Second mesiobuccal root canal in maxillary molars—A systematic review and meta-analysis of prevalence studies using cone beam computed tomography
Abstract
Objective: To assess the influence of cone-beam computed tomographic (CBCT) voxel size and population demographic aspects (age, gender and geographic region) on the prevalence of the second mesiobuccal root canal (MB2) in maxillary first and second molars.
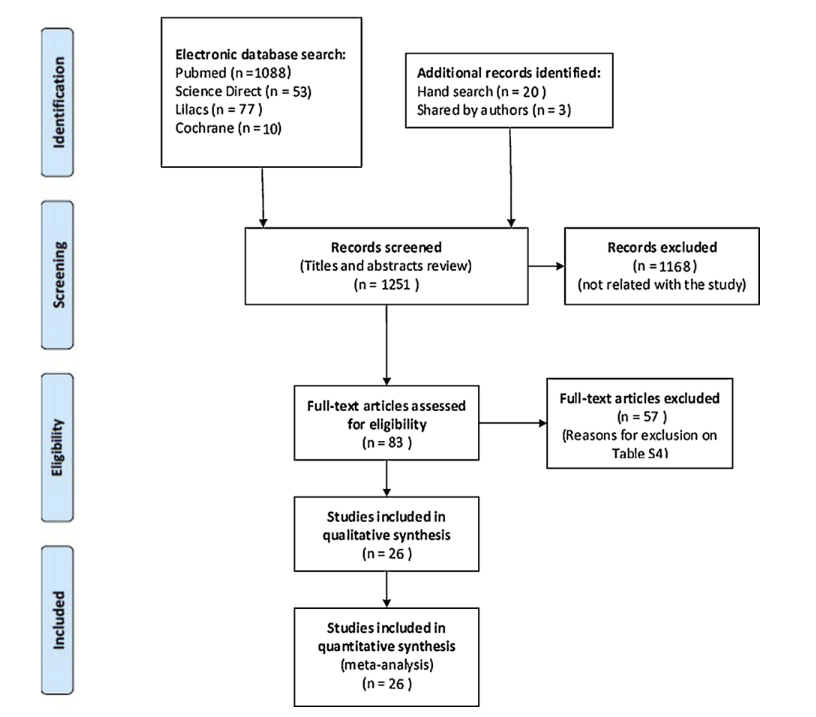
Design: Prevalence studies using CBCT technology on MB2 canal were searched between May and September 2019. The protocol was registered in PROSPERO. Four electronic databases and 5 peer-reviewed endodontic journals were screened. Authors were contacted and bibliographic references hand-searched. Eighty three studies were submitted to full text analysis and scientific merit evaluation by 2 evaluators using Joanna Briggs Institute Critical Appraisal tool. Twenty six studies were finally pooled into a meta-analysis. Forest plots with a 95% confidence interval were undertaken. Meta-regression was used to identify possible sources of heterogeneity and funnel plot visual analysis to assess publication bias.
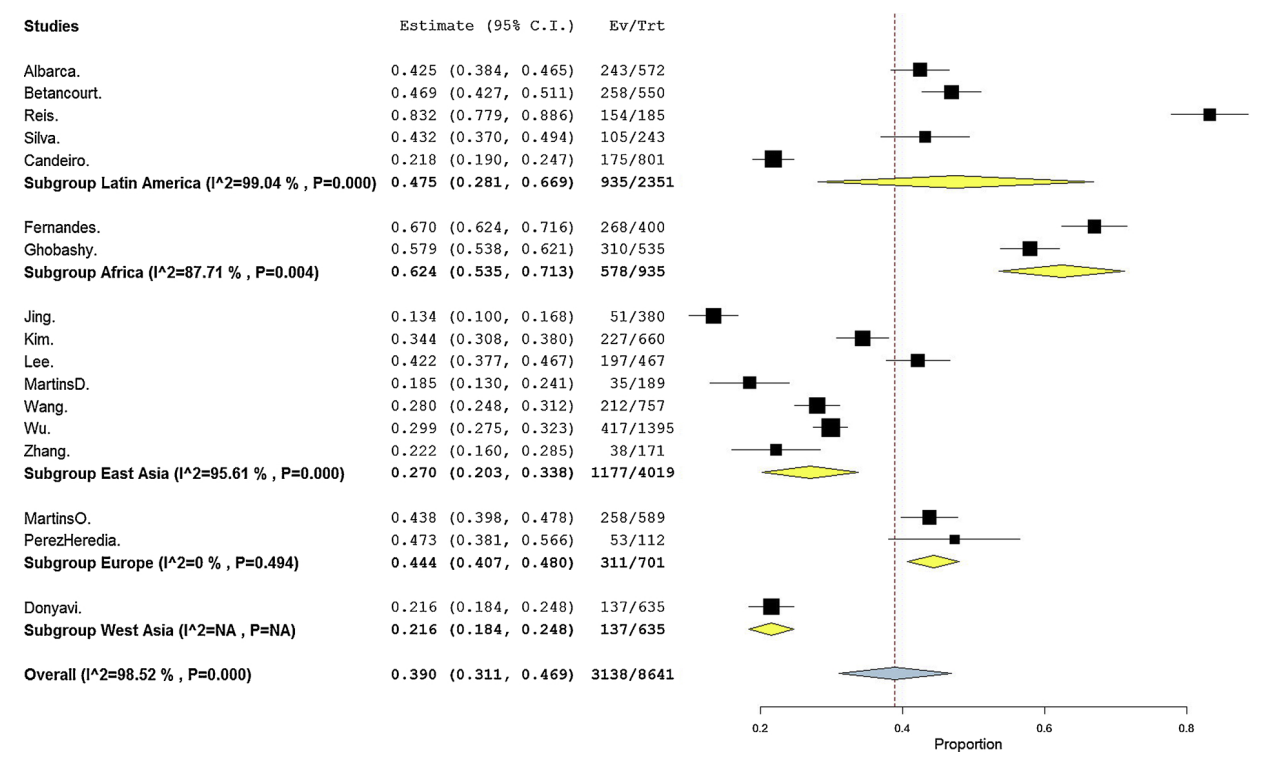
Results: The 26 studies reported anatomical data from the mesiobuccal root of 15,285 first molars and 8,641 second molars. Pooled prevalence of MB2 canal was higher in maxillary first molar (69.6%; 64.5%-74.8%) than in second molars (39.0%; 31.1%-46.9%) (p < 0.05). A significantly higher prevalence odds of having MB2 canal was detected in males (p < 0.05). Meta-regression excluded gender, age and voxel size as a source variance, but identified tooth group and geographic region as possible sources of heterogeneity.
Conclusion: MB2 canal prevalence was significantly higher in maxillary first molars. Males showed higher odds of having MB2 canal than females. Geographic region seemed to influence MB2 prevalence outcome. Knowing these preoperative factors would help to anticipate MB2 morphologies in clinics.
Introduction
In the last decades, the morphology of the mesiobuccal (MB) root of maxillary molars has been more extensively studied than any other root (Cleghorn, Christie, & Dong, 2006). This root commonly presents 2 main root canals, named MB1 and MB2, and a high incidence of fine anatomical structures including intercanal communications, loops, accessory canals and apical ramifications (Gu, Lee, & Spangberg, 2011), resulting in a very complex canal system. The orifice of the MB2 is usually located either mesial to or in the sub pulpal groove within 3.5 mm palatally and 2 mm mesially from MB1 (Gorduysus, Gorduysus, & Friedman, 2001), often hidden under the shelf of the dentine wall or calcifications in a small groove (Pattanshetti, Gaidhane, & Al Kandari, 2008). Consequently, it can be missed in routine clinical practice, especially without using magnification or special lighting equipment (Buhrley, Barrows, BeGole, & Wenckus, 2002). This inability to recognize its presence and to adequately treat it have been considered the major cause of failure in root canal therapy of maxillary molars (Huumonen, Kvist, Grondahl, & Molander, 2006; Karabucak, Bunes, Chehoud, Kohli, & Setzer, 2016; Wolcott, Ishley, Kennedy, Johnson, &Minnich, 2002). Clinicians, therefore, must be aware of MB2 prevalence and adopt procedural steps to locate and prepare it properly (Buhrley et al., 2002; Gorduysus et al., 2001). In the literature, percentage frequency of MB2 canal in maxillary molars has ranged from 10 to 95%, depending not only on the method used in the study, such as sectioning, dye injection, radiography, scanning electron microscopy, or micro-CT (Gu et al., 2011; Reis, Grazziotin-Soares, Barletta, Fontanella, & Mahl, 2013; Vertucci, 1984; Wolcott et al., 2005), but also on ethnic and demographic factors related to the studied population (Guo, Vahidnia, Sedghizadeh, & Enciso, 2014; Martins, Alkhawas, & Altaki, 2018), which may include geographic region, age and gender.
According to a joint position statement of the American Association of Endodontics and American Academy of Oral and Maxillofacial Radiology (AAE & AAOMR joint position statement, 2015) and, more recently, an updated consensus of an expert committee convened by the European Society of Endodontology (Patel, Brown, Semper, Abella, & Mannocci, 2019) regarding the use of CBCT in clinics, intraoral radiographs is still the imaging modality of choice for pre-operative diagnosis. However, small field of view (FOV) CBCT might be considered, for example, when complex anatomy is expectable and for non-surgical retreatment of cases with possible untreated canals. Nowadays, the gold-standard imaging technique to evaluate the presence of a MB2 canal in a clinical setup is indeed through the cone-beam computed tomographic (CBCT) (Lee, Kim, & Lee, 2011; Martins et al., 2018a; Reis et al., 2013). CBCT has been considered the most reliable tool to be used in observational in vivo studies as it allows to evaluate, in a consecutive manner, specific anatomical characteristics of all groups of teeth in large populations. However, an evidence-based background on the impact of some demographic characteristics of this anatomical feature in different populations using this new imaging technology has never been published. Therefore, the purpose of this systematic review and meta-analysis was to assess the influence of nominal CBCT resolution (voxel size) and specific demographic aspects of populations including age, gender, and geographic region, on the prevalence of the MB2 canal, by critically appraising cross-sectional studies that used CBCT technology as an objective analytical tool to ascertain root canal anatomy of the mesiobuccal root of maxillary first and second molars. The null hypotheses tested were that there was no difference between (i) gender, (ii) age, (iii) geographic region or (iv) image voxel size regarding the prevalence of MB2 canal in maxillary molars.
Material and Methods
This systematic review and meta-analysis was designed taking into consideration the AMSTAR 2 assessment tool (Kattan, Lee, Kohli, Setzer, & Karabucak, 2018; Shea, Reeves, & Wells, 2017). The review protocol was registered in PROSPERO with the identification CRD42018080827.
Search strategy and scientific merit assessment
Literature review followed a “3 stage assessment”. In the first stage, titles and abstracts of the studies were accessed and, considering pre-defined inclusion/exclusion criteria (Supplemental Table S1), were labeled as ‘relevant’ or ‘irrelevant’. In the second step, the full text of the relevant studies were analyzed and re-labeled according to the same criteria. In the third step, selected relevant studies were submitted to a critical appraisal considering their scientific merit.
Four electronic databases (PubMed, Science Direct, Lilacs and Cochrane Collaboration) were accessed from January 1990 to September 2019 and a search was undertaken for prevalence studies on root/canal anatomy using CBCT imaging. Supplemental Table S2 summarizes the terms and filters used in each database. The reference list from the relevant studies as well as the five peer-reviewed journals (International Endodontic Journal, Journal of Endodontics, Australian Endodontic Journal, Evidence Based Dentistry, and Journal of Evidence-Based Dental Practice) were also hand searched. Additionally, when available, authors from the included studies were contacted via email and asked for additional material from their research group, whether as a format of scientific articles or grey literature, or if they were aware of any on-going project which could be accessed. Literature search was conducted between May and August 2018, and updated at October 2019, without language restrictions.
The quality assessment of the selected studies followed the checklist for prevalence studies from the Joanna Briggs Institute (JBI) Critical Appraisal tool for use in systematic reviews (Munn, Moola, Lisy, Riitano, & Tufanaru, 2015). Two evaluators (JM and DM) independently assessed the eligible studies. Inter-rater reliability tests between both evaluators were undertaken with kappa above 0.674 (Supplemental Table S3), which is considered as good agreement. The assessment discrepancies were discussed until consensus was reached.
Statistical analysis
The pooled prevalence of MB2 was calculated based on the prevalence reported in the included studies. Data was analyzed using OpenMeta [Analyst] v. 10.10 (http://www.cebm.brown.edu/openmeta/) software and forest plots generated with untransformed proportions or prevalence odds ratio (OR) with the corresponding 95% confidence interval (CI) for each study. The overall random-effects (Dersimonian-Laird test) pooled estimate and CI were reported. The statistical heterogeneity among studies was assessed with Tau2 (estimate of between-study variance), Q-Cochran test according to Dersimonian and Laird (occurrence of heterogeneity), and I2 index for level of inconsistency, quantified as low (25%), moderate (50%), or high (75%). Meta-regression was conducted to identify sources of between-study heterogeneity (Higgins & Thompson, 2002; Higgins, 2011) in the pooled proportion estimates using tooth, age, geographic region and voxel size subgroups as explanatory variables. Funnel Plot visual analysis was undertaken to assess publication bias using RevMan software (RevMan v5.3.5; Cochrane Collaboration, Denmark). Statistical significance was set as 5%.
Results
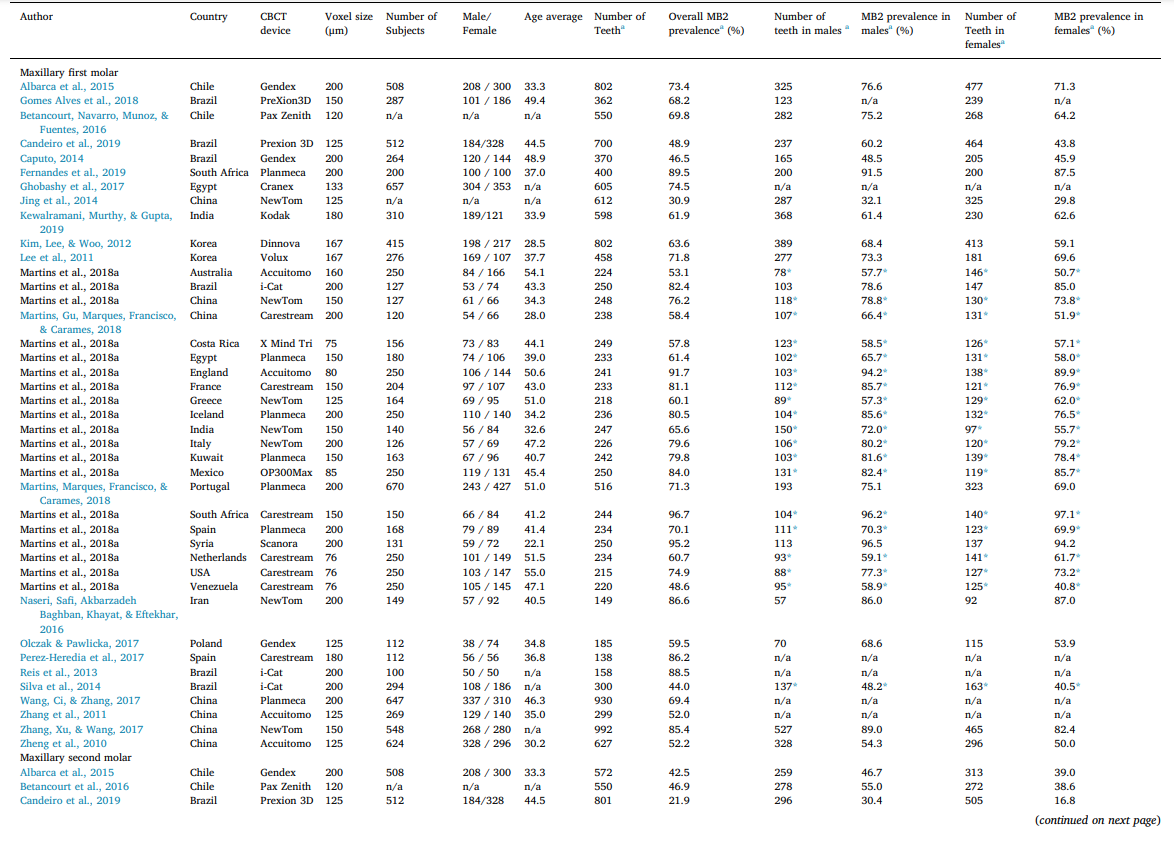
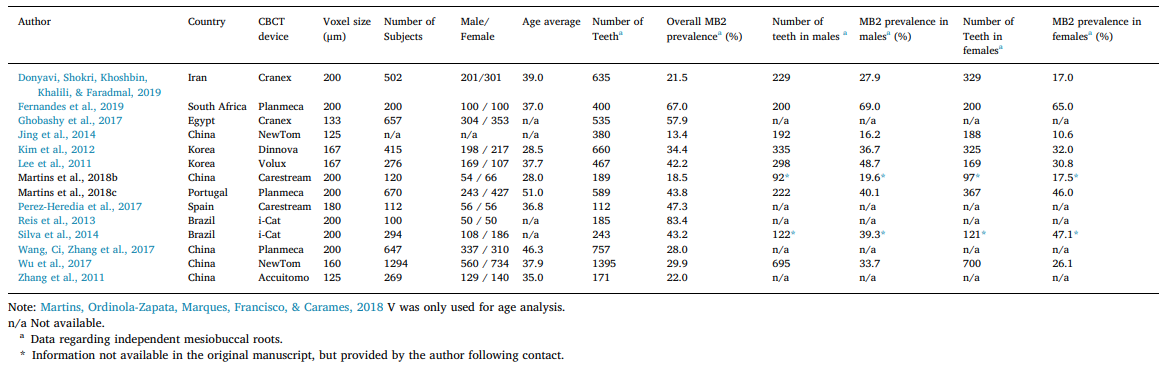
The electronic and manual searches identified 80 relevant studies. E-mail contact return rate with authors was 27.4% (17 replies out of 62 contacts) and 3 studies were added. From a full textual analysis of these 83 studies, 57 were excluded (Supplemental Table S4) and a final pool of 26 studies, with an average JBI score of 81.8%, were included in this review (Fig. 1). The included studies reported data of 23,926 maxillary molars (15,285 maxillary first molars and 8,641 maxillary second molars) from at least 12,456 patients, comprising 5,541 males and 6,915 females (2 studies did not report the number of patients). The average age of the patients was 40.9 years and was calculated based on 20 studies that reported this information. The included studies were published in English (n = 24), Chinese (n = 1) and Portuguese (n = 1) and represented data from 24 countries. Table 1 summarizes the overall results on the prevalence of MB2 canal according to tooth group, age, gender, geographic region, and image voxel size.
Overall prevalence of MB2 canal
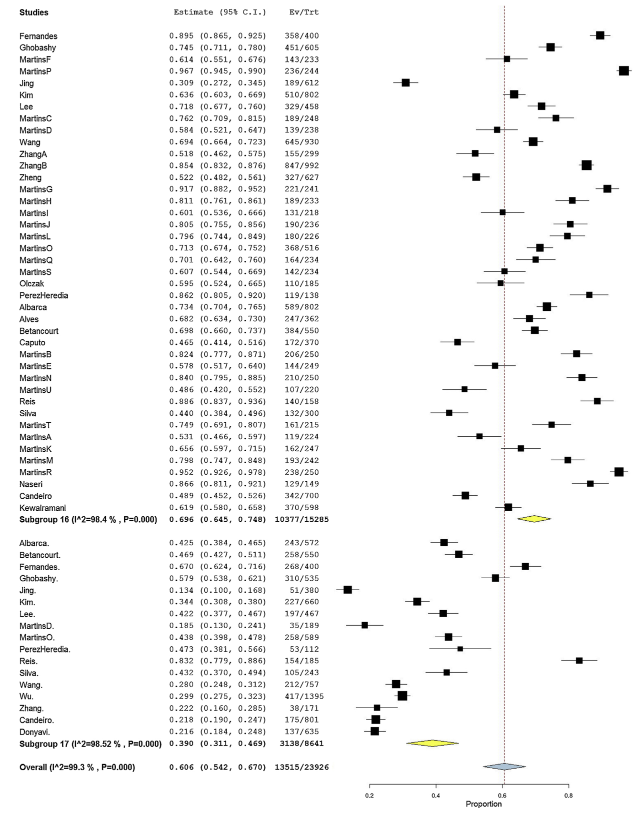
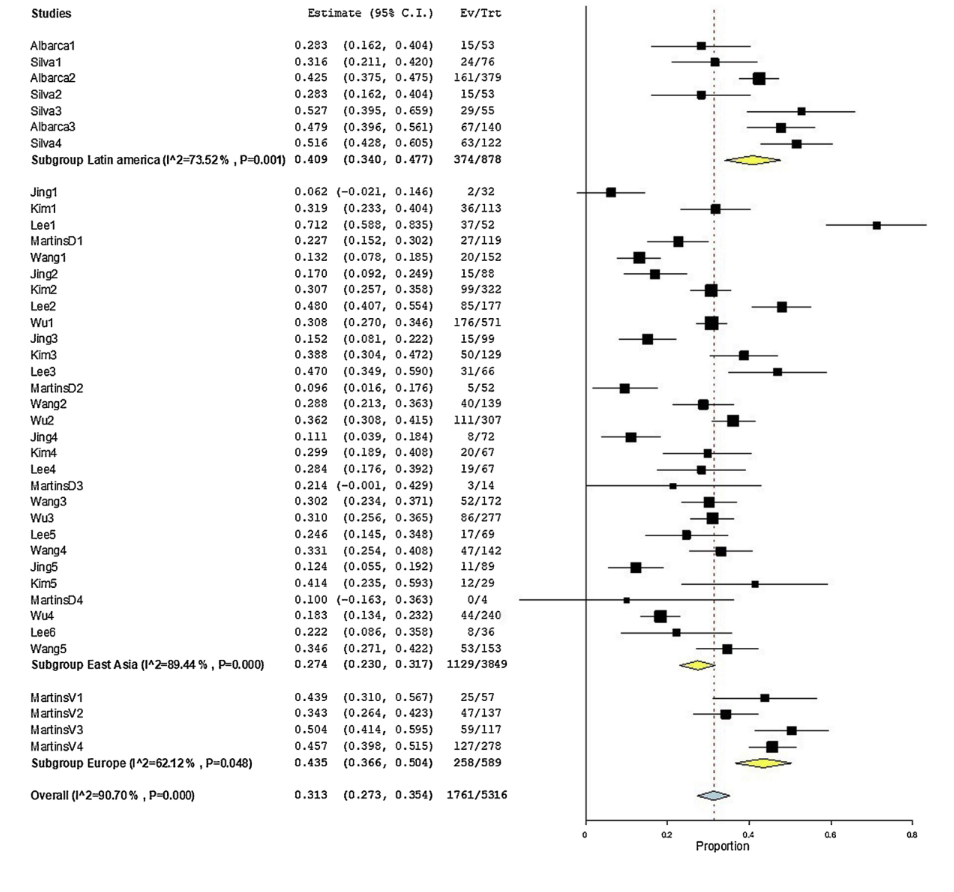
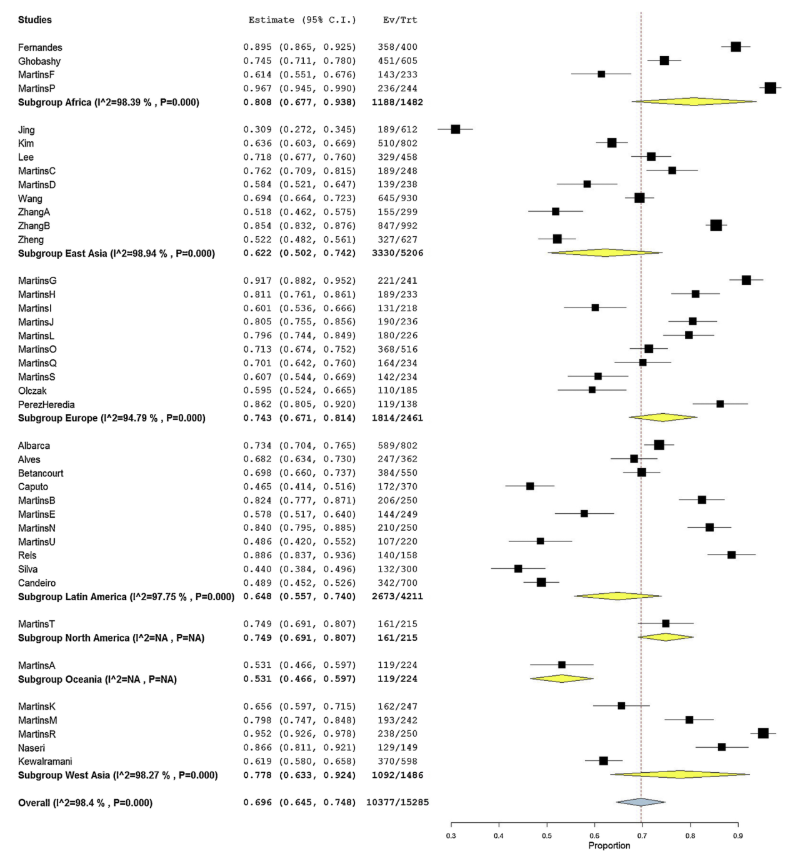
The presence of MB2 canal in maxillary first molars were addressed in 22 studies (41 population groups) with a pooled prevalence of 69.6% (64.5%-74.8%) and high heterogeneity value (I2 = 98.4%), while MB2 in maxillary second molars was reported in 16 studies (17 population groups) with a pooled prevalence of 39.0% (31.1%-46.9%) and also a high heterogeneity (I2 = 98.5%). Prevalence of MB2 canal in maxillary first molars was significantly higher compared to the second molars (p < 0.05) (Fig. 2).
MB2 canal and gender
Influence of gender on the prevalence of MB2 canal in maxillary first molars was compared in 16 studies (35 population groups). Statistical comparison of untransformed proportions of MB2 for males (71.9%; 66.5%-77.4%) and females (66.8%; 60.4%-73.2%) was not significant (p > 0.05). The overall heterogeneity was high with an I2 value of 97.7% (Fig. 3). These studies were pooled in a prevalence odds ratio forest plot (Fig. 4) which significantly favored females with lower odds of having a MB2 root canal than males (OR = 1.324; 1.208-1.452 CI 95%) (p < 0.05), and also a very low heterogeneity [(Tau² = 0.00; Chi² = 41.74, df = 34 (p = 0.17); I² = 18.54%)].
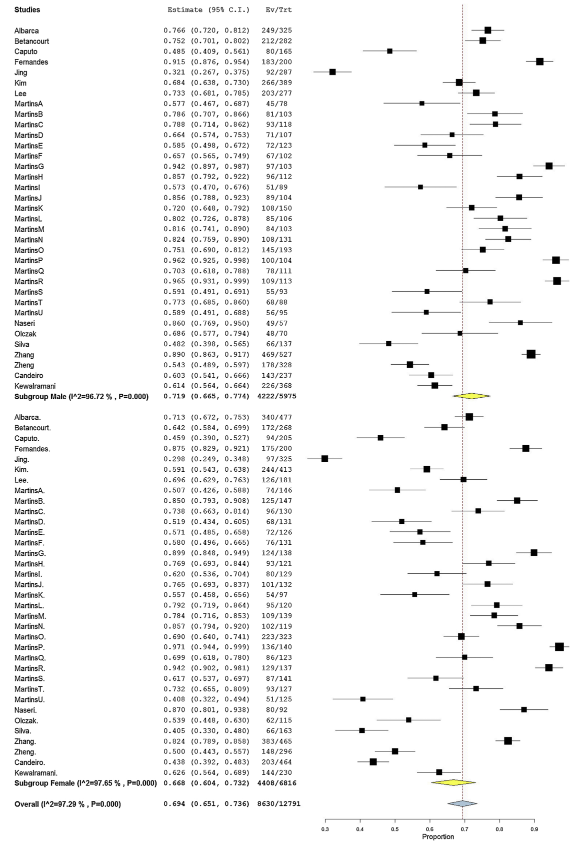
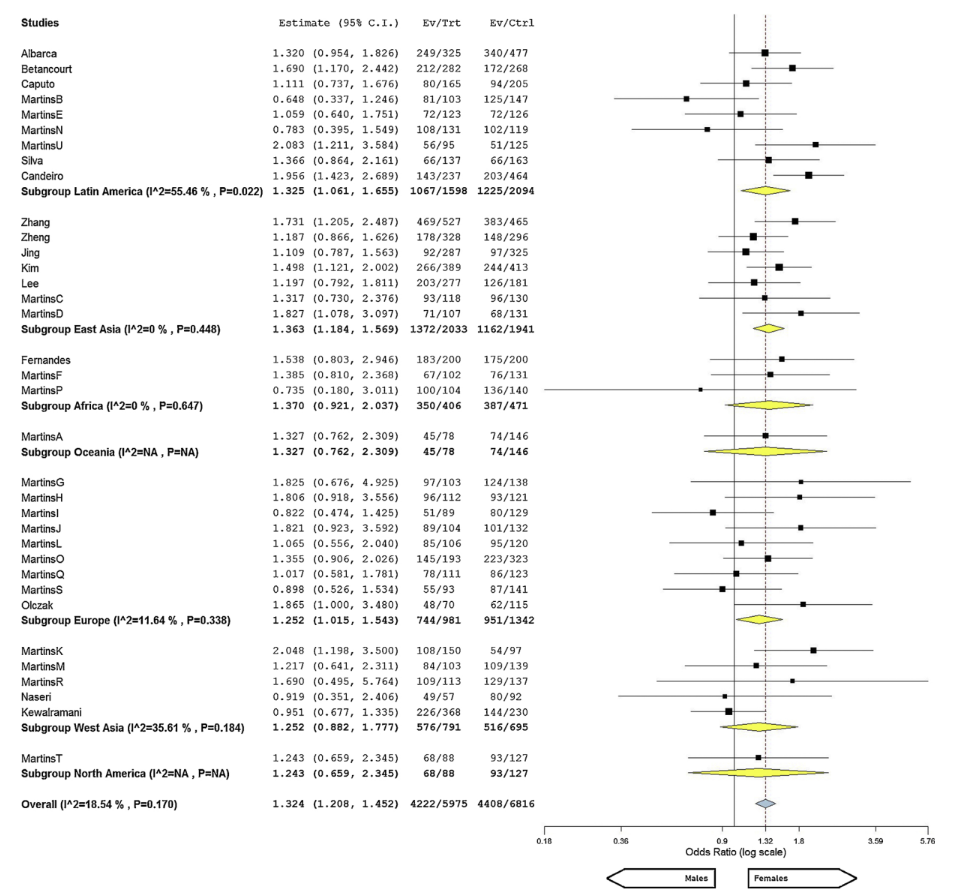
rhombus shapes represent the combined results for each sub-group or overall analysis, respectively, while the vertical black line represents the no-effect line. The
yellow shape not overlapped onto the no-effect line represent results with statistically significant differences on the odds ratio between the two groups under
comparison).
Meta-regression analysis was undertaken to assess gender and region as possible confounding factors in the heterogeneity of the MB2 prevalence in maxillary molars. In maxillary first molars, gender meta- regression omnibus p-value (0.180) displayed a non-significant effect in the prevalence variance explanation, with females presenting -5.1% [-12.5%-2.4%] MB2 root canals compared to males. On the other hand, meta-regression omnibus p-value for geographic region (0.002) revealed it as a possible source for prevalence variance of the included studies.
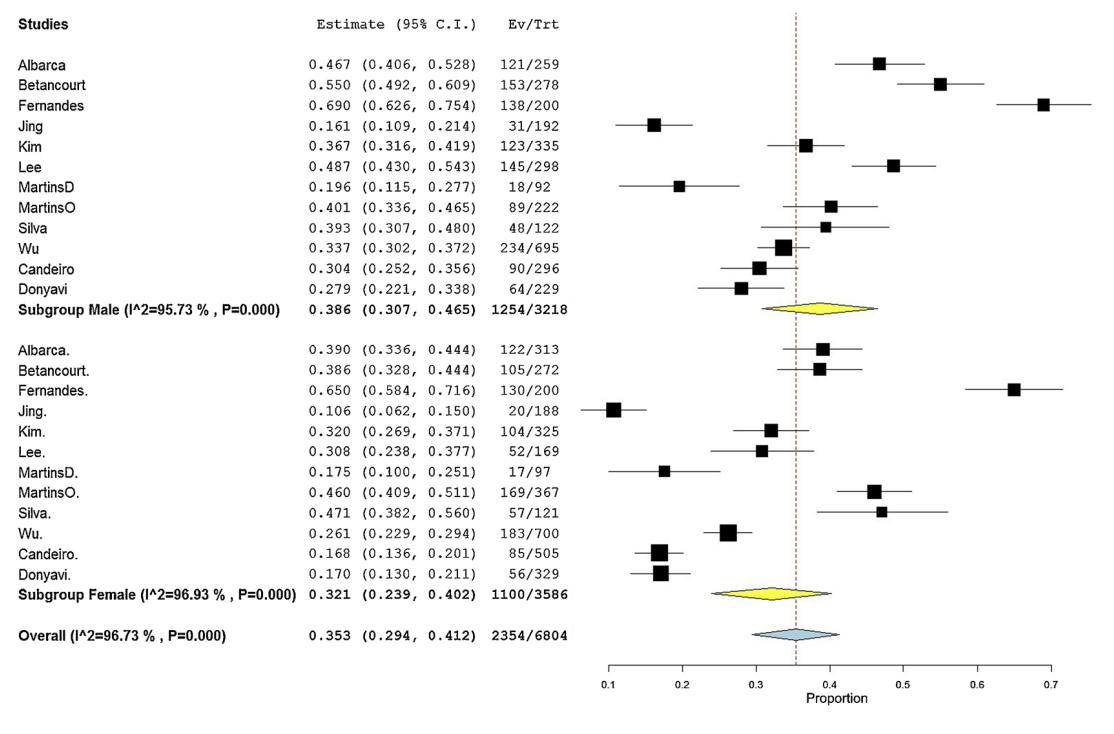
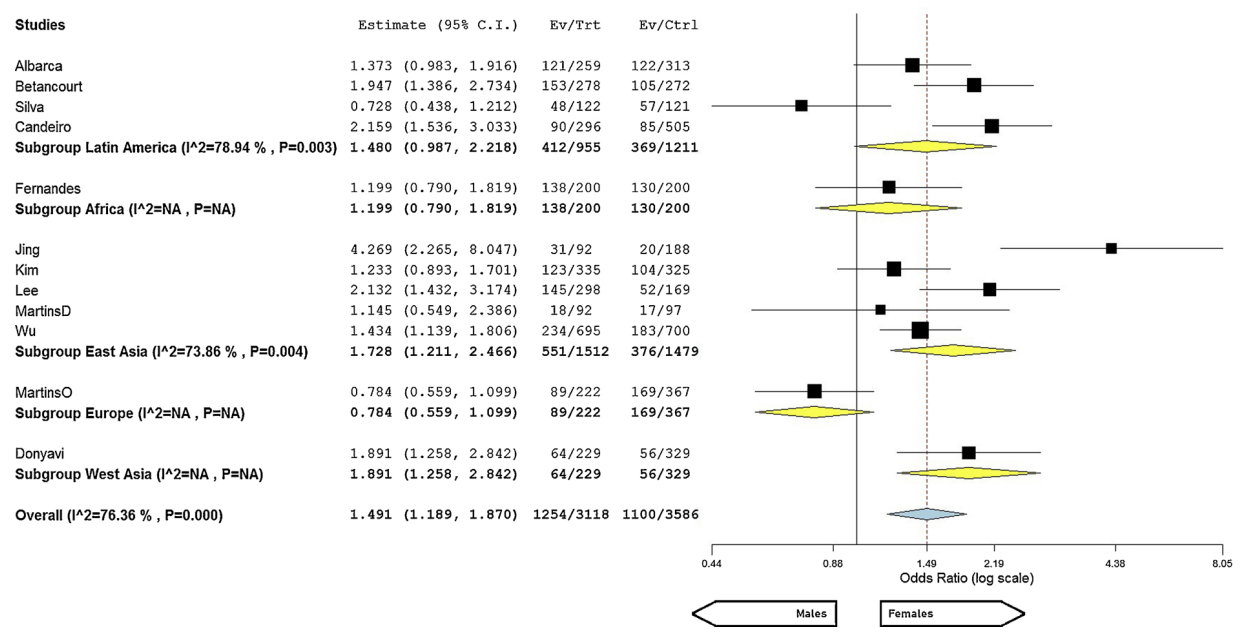
Meta-analysis calculation of 11 studies (12 population groups) on MB2 canal in maxillary second molars showed a high heterogeneity value (I2 = 96.7%) and no statistical difference in its prevalence when comparing males (38.6%; 30.7%-46.5%) with females (32.1%; 23.9%- 40.2%) (Fig. 5) (p > 0.05). Odds ratio favored females with significantly lower odds of having MB2 canal than males (OR = 1.491; 1.189-1.870 CI 95%) (p < 0.05), although with moderate heterogeneity [Tau² = 0.07; Chi² = 46.53, df = 11 (P < 0.001); I² = 76.36%]. Similarly to maxillary first molars, gender meta-regression omnibus p-value (0.275) excluded this factor as source variance for this group of teeth, but indicated geographic region (omnibus p-value < 0.001) as a possible source of explainable heterogeneity. Funnel plots in both maxillary molars did not detect publication bias (Supplemental Figure S1).
MB2 canal and age
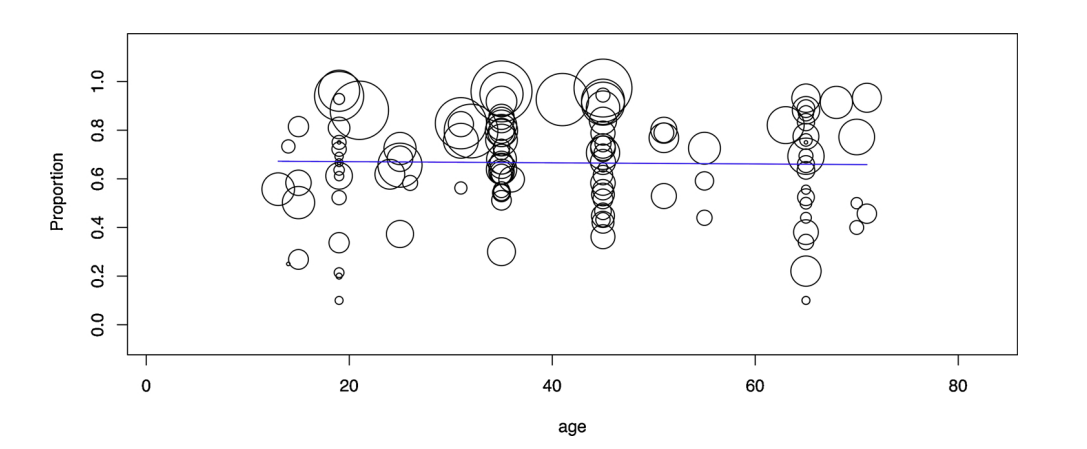
The influence of age on the prevalence of the MB2 canal in maxillary first molars was assessed in 11 studies from 30 population groups.
However, considering that authors reported 123 different age intervals, meta-regression calculation of age as a continuous variable was performed using the middle age value calculated to each one of these intervals. The subgroups were ordered by age increasing and pooled in a forest plot chart according to geographic regions. Overall prevalence of MB2 was 66.6% (63.3%-70.0%) with a high heterogeneity I2 value (I2 = 94.9%) (Supplemental Figure S2). Meta-regression calculation depicted a constant MB2 prevalence over the years (Fig. 6) and omnibus p-value (0.818) excluded age as a source variance of heterogeneity. However, geographic region meta-regression (omnibus p-value of 0.017) reveal it as a possible source of explainable heterogeneity of the selected studies.
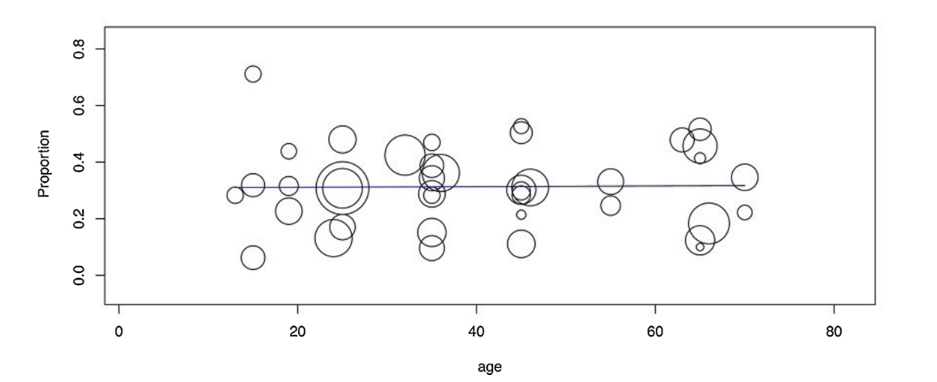
In maxillary second molars, middle age interval value of 8 studies (40 age intervals) from 9 population groups was also calculated to determine MB2 prevalence. A proportion forest plot revealed a MB2 prevalence of 31.3% (27.3%-35.4%) with a high heterogeneity value (I2 = 90.7%) (Fig. 7). Age meta-regression chart depicted a constant MB2 prevalence over the years (Fig. 7) and, similarly to the first molar analysis, meta-regression excluded age (omnibus p-value of 0.923), but revealed region (omnibus p-value of 0.004) as a source of explainable heterogeneity in the included studies.
ordered by age increasing according to different geographic regions; bottom: age meta-regression. (To the proportion forest plots, the yellow and blue rhombus
shapes represent the combined results for each sub-group or overall analysis, respectively. The non-overlapped yellow shapes represent statistically significant
differences among sub-groups. As for the meta-regression, the black line represents the regression line, while each circle represents a study whose diameter is
proportional to its weight in the analysis).
MB2 canal and geographic region
Geographic region meta-analysis on MB2 prevalence in maxillary first and second molars were performed in 22 (41 population groups) (Fig. 8) and 16 (17 population groups) (Fig. 9) studies, respectively. In maxillary first molars, the highest proportion of MB2 canal was observed in Africa (80.9%; 67.7%-93.8%) (4 population groups combined) and the lowest in Oceania (53.1%; 46.6%-59.7%) (1 single population group), with statistical difference among a few regions (p < 0.05). Regarding maxillary second molars, Africa showed also the highest MB2 prevalence (62.4%; 53.5%-71.3%) (2 population groups combined), while the lowest was observed in West Asia (21.6%; 18.4%- 24.8%) (1 single population group), with statistical significant differences between regions (p < 0.05). Geographic region meta-regression analysis of maxillary first (omnibus p-value of 0.078) and second (omnibus p-value of 0.001) molars revealed region as a significant factor for explainable variance in the prevalence of MB2 canal for the second molar.
MB2 canal and voxel size
Image voxel size meta-regression showed an almost constant MB2 prevalence when compared studies using different image voxel sizes for both molars (Supplemental Figure S3). According to the omnibus p-value for the first (p-value of 0.132) and second (p-value of 0.212) molars, the heterogeneity of the studies cannot be explained by the image voxel size.
Discussion
Although several observational studies have been published regarding the anatomy and the incidence of the MB2 canal in maxillary molars, the current study provides two innovative results regarding this topic. First, it pooled together all relevant studies that used similar methodology (CBCT imaging) in order to obtain an evidence-based background of the impact of gender, age or region on this anatomical feature. Another relevant original data was to propose an explanation for the observed differences based on anthropological and forensic researches. In summary, the present findings help to fill the gap identified in the literature regarding the relationship between MB2 and some demographic data which might be valuable on either clinical practice or anthropological perspective.
In the present study, prevalence of MB2 canal in maxillary first molars ranged from 96.7% (Belgium sub-population) (Martins et al., 2018a) to 30.9% (Chinese sub-population) (Jing, Ye, Liu, Zhang, & Ma, 2014), while in second molars, the highest and lowest prevalence were reported in the Brazilian (83.2%) (Reis et al., 2013) and Chinese (13.4%) sub-populations (Jing et al., 2014). Overall, mean prevalence of MB2 was higher in maxillary first molars (69.6%) than in second molars (39.0%), which is in agreement with previous studies (Lee et al., 2011; Martins, Marques, Mata, & Carames, 2017). The heterogeneity noted in the meta-analysis could be likely due to differences in case definitions, biases, or outcome evaluation methods. For that purpose, a two-step heterogeneity assessment was performed. Firstly, JBI Critical Appraisal tool was applied and articles with scores below 50% were excluded, decreasing the risk of bias. Then, demographic factors (age, gender, and geographic region), tooth group, and nominal resolution of the CBCT devices (voxel size) were stratified aiming to accurately assess heterogeneity weight.
In the present review, odds ratio calculation between genders showed significant higher odds for presenting maxillary first molars MB2 in males (1.324) than in females (0.676), with a low heterogeneity value (I2 value: 18.54%). Therefore, the first null hypothesis was rejected.
Differences in the age intervals reported in the studies hampered the analysis and the middle age value of each interval had to be calculated for meta-regression evaluation. Despite middle interval value may not represent the average of the ages in a specific age interval, forest plot and meta-regression analysis confirmed that prevalence of MB2 remained constant over the years (Figs. 6 and 7), while the omnibus p-value (0.818) excluded age as a source of heterogeneity, accepting the second null hypothesis. This result is not in accordance with some studies that reported lower prevalence of MB2 in older patients (Jing et al., 2014; Lee et al., 2011; Wu, Zhang, & Liang, 2017), explaining this finding as a result of dentine deposition over the years. Thomas, Moule, and Bryant (1993)) evaluated the influence of aging on the internal morphology of the mesiobuccal roots of maxillary first molars. According to the authors, all mesiobuccal roots of patients less than 8 years had only a single and large root canal. However, by the age of 10, a two-directional calcification pattern could be noted. Initially in a mesio-distal direction with apposition in the center of the large root canal resulting in the formation of 2 canals (MB1 and MB2), and later in a lingual-towards-buccal direction, narrowing the root canal at the lingual aspect of the root. One limitation of the present review is that only one study reported the use of CBCT technology in children (Albarca et al., 2015), while the lowest average age of the population in the other studies was 22 years (Martins et al., 2018a). Consequently, the anatomy of the mesiobuccal roots of maxillary molars in young patients were not available and this review was unable to detect changes in the anatomy of this root canal system due to aging. Apparently, narrowing or even closure of the MB2 canal system in older patients were not expressed under CBCT analysis.
In this review, different assessments (analysis by tooth group, age, gender or geographic region) were performed to evaluate the prevalence of MB2 based on studies that evaluated the internal anatomy of the mesiobuccal root of maxillary first and second molars using CBCT technology in different populations. Each assessment had its own requirements and pooled studies were not necessarily the same.
Notwithstanding, prevalence of MB2 canal acquired in the different assessments was similar. Overall, MB2 proportions for tooth group, gender, age and geographic region were 69.6%, 69.4%, 66.6% and 69.6% for maxillary first molars, respectively, and 39.0%, 35.3%, 31.3% and 39.0% for maxillary second molars, respectively. The largest deviation of MB2 proportion observed in the analysis of age in maxillary second molars (31.3%) may be partially explained because most of pooled studies (72.5%) were from East Asia, a region associated with a low prevalence of MB2 canal (Jing et al., 2014; Wang, Ci, & Yu, 2017). Additionally, stratification and meta-regression of the demographic factors also demonstrated that tooth group and geographic region presented a significant omnibus p-value, thus apparently interfering in the obtained heterogeneity. Consequently, the third null hypothesis was rejected. Taken together, these findings reinforce the hypothesis that geographic region may influence the prevalence of MB2 canal in maxillary molars.
Despite most of prevalence studies published on the anatomy of the mesiobuccal root of maxillary molars explained the results based on gender or ethnic factors, endodontic literature still lacks from proper explanation of these anatomical differences based on the Forensic (Capitaneanu, Willems, & Thevissen, 2017) and Anthropological (Mizoguchi, 2013; Noss, Scott, Potter, Dahlberg, & Dahlberg, 1983) research findings. In the Forensic sciences, for instance, sex estimation is commonly based on several parameters including dental metric and non-metric measurements (Capitaneanu et al., 2017). Studies in different populations using several methodologies are consensual in demonstrating that linear (Lakhanpal, Gupta, Rao, & Vashisth, 2013; Macaluso, 2011; Noss et al., 1983; Omar, Alhajrasi, Felemban, & Hassan, 2018) and diagonal (Karaman, 2006) dimensions of maxillary molars are larger in males than in females. Additionally, although the degree of sexual dimorphism in humans may vary within populations, differential effects of the X and Y chromosomes on growth (Alvesalo, 2013) have been also used to explain why teeth dimensions of males, in both primary and permanent dentitions, are generally larger than their female counterpart (Alvesalo, 2013; Scott, Potter, Noss, Dahlberg, & Dahlberg, 1983). The Y chromosome promotes tooth crown enamel and dentine grow, while the X chromosome action seems to be restricted to enamel formation (Alvesalo, 2013). Therefore, differential effect of the X and Y chromosomes explains gender dimorphism including the presence of larger molars in males and, possibly, an increasing in the number of root canals.
Differences in the size of maxillary molars can be also found when comparing different geographic regions. The Australian aboriginals typically present the largest sized teeth, followed by the Africans, while Asians and Europeans have teeth with similar sizes (Mizoguchi, 2013). Regarding ethnic traits non-metric parameter, a few differences were also reported, including a higher prevalence of Carabelli cusp in maxillary first molar and 3-rooted configuration of maxillary second molars in Europeans and Africans, when compared to Asian populations (Irish, 2013; Yaacob, Nambiar, & Naidu, 1996). These anatomical variations observed in different geographic regions may be explained based on anthropological studies. Research based on genetics and morphologic data were able to trace genetic ancestry of modern humans in the Africa sub-Saharan region (Hanihara, 2013). From there, the world colonization by the human species may occurred by the northern (the Levant corridor) or southern (the Horn of Africa) routes (Hanihara, 2013). After leaving the Africa, prehistoric human dispersal continued mostly to southeast and northwest directions, including Euroasia and Siberian routes (Hanihara, 2013). This split created three main branches of phenotype evolution (Caucasian, Africans and Asians) and might be the origin of the morphological dissimilarities observed nowadays in different populations. Considering that prehistoric colonization possibly submitted human species to environmental variability and shifting se- lection pressures (variability selection) such as nutrition, weather temperature, genetic aspects (allele B of the ABO blood group) (Mizoguchi, 2013), hormonal activity and postnatal functions mod- ifications (Yaacob et al., 1996), these factors may impact the final phenotypes for each ethnic group, including the morphology of jaws and teeth. Natural selective forces have been also associated with phenotype change. According to some authors, large tooth sizes were maintained as strong natural selection (Africans), while reduction in tooth size occurred in the absence of such pressure, being influenced by the early development of food preparation and pottery use (Euroasians) (Hanihara, 2013).
Based on the aforementioned evolutive evidences and taking into consideration the influence of the external anatomy on the inner morphology of teeth reported in previous studies (Fan, Cheung, Fan, Gutmann, & Bian, 2004; Ordinola-Zapata et al., 2017), it would be expected different proportions of MB2 root canals in maxillary molars depending on the geographic location and gender. For instance, Africans developed larger teeth and are also a geographic region associated with a higher proportion of MB2 canal in maxillary molars (Figs. 8 and9). On the other hand, lower proportions of MB2 canal observed in Asians and Europeans (Figs. 8 and 9) might be correlated with a smaller tooth size when compared to Africans (Irish, 2013). Interestingly, in the present study, Australian region showed a low MB2 proportion (Fig. 8), despite literature reported the largest tooth size in Australian aboriginals (Mizoguchi, 2013). This result can be explained because the single study used in the present review included patients selected from a dental office, which might not represent the original population from Australia (Martins et al., 2018a).
A possible limitation of this systematic review was to restrict the analysis to 3-rooted maxillary first and second molars, despite several root configurations have been previously reported in these groups of teeth (Zhang, Chen, Fan, Fan, & Gutmann, 2014). Nevertheless, it is important to emphasize that the number/configuration of roots has been associated with ethnic background, which may vary from region to region, influencing the internal morphology of teeth (Ghobashy, Nagy, & Bayoumi, 2017; Martins et al., 2018a) with a direct impact on the prevalence of MB2 canal which, ultimately, would be an uncontrolled confounding factor. Besides, other root configurations have been reported in only a small percentage frequency of maxillary first and second molars (Martins, Mata, Marques, & Carames, 2016). Other important aspects regarding the anatomical assessment of the mesiobuccal root canal system may have also influenced the outcome of the studies, including the ability of the observer to identify and classify the anatomy, or even to properly manage the imaging visualization software. This review tried to reduce the influence of these factors by defining a dichotomic outcome (i.e., presence or absence of MB2 canal) including only studies in which this information was clearly stated. However, if data was presented following a classification system, this information was converted in order to calculate the proportion of MB2 independently. For example, Vertucci’s Type I configuration was considered as the absence of MB2, while all the other types indicated its presence. Finally, the reliability of CBCT method used to identify MB2 canal in each study would be also a limiting factor. Thus, a CBCT voxel size equal or lower than 200 μm was established as an inclusion criteria in this study, since a previous research reported a high accuracy (0.88) of CBCT at this voxel size to detect MB2 canal in maxillary molars (Vizzotto et al., 2013). The meta-regression of different voxel sizes used in the studies showed omnibus p-values (0.132 and 0.212) that prevent the possibility to associate the obtained heterogeneity with voxel size (Supplemental Figure S3). Therefore, the fourth null hypothesis was accepted. The present results reinforce the evidence that the limitation of the voxel size to 200 μm was effective in reducing the variability attributed to CBCT method, highlighting the influence of demographic factors. Although smaller voxel sizes would allow a better image quality, it does not seem to be needed for detecting the presence of the MB2 canal, when limited its size up to 200 μm.
Conclusions
Overall, prevalence of MB2 canal in maxillary first and second molars was 69.6% and 39.0%, respectively. Meta-analysis demonstrated not only that males had higher odds of having MB2 canal than females in both maxillary molars, but also significant differences amongst geographic region, while age and voxel size could not be associated to possible sources of heterogeneity.
Authors: Jorge N.R. Martins, Duarte Marques, Emmanuel João, Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani.
References:
- AAE and AAOMR joint position statement (2015). AAE and AAOMR joint position statement: use of cone beam computed tomography in Endodontics 2015 update. Journal of Endodontics, 41, 1393–1396.
- Albarca, J., Gomez, B., Zaror, C., Monardes, H., Bustos, L., & Cantin, M. (2015). Assessment of Mesial Root Morphology and Frequency of MB2 Canals in Maxillary Molars using Cone Beam Computed Tomography. International Journal of Morphology, 33, 1333–1337.
- Alvesalo, L. (2013). The expression of human sex chromossome genes in oral and craniofacial growth. In G. R. Scott, & J. Irish (Eds.). Anthropological perspectives on tooth morphology. Genetics, evolution, variation (pp. 92–107). (1st ed). New York: Cambridge University Press.
- Betancourt, P., Navarro, P., Munoz, G., & Fuentes, R. (2016). Prevalence and location of the secondary mesiobuccal canal in 1,100 maxillary molars using cone beam computed tomography. BMC Medical Imaging, 16, 66.
- Buhrley, L. J., Barrows, M. J., BeGole, E. A., & Wenckus, C. S. (2002). Effect of magnification on locating the MB2 canal in maxillary molars. Journal of Endodontics, 28, 324–327.
- Candeiro, G., Gonçalves, S., Lopes, L., Lima, I., Alencar, P., & Iglecias, E. (2019). Internal configuration of maxillary molars in a subpopulation of Brazil’s Northeast region: a CBCT analysis. Brazilian Oral Research, 33, e082.
- Capitaneanu, C., Willems, G., & Thevissen, P. (2017). A systematic review of odontological sex estimation methods. Journal of Forensic Odontostomatology, 2, 1–19.
- Caputo, B. V. (2014). Estudo da tomografia computadorizada de feixe cônico na avaliação morfológica de raizes e canais dos molares e pré molares da população brasileira (PhD). São Paulo: Universidade de São Paulo.
- Cleghorn, B. M., Christie, W. H., & Dong, C. C. (2006). Root and root canal morphology of the human permanent maxillary first molar: a literature review. Journal of Endodontics, 32, 813–821.
- Donyavi, Z., Shokri, A., Khoshbin, E., Khalili, M., & Faradmal, J. (2019). Assessment of root canal morphology of maxillary and mandibular second molars in the Iranian population using CBCT. Dental and Medical Problems, 46, 45–51.
- Fan, B., Cheung, G. S., Fan, M., Gutmann, J. L., & Bian, Z. (2004). C-shaped canal system in mandibular second molars: Part I–Anatomical features. Journal of Endodontics, 30, 899–903.
- Fernandes, N. A., Herbst, D., Postma, T. C., & Bunn, B. K. (2019). The prevalence of second canals in the mesiobuccal root of maxillary molars: A cone beam computed tomography study. Australian Endodontic Journal, 45, 46–50.
- Ghobashy, A. M., Nagy, M. M., & Bayoumi, A. A. (2017). Evaluation of Root and Canal Morphology of Maxillary Permanent Molars in an Egyptian Population by Cone-beam Computed Tomography. Journal of Endodontics, 43, 1089–1092.
- Gomes Alves, C. R., Martins Marques, M., Stella Moreira, M., Harumi Miyagi de Cara, S. P., Silveira Bueno, C. E., & Lascala, C. A. (2018). Second Mesiobuccal Root Canal of Maxillary First Molars in a Brazilian Population in High-Resolution Cone-Beam Computed Tomography. Iranian Endodontic Journal, 13, 71–77.
- Gorduysus, M. O., Gorduysus, M., & Friedman, S. (2001). Operating microscope improves negotiation of second mesiobuccal canals in maxillary molars. Journal of Endodontics, 27, 683–686.
- Gu, Y., Lee, J. K., Spangberg, L. S., et al. (2011). Minimum-intensity projection for in-depth morphology study of mesiobuccal root. Oral Surgery Oral Medicine Oral Pathology Oral Radiology Endodontics, 112, 671–677.
- Guo, J., Vahidnia, A., Sedghizadeh, P., & Enciso, R. (2014). Evaluation of root and canal morphology of maxillary permanent first molars in a North American population by cone-beam computed tomography. Journal of Endodontics, 40, 635–639.
- Hanihara, T. (2013). Geographic structure of dental variation in the major human populations of the world. In R. Scott, & J. Irish (Eds.). Anthropological perspectives on tooth morphology. Genetics, evolution, variation (pp. 479–509). (1st ed). New York: Cambridge University Press.
- Higgins, J. P. (2011). Cochrane handbook for systematic reviews of interventions. John Wiley & Sons.
- Higgins, J. P., & Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21, 1539–1558.
- Huumonen, S., Kvist, T., Grondahl, K., & Molander, A. (2006). Diagnostic value of computed tomography in re-treatment of root fillings in maxillary molars. International Endodontic Journal, 39, 827–833.
- Irish, J. (2013). Afridonty: the "Sub-Saharan African Dental Complex" revisited. In G. R. Scott, & J. Irish (Eds.). Anthropological perspectives on tooth morphology. Genetics, evolution, variation (pp. 278–295). (1st edn). New York: Cambridge University Press.
- Jing, Y. N., Ye, X., Liu, D. G., Zhang, Z. Y., & Ma, X. C. (2014). [Cone-beam computed tomography was used for study of root and canal morphology of maxillary first and second molars]. Beijing Da Xue Xue Bao, 46, 958–962.
- Karabucak, B., Bunes, A., Chehoud, C., Kohli, M. R., & Setzer, F. (2016). Prevalence of Apical Periodontitis in Endodontically Treated Premolars and Molars with Untreated Canal: A Cone-beam Computed Tomography Study. Journal of Endodontics, 42, 538–541.
- Karaman, F. (2006). Use of Diagonal Teeth Measurements in Predicting Gender in a Turkish Population. Journal of Forensic Sciences, 51, 630–635.
- Kattan, S., Lee, S. M., Kohli, M. R., Setzer, F. C., & Karabucak, B. (2018). Methodological Quality Assessment of Meta-analyses in Endodontics. Journal of Endodontics, 44, 22–31.
- Kewalramani, R., Murthy, C., & Gupta, R. (2019). The second mesiobuccal canal in three-rooted maxillary first molar of Karnataka Indian sub-populations: A cone-beam computed tomography study. Journal of Oral Biology and Craniofacial Research, 9, 347–351.
- Kim, Y., Lee, S. J., & Woo, J. (2012). Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a korean population: variations in the number of roots and canals and the incidence of fusion. Journal of Endodontics, 38, 1063–1068.
- Lakhanpal, M., Gupta, N., Rao, N., & Vashisth, S. (2013). Tooth Dimension Variations as a Gender Determinant in Permanent Maxillary Teeth. JSciMed Dentistry, 1, 1014–1019. Lee, J. H., Kim, K. D., Lee, J. K., et al. (2011). Mesiobuccal root canal anatomy of Korean maxillary first and second molars by cone-beam computed tomography. Oral Surgery
- Oral Medicine Oral Pathololy Oral Radiology Endodontics, 111, 785–791.
- Macaluso, P. J. (2011). Investigation on the utility of permanent maxillary molar cusp areas for sex estimation. Forensic Science Medicine and Pathology, 7, 233–247.
- Martins, J. N., Mata, A., Marques, D., & Carames, J. (2016). Prevalence of Root Fusions and Main Root Canal Merging in Human Upper and Lower Molars: A Cone-beam Computed Tomography In Vivo Study. Journal of Endodontics, 42, 900–908.
- Martins, J. N. R., Alkhawas, M. A. M., Altaki, Z., et al. (2018a). Worldwide Analyses of Maxillary First Molar Second Mesiobuccal Prevalence: A Multicenter Cone-beam Computed Tomographic Study. Journal of Endodontics, 44, 1641–1649.
- Martins, J. N. R., Gu, Y., Marques, D., Francisco, H., & Carames, J. (2018b). Differences on the Root and Root Canal Morphologies between Asian and White Ethnic Groups Analyzed by Cone-beam Computed Tomography. Journal of Endodontics, 44, 1096–1104.
- Martins, J. N. R., Marques, D., Francisco, H., & Carames, J. (2018c). Gender influence on the number of roots and root canal system configuration in human permanent teeth of a Portuguese subpopulation. Quintessence International, 49, 103–111.
- Martins, J. N. R., Marques, D., Mata, A., & Carames, J. (2017). Root and root canal morphology of the permanent dentition in a Caucasian population: a cone-beam computed tomography study. International Endodontic Journal, 50, 1013–1026.
- Martins, J. N. R., Ordinola-Zapata, R., Marques, D., Francisco, H., & Carames, J. (2018d). Differences in root canal system configuration in human permanent teeth within different age groups. International Endodontic Journal, 51, 931–941.
- Mizoguchi, Y. (2013). Significant among-population associations found between dental characters and envirinmental factors. In R. Scott, & J. Irish (Eds.). Anthropological perspectives on tooth morphology. Genetics, evolution, variation (pp. 108–125). (1st ed). New York: Cambridge University Press.
- Munn, Z., Moola, S., Lisy, K., Riitano, D., & Tufanaru, C. (2015). Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. International Journal of Evidence-Based Healthcare, 13, 147–153.
- Naseri, M., Safi, Y., Akbarzadeh Baghban, A., Khayat, A., & Eftekhar, L. (2016). Survey of Anatomy and Root Canal Morphology of Maxillary First Molars Regarding Age and Gender in an Iranian Population Using Cone-Beam Computed Tomography. Iranian Endodontic Journal, 11, 298–303.
- Noss, J. F., Scott, G. R., Potter, R. H., Dahlberg, A. A., & Dahlberg, T. (1983). The influence of crown size dimorphism on sex differences in the Carabelli trait and the canine distal accessory ridge in man. Archives of Oral Biology, 28, 527–530.
- Olczak, K., & Pawlicka, H. (2017). The morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a polish population. BMC Medical Imaging, 17, 68.
- Omar, H., Alhajrasi, M., Felemban, N., & Hassan, A. (2018). Dental arch dimensions, form and tooth size ratio among a Saudi sample. Saudi Medical Journal, 39, 86–91.
- Ordinola-Zapata, R., Martins, J. N. R., Bramante, C. M., Villas-Boas, M. H., Duarte, M. H., & Versiani, M. A. (2017). Morphological evaluation of maxillary second molars with fused roots: a micro-CT study. International Endodontic Journal, 50, 1192–1200.
- Patel, S., Brown, J., Semper, M., Abella, F., & Mannocci, F. (2019). European Society of Endodontology position statement: use of cone beam computed tomography in Endodontics: European Society of Endodontology (ESE) developed by. International Endodontic Journal in-press.
- Pattanshetti, N., Gaidhane, M., & Al Kandari, A. M. (2008). Root and canal morphology of the mesiobuccal and distal roots of permanent first molars in a Kuwait population—A clinical study. International Endodontic Journal, 41, 755–762.
- Perez-Heredia, M., Ferrer-Luque, C. M., Bravo, M., Castelo-Baz, P., Ruiz-Pinon, M., & Baca, P. (2017). Cone-beam Computed Tomographic Study of Root Anatomy and Canal Configuration of Molars in a Spanish Population. Journal of Endodontics, 43, 1511–1516.
- Reis, A. G., Grazziotin-Soares, R., Barletta, F. B., Fontanella, V. R., & Mahl, C. R. (2013). Second canal in mesiobuccal root of maxillary molars is correlated with root third and patient age: a cone-beam computed tomographic study. Journal of Endodontics, 39, 588–592.
- Scott, G. R., Potter, R. H., Noss, J. F., Dahlberg, A. A., & Dahlberg, T. (1983). The dental morphology of Pima Indians. American Journal of Physical Anthropology, 61, 13–31.
- Shea, B. J., Reeves, B. C., Wells, G., et al. (2017). AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. British Medical Journal, 21, 358.
- Silva, E. J., Nejaim, Y., Silva, A. I., Haiter-Neto, F., Zaia, A. A., & Cohenca, N. (2014). Evaluation of root canal configuration of maxillary molars in a Brazilian population using cone-beam computed tomographic imaging: an in vivo study. Journal of Endodontics, 40, 173–176.
- Thomas, R. P., Moule, A. J., & Bryant, R. (1993). Root canal morphology of maxillary permanent first molar teeth at various ages. International Endodontic Journal, 26, 257–267.
- Vertucci, F. J. (1984). Root canal anatomy of the human permanent teeth. Oral Surgery Oral Medicine Oral Pathology, 58, 589–599.
- Vizzotto, M. B., Silveira, P. F., Arus, N. A., Montagner, F., Gomes, B. P., & da Silveira, H. E. (2013). CBCT for the assessment of second mesiobuccal (MB2) canals in maxillary molar teeth: effect of voxel size and presence of root filling. International Endodontic Journal, 46, 870–876.
- Wang, H., Ci, B., Yu, H., et al. (2017). Evaluation of root and canal morphology of maxillary molars in a Southern Chinese subpopulation: a cone-beam computed tomographic study. International Journal of Clinical and Experimental Medicine, 10, 7030–7039.
