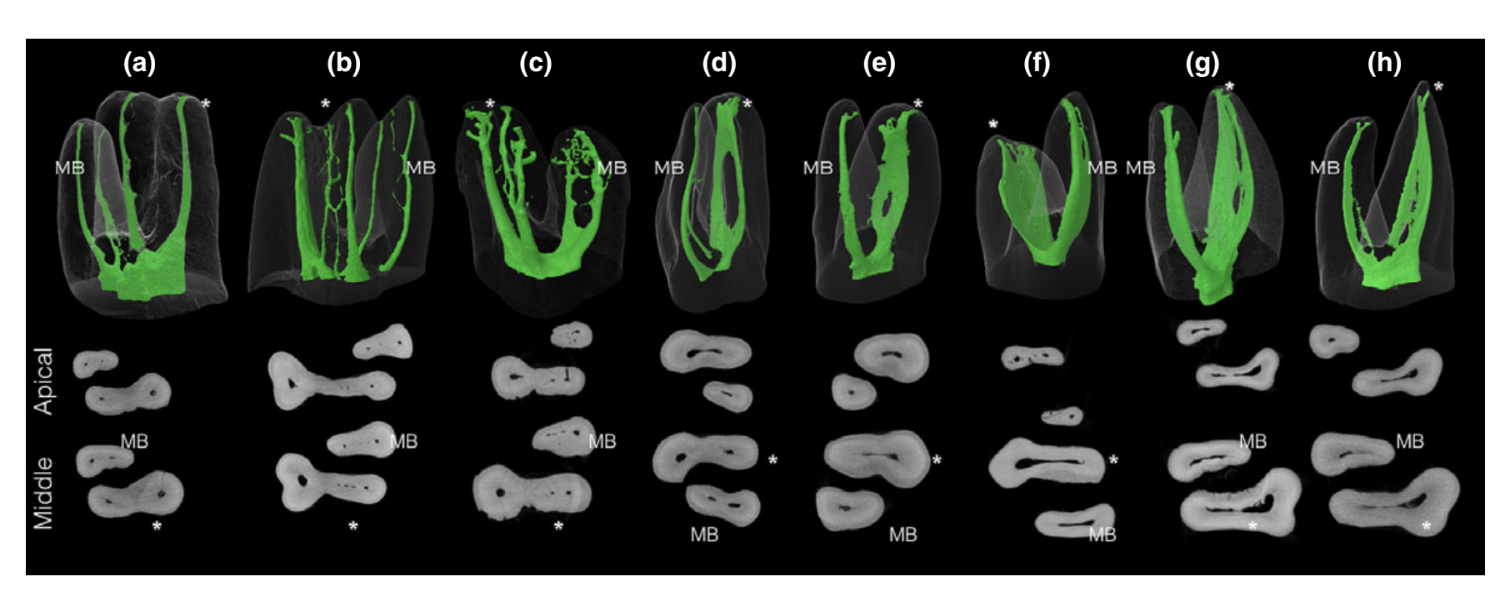
Methodology: A total of 100 fused-rooted maxillary second molars from a Brazilian subpopulation were divided into six groups according to the root morphology. The samples were scanned at a resolution of 19.6 μm and evaluated with regard to the external morphology of the roots, the root canal configuration, the percentage frequency of C-shaped canals and isthmuses, as well as the morphology of the root canal system at 1, 2 and 3 mm from the anatomical apex of the fused roots.
Results: The most prevalent root canal fusions were type 1, mesiobuccal root fused with distobuccal root (32%), followed by type 3, DB root fused with P root (27%), and type 4, MB root fused with DB root, and P root fused with MB or DB roots (21%). The prevalence of C-shaped root canal systems were 22%. Depending on the type of root fusion, the percentage frequency of isthmuses in the apical level varied from 9.3% to 42.8%, whilst the presence of apical deltas ranged from 18.5% to 57.1% of teeth.
Conclusions: The root canal system of maxillary second molars with fused roots may have a high incidence of merging canals, isthmuses, apical deltas and C-shaped configurations.
Introduction
A comprehensive understanding of the internal anatomy of the posterior teeth and an expectation of their likely variations is paramount to minimize root canal treatment failure caused by the persistence of the infected necrotic pulp, bacteria or by-products (Vertucci 1984, 2005). The maxillary second molar usually has three roots, two buccal and one palatal (Vertucci 1984, Cleghorn et al. 2006). Statistically, the most common anatomical variation studied in this tooth is related to the presence or absence of the mesiopalatal or MB2 canal (Alavi et al. 2002). Although the maxillary second molar resembles the maxillary first molar, the distinctive morphologic characteristic of this tooth is that its roots are grouped closer together or are occasionally fused (Vertucci 2005). Fused roots can be a challenge not only from a cleaning and shaping perspective but also from a surgical point of view. A fused root can combine the variability of the root canal system with the presence of isthmuses or additional canals connecting some (or all) of the roots (Fan et al. 2004, Zhang et al. 2014). Previous studies have shown that the prevalence of fused roots in maxillary second molars ranges from 9.0% to 42.25% (Peikoff et al. 1996, Zhang et al. 2014). In addition, the prevalence of fused roots in maxillary second molars is four times higher when compared to maxillary first molars (Martins et al. 2016a).
Although a wide range of anatomical variations associated with maxillary molars have been reported (Vertucci 2005, Versiani et al. 2012), understanding of the morphological aspects of fused-rooted maxillary second molars is limited. Research on this group of teeth has been based on studies with small sample sizes (Al Shalabi et al. 2000, Alavi et al. 2002). In other studies, researchers used methodological approaches that do not allow the analysis of fine details of the internal anatomy such as isthmuses, apical ramifications and C-shaped canals (Kim et al. 2012, Martins et al. 2016a). The micro-computed tomography (micro-CT) imaging system is currently considered the gold standard for the study of root canal anatomy as it provides reproducible and detailed information regarding the two- and three-dimensional aspects of the teeth (Ordinola-Zapata et al. 2013, 2015, Filpo-Perez et al. 2015). Micro-CT methods have major advantages over conventional clearing techniques (Lee et al. 2014, Ordinola-Zapata et al. 2017). To date, only one study performed in an Asian population addressed the morphological variations of the maxillary second molar root canal system using this new technology. However, it did not describe certain morphological aspects such as the apical anatomy or the presence of C-shaped canals (Zhang et al. 2014). Thus, the aim of this study was to evaluate the internal and external morphologies of maxillary second molars with fused roots by means of micro-CT image analysis.
Materials and methods
After local research ethics committee approval (Protocol #131-2010), 100 extracted fused-rooted maxillary second molars were selected from a Brazilian subpopulation and scanned in a micro-CT device (SkyScan 1174v2; Bruker micro-CT, Kontich, Belgium) at 50 kV, 800 mA, rotation step of 0.8, 360° rotation, voxel size of 19.6 μm and 1304 9 1024 pixels resolution. The gender and age were unknown. Images of each specimen were reconstructed (NRecon v. 1.6.3; Bruker micro-CT), and the analysis of axial cross sections of their inner structure was performed using DataViewer v. 1.5.2.4 software (Bruker micro-CT). In addition, 3D models were achieved by the binarization of the dentine and the root canal system using the CTAn v. 1.16 (Bruker micro-CT) and CTVol v. 2.3 software (Bruker micro-CT). The root canal configuration, the percentage frequency of C-shaped canals and isthmuses, as well as the morphology of the root canal system at 1, 2 and 3 mm from the anatomical apex of the fused roots, were evaluated by a single operator experienced in analysing the morphology of roots and root canals using micro-CT technology.
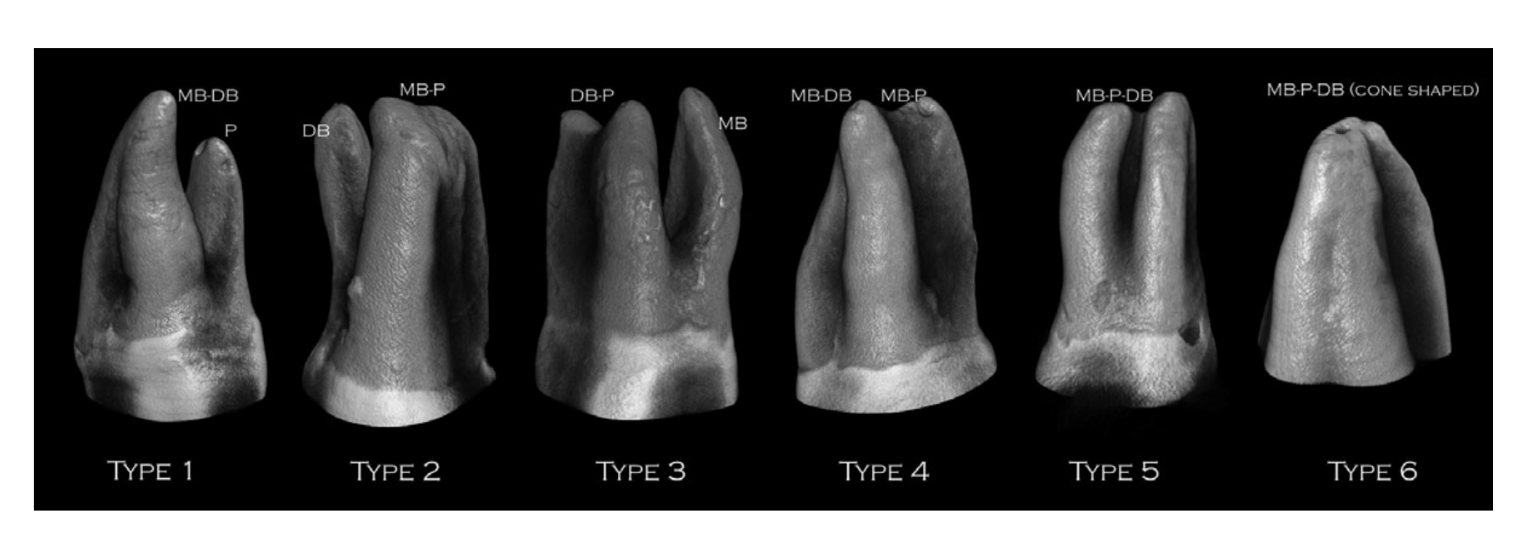
Root and root canal morphologies
The external morphology of the roots was classified into six types (Zhang et al. 2014): type 1—mesiobuccal (MB) root fused with distobuccal (DB) root; type 2—MB root fused with palatal (P) root; type 3—DB root fused with P root; type 4—MB root fused with DB root, and P root fused MB or DB roots; type 5—P root fused with MB and DB roots; and type 6—MB, DB and P roots fused to a cone-shaped root (Fig. 1). The root canal configurations were described according to Vertucci (1984).
C-shaped canals
The axial cross-sectional images were analysed at the full extension of the fused roots. The root canal system was classified as C-shaped if they followed two criteria, according to Martins et al. (2016b): (i) root fusion and (ii) three consecutive axial cross sections with a continuous large C-shaped canal system or continuous C-shaped canal with two main canal lumen in the extremities connected by a large isthmus.
Apical anatomy
Axial cross sections obtained at 1, 2 and 3 mm from the anatomical apex of the fused roots were evaluated regarding the percentage frequency of apical delta, defined as a ramification that included the presence of a minimum of two accessory canals beside the main root canals in a single fused root apical area, and the presence of complete or incomplete isthmus, classified according to Hsu & Kim (1997) into: type I—2 or 3 canals with no communication; type II—2 main canals with a connection between them; type III—3 canals with a connection between them; type IV— main canals project into the isthmus area; and type V—true connection or corridor between the canals along the cross sections.
Statistical analysis
The Z-test for proportions in independent groups with a level of significance of 5% was used to analyse the differences between proportions of C-shaped morphologies and apical delta amongst different types of fused-rooted molars.
Results
Root and root canal morphologies
Table 1 shows the percentage frequency of the external morphology in 100 maxillary second molars with fused roots (types 1–6). Table 2 summarizes the root canal configuration types of maxillary molars with root fusion types 1–3. Due to the complexity of the root canal system in fused molars types 4 and 5, most of their canal configurations were classified as ‘other types’. Type 6 fusion included only 1 sample and was not considered in the analysis. Representative 3D images of the root canal system of fused molars types 1–6 are shown in Figs 2–4.
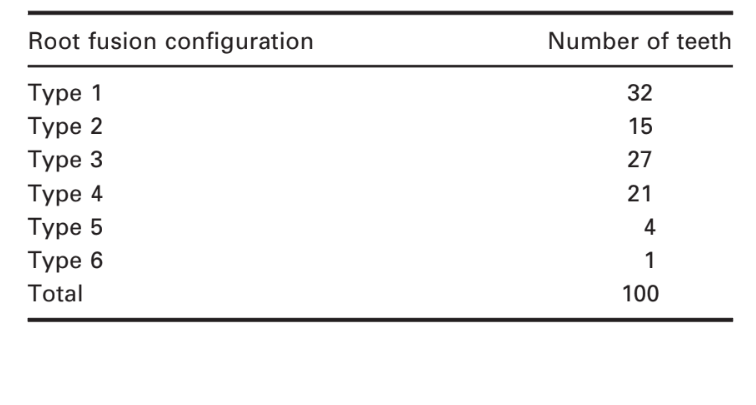

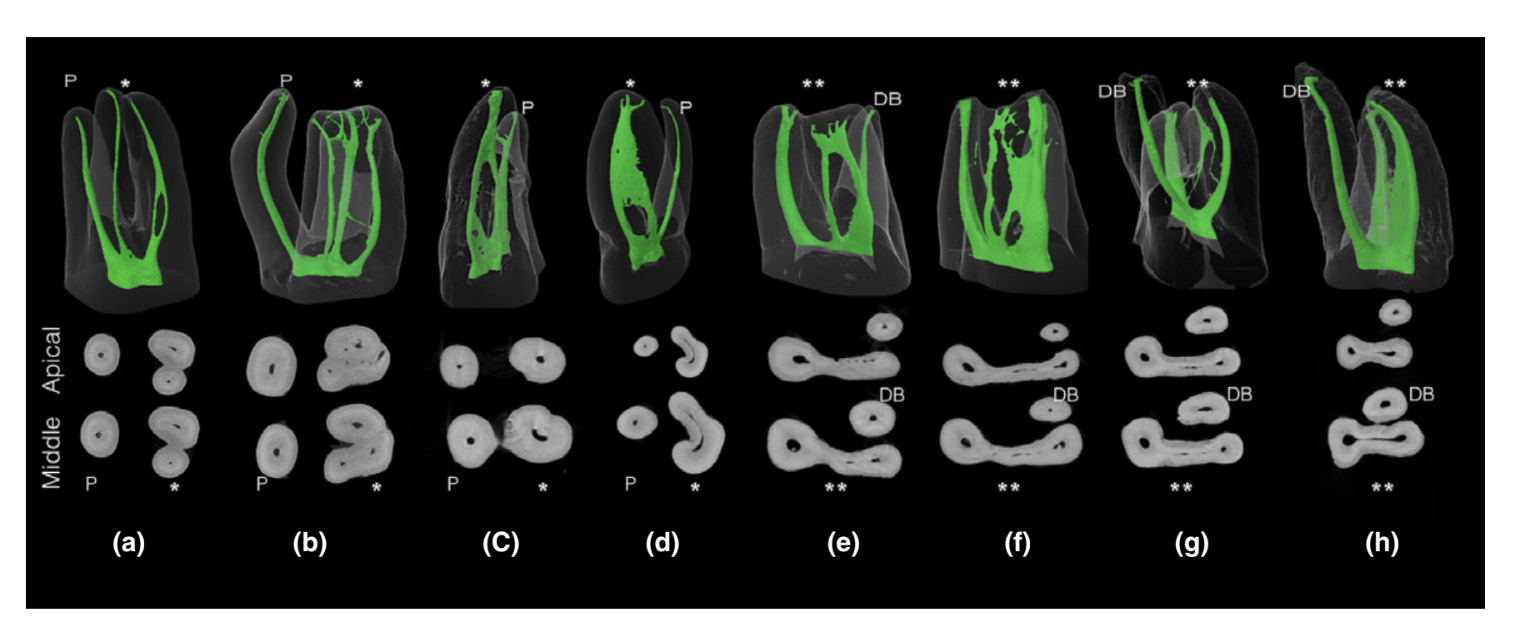

Complex canal configurations were commonly observed in the MB root (Table 2). The presence of a third canal in the MB root was observed in four teeth when this root was fused to the palatal root (type 2 configuration), whilst a double canal system in the DB root was observed in four molars in which DB root was fused to the palatal root (type 3).
In molars with fused root type 4 (n = 21), at least four root canal configurations were identified: (i) buccal canals merged into the apical third (n = 5); (ii) only one buccal canal with or without communication with the palatal canal (n = 8); (iii) MB and DB canals did not merge, but had communication with the palatal canal (n = 3); and (iv) independent MB, DB and palatal root canals (n = 5). New canal configurations that are not included in the classic Vertucci’s configuration system (Vertucci 1984) or its supplemental configurations (Sert & Bayirli 2004), named here as ‘other types’, were also observed (Table 2, Figs 2–4).
In total, 49% of the evaluated teeth did not differ from the common internal anatomy of maxillary molars with three separated roots (absence of communications or confluences between buccal canals or between MB or DB canal with the palatal system), 24 samples in type 1, 7 samples in type 2, 13 samples in type 3 and 5 samples in type 4.
C-shaped canals
The C-shaped root canal configuration was found in 22 specimens. This anatomy was more commonly observed in single-rooted types 4–5 (31%; 8 out of 26) compared to double-rooted types 1–3 (19%; 14 out of 74; Table 3). However, the difference of proportions of C-shaped morphologies between fused root types (types 1–5) was considered nonsignificant (P > 0.05).
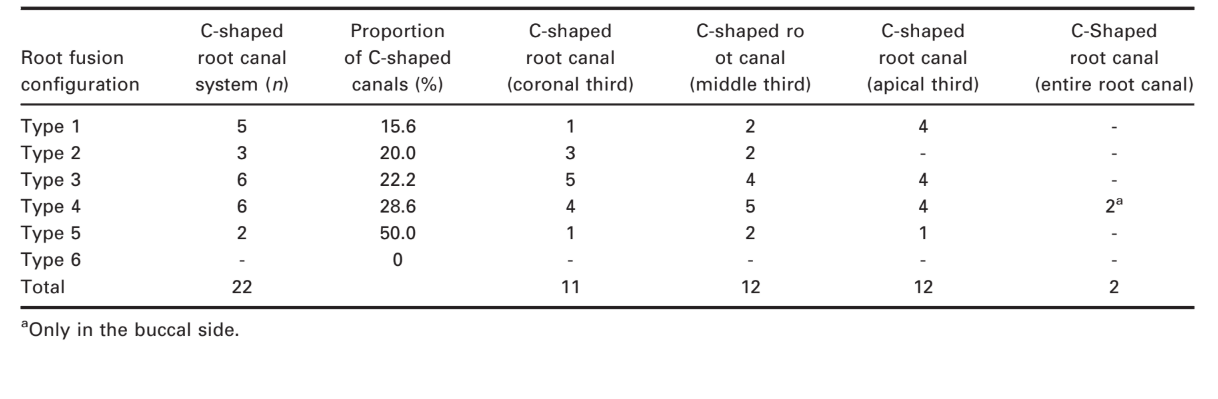
In most of teeth, the C-shaped configuration was observed in the confluence of the canals in the middle and apical thirds of the fused roots; however, this configuration was located at the cervical and middle thirds of the type 2 roots (Table 3).
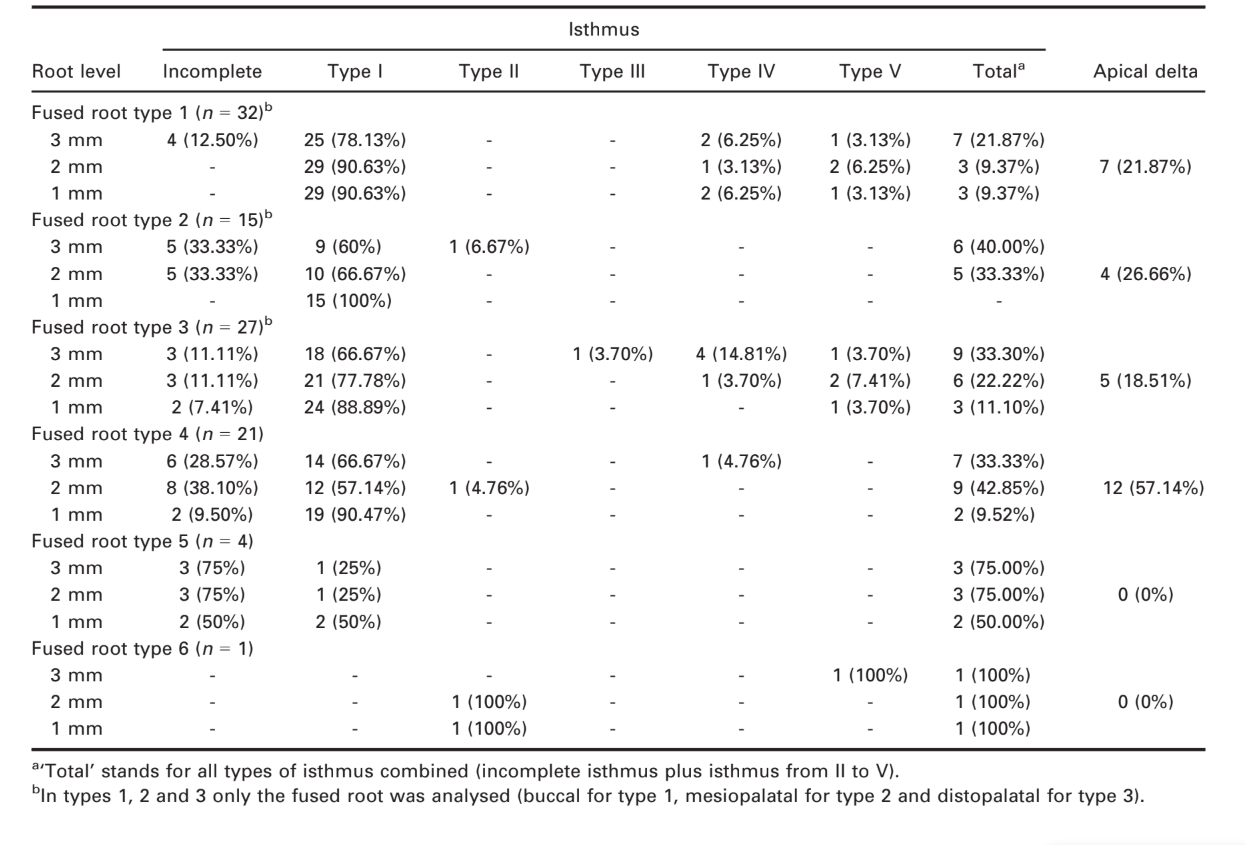
Apical anatomy
The analysis of the apical morphology of the maxillary second molars with fused roots revealed a high prevalence of isthmuses 3 mm from the apex, which decreased towards to the apex (Table 4). The highest proportion of isthmuses (43%) and apical deltas (57%) was found in molars with root fusion type 4 when compared to other types of fused molar teeth. The prevalence of apical deltas at the apical 3 mm in root fusion type 4 was significant (P < 0.05).
Discussion
Several studies have pointed out a strong correlation between the external morphology of the roots and the internal anatomy of teeth. It is well known that fusions and radicular grooves (Fan et al. 2004, 2008, Ordinola-Zapata et al. 2013, 2015) have been associated with highly complex root canal systems in mandibular second molars and mandibular premolars (Fan et al. 2004, Ordinola-Zapata et al. 2015). As shown in this study, maxillary second molars with fused roots have a relatively high frequency of C-shaped and merging canals. According to the literature, the frequency of maxillary second molars with fused roots varies between different geographical locations, ranging from 6.7% in India (Neelakantan et al. 2010) to 42.25% in China (Zhang et al. 2014). The different information gained by previous studies cannot be compared to the results of this research mainly because of the presence of different populations, observational methods, classification criteria and terms used in previous studies (Yang et al. 1988, Carlsen et al. 1992, Martins et al. 2016a).
It is important to point out that the term ‘fused roots’ previously defined by Zhang et al. (2014) and Martins et al. (2016a) was used in this study to describe two or more roots that joined together. Fused roots may form by either age-related deposits that can cement root structures together (Carlsen et al. 1992) or as a result of the failure of Hertwig’s epithelial sheath to develop or fuse in the furcation area (Al-Fouzan 2002, Gao et al. 2006). Based on the former, it may be hypothesized that age-related cementum deposition would be associated with teeth with independent canals. In this study, the evaluation of the different canal configurations showed that 49% of the sample did not differ from the common internal anatomy of maxillary molars with three separated roots; however, it was not possible to evaluate the impact of age because patients’ age and the condition of the teeth after root development were unknown. However, the high percentage frequency of C-shaped canals, merging canals, and communications amongst the canal systems found in 51% of the sample suggests that fused root in these teeth may have occurred due to a developmental anomaly during root formation.
The analysis of the external morphology of maxillary second molar teeth identified all of the types of root fusion proposed by Zhang et al. (2014; Fig. 1). Each root fusion had its own morphological features related to the involved roots (Figs 2 and 3). In type 1 molars (MB-DB fusion), eight teeth (25% of the sample) had a confluence or communication between the buccal canals within the fused buccal roots. In types 2 (MB-P fusion), 3 (DB-P fusion) and 4, the confluence of the canals increased to 53.3% (8 molars), 51.8% (14 molars) and 76.1% (16 molars), respectively. Consequently, it is reasonable to consider that maxillary second molars types 1–4 are prone to have additional canals and confluences in the fused roots.
The presence of C-shaped canals in maxillary molars is rare (Vertucci 2005). Newton & McDonald (1984) were the first to report a C-shaped configuration formed by the joining of the distobuccal and palatal orifices in a maxillary first molar, similar to the C-shaped configuration reported in mandibular molars. Carlsen et al. (1992) hypothesized that the presence of fused roots increased the possibility that two or more root canals merge and assume a C-shaped configuration. Later, the presence of C-shaped canals in fused roots of maxillary molars was confirmed (Yang et al. 1988, Martins et al. 2016b). In this study, C-shaped canals were observed in 22% of the sample with fused roots types 1–5. This high incidence is unusual and still not reported in the literature; however, it might be explained by the observational method used and the large sample size. In this study, 100 maxillary second molars with fused roots were evaluated using nondestructive and accurate micro-CT technology, which allowed for a more precise and detailed analysis of the fine structures of the root canal system (Zhang et al. 2014, Ordinola-Zapata et al. 2017). Unlike mandibular molars, it is interesting to notice that the C-shaped configuration in maxillary second molars with fused roots rarely extends from the pulp chamber to the apex. Interestingly, in two molars with root fusion type 4, a C-shaped canal was observed only in the buccal aspect of the root, without involving the palatal canal, a configuration classified as type B by Martins et al. (2016b).
In this study, the morphological analysis of the apex of maxillary molars with fused roots was also performed in order to evaluate the percentage frequency of isthmuses and ramifications. Previous studies on resected roots of teeth with failed root canal therapy have associated the persistence of apical periodontitis with anatomy that was not prepared or filled adequately (Wada et al. 1998, Song et al. 2011, Karabucak et al. 2016). The present results showed that the percentage frequency of isthmus and apical delta ranged from 9% to 43% and from 19% to 57%, respectively, depending on the type of root fusion. Amongst them, molars with fused root type 4 had the highest frequency of complexities in the apical area.
If microsurgery is necessary, the following surgical challenges can be expected in these teeth: (i) With the exception of the type 1 fusion, most of the variations include the fusion of the palatal root. Clinicians need to be aware of the presence of anatomical structures in proximity to the palatal canal specially the maxillary sinus. (ii) The difficulty of visualizing the palatal apical third when a buccal osteotomy is used is well known. (iii) Root-end ultrasonic preparation should include the thin isthmuses that can be present in C-shaped canals and fused roots. 4. Root-end resection of type 4 and 5 variations includes simultaneous resection of three roots, which can be difficult. In selected cases, the less invasive intentional replantation procedure should be considered. One limitation of the present study is that the axial cross-sectional analysis was performed only at the critical apical 3 mm of the fused root. It would be interesting in future research to perform a dentine thickness analysis of the root structure especially in concavities and in the apical third area in order to gain more information that can improve the clinical management of these anatomical variations.
Conclusion
The root canal system of maxillary second molars with fused roots has a high incidence of merging canals, isthmuses, apical deltas and C-shaped configuration.
Authors: R. Ordinola-Zapata, J. N. R. Martins, C. M. Bramante, M. H. Villas-Boas, M. H. Duarte, M. A. Versiani
References:
- Al Shalabi RM, Omer OE, Claffey N (2000) Root canal anatomy of maxillary first and second permanent molars. International Endodontic Journal 33, 405–14.
- Alavi AM, Opasanon A, Ng YL, Gulabivala K (2002) Root and canal morphology of Thai maxillary molars. International Endodontic Journal 35, 478–85.
- Al-Fouzan KS (2002) C-shaped root canals in mandibular second molars in a Saudi Arabian population. International Endodontic Journal 35, 499–504.
- Carlsen O, Alexandersen V, Heitmann T, Jakobsen P (1992) Root canals in one-rooted maxillary second molars. Scandinavian Journal of Dental Research 100, 249–56.
- Cleghorn BM, Christie WH, Dong C (2006) Root and root canal morphology of the human permanent maxillary first molar: a literature review. Journal of Endodontics 32, 813– 21.
- Fan B, Cheung GSP, Fan M, Gutmann JL, Bian Z (2004) C- shaped canal system in mandibular second molars: part I – anatomical features. Journal of Endodontics 30, 899–903.
- Fan B, Yang J, Gutmann J, Fan M (2008) Root canal systems in mandibular first premolars with C-shaped root canal configurations. Part I: microcomputed tomography mapping of the radicular groove and associated root canal cross-sections. Journal of Endodontics 34, 1337–41.
- Filpo-Perez C, Bramante CM, Villas-Boas MH, Húngaro Duarte MA, Versiani MA, Ordinola-Zapata R (2015) Micro-computed tomographic analysis of the root canal morphology of the distal root of mandibular first molar. Journal of Endodontics 41, 231–6.
- Gao Y, Fan B, Cheung GS, Gutmann JL, Fan M (2006) C-shaped canal system in mandibular second molars part IV: 3-D morphological analysis and transverse measurement. Journal of Endodontics 32, 1062–5.
- Hsu Y, Kim S (1997) The resected root surface: the issue of canal isthmuses. Dental Clinics of North America 41, 529–40.
- Karabucak B, Bunes A, Chehoud C, Kohli MR, Setzer F (2016) Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: a cone-beam computed tomography study. Journal of Endodontics 42, 538–41.
- Kim Y, Lee SJ, Woo J (2012) Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in Korean population: variations in the number of roots and canals and the incidence of fusion. Journal of Endodontics 38, 1063–8.
- Lee KW, Kim Y, Perinpanayagam H (2014) Comparison of alternative image reformatting techniques in micro-computed tomography and tooth clearing for detailed canal morphology. Journal of Endodontics 40, 417–22.
- Martins JNR, Mata A, Marques D, Caramês J (2016a) Prevalence of root fusions and main root canal merging in human upper and lower molars – a CBCT in vivo study. Journal of Endodontics 42, 900–8.
- Martins JNR, Mata A, Marques D, Anderson C, Caramês J (2016b) Prevalence and characteristics of the maxillary C-shaped molar. Journal of Endodontics 42, 383–9.
- Neelakantan P, Subbarao C, Ahuja R, Subbarao CV, Gutmann JL (2010) Cone-beam computed tomography study of root and canal morphology of maxillary first and second molars in an Indian population. Journal of Endodontics 36, 1622–7.
- Newton CW, McDonald S (1984) A C-shaped canal configuration in a maxillary first molar. Journal of Endodontics 10, 397–9.
- Ordinola-Zapata R, Bramante CM, Villas-Boas MH, Cavenago BC, Duarte MH, Versiani MA (2013) Morphologic micro-computed tomography analysis of mandibular premolars with three root canals. Journal of Endodontics 39, 1130–5.
- Ordinola-Zapata R, Monteiro Bramante C, Gagliardi Minotti P et al. (2015) Micro-CT evaluation of C-shaped mandibular first premolars in a Brazilian subpopulation. International Endodontic Journal 48, 807–13.
- Ordinola-Zapata R, Bramante CM, Versiani MA, Moldauer BI, Topham G (2017) Comparative accuracy of clearing technique, CBCT and micro-CT methods in studying mesial root canal configurations of mandibular first molars. International Endodontic Journal 50, 90–6.
- Peikoff M, Christie W, Fogel H (1996) The maxillary second molar: variation in the number of roots and canals. International Endodontic Journal 29, 365–9.
- Sert S, Bayirli G (2004) Evaluation of the root canal configuration of the mandibular and maxillary permanent teeth by gender in the Turkish population. Journal of Endodontics 30, 391–8.
- Song M, Kim H, Lee W, Kim E (2011) Analysis of the causes of failure in nonsurgical endodontic treatment by microscope inspection during endodontic microsurgery. Journal of Endodontics 37, 1516–9.
- Versiani MA, Pécora JD, Sousa-Neto MD (2012) Root and root canal morphology of four-rooted maxillary second molars: a micro-computed tomography study. Journal of Endodontics 38, 977–82.
- Vertucci FJ (1984) Root canal anatomy of the human permanent teeth. Oral Surgery Oral Medicine Oral Pathology 58, 589–99.
- Vertucci FJ (2005) Root canal morphology and its relationship to endodontic procedures. Endodontic Topics 10, 3–29.
- Wada M, Takase T, Nakanuma K, Arisue K, Nagahama F, Yamazaki M (1998) Clinical study of refractory apical periodontitis treated by apicectomy Part 1. Root canal morphology of resected apex. International Endodontic Journal 31, 53–6.
- Yang Z, Yang S, Lee G (1988) The root and root canal anatomy of maxillary molars in a Chinese population. Endodontic and Dental Traumatology 4, 215–8.
- Zhang Q, Chen H, Fan B, Fan W, Gutmann J (2014) Root and root canal morphologies in maxillary second molar with fused root from a native Chinese population. Journal of Endodontics 40, 871–85.
