Middle Mesial Canal Preparation Enhances the Risk of Fracture in Mesial Root of Mandibular Molars
Abstract
Introduction: The aim of this investigation was to evaluate the effect of the presence and preparation of middle mesial (MM) canals on the fracture resistance of the mesial root of mandibular molars. Methods: Forty intact mesial roots of mandibular first molars having 2 (n = 20) or 3 (n = 20) independent canals from the furcation level for up to at least 5 mm apically were selected based on preoperative micro–computed tomographic scanning. The selected roots were then distributed into 2 experimental (n = 10) and 2 control groups (n = 10) according to the root length, canal configuration (2 or 3 independent canals), and root thickness at the furcation level. In the experimental groups 1 (2 independent canals) and 3 (3 independent canals), root canals were enlarged up to the ProTaper Next X3 rotary instrument (Dentsply Sirona, Ballaigues, Switzerland), whereas in groups 2 (2 independent canals) and 4 (3 independent canals) root canals were not prepared. The specimens were embedded in acrylic resin after their surfaces were coated with a thin layer of silicone and subjected to a fracture strength using a universal testing machine. The types of fracture extension and course were recorded and statistically compared with the chi-square test, whereas fracture strength was analyzed using 1-way analysis of variance and post hoc Tukey tests (α = 5%).
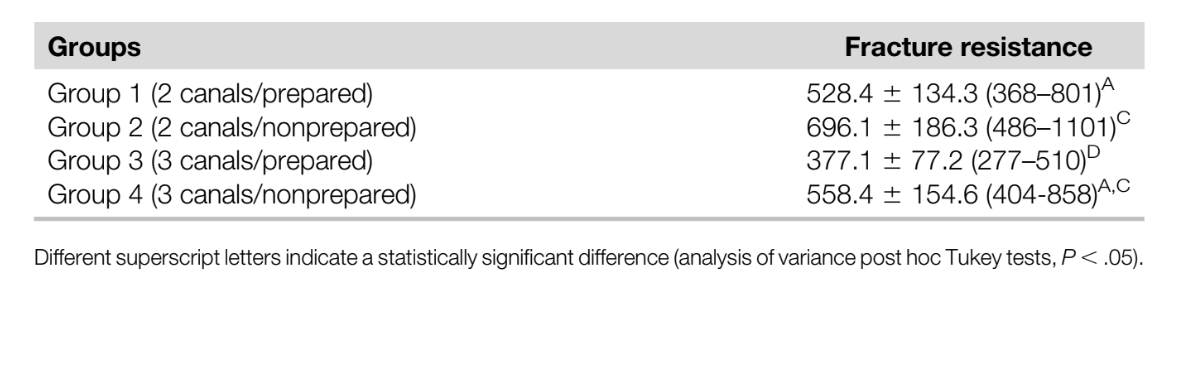
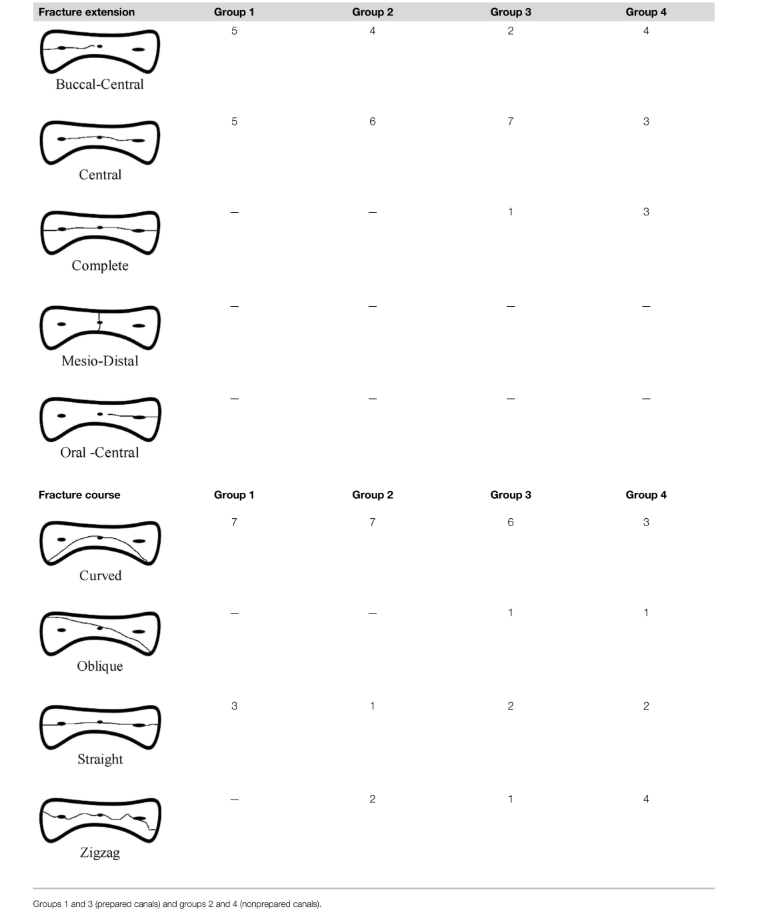
Results: No statistical difference in fracture strength was observed between nonprepared roots with 2 (group 2, 696.1 ± 186.3 N) or 3 (group 4, 558.4 ± 154.6 N) independent canals (P ˃ .05), whereas the lowest values were obtained in the prepared roots with an MM canal (groups 3, 377.1 ± 77.2 N) (P ˂ .05). The mean fracture strength observed in the prepared roots with 2 canals (group 1, 528.4 ± 134.3 N) showed no statistically significant difference compared with nonprepared roots with 3 canals (group 4, 558.4 ± 154.6 N) (P ˃ .05). The chi-square test revealed no significant differences in fracture extent, types, and courses among groups (P ˃ .05). Fracture extensions in all groups were mostly central and buccal-central types, whereas the highest frequency of fracture course was the curved and zigzag types.
Conclusions: The fracture resistance of the mesial roots of the mandibular molars decreased after the preparation of mesial canals with large-tapered instruments. Preparation of the MM canal further diminished the fracture resistance of the mesial roots. The resultant fracture displayed a distinct pattern in the buccolingual plane. (J Endod 2020;46:1323–1329.)
Vertical root fracture (VRF) has been described as a longitudinal fracture confined within the root structure. It is generally oriented in the buccal-lingual direction while extending vertically along the root. It occurs most often in teeth that have previously received endodontic treatment. The risk factors that increase the predilection of VRF in a tooth can be broadly categorized as anatomic (noniatrogenic) and iatrogenic factors. The iatrogenic factors include the degree of root canal enlargement, the prepared canal shape, and post space preparation/placement, whereas anatomic (noniatrogenic) factors include the canal number, the remaining dentinal thickness, the presence of isthmus, and root dimensions. It was also reported that most of the VRF cases were related to teeth with roots presenting a cross-sectional mesiodistal dimension narrower than their buccolingual dimension, indicating that this specific anatomy may be a significant risk factor that predisposes such teeth to VRF. For the same reason, VRF is among the primary causes of loss of endodontically treated mandibular molars with extraction rates ranging from 51.8% to 67%.
The mesial root of mandibular molars usually presents 2 main canals (mesiobuccal [MB] and mesiolingual [ML]); however, an additional canal that is located within the developmental groove between the 2 main canals named the middle mesial (MM) canal has been reported. The MM canal might exist with its own orifice or branch from the MB or ML canals and terminate independently or join 1 of these main canals. Earlier studies using conventional analytical tools have reported that the frequency of the MM canal varies from 0.26%–6%. However, recent investigations based on in vivo high-magnification–based analysis and nondestructive micro–computed tomographic (micro-CT) technology have demonstrated that its incidence may be as high as 46.1%. A previous study showed that mesial roots of mandibular molars with 2 main canals are more susceptible to VRF than the distal root with a single canal; yet, the current endodontic literature lacks studies examining the influence of root canal preparation on the resistance to fracture for roots presenting with extra canals and susceptible morphology.
Therefore, the purpose of this study was to evaluate the effect of MM canal preparation on the fracture resistance of mesial roots of mandibular molars. The null hypothesis tested was that neither the presence nor the preparation of the MM canal significantly affected the fracture resistance of mesial roots of mandibular first molars.
Materials and methods
Sample Size Calculation
Sample size was calculated using the effect size (2.03) of a previous study on root fracture. This value was input into a priori analysis of variance (ANOVA) selected from the F test family (fixed effects, omnibus, 1 way) using an alpha-type error of 0.05 and a beta power of 0.90 (G*Power 3.1 for Macintosh; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany). The software indicated a number of 10 specimens per group as a minimum ideal size required to observe a significant effect.
Sample Selection and Groups
This study protocol was approved by the local university ethics committee (KAEK/67). Two hundred sixty-nine mandibular first molar teeth were collected from a Turkish subpopulation and stored at 37◦C with 100% humidity during all of the experimental procedures. To prevent the introduction of confounding variables, the coronal portions and distal roots of all teeth were removed by using a low-speed saw with water cooling (Isomet; Buehler Ltd, Lake Bluff, IL). Then, the mesial roots were scanned on a micro-CT system (SkyScan 1172; Bruker- microCT, Kontich, Belgium) at 10 mm (pixel size), 100 kV, 100 mA, 180◦ rotation around the vertical axis, a rotation step of 0.4◦, camera exposure time of 1400 milliseconds, and a frame average of 3. X-rays were filtered with 500-mm-thick aluminum and 38-mm-thick copper filters. Data were reconstructed using NRecon v.1.7.4.2 software (Bruker-microCT) with a beam hardening correction of 45% and an attenuation coefficient ranging from 0.0–0.06. Data Viewer v.1.5.6 software (Bruker-microCT) was used to evaluate the root canal configuration of each specimen and exclude specimens showing defects, craze lines, cracks, caries, resorption, fractures, or incomplete root formation.
From the scanned specimens, 20 mesial roots showing 2 independent canals (MB and ML) and 20 roots showing 3 independent canals (MB, MM, and ML) from the furcation level up to at least 5 mm toward the apical direction were selected. The selected roots (N = 40) were then distributed into 2 experimental (n = 20) and 2 control (n = 20) groups according to the root length (10.0 ± 1.0 mm), the number of root canal orifices at the coronal third (2 or 3 independent canals), and the root thickness at the furcation level (in both the buccolingual and mesiodistal directions), aiming to create well-balanced and anatomically based experimental groups (Table 1). Dentin thickness was calculated according to a previous study.

Sample Preparation
In the experimental groups 1 (n = 10, 2 independent canals) and 3 (n = 10, 3 independent canals), root canals were initially negotiated with a size 06 K-file (Dentsply Sirona, Ballaigues, Switzerland), and patency was established up to a size 10 K-file (Dentsply Sirona). The working length was determined 1 mm short of the apical foramen. The root canals were sequentially enlarged with ProTaper Next X1 (size 17, .04 taper), X2 (size 25, .06 taper), and X3 (size 30, .07 taper) instruments (Dentsply Sirona) according to the manufacturer’s directions. A total of 15 mL 5.25% sodium hypochlorite delivered through a 31-G needle (NaviTip; Ultradent Products, Inc, South Jordan, UT) placed up to 2 mm short of the working length was used as irrigant in each root. The final irrigation was performed with 5 mL 17% EDTA for 1 minute followed by 5 mL distilled water. A single experienced endodontist performed all preparation procedures. Root canals in groups 2 (n = 10, 2 independent canals) and 4 (n = 10, 3 independent canals) received no treatment and served as controls.
Fracture Resistance Test
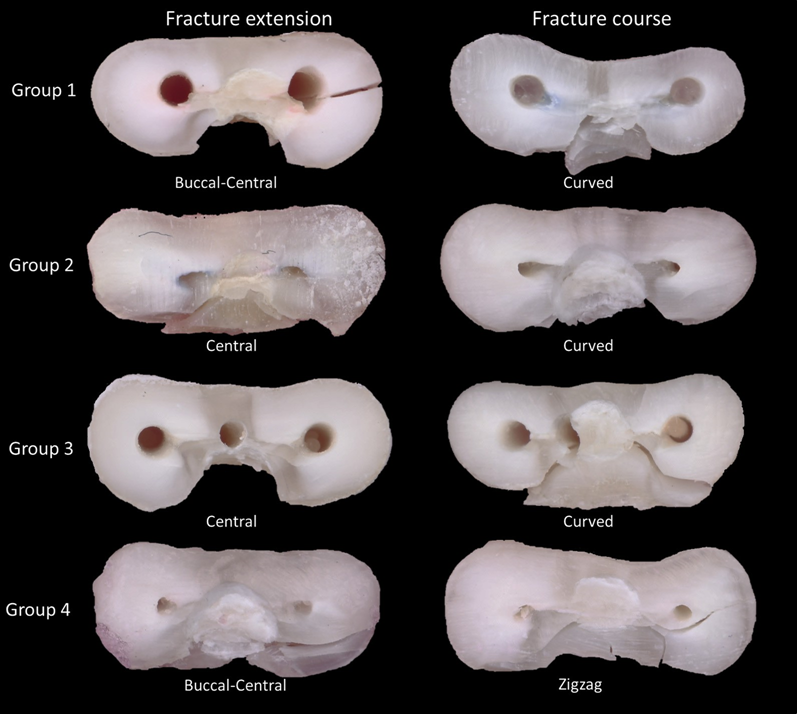
The roots were covered with 0.2-mm-thick aluminum foil and embedded into acrylic resin (Meliodent; Bayer Dental, Leverkusen, Germany) using cylindrical plastic molds (20 X 20 mm) by aligning their vertical axis with a protractor and exposing 2 mm of their coronal portions. After complete resin polymerization, roots were removed from the acrylic mold and the aluminum foils replaced with a thin layer of silicone (Oranwash L plus Indurent Gel; Zhermack, Badia Polestine, Italy) to simulate the periodontal ligament. Each acrylic block was positioned and stabilized on the lower plate of a universal testing machine (AGS-X; Shimadzu Corporation, Tokyo, Japan) to allow the tip of a stainless steel spherical tip (1 mm in diameter) to be positioned at the center of the coronal surface of the root on the sound dentin, avoiding the root canal orifice. The load was applied at a crosshead speed of 1 mm/min until fracture occurred, which was represented by a sharp drop in the force detected by dedicated software (Trapezium X, Shimadzu Corporation). The force required to fracture was recorded in newtons. All roots were kept in an environment of 100% humidity throughout the fracture test. After the experimental procedure, 2 previously calibrated evaluators examined the roots under X10 magnification (Stemi 2000; Carl Zeiss, Göttingen, Germany) together and classified the horizontal extent (complete, buccal-central, oral-central, central, or mesiodistal) and course (straight, oblique, curved, or zigzag) of the fractures according to the classification proposed by von Arx and Bosshardt. If the evaluators failed to reach a consensus, a third examiner was consulted.
Statistical Analysis
Preoperative anatomic parameters (Table 1) and fracture resistance data revealed normal distribution (Shapiro-Wilk test, P ˃ .05), and the results were statistically compared among groups using 1-way analysis of variance and post hoc Tukey tests. The distribution, extent, types, and courses of the fracture were compared with the chi-square test. Statistical analyses were performed with SPSS v.21 (IBM Corp, Armonk, NY) with a significant threshold set at 5%.
Results
Table 2 presents the descriptive statistics for the fracture resistance values, whereas Table 3 reveals the fracture extension types and courses observed in all specimens. The mean fracture resistance values measured in the nonprepared mesial roots with 2 (group 2, 696.1 ± 186.3 N) or 3 (group 4, 558.4 ± 154.6 N) independent canals showed no significant difference (P ˃ .05), whereas the lowest values were observed in the prepared roots with an MM canal (groups 3, 377.1 ± 77.2 N) (P ˂ .05). Fracture resistance in group 1 (prepared roots with 2 canals, 528.4 ± 134.3 N) also showed no statistically significant difference compared with nonprepared roots with 3 canals (group 4, 558.4 ± 154.6 N) (P ˃ .05) (Table 2). Stereomicroscopic examination of the fractured specimens (Fig. 1) revealed that fracture extensions in all groups were mostly in the central (n = 16) and buccal-central (n = 21) types, whereas the highest frequencies of fracture course were curved (n = 23) and oblique (n = 8) (Table 3). The chi-square test revealed no significant difference in the types of fracture among the different groups (P ˃ .05).
Discussion
Currently, considerable attention has been given to the minimally invasive therapeutics in dentistry. This approach aimed to preserve healthy dental hard tissue in order to avoid structural failures. In endodontics, the preservation of the pericervical dentin, extending approximately 4 mm coronal and 4 mm apical to the alveolar crestal bone, has been considered crucial once this structure is responsible to transfer the functional load to the surrounding alveolar bone. Therefore, the resistance to fracture has been related to the amount of residual root structure at this level. The present study evaluated the fracture resistance of mesial roots containing 2 or 3 independent canals at the pericervical aspect of the root. As in all experimental laboratory tests, the standardization of teeth is always a challenging task because of possible variations in dentin mechanical properties, storage time, and storage medium after extraction, and this is 1 of the limitations of the present study. Notwithstanding, strict sample selection and homogenous distribution based on morphometric data of root and root canals obtained by micro-CT analysis aimed to increase the internal validity of the method and, consequently, the reliability of the results.
Overall, the results from this investigation showed that although the preparation of MM canals significantly reduced the fracture resistance of the mesial root, its presence was not found as a predisposing factor, and the null hypothesis was partially rejected.
A recent study demonstrated that the enlargement of the MM canal with the ProTaper Next X2 or X3 instrument resulted in a significantly thinner root dentin compared with the MB and ML canals with almost 26% of the analyzed cross sections showing less than 0.5-mm dentin thickness, which may partially explain the observed results in the present study. It was also revealed that the mesial roots with MM canals displayed an asymmetric root shape in its cross section with a deep developmental distal root groove that commonly results in a dentin thickness of 0.5– 1 mm. Therefore, the increased susceptibility to fracture of the selected specimens would be attributed to the combined effect of the reduced dentin thickness, the irregular canal shape, and the asymmetric cross section of the mesial root. Additionally, it is important to note that the root depression in the interproximal aspect can predispose the mesial root of the mandibular molar not only to fracture but also to root perforation when the canals are prepared with large-tapered instruments. These iatrogenic factors may compromise the long-term outcome of the endodontic treatment.
The primary objective of this in vitro fracture resistance experiment was to compare the relative variation in the fracture strength values between the different experimental groups. The findings from this investigation displayed the highest fracture resistance values in the nonprepared roots with 2 independent canals (group 2) (Table 2). This may be because of the thicker (more than 1 mm) coronal dentin in the distal/mesial directions. Interestingly, the fracture resistance in the nonprepared roots with MM canals (group 4) was similar to the prepared mesial roots with 2 independent canals (group 1) (Table 2). According to a previous study, the percentage of mesial root cross sections with a dentin thickness ,1 mm after preparation of the MB and ML canals with the ProTaper Next X3 instrument was similar to that observed in the nonprepared roots with MM canals.
Based on these findings, if an additional apical enlargement of a mesial root with an MM canal is required to improve disinfection, it may be recommended to use a less-tapered final instrument with a larger tip. This would aid in mitigating the risk of perforation and root fracture. The influence of root canal enlargement with instruments having different designs in variable root cross-sectional shapes remains to be determined by further studies.
Most of the fractures observed herein occurred in the middle location of the root with a curved course passing through the concavity created by the presence of the developmental distal groove, irrespective of the experimental group (Table 3). All of the fractures occurred in the buccolingual direction in accordance to the previous reports. This direction has been associated with a decreased thickness of the proximal dentin in the mesial root. In biomechanics, it is known that tensile stress in the circumferential direction causes a different amount of expansions dependent on the thickness of the walls when stress is applied in a radial direction perpendicular to the long axis of a cylinder. Therefore, thin parts of an asymmetric walled vessel would expand more readily than thicker parts, and this rapid expansion results in bending outward, which also creates additional tensile stress that might lead to cracks or fractures in the inner surface of the thick-walled parts. Therefore, the thinner dentin thickness usually related to the distal aspect of the mesial roots of mandibular molars might influence the stress distribution on root canal walls leading to accumulation in the buccolingual direction by the outward bending of the thinner dentin walls around the root canals. Besides, despite mechanical experiments showing that functional stresses are predominantly distributed at the cervical dentin, the root dentin removal shifts the stress patterns more apically and along the buccolingual plane, contributing to the propagation of fracture in the buccolingual direction, as observed in the present study. Finally, considering that the role of instrumentation size in VRF is still not clear, future studies should be designed to evaluate the influence of canal preparation with different sizes in the fracture resistance of roots with variable cross-sectional shapes either using extracted pair-matched contralateral teeth obtained from patients with a known age or the finite element analysis method with 3-dimensional models of real roots and alveolar bone acquired by micro-CT technology.
Conclusion
The current study highlighted the influence of anatomic features of the mesial root of mandibular molars on canal instrumentation and subsequent fracture predilection. It was concluded that the fracture resistance of mesial roots decreased significantly after the preparation of mesial canals with large-tapered instruments. Also, although the presence of MM canals was not found to be a predisposing factor, their preparation reduced the fracture resistance of the mesial root of mandibular molars.
Authors: Ali Keleş, Cangül Keskin, Emrah Karataşlioğlu, Anil Kishen, Marco Aurélio Versiani
References:
- American Association of Endodontists. Glossary of Endodontics Terms. 9th ed. Chicago: American Association of Endodontists; 2016.
- Munari LS, Bowles WR, Fok ASL. Relationship between canal enlargement and fracture load of root dentin sections. Dent Mater 2019;35:818–24.
- Chai H, Tamse A. The effect of isthmus on vertical root fracture in endodontically treated teeth. J Endod 2015;41:1515–9.
- Kishen A. Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endod Topics 2006;13:57–83.
- Kishen A. Biomechanics of fractures in endodontically treated teeth. Endod Topics 2015;33:3– 13.
- Lertchirakarn V, Palamara JE, Messer HH. Patterns of vertical root fracture: factors affecting stress distribution in the root canal. J Endod 2003;29:523–8.
- Meister F Jr, Lommel TJ, Gerstein H. Diagnosis and possible causes of vertical root fractures. Oral Surg Oral Med Oral Pathol 1980;49:243–53.
- Sathorn C, Palamara JE, Messer HH. A comparison of the effects of two canal preparation techniques on root fracture susceptibility and fracture pattern. J Endod 2005;31:283–7.
- Von Arx T, Bosshardt D. Vertical root fractures of endodontically treated posterior teeth. Swiss Dent J 2017;127:14–23.
- Wilcox LR, Roskelley C, Sutton T. The relationship of root canal enlargement to finger-spreader induced vertical root fracture. J Endod 1997;23:533–4.
- Rundquist BD, Versluis A. How does canal taper affect root stresses? Int Endod J 2006;39:226–37.
- Tamse A, Fuss Z, Lustig J, Kaplavi J. An evaluation of endodontically treated vertically fractured teeth. J Endod 1999;25:506–8.
- Yoshino K, Ito K, Kuroda M, Sugihara N. Prevalence of vertical root fracture as the reason for tooth extraction in dental clinics. Clin Oral Investig 2015;19:1405–9.
- Gher ME Jr, Dunlap RM, Anderson MH, Kuhl LV. Clinical survey of fractured teeth. J Am Dent Assoc 1987;114:174–7.
- Azim AA, Deutsch AS, Solomon CS. Prevalence of middle mesial canals in mandibular molars after guided troughing under high magnification: an in vivo investigation. J Endod 2015;41:164– 8.
- Keleş A, Keskin C, Alqawasmi R, Versiani MA. Evaluation of dentine thickness of middle mesial canals of mandibular molars prepared with rotary instruments: a micro-CT study. Int Endod J 2020;53:519–28.
- Kim SY, Kim BS, Woo J, Kim Y. Morphology of mandibular first molars analyzed by cone-beam computed tomography in a Korean population: variations in the number of roots and canals. J Endod 2013;39:1516–21.
- Versiani MA, Ordinola-Zapata R, Keleş A, et al. Middle mesial canals in mandibular first molars: a micro-CT study in different populations. Arch Oral Biol 2016;61:130–7.
- Hammad M, Qualtrough A, Silikas N. Effect of new obturating materials on vertical root fracture resistance of endodontically treated teeth. J Endod 2007;33:732–6.
- Liu R, Kaiwar A, Shemesh H, et al. Incidence of apical root cracks and apical dentinal detachments after canal preparation with hand and rotary files at different instrumentation lengths. J Endod 2013;39:129–32.
- Mireku AS, Romberg E, Fouad AF, Arola D. Vertical fracture of root filled teeth restored with posts: the effects of patient age and dentine thickness. Int Endod J 2010;43:218–25.
- Turk T, Kaval ME, Sarikanat M, et al. Effect of final irrigation procedures on fracture resistance of root filled teeth: an ex vivo study. Int Endod J 2017;50:799–804.
- Gluskin AH, Peters CI, Peters OA. Minimally invasive endodontics: challenging prevailing paradigms. Br Dent J 2014;216:347–53.
- Asundi A, Kishen A. A strain gauge and photoelastic analysis of in vivo strain and in vitro stress distribution in human dental supporting structures. Arch Oral Biol 2000;45:543–50.
- Huynh N, Li FC, Friedman S, Kishen A. Biomechanical effects of bonding pericervical dentin in maxillary premolars. J Endod 2018;44:659–64.
- Jiang Q, Huang Y, Tu X, et al. Biomechanical properties of first maxillary molars with different endodontic cavities: a finite element analysis. J Endod 2018;44:1283–8.
- Cohen S, Berman LH, Blanco L, et al. A demographic analysis of vertical root fractures. J Endod 2006;32:1160–3.
- De-Deus G, Rodrigues EA, Belladonna FG, et al. Anatomical danger zone reconsidered: a micro- CT study on dentine thickness in mandibular molars. Int Endod J 2019;52:1501–7.
- Lim SS, Stock CJ. The risk of perforation in the curved canal: anticurvature filing compared with the stepback technique. Int Endod J 1987;20:33–9.
- Kim SY, Kim SH, Cho SB, et al. Different treatment protocols for different pulpal and periapical diagnoses of 72 cracked teeth. J Endod 2013;39:449–52.
- Selden HS. Repair of incomplete vertical root fractures in endodontically treated teeth—in vivo trials. J Endod 1996;22:426–9.
- Beer F, DeWolf J, Johnston ER Jr, Mazurek D. Mechanics of Materials. 7th ed. New York: McGraw-Hill Education; 2014.
- Ossareh A, Rosentritt M, Kishen A. Biomechanical studies on the effect of iatrogenic dentin removal on vertical root fractures. J Conserv Dent 2018;21:290–6.
