Evaluation of dentine thickness of middle mesial canals of mandibular molars prepared with rotary instruments: a micro-CT study
Abstract
Aim: To evaluate, using micro-CT, the remaining dentine thickness after preparation of the mesiobuccal (MB), mesiolingual (ML) and middle mesial (MM) canals of mandibular first molars with the ProTaper Next rotary system.
Methodology: Eleven mesial roots of mandibular first molars having three independent canals from the furcation level up to at least 5 mm towards the apical direction were selected. Preparation of MM canals was performed in two steps using ProTaper Next X2 (step 1) and X3 (step 2) instruments, whilst MB and ML canals were prepared in a single step up to X3 instruments. The roots were scanned (pixel size of 10 µm) before and after each step, and the dentine volume was calculated. Postoperative models of the roots were coregistered with their preoperative dataset and colour-coded cross-sections of the roots were used to measure the smallest dentine thickness of each canal at 1.0-mm intervals from the furcation level up to 5 mm in the apical direction, in both mesial and distal aspects of the roots. Changes in the remaining wall thickness between mesial canals were analysed with repeated-measures ANOVA and post hoc Tukey test. Significance level was set at 5%.
Results: Mean percentage reduction of dentine volume after steps 1 and 2 was 4.66% and 5.16%, respectively. Overall, pre- and postoperative dentine thickness of the MM canal walls, in both mesial and distal aspects of the root, were significantly thinner than those of MB and ML canals (P < 0.05). No significant difference was observed when comparing dentine thickness in the mesial and distal directions of MM canal after preparation step 1 (0.88 0.18 mm and 0.73 0.26 mm, respectively) or 2 (0.83 0.17 mm and 0.67 0.26 mm, respectively) (P> 0.05). Dentine thickness values less than 0.5 mm were observed mostly towards the distal aspect of the MM canal. Mesial roots were not associated with strip perforations after canal preparation procedures.
Conclusions: A significant decrease in the thickness of canal walls at all levels evaluated in the mesial roots of mandibular molars suggests that files with smaller taper should be used in preference to instruments with large taper to prepare mesial canal in mandibular molars.
Introduction
Disinfection of the root canal system is one of the main objectives of the root canal treatment (Siqueira 2001). However, if infected canals are missed, remaining bacteria may maintain or cause disease, compromising the prognosis of the treatment. Indeed, it has been reported that root filled teeth with missed canals are 4.38 (Karabucak et al. 2016) to 6.25 (Costa et al. 2019) times more likely to be associated with apical periodontitis. Therefore, considering that complex morphologies, such as a single root with multiple canal systems, are challenging to debride effectively, knowledge of the prevalence of additional canals in a tooth group should helps clinicians to anticipate their presence in clinical practice (Martins et al. 2019).
The mesial roots of mandibular molars commonly have two main root canals [mesiobuccal (MB) and mesiolingual (ML)], but the presence of an extra canal in this root, the so-called middle mesial (MM) canal, has been also reported in 0.26% (Kim et al. 2013) to 46.15% (Azim et al. 2015) of cases. Considering that the MM canal lies within a thin developmental groove between the orifices of the MB and ML canals, troughing this groove under high magnification has been suggested in order to identify its presence (Azim et al. 2015). However, in a detailed morphological description of the mesial root of mandibular molars with MM canal, it has been reported that the presence of a thin root canal wall towards the furcation side of the MM canal at the orifice level (0.80–2.20 mm) would increase the risk of root perforation after preparation with instruments with large tapers (Versiani et al. 2016). Therefore, the use of low-tapered or decreasing percentage tapered instrument designs have been recommended to avoid the weakening of the root structure during shaping procedures (Gluskin et al. 2014).
The purpose of the present study was to evaluate the remaining dentine thickness at the coronal third of the mesial root of mandibular first molars after preparation of the MB, ML and MM canals using ProTaper Next rotary instruments (Dentsply Sirona, Ballaigues, Switzerland) by means of nondestructive micro-CT technology. The null hypothesis tested was that there was no difference in the remaining dentine thickness after preparation of the mesial canals of mandibular molars using instruments with large tapers.
Materials and methods
Specimen selection and imaging
This ex vivo study was approved by the local Ethical Research Committee (No.KAEK/67). Two hundred and sixty-nine two-rooted mandibular first molar teeth, extracted for reasons not related to this study, were collected from a Turkish subpopulation and scanned on a micro-CT system (SkyScan 1172, Bruker-microCT, Kontich, Belgium) at 10 µm (pixel size), 100 kV, 100 µA, 180° rotation around the vertical axis, rotation step of 0.4°, camera exposure time of 1400 ms and frame average of 3. X-rays were filtered with a 500-mm-thick aluminium and a 38-mm-thick copper filters. Ages of the patients were unknown. NRecon v. 1.7.4.2 software (Bruker-microCT) was used to reconstruct the data with a beam-hardening correction of 45%, smoothing of 2, ring artefact correction of 5, and an attenuation coefficient range of 0–0.06. DataViewer v.1.5.6 software (Bruker-microCT) was used to evaluate the root canal configuration of each specimen. Then, 11 moderately curved mesial roots (10-20°) with 3 independent canals (MB, ML and MM) from the furcation level up to at least 5 mm towards the apical direction were selected. None of the specimens had root fillings, caries, cracks, fractures, and internal or external resorption.
Root canal preparation
Mesial canals were accessed and apical patency was confirmed with a size 10 K-file (Dentsply Sirona, Ballaigues, Switzerland). When the tip of the instrument was visible through the main foramen, 1.0 mm was subtracted to determine the working length (WL). No coronal flaring was performed and a glide path was achieved to the WL with a size 15 K-file (Dentsply Sirona). Then, canal preparation was performed in 2 steps. In step 1, MB and ML canals were prepared with ProTaper Next X1 (size 17, .04 taper), X2 (size 25, .06 taper) and X3 (size 30, .07 taper) instruments (Dentsply Sirona), whilst MM canals were enlarged using ProTaper Next X1 (size 17, .04 taper) and X2 (size 25, .06 taper). Instruments were used sequentially in a continuous clockwise rotation (300 rpm and 3 N.cm) up to the WL (VDW Silver Motor, VDW GmbH, Munich, Germany). After three gentle in-and-out motion strokes in an apical direction, the instrument was removed from the canal and cleaned. Irrigation was performed throughout the preparation procedures with a total of 10 mL of 5.25% sodium delivered by using a 31-gauge NaviTip needle (Ultradent Products Inc., South Jordan, UT, USA) adapted to a disposable plastic syringe placed up to 2 mm short of the WL, with a gentle in-and-out movement. A final rinse with 5 mL of 17% EDTA was followed by a 5-mL rinse with distilled water. An experienced operator performed all canal preparation procedures.
Image analysis
After preparation step 1, the canals were dried with paper points (Dentsply Sirona) and the specimens submitted to a postoperative scan and reconstruction applying the aforementioned parameter settings. Then, after the additional enlargement of the MM canal (preparation step 2), the specimens were subjected to final micro-CT scanning. Postoperative models of the roots were rendered with CTAn v.1.18.8 software (Bruker-microCT) and coregistered with their respective preoperative dataset using the rigid registration module of the DataViewer v.1.5.6 software (Bruker-microCT). The volume of interest (VOI) was selected extending from the furcation level up to 5 mm in the apical direction of the mesial roots, corresponding to approximately 500 slices per root.
The percentage volume decrease of the dentine within the VOI was calculated as follows: (DVB — DVA)/DVB 9 100, where DVB is the total dentine volume (in mm3) before preparation and DVA is the total dentine volume (in mm3) after preparation. An image analysis routine was developed to measure the minimal dentine thickness from both distal and mesial aspects of the MB, ML and MM canals. Using CTAn v.1.18.8 software (Bruker-microCT), a 3D mapping of the dentine thickness was created and saved for structure thickness. Then, colour-coded cross-sections of the roots were used to identify and measure the smallest dentine thickness of each canal at 1.0-mm interval from the furcation level (level 0) up to 5 mm (levels 1–5) in the apical direction, in both mesial and distal aspects of the root. Qualitative comparisons of the root thickness before and after preparation procedures were also performed using 3D colour-coded models of the matched roots with CTVox v.3.3.0 software (Bruker-microCT).
Statistical analysis
Data were normally (Shapiro–Wilk test) and homoscedastically (Levene test) distributed. Repeated-measures ANOVA and post hoc Tukey test were used to compare the changes in the remaining wall thickness between mesial canals after preparation procedures, in both mesial and distal directions. Significance level was set at 5% (SPSS v.21.0 software, SPSS Inc., Chicago, IL, USA).
Results
Tables 1 and 2 display the descriptive statistics (mean, standard deviation and range values) of den- tine thickness, expressed in millimetres, before and after preparation of mesial canals of mandibular first molars, at 1.0-mm interval from the furcation level (level 0) up to 5 mm (levels 1–5) in the apical direction, in both mesial and distal aspects of the root. Table 3 shows the number of cross-sections evaluated for each canal preparation step according to the thickness of the dentine, before and after preparation, in both mesial and distal directions. Figure 1 shows distribution plots of dentine thickness values measured in both directions of each root canal at all levels, and Fig. 2 depicts colour-coded 3D models of representative mesial roots of mandibular molars, before and after preparation, and Fig. 3 displays superimposed cross-sections in which the thinnest area of dentine was not affected by the canal enlargement.
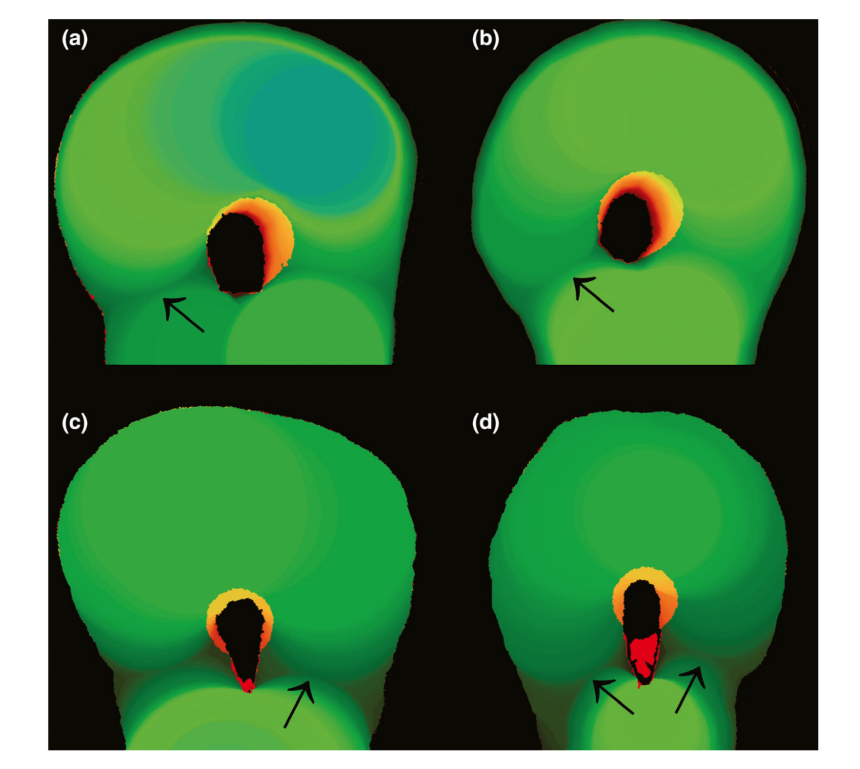
Before preparation, mean dentine thickness of the MM canal in either mesial (1.11 ± 0.22 mm) or distal (0.99 ± 0.25 mm) directions was significantly thinner than that of the MB (1.25 ± 0.16 mm and 1.16 ± 0.20 mm, respectively) and ML (1.22 ± 0.14 mm and 1.19 ± 0.18 mm, respectively) canals (P < 0.05; Tables 1 and 2; Fig. 1). In the mesial direction, dentine thickness of MM canal was similar to MB and ML canals at levels 0, 1 and 5 (P> 0.05) (Table 1; Fig. 1a,b and f) whilst, in the distal direction, statistical similarity was observed only at the furcation level (level 0) (P> 0.05; Table 2; Fig. 1a). Dentine thickness less than 0.5 mm was not observed at any level before preparation, but whilst more than 77% of the measurements related to the MB and ML canals had thicknesses greater than 1.0 mm in both directions, 66.7% of the MM canal cross-sections had dentine thickness between 0.5 and 1.0 mm in the distal direction (Table 3).
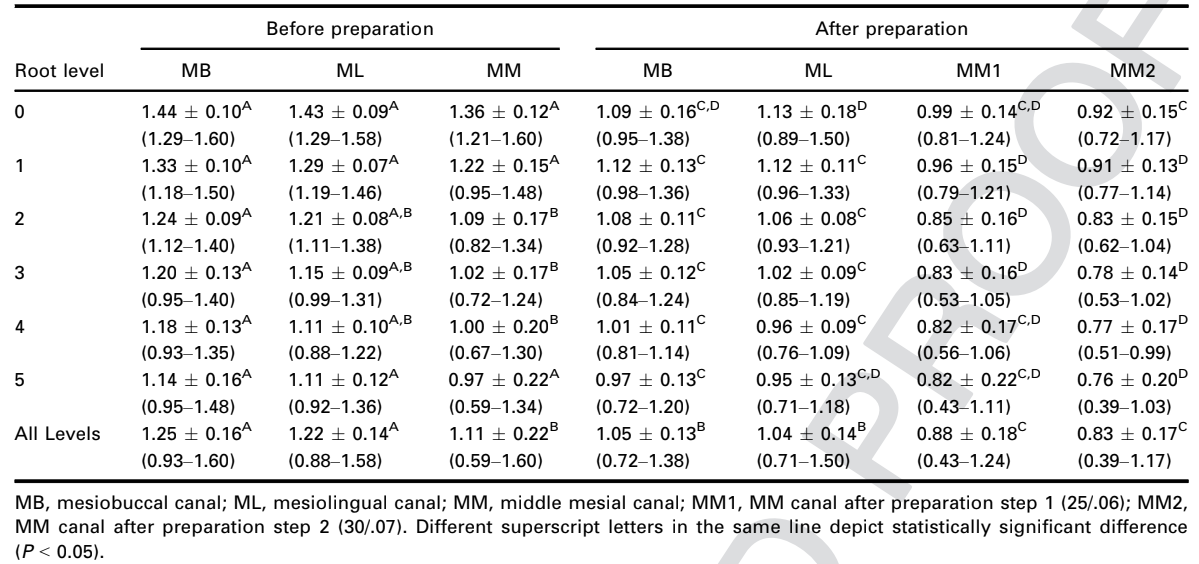
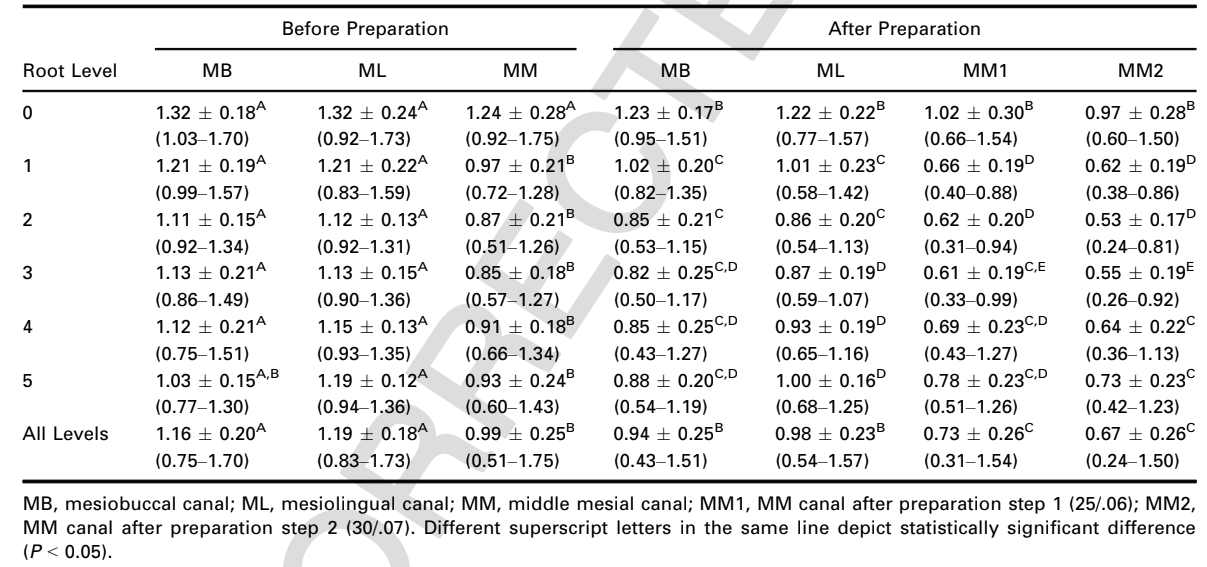
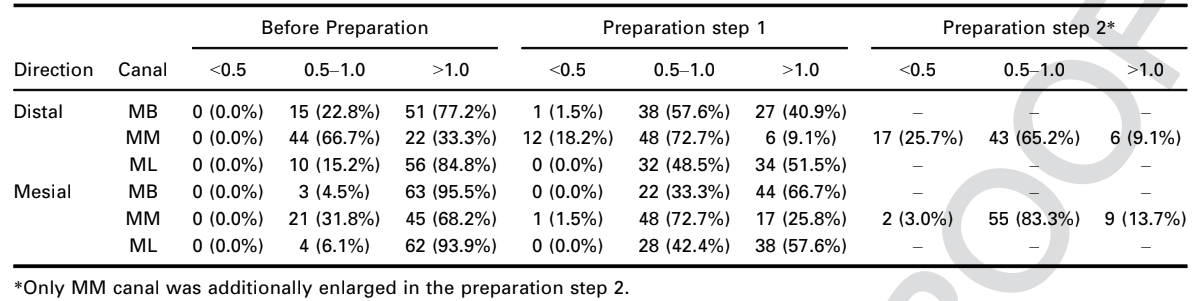
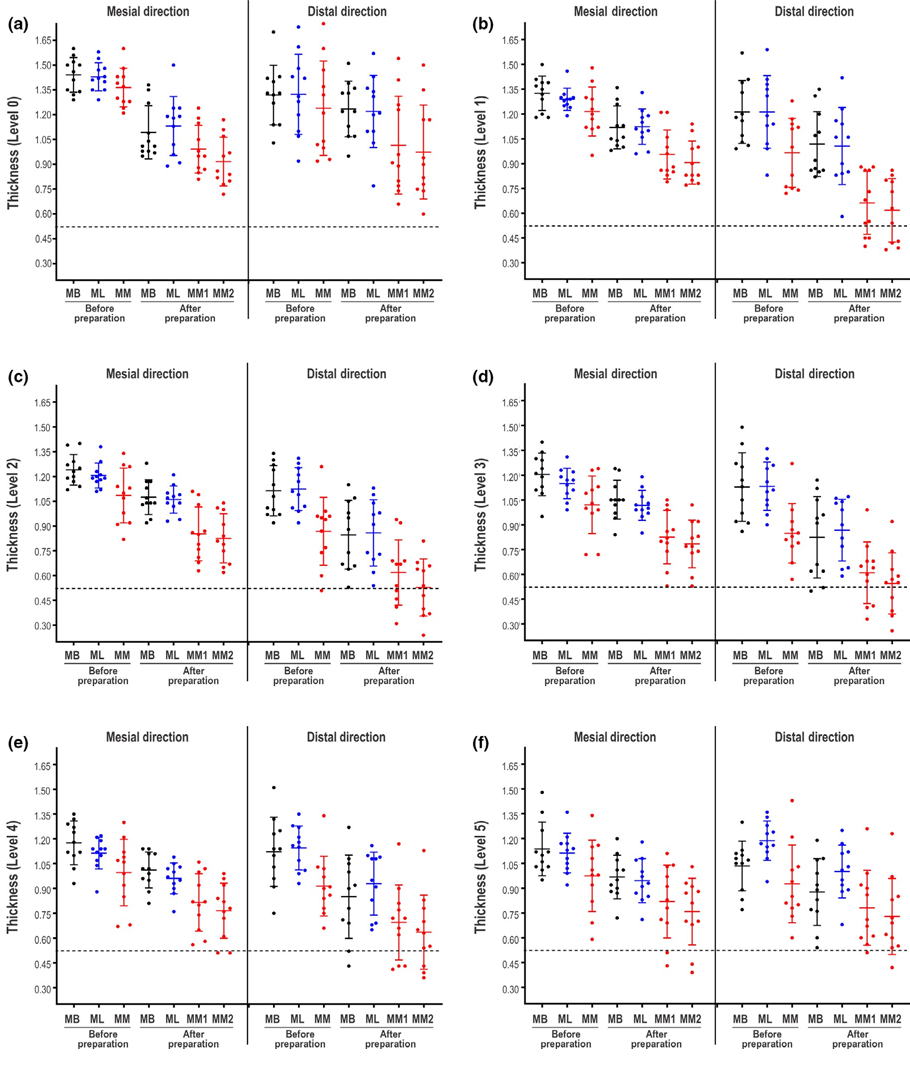
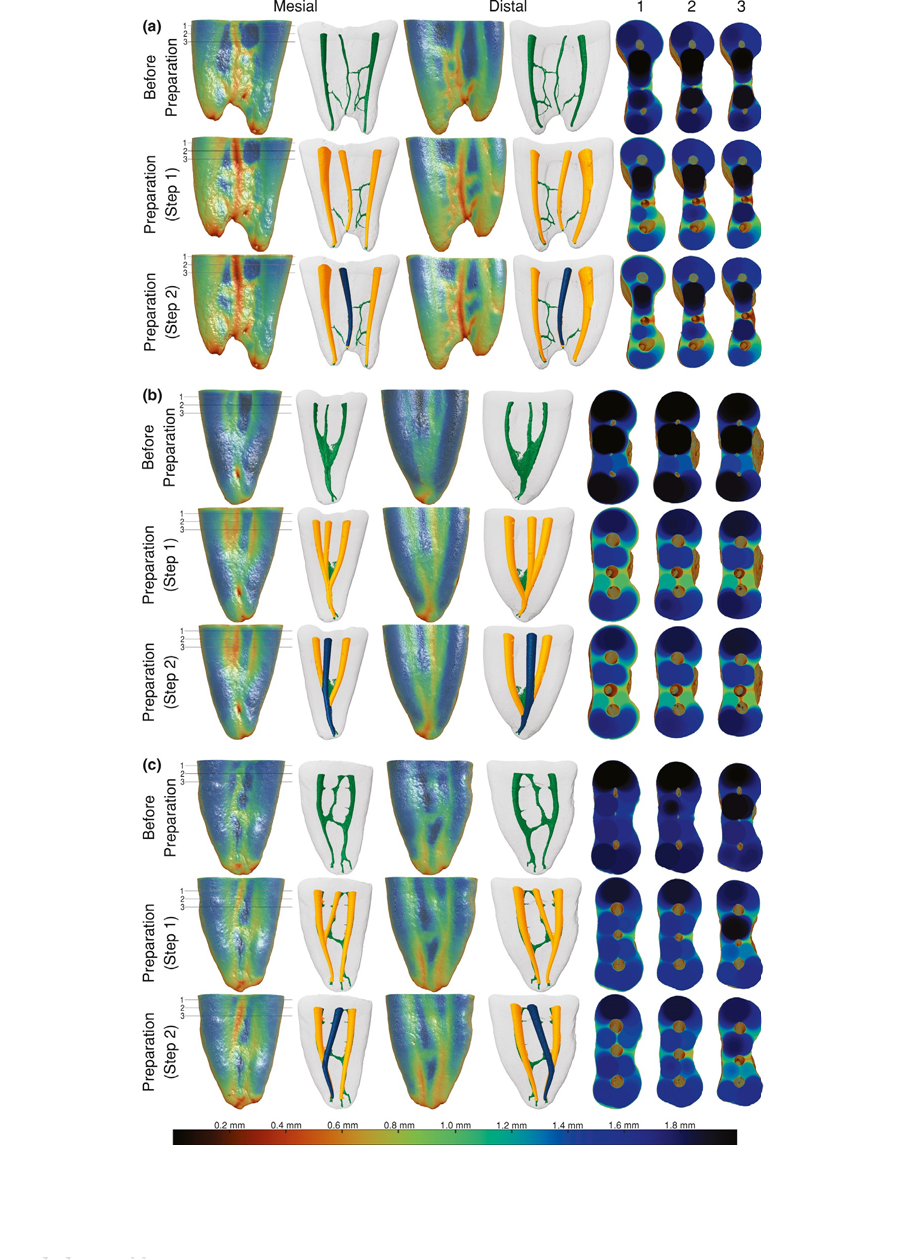
Minimum preoperative dentine thickness was observed towards the mesial (0.59 mm; Table 1) and distal (0.51 mm; Table 2) directions of the MM canal (Fig. 2a). After preparation step 1, dentine thickness of the MM canal in both mesial (0.88 ± 0.18 mm) and distal (0.73 ± 0.26 mm) aspects of the root was significantly thinner than that of the MB (1.05 ± 0.13 mm and 0.94 ± 0.25 mm, respectively) and ML (1.04 ± 0.14 mm and 0.98 ± 0.23 mm, respectively) canals (P < 0.05; Tables 1 and 2; Fig. 1a–f). Dentine thickness less than 0.5 mm was observed mostly towards the distal aspect of the MM canal (18.2%, n = 12; Table 3) from levels 1 to 4 (Fig. 1b–e), whilst to the mesial direction, 72.7% of the slices from levels 2 to 5 (Fig. 1c–f) had dentine thickness ranging from 0.5 to 1 mm (Table 3). After the enlargement of the MB and ML canals with ProTaper Next X3, most of the cross-sections still had a dentine thickness greater than 1 mm. However, 57.6% of the measurements towards the distal direction of the MB canal had thickness between 0.5 and 1 mm (Table 3; Fig. 1). The mean percentage reduction of total dentine volume after preparation step 1 ranged from 2.7% to 7.5% (4.7 ± 1.4%). Although the additional enlargement of the MM canal with ProTaper Next X3 instrument (preparation step 2) resulted in more cross-sections with dentine thickness less than 0.5 mm (Table 3), mean thickness was statistically similar to the results obtained after preparation step 1 at all levels and in both directions (Tables 1 and 2). Minimal thickness was observed at level 2 of MM canals (0.24 mm; Fig. 1), and the mean percentage reduction of dentine volume ranged from 2.8% to 8.5% (5.2 ± 1.7%).
Even though the enlargement of all mesial canals up to the ProTaper X3 instrument reduced dentine thickness in most evaluated root cross-sections, strip perforations were not observed (Fig. 2). Colour-coded models revealed that the noncentred position of the mesial canals and the asymmetric shape of the roots results in a variable dentine thickness at different levels and directions of the roots (Fig. 2). Interestingly, preparation procedures in some cross-sections of 5 specimens did not affect the minimal dentine thickness (Fig. 3).
Discussion
In the classical article of Abou-Rass et al. (1980), the anticurvature technique was introduced to prevent weakening and/or perforation of the root by controlling the direction of preparation away from the thinner portions of the root, the so-called ’danger zone’, a thin area in the inner root canal wall vulnerable to stripping by injudicious filing. This area was illustrated by the authors using clinical cases and schematic drawings of the mesial root of mandibular molars. Since then, the danger zone of mandibular molars has been studied extensively and values ranging from 0.78 to 1.1 mm regarding dentine thickness at the furcation area of the MB and ML canals have been reported (Kessler et al. 1983, Montgomery 1985, Lim & Stock 1987, Garcia Filho et al. 2003). Overall, the results from these studies suggest the pre-operative evaluation of root dentine thickness at the danger zone prior to mechanical preparation of the root canals in order to avoid overinstrumentation or strip perforations. However, in contrast to accepted knowledge, the thought of thinner dentine walls related only to the distal aspect of the mesial roots of mandibular molars has been challenged (Lee et al. 2015, De-Deus et al. 2019). Using micro-CT technology and evaluating hundreds of root cross-sections, it was demonstrated that in 33% (Lee et al. 2015) to 40% (De-Deus et al. 2019) of the evaluated specimens, the thinnest dentine surrounding MB and ML canals was towards the mesial portion of the root, and not the distal direction (furcation area). Notwithstanding this was not the purpose of the present study, it was observed that the position of the thinnest dentine around the MB and ML canal wall also varied in some cross-sections. Thus far, however, only limited information is available regarding this morphological aspect related to the MM canal (Versiani et al. 2016, Akbarzadeh et al. 2017). Therefore, this study attempted to fill this gap in the literature by evaluating the effect of mechanical enlargement on remaining dentinal thickness around MM canals of mandibular first molars.
Overall, preoperative dentine thickness of the MM canal was significantly thinner than that of the MB and ML canals in both directions. These thinnest areas (0.5–1.0 mm) were always located towards the distal aspect of the root (Table 3), with the lowest thickness values (0.5 mm) observed around the MM canal (Tables 1 and 2; Fig. 1). As it would be expected, dentine thickness of the mesial canals decreased significantly in both directions (Tables 1 and 2) at all levels after preparation step 1 (Figs 1 and 2). Once again, MM canals had thinner dentine walls than MB and ML canals (Tables 1 and 2; Fig. 1) and the null hypothesis was rejected. Almost 50% of the evaluated cross-sections of the MB and ML canals had dentine less than 1.0 mm thick after preparation step 1, whilst in 18.2% of the MM canals thickness was less than 0.5 mm towards the distal aspect of the root (Table 3). These findings can be explained by the location of MM canal, since it lies between MB and ML canals where the root thickness is decreased by the presence of a developmental concavity. This information is important clinically as troughing has been suggested as a standardized protocol to access MM canal orifices (Azim et al. 2015), and in some situations, the orifice may be even deeper than 2 mm (Keleş & Keskin 2017). Therefore, because of the thin dentine related to the distal aspect of the MM canal and the position of the orifice, the integrity of root structure at the coronal level might be jeopardized by deep troughing if large instruments are used.
Even though additional enlargement of the MM canal with ProTaper Next X3 increased the number of specimens with dentine thickness less than 0.5 mm (Table 3), the mean thickness was similar to that obtained after preparation with ProTaper Next X2 (Tables 1 and 2). This can be explained by the design of the ProTaper Next instruments. According to the manufacturer, one of advantages of this rotary system is the decreasing taper over the active portion on the same instrument, aiming to preserve coronal dentine during shaping procedures (Ruddle et al. 2013). This design feature results in similar dimensions of X2 (0.84–1.20 mm) and X3 (0.89–1.20 mm) instruments from halfway up the active part up to the shank, that is the portion of the instrument that effectively touches the root canal walls at the levels evaluated in this study. Although these instruments are made of M-Wire alloy to increase flexibility, in some cross-sections it was possible to observe transportation of the canal towards the mesial direction, without affecting dentine thickness along the distal aspect of the root (Fig. 3a,b). In disagreement with this finding, a previous study on the mechanical preparation of mesial canals of mandibular molars with ProTaper Next resulted in well-centred canal flaring and nonsignificant transportation values (mean of 0.09 ± 0.05 mm) (Gagliardi et al. 2015). This difference can be explained because, in that study, the coronal third of the mesial canals was previously flared with Gates-Glidden drills, unlike here in which no coronal enlargement was performed.
Interestingly, even after root canal preparation with rotary instruments with large taper, strip perforations were not observed at any of the evaluated levels (up to 5 mm below the furcation area). Strip perforation in the mesial root of mandibular molars would be more prone to occur at the middle third because the danger zone in this root is usually located between 4 and 7 mm below the furcation area (De-Deus et al. 2019), which helps to explain the present results. One of the methodological limitations of the present study was the inability to evaluate changes in dentine thickness surrounding the MM canal throughout the root in a large number of specimens because this type of sample is relatively rare (Versiani et al. 2016). Moreover, patients’ age, which was unknown in the present study, is a contributing factor for root and root canal anatomy given its effect on the reduction of root canal size following dentine apposition on the canal walls throughout life (Reis et al. 2013).
According to Lim & Stock (1987), dentine thickness values less than 0.3 mm would endanger the integrity of roots, compromising their mechanical resistance. Additionally, it has been reported that resistance to fracture is closely related to the amount of residual tooth structure at the pericervical dentine level, that is the dentine near the alveolar crest extending 4 mm apical to the crestal bone (Clark & Khademi 2010a, 2010b). In this study, an attempt was also made to measure the volume of the root structure after each preparation step, but the results revealed only a small mean percentage reduction of the dentine after preparation steps 1 (4.7%) and 2 (5.2%). Considering that most of the vertical root fractures have a buccolingual pattern and, very rarely, a mesiodistal orientation (Tsesis et al. 2010), there is still no evidence correlating this type of fracture to the reduction of root dentine structure to the mesial or distal direction. Therefore, the removal of dentine alone is unlikely to result in an increased fracture susceptibility, but an interaction of various influencing factors (Sathorn et al. 2005). Therefore, further studies are required to determine precisely what would be the critical dentine thickness values that might jeopardize the integrity of root structure in cases of excessive mechanical preparation or deep troughing procedures. Besides, additional research testing different canal configurations would provide more comprehensive data about this topic.
Conclusion
Dentine thickness of all mesial roots evaluated in this study was affected by the canal preparation procedures using a decreasing percentage tapered rotary system, and even though strip perforations were not created, the present findings support the controlled use of less tapered instruments for troughing and controlled removal of dentine from the mesial canals of mandibular molars during shaping procedures.
Authors: A. Keles, C. Keskin, R. Alqawasmi, M. A. Versiani
References:
- Abou-Rass M, Frank AL, Glick DH (1980) The anticurvature filing method to prepare the curved root canal. Journal of American Dental Association 101, 792–4.
- Akbarzadeh N, Aminoshariae A, Khalighinejad N et al. (2017) The association between the anatomic landmarks of the pulp chamber floor and the prevalence of middle mesial canals in mandibular first molars: an in vivo analysis. Journal of Endodontics 43, 1797–801.
- Azim AA, Deutsch AS, Solomon CS (2015) Prevalence of middle mesial canals in mandibular molars after guided troughing under high magnification: an in vivo investigation. Journal of Endodontics 41, 164–8.
- Clark D, Khademi J (2010a) Modern molar endodontic access and directed dentin conservation. Dental Clinics of North America 54, 249–73.
- Clark D, Khademi JA (2010b) Case studies in modern molar endodontic access and directed dentin conservation. Dental Clinics of North America 54, 275–89.
- Costa FFNP, Pacheco-Yanes J, Siqueira JF Jr et al. (2019) Association between missed canals and apical periodontitis. International Endodontic Journal 52, 400–6.
- De-Deus G, Rodrigues EA, Belladonna FG et al. (2019) Anatomical danger zone reconsidered: a micro-CT study on dentine thickness in mandibular molars. International Endodontic Journal 52, 1501–7.
- Gagliardi J, Versiani MA, de Sousa-Neto MD et al. (2015) Evaluation of the shaping characteristics of ProTaper Gold, ProTaper NEXT, and ProTaper universal in curved canals. Journal of Endodontics 41, 1718–24.
- Garcia Filho PF, Letra A, Menezes R, Carmo AM (2003) Danger zone in mandibular molars before instrumentation: an in vitro study. Journal of Applied Oral Science 11, 324–6.
- Gluskin AH, Peters CI, Peters OA (2014) Minimally invasive endodontics: challenging prevailing paradigms. British Dental Journal 216, 347–53.
- Karabucak B, Bunes A, Chehoud C et al. (2016) Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: a cone-beam computed tomography study. Journal of Endodontics 42, 538–41.
- Keleş A, Keskin C (2017) Detectability of middle mesial root canal orifices by troughing technique in mandibular molars: a micro-computed tomographic study. Journal of Endodontics 43, 1329–31.
- Kessler JR, Peters DD, Lorton L (1983) Comparison of the relative risk of molar root perforations using various endodontic instrumentation techniques. Journal of Endodontics 9, 439–47.
- Kim SY, Kim BS, Woo J, Kim Y (2013) Morphology of mandibular first molars analyzed by cone-beam computed tomography in a Korean population: variations in the number of roots and canals. Journal of Endodontics 39, 1516–21.
- Lee JK, Yoo YJ, Perinpanayagam H et al. (2015) Three-dimensional modelling and concurrent measurements of root anatomy in mandibular first molar mesial roots using micro-computed tomography. International Endodontic Journal 48, 380–89.
- Lim SS, Stock CJ (1987) The risk of perforation in the curved canal: anticurvature filing compared with the stepback technique. International Endodontic Journal 20, 33–9.
- Martins JNR, Marques D, Silva E et al. (2019) Prevalence studies on root canal anatomy using cone-beam computed tomographic imaging: a systematic review. Journal of Endodontics 45, 372–86.
- Montgomery S (1985) Root canal wall thickness of mandibular molars after biomechanical preparation. Journal of Endodontics 11, 257–63.
- Reis AGAR, Soares-Grazziotin R, Barletta FB et al. (2013) Second canal in mesiobuccal root of maxillary molars is correlated with root third and patient age: a cone-beam computed tomography study. Journal of Endodontics 39, 588–92.
- Ruddle CJ, Machtou P, West JD (2013) The shaping movement: fifth-generation technology. Dentistry Today 32, 96– 99.
- Sathorn C, Palamara JE, Palamara D, Messer HH (2005) Effect of root canal size and external root surface morphology on fracture susceptibility and pattern: a finite element analysis. Journal of Endodontics 31, 288–92.
- Siqueira JF Jr (2001) Aetiology of root canal treatment failure: why well-treated teeth can fail. International Endodontic Journal 34, 1–10.
- Tsesis I, Rosen E, Tamse A, Taschieri S, Kfir A (2010) Diagnosis of vertical root fractures in endodontically treated teeth based on clinical and radiographic indices: a systematic review. Journal of Endodontics 36, 1455–8.
- Versiani MA, Ordinola-Zapata R, Keleş A et al. (2016) Middle mesial canals in mandibular first molars: A micro-CT study in different populations. Archives of Oral Biology 61, 130–7.