Clinical management and subsequent healing of teeth with horizontal root fractures
Abstract
Horizontal root fractures are uncommon, mainly occurring on the cervical and middle third of the root of permanent upper incisors. The diagnosis is essentially radiographic and requires different healing patterns, depending on some pre- and postinjury factors. The aim of this article was to report the clinical management and different healing types in three cases of horizontal root fractures on permanent dentition. In case 1, the pulp tissue was vital and no treatment was necessary. In case 2, a root canal treatment of the cervical fragment was necessary and in case 3, pulpal necrosis was verified and an apical surgery was performed.
Root fractures are uncommon lesions accounting for 0.5–7% of traumas that occur in the permanent dentition. They involve the tooth’s supportive tissue, dental pulp and mineralized structures, affecting predominantly the middle-third of upper incisors from male patients during the second decade of life. Indeed, root fractures can be associated with bone alveolar fracture.
They can be classified according to the direction in which they occur (horizontal or vertical), the number of fractures lines (simple or multiple), or according to the root affected locally (cervical, middle, or apical). The diagnosis is essentially radiographic, as clinical features similar to luxations and alveolar ridge fractures can be presented.
There are different types of fracture healing depending on some pre- and postinjury factors, such as the stage of root formation, patients’ age, tooth mobility, and location of root fracture. After adequate clinical management, it is fundamental that patients be followed up during a certain period of time for clinical treatment success. Considering these facts, the aim of this article was to report the clinical management and different healing types in three cases of horizontal root fractures in permanent dentition, with long-term follow-up.
Case reports
Case 1
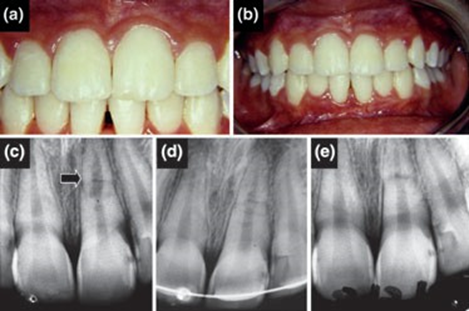
A 19-year-old female patient attended the Department of Endodontics, Brazilian Association of Dentistry, Uberlândia, Minas Gerais, Brazil, immediately after a trauma suffered on the maxillary anterior region. The patient complained of cold-induced sensibility in the left upper central incisor. Intraoral examination revealed well-preserved maxillary teeth, without mobility or discolored crown and all of them showed pulp vitality to thermal testing (Fig. 1a,b). Radiographically, a horizontal fracture on the root middle-third of the left upper central incisor with diastasis of 0.1 mm was observed (Fig. 1c). The fractured root was completely formed (mature) and no periapical changes were noted. Based on the clinical aspects that showed pulp with cold-induced sensibility, absence of dental mobility or periapical changes and non-discolored crown, we performed a rigid splinting with an orthodontic wire bonded to the labial surfaces of the maxillary anterior teeth using composite resin. Afterward, the patient was followed up weekly to evaluate pulp sensibility and dental mobility, as well as to assess the radiographic characteristics. After 45 days of observation, the clinical findings remained unaltered and the rigid fixation was removed (Fig. 1d). After 4 years of clinical follow-up, we verified that there were no signs or symptoms associated with the previously fractured tooth. Radiographically, it was possible to observe healthy pulp tissue, periodontal structure maintenance and complete healing of the fractured root with fragments in close contact (Fig. 1e).
Case 2
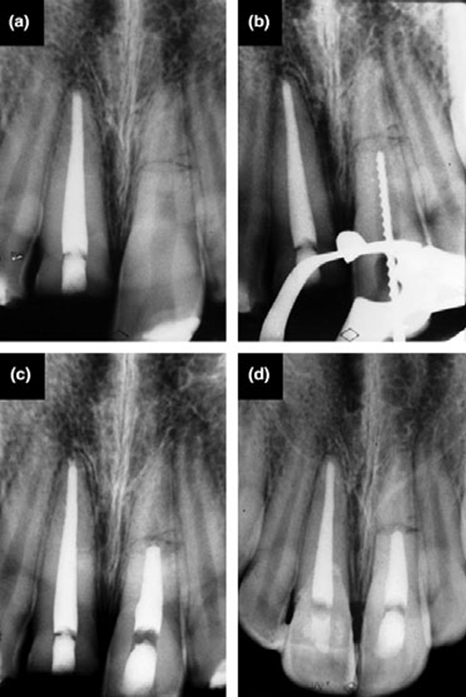
A 38-year-old male patient was referred to the Department of Endodontics, Brazilian Association of Dentistry, Uberlândia, Minas Gerais, Brazil, complaining of pain in the maxillary anterior teeth associated with a history of trauma on this region 60 days ago. During intraoral clinical examination, a cervical crown fracture in the right upper central incisor was observed, while the left central incisor presented slight mobility and spontaneous pain. Both teeth crowns remained unaltered. Radiographic examination revealed a horizontal root fracture on the middle-third of the left maxillary central incisor. The right central incisor root was intact (Fig. 2a). The roots of both traumatized teeth presented full development and the right upper central incisor had the radicular canal endodontically treated. As the left maxillary central incisor showed irreversible pulpits, the cervical fragment was submitted to endodontic treatment (Fig. 2b), using calcium hydroxide for 30 days as intracanal medication. This root fragment was later definitively obturated, without overfilling (Fig. 2c). A rigid fixation of the cervical fragment was not performed because of slight mobility and the impossibility of preserving vitality in both fragments. The crown fragment of the right central incisor was correctly positioned and bonded to the dental surface with composite resin. The patient was under weekly clinical and radiographic follow-up for 1 month. After 3 years of treatment and under follow-up every 6 months, the patient did not present clinical symptoms. Radiographically, a complete healing of the root fracture with interposition of hard and soft tissue between fragments was observed (Fig. 2d).
Case 3
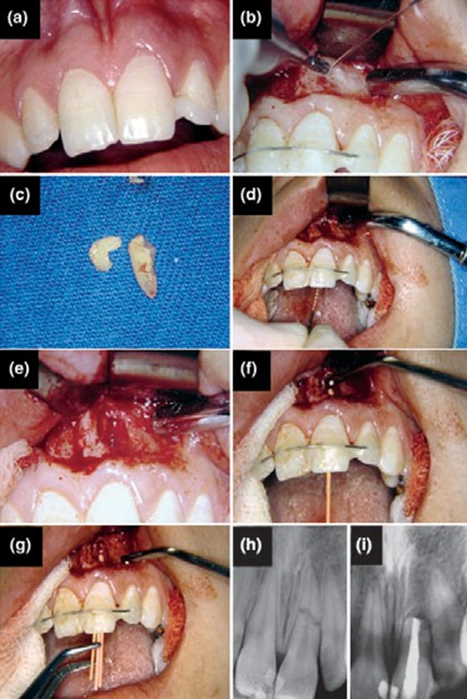
A 22-year-old female patient was referred to the Department of Endodontics, Brazilian Association of Dentistry, Uberlândia, Minas Gerais, Brazil, reporting a history of trauma on the maxillary anterior region 40 days ago. Clinically, the left maxillary central incisor was bonded to the left maxillary lateral incisor through fiber-reinforced composite (Fig. 3a). The patient complained of spontaneous pain and intense percussion sensibility in the left upper central incisor. On this maxillary region, color alteration of the vestibular alveolar mucosa was also verified. The remaining anterior maxillary teeth were intact and with normal color. During radiographic examination, it was possible to identify a horizontal root fracture on the middle-third of the left maxillary central incisor (Fig. 3h). All anterior maxillary teeth presented complete radicular development, including the traumatized tooth, and no bone alterations were noted. We carried out a rigid fixation with orthodontic wire bonded to the vestibular surfaces of the maxillary anterior teeth using composite resin (Fig. 3b). Necroses of both cervical and apical fragments of the central incisor were observed. Thus, endodontic treatment of the cervical fragment was performed followed by surgical removal of the apical fragment (Fig. 3c–g). Thereafter, the cervical fragment was endodontically instrumented and carefully obturated, without overfilling. As performed in cases 1 and 2, the patient was followed up weekly through clinical and radiographic examination during the first month. After 3 months, the rigid fixation was removed. After 5 years of treatment, the patient presented full bone healing on the surgical region, and periodontal structures were visibly healthy (Fig. 3i).
Discussion
Root fractures occur as a consequence of direct trauma on the jaws or individually on the proper tooth, because of automobile accidents, sporting activity, violence, or malocclusion. Pathologic factors may also be involved. Commonly, teeth with fractured roots present slight extrusion. In some situations, fractured teeth show displacement to the palatine or lingual region and mobility. The final clinical diagnosis is always established through radiographic examination. In our cases, we did not observe dental extrusion. In case 1, there was a discrete root fracture, while in the subsequent cases the reference point was lost. In case 2, the adjacent tooth presented a fracture crown and in case 3, the patient received emergency oral care and showed a fractured tooth bonded to the adjacent tooth. Isolated transversal fracture is the most common form, as observed in our cases, although oblique line or multiple fractures can also occur. Clinical symptomatology is variable, depending on the severity of trauma and damage extension in dental structures. In the presented cases, the symptoms varied from cold-induced sensitivity to spontaneous pain. The cases with more sensitivity were those that presented greater diastases between the fractured fragments.
Complete clinical and radiographic examinations combined with a correct diagnosis of dental pulp status are fundamental for the success in root fracture prognosis. Generally, the root fracture treatment is performed in two steps. If the fractured tooth presents mobility and/or displacement, an immediate repositioning and immobilization of fracture should be accomplished. According to dental pulp status, the rigid reduction should be followed by endodontic treatment. After these trials, the patients should be under clinical and radiographic follow-up to assess the healing status. In the first month, they should be observed weekly, and radiographic examinations, tests of pulp sensibility, and dental mobility should be performed. Later, they should remain under periodical control every 6 months for 5–10 years. During this period, patients who present inflammatory symptoms related to pulp tissue should undergo endodontic treatment. After clinical and radiographic examinations, if the apical fragment shows evidence of pulp vitality (detected by the presence of hard lamina and pain during the exploration) only the cervical root portion should be treated.
The process of healing after a root fracture begins on the local of pulp and periodontal involvement. If no infectious process is observed, healing would occur by the formation of hard tissue and/or by the interposition of connective tissue between the two fractured fragments. In this respect, Andreasen and Hjørting-Hansen classified fracture healing into four groups: (i) with hard tissue; (ii) with interposition of hard and soft tissue between fragments; (iii) with interposition of soft tissue; and (iv) no healing.
After a root fracture, the apical fragment remains vital in approximately 99% of cases, while the pulp tissue on the cervical fragment can develop necrosis with consequent formation of granulation tissue between the fragments. The ideal repair process should be the formation of hard tissue between the two fragments, creating a functional unit with normal dental mobility and pulp vitality. Nevertheless, the interposition of connective tissue is also efficient, corresponding to the most common healing type. In the present study, different fracture healings were verified according to the severity and attendance time after the trauma. In case 1, we observed healing with hard tissue and preservation of pulp vitality in both fragments; in case 2, interposition of hard and soft tissue with necrosis of cervical fragment and in case 3, interposition of granulation tissue and necrosis of both fractured fragments, leading to surgical removal of the apical fragment.
Generally, root fractures present good prognosis, as a large communication between the pulp and periodontal tissue is formed, characterizing the fracture line. This process promotes the reestablishment of collateral circulation and drains the edema caused by trauma, thus decreasing tension in the pulp vessels. Teeth with root fractures show more chances of maintaining pulp vitality than non-fractured luxated teeth. However, there are a large number of variables that can influence the prognosis of root fractures. Hard tissue healing is usually efficient in teeth with no more than one-half root formation, in young patients, in non-displaced teeth, and when no mobility of coronal fragment is observed. Moreover, the presence of pain with great separation between the two fragments is associated with high possibility of pulp necrosis, decreasing the chance of hard tissue healing. Another important factor in teeth prognosis is the location where the fracture occurred. Horizontal root fractures situated on the middle or apical third of the root present better prognosis when compared with vertical fractures. In the present cases, hard tissue healing occurred only in case 1, in which the patient was attended immediately after the trauma and presented discrete diastasis, absence of mobility, and dental pulp with normal vitality. In contrast, the remaining cases showed greater diastasis, leading to necrosis of the cervical fragment. In case 2, the healing consisted of hard and soft tissue interposition between the fragments and in case 3, we could observe complete pulp necrosis of the cervical and apical fragments.
The aim of the splinting procedure is to completely immobilize the traumatized region and it is used in situations that show tooth mobility or after repositioning of dislodged tooth. The splint type seems to be related to root fracture prognosis. Some authors found that the use of cap splints caused an increase in pulp necrosis, probably due to the additional trauma produced by impression and cementation of this type of splint. The splinting period varied according to the severity of each case. However, the use of splints beyond 3–4 weeks seems to be unnecessary. In our cases, splinting for 3 months was used only in case 3 who presented dental mobility. We used an excessive period of splinting because the apical fragment of the tooth was surgically removed. The use of antibiotics seems not to influence root fracture prognosis.
In summary, the presented cases of root fractures showed good prognosis. Correct diagnosis, clinical management and subsequent radiographic follow-up are essential for the success of treatment.
Authors: Marco Aurélio Versiani, Cássio José Alves de Sousa, Antônio Miranda Cruz-Filho, Danyel Elias da Cruz Perez, Manoel Damião Sousa-Neto
References:
- Çaliskan MK, Pehelivan Y. Prognosis of root-fractured permanent incisors. Endod Dent Traumatol 1996;12:129–36.
- Yates JA. Root fractures in permanent teeth: a clinical review. Int Endod J 1992;25:150–7.
- Andreasen JO, Andreasen FM. Textbook and color atlas of traumatic injuries to the teeth. Copenhagen, Denmark: Munksgaard; 1994. p. 750.
- Andreasen JO, Andreasen FM, Mejàre I, Cvek M. Healing of 400 intra-alveolar root fractures. 2. Effect of treatment factors such as treatment delay, repositioning, splinting type and period and antibiotics. Dent Traumatol 2004;20:203–11.
- Jin H, Thomas HF, Chen J. Wound healing and revascularization. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;81:26–30.
- Bender IB, Freedland JB. Clinical considerations in the diagnosis and treatment of intra-alveolar root fractures. J Am Dent Assoc 1983;107:595–600.
- Andreasen FM. Pulpal healing after luxation injuries and root fracture in the permanent dentition. Endod Dent Traumatol 1989;5:111–31.
- Feiglin B. Clinical management of transverse root fracture. Dent Clin North Am 1995;39:53–78.
- Andreasen JO, Hjørting-Hansen E. Intra-alveolar root fractures: radiographic and histologic study of 50 cases. J Oral Surg 1967;25:414–26.
- Andreasen JO, Andreasen FM, Mejàre I, Cvek M. Healing of 400 intra-alveolar root fractures. 1. Effect of pre-injury and injury factors such as sex, age, stage of root development, fracture type, location of fracture and severity of dislocation. Dent Traumatol 2004;20:192–202.
- Mata E, Gross MA, Koren LZ. Divergent types of repair associated with root fractures in maxillary incisors. Endod Dent Traumatol 1985;1:150–3.
