Micro-CT analysis of danger zone thickness in the mesiobuccal roots of maxillary first molars
Abstract
Aim: To evaluate dentine thickness from both distal (‘danger zone’) and mesial (‘safety zone’) aspects of the MB1 and MB2 canals of maxillary first molars at the furcation level using micro-CT imaging.
Methodology: One hundred maxillary first molars with two canals in the MB root were selected from a Brazilian subpopulation and scanned at a resolution of 19.6 μm in a micro-CT device. From each specimen, two axial cross-sectioned images were selected at 2 and 3 mm apical to the furcation level of the MB root and evaluated for the smallest dentinal thickness. Measurements were made from the outer perimeter of the MB1 and MB2 canals towards the external root surface from both distal (danger zone) and mesial (safety zone) aspects of the root. The influence of an isthmus was also considered in the analysis, and samples were classified according to the presence or absence of an isthmus in the axial sections. Non-parametric Wilcoxon signed-rank tests were used to compare dentinal thickness between MB1 and MB2 canals with a significant level set at 5%. Colour-coded 3D models of dentine thickness throughout the MB root were created and evaluated qualitatively.
Results: At both levels, median dentine thickness of the MB2 canal was significantly lower in both distal and mesial aspects of the root in comparison with the MB1 canal (P < 0.01). The presence of an isthmus was not a variable that influenced dentinal thickness. Colour-coded models indicated that dentine thickness was dependent on the cross-sectional shape of the MB root. At least 50% of the sample had <1 mm of dentine thickness at the danger zone of the MB2 canal.
Conclusions: Danger zones in the MB roots of maxillary first molars were not symmetrical. MB2 canals had less dentine thickness on both aspects of the root compared to the MB1 canal.
Introduction
The anatomy of maxillary first molars is complex, and root canal treatment is a major challenge for clinicians from both conventional and surgical approaches (Vertucci 2005). Numerous publications using different methodological approaches have discussed the complexity of the internal morphology of this group of teeth, especially the occurrence of a second canal in the mesiobuccal root (MB2; Weine et al. 1969, Cleghorn et al. 2006). Moral (1915) reported the presence of this additional canal in 63% of maxillary molars; however, the prevalence of MB2 canals in maxillary first molars has been reported to be as high as 90% (Stropko 1999, Cleghorn et al. 2006) and persistence of endodontic disease associated with this tooth is often related to the presence of an untreated MB2 canal (Weine et al. 1969, Karabucak et al. 2016).
Because of secondary dentine apposition over time, the MB2 orifice is smaller than the MB1 canal (Degerness & Bowles 2010) and is often covered by a ledge of dentine. From the orifice, the canal deviates palatally before curving abruptly back to the centre and apically (Vertucci 2005). According to Degerness & Bowles (2010), the mesiodistal diameter of the MB1 canal at the cervical third is 0.81 mm, whilst the MB2 can be as low as 0.24 mm at the same level. These anatomical features make location and negotiation of these canals challenging, demanding technical expertise and the appropriate equipment, such as operating microscopes, ultrasonic tips, chamber floor staining, long-shank round burs, modified chamber access (Stropko 1999, Vertucci 2005) and reciprocating instruments (Zuolo et al. 2015).
Mechanical instrumentation of the root canal space has always been associated to some degree with coronal canal transportation mainly in curved root canals (Bergmans et al. 2003); thus, an exhaustive anatomical study of the danger zone in the mesiobuccal root of maxillary molars is mandatory to reduce the risk of perforation towards the furcation area and to avoid decreasing the resistance of the root to fracture.
Although several morphological aspects of the MB root of maxillary first molars have been investigated (Cleghorn et al. 2006), there are limited reports addressing dentine thickness at the furcation level, also called ‘danger zone’, in this group of teeth (Degerness & Bowles 2010). In this context, micro-CT technology is of special interest, because this technique allows precise and reliable cross-sectional and three-dimensional analysis of the root canal system without damaging the tooth. Thus, the aim of this study was to evaluate the dentine thickness from both distal (‘danger zone’) and mesial (‘safety zone’) aspects of the MB1 and MB2 canals of maxillary first molars at the furcation level using micro-CT imaging system.
Material and methods
After ethics committee approval (Protocol No. 131-2010), 100 maxillary first molars extracted for reasons not related to this study and having two root canals in the MB root (MB1 and MB2), connected or not by an isthmus, were selected from a Brazilian subpopulation. Gender and age were unknown. Each specimen was scanned in a micro-CT device (SkyScan 1174v2; Bruker-microCT, Kontich, Belgium) using an isotropic resolution of 19.6 μm at 50 kV and 800 mA through 360° rotation around the vertical axis, rotation step of 0.8° and 1304 9 1024 pixels resolution. The acquired projections were reconstructed into cross-sectional slices with NRecon v.1.6.3 software (Bruker-microCT) using standardized parameters.
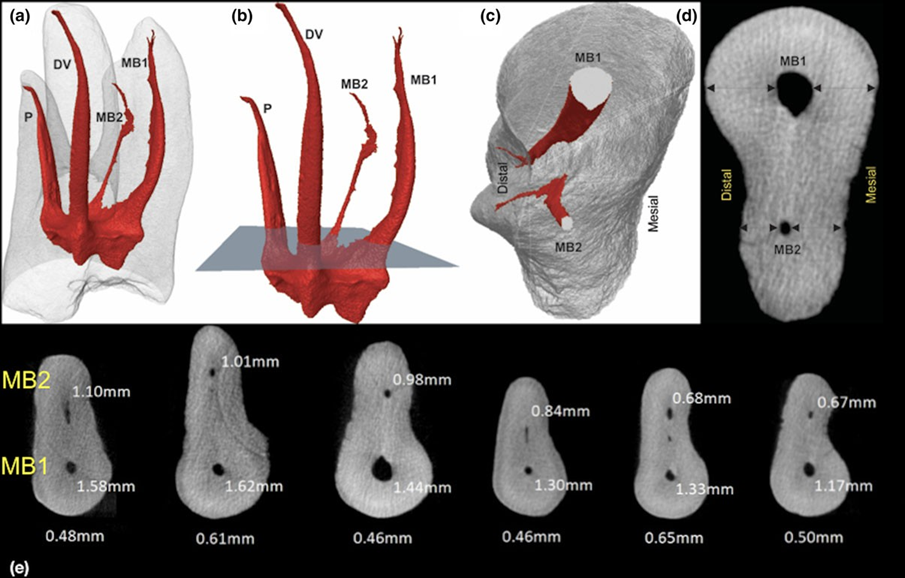
From each specimen, two axial cross-sectioned images were selected at 2 and 3 mm apical to the furcation level of the MB root and evaluated for the smallest dentinal thickness. Measurements were made from the outer perimeter of the MB1 and MB2 canals towards to the external root surface limit from both distal (danger zone) and mesial (safety zone) aspects of the root (Fig. 1) by a single operator using Data-Viewer v.1.5.2.4 software (Bruker-microCT). In addition, the influence of the isthmus was also considered for analysis and samples were classified according to the presence or absence of an isthmus in the axial sections.
The same evaluator who was blind to the first analysis repeated this procedure 4 weeks later and the average of the two measurements was recorded. A further evaluation was done if the difference was >50 μm between both measurements. Additionally, representative colour-coded 3D models of dentine thickness throughout the MB root were created by CTAn v.1.14.4 software (Bruker-microCT) and evaluated qualitatively (CTVol v.2.2.1; Bruker-microCT).
Statistical analysis
Considering that normality assumptions could not be verified (Shapiro–Wilk test; P < 0.05), results of thickness analyses were described in terms of median and range. The non-parametric Wilcoxon signed-rank test was used to compare dentinal thickness related to the MB1 and MB2 canals with a significant level set at 5%.
Results
Table 1 and Fig. 2 show the dentine thickness values of the 100 samples measured from MB1 and MB2 root canals at 2 and 3 mm apical to the furcation level. At both levels, the median dentine thickness of the MB2 canal was significantly lower in either distal or mesial aspects of the root in comparison with the MB1 canal (P < 0.01). Overall, MB2 canals were 250–260 μm thinner at the danger zone and 160–200 μm thinner at the safety zone compared to MB1 canals. In addition, at least 50% of the samples had dentine thickness values less than 1 mm at the danger zone and 26 roots had <1 mm of dentine thickness at the safety zone of the MB2 canal (Table 1).
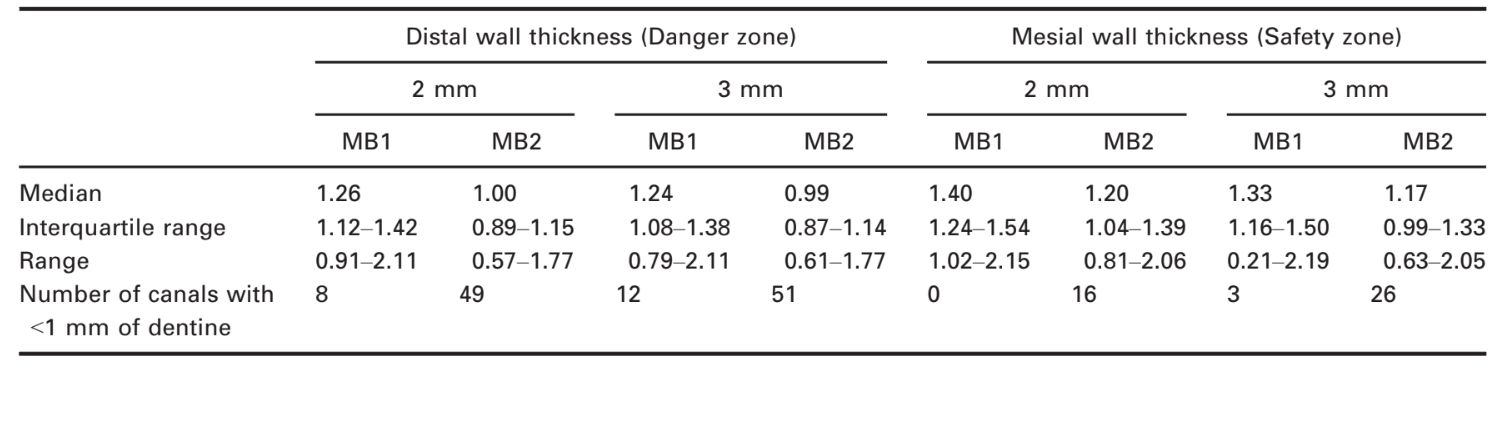
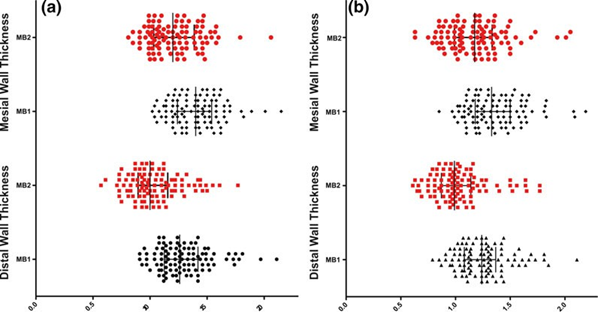
The presence of an isthmus did not influence dentinal thickness. The MB2 canal had lower values of dentine thickness in the presence or absence of an isthmus. Forty-one samples had an isthmus in the MB root at the 2-mm level and 53 at the 3-mm level. The average dentine thickness at the MB2 danger zone level was 190 μm thinner compared to the MB1 at the 2-mm furcation level and 180 μm thinner at the 3-mm level (P < 0.01). Differences between dentine thickness of MB2 and MB1 canals without an isthmus were also significant (P < 0.01).
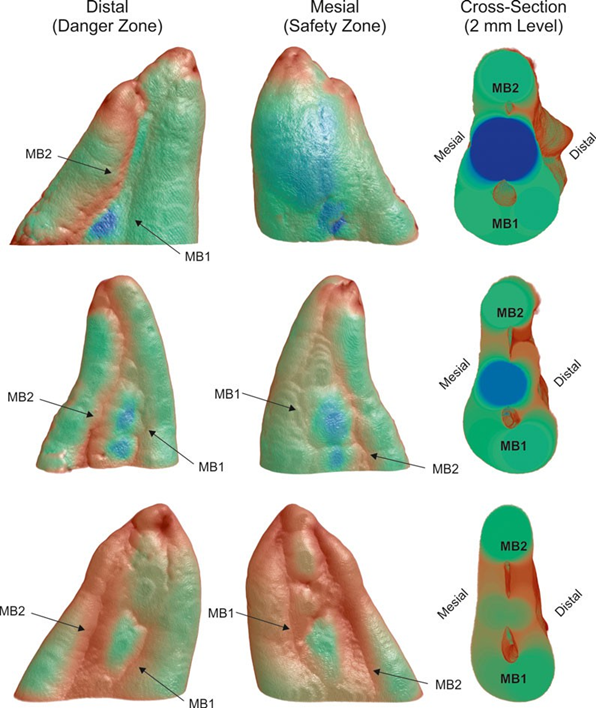
Figure 3 shows a colour-coded models depicting dentine thickness throughout the MB root of three representative maxillary first molars. Thick structures are indicated in blue and green, whereas red indicates areas of thin dentine, outlining the pathway of the MB2 canal in both aspects of the root.
Discussion
Contemporary procedures in restorative dentistry focus on preventing excessive loss of coronal tooth tissue, so as to minimize structural failure (Sorensen & Martinoff 1984, Real Dias et al. 2018). Loss of tooth structure at the cervical region has been considered an important aetiologic factor that may lead to vertical root fracture (Reeh et al. 1989). Consequently, conservative access and canal preparations have been suggested to preserve tooth structure in this area (Clark & Khademi 2010, Plotino et al. 2017).
Although information regarding danger zones and dentine thickness is scarce for the MB roots of maxillary first molars (Degerness & Bowles 2010), several publications on this subject are available for the mesial root of mandibular molars. Using micro-CT technology, Harris et al. (2013) reported that the dentine thickness 1.5 mm below the furcation area ranged from 0.81 to 1.22 mm on the distal aspect of the mesial root. These data were confirmed by Garala et al. (2003) who reported a mean value of 1.27 0.27 mm. In both studies, no differences were observed in dentine thicknesses between the mesiobuccal and mesiolingual root canals. In the present study, 100 mesiobuccal roots of maxillary first molars with two root canals (MB1 and MB2) were evaluated. The dentine thickness on the distal aspect of the MB2 canal (danger zone) varied from 0.57 to 1.77 mm (median 1.00 mm) and from 0.61 to 1.77 mm (median 0.99 mm) at the levels evaluated. It was also demonstrated that dentine thickness of the MB2 canal was significantly thinner (0.20–0.25 mm) than the MB1 canal on both aspects of the root. This result differs from the reported values of mandibular molars in which the dentine thickness was similar for both mesial canals (Harris et al. 2013). Thus, MB roots of maxillary molars can be considered to have an asymmetrical shape, in comparison with mesial roots of mandibular molars.
Considering the high prevalence of MB2 canals in maxillary first molars, the present findings emphasize the need to establish a safe shaping protocol when tapered rotary or reciprocating NiTi instruments are used. Although several micro-CT studies have reported safe enlargement of the MB1 canal with several rotary systems (Peters et al. 2001, 2003, Peters & Paqué 2011), to date, there are no laboratory studies addressing the remaining dentine thickness related to the MB2 canal after preparation. According to the present results, the MB2 canal has on average a dentine thickness 250 μm less than the MB1 canal. Consequently, clinicians may benefit from preoperative cross-sectional images that show the dentine thickness of the MB root acquired from CBCT scans, even if this protocol has not been recommended for every patient (Hiebert et al. 2017). Considering the nontapered morphology and the thin dentine walls of the MB2 canal at the furcation level of maxillary first molars, mechanical preparation procedures may require adjustments to avoid procedural errors.
One limitation of the present study is the fact that the analysis was exclusive to the critical zone of the furcation area and not the entire root. A full root assessment is a valid recommendation for future research.
Conclusions
The danger zone in the MB root of the maxillary first molars is asymmetrical. MB2 canals had significant less dentine thickness in both mesial (safety zone) and distal (danger zone) aspects of the root compared to the MB1 canal.
Authors: R. Ordinola-Zapata, J. N. R. Martins, M. A. Versiani, C. M. Bramante
References:
- Bergmans L, Van Cleynenbreugel J, Beullens M, Wevers M, Van Meerbeek B, Lambrechts P (2003) Progressive versus constant tapered shaft design using NiTi rotary instruments. International Endodontic Journal 36, 288–95.
- Clark D, Khademi J (2010) Modern molar endodontic access and directed dentin conservation. Dental Clinics of North America 54, 249–73.
- Cleghorn BM, Christie WH, Dong CC (2006) Root and root canal morphology of the human permanent maxillary first molar: a literature review. Journal of Endodontics 32, 813– 21.
- Degerness RA, Bowles WR (2010) Dimension, anatomy and morphology of the mesiobuccal root canal system in maxillary molars. Journal of Endodontics 36, 985–9.
- Garala M, Kuttler S, Hardigan P, Steiner-Carmi R, Dorn S (2003) A comparison of the minimum canal wall thickness remaining following preparation using two nickel-titanium rotary systems. International Endodontic Journal 36, 636–42.
- Harris SP, Bowles WR, Fok A, McClanahan SB (2013) An anatomic investigation of the mandibular first molar using micro-computed tomography. Journal of Endodontics 39, 1374–8.
- Hiebert BM, Abramovitch K, Rice D, Torabinejad M (2017) Prevalence of second mesiobuccal canals in maxillary first molars detected using cone-beam computed tomography, direct occlusal access, and coronal plane grinding. Journal of Endodontics 43, 1711–5.
- Karabucak B, Bunes A, Chehoud C, Kohli M, Setzer F (2016) Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: a cone-beam computed tomography study. Journal of Endodontics 42, 538–41.
- Moral H (1915) Ueber das Vorkommen eines vierten Kanals in oberen Molaren. ÖstUng Vschr Zahnheilk 33, 313–25. Peters OA, Paqué F (2011) Root canal preparation of maxillary molars with the self-adjusting file: a micro-computed tomography study. Journal of Endodontics 37, 53–7.
- Peters OA, Schönenberger K, Laib A (2001) Effects of four Ni-Ti preparation techniques on root canal geometry assessed by micro computed tomography. International Endodontic Journal 34, 221–30.
- Peters OA, Peters CI, Schönenberger K, Barbakow F (2003) ProTaper rotary root canal preparation: effects of canal anatomy on final shape analysed by micro CT. International Endodontic Journal 36, 86–92.
- Plotino G, Grande N, Isufi A et al. (2017) Fracture strength of endodontically treated teeth with different access cavity designs. Journal of Endodontics 43, 995–1000.
- Real Dias MC, Martins JNR, Chen A, Quaresma SA, Luıs H, Carames J (2018) Prognosis of indirect composite resin cuspal coverage on endodontically treated premolars and molars: an in vivo prospective study. Journal of Prosthodontics 27, 598–604.
- Reeh ES, Messer HH, Douglas WH (1989) Reduction in tooth stiffness as a result of endodontic and restorative procedures. Journal of Endodontics 15, 512–6.
- Sorensen JA, Martinoff JT (1984) Intracoronal reinforcement and coronal coverage: a study of endodontically treated teeth. Journal of Prosthetic Dentistry 51, 780–4.
- Stropko JJ (1999) Canal morphology of maxillary molars: clinical observations of canal configurations. Journal of Endodontics 25, 446–50.
- Vertucci FJ (2005) Root canal morphology and its relationship to endodontic procedures. Endodontic Topics 10, 3–29.
- Weine FS, Healey HJ, Gerstein H, Evanson L (1969) Canal configuration in the mesiobuccal root of the maxillary first molar and its endodontic significance. Oral Surgery Oral Medicine Oral Patholology 28, 419–25.
- Zuolo ML, Carvalho MC, De-Deus G (2015) Negotiability of second mesiobuccal canals in maxillary molars using a reciprocating system. Journal of Endodontics 41, 1913–7.
