Preserving dentine in minimally invasive access cavities does not strength fracture resistance of restored mandibular molars
Abstract
Aim: To evaluate the correlation between the volume of dental hard tissues removed and the fracture resistance of mandibular molar teeth with ultraconservative (UltraAC) or traditional (TradAC) access cavity preparations.
Methodology: Sixty recently extracted and intact mandibular first molars were scanned in a microcomputed tomographic (micro-CT) device, anatomically matched and assigned at random to 2 groups (n = 30), according to the access cavity type: UltraAC or TradAC. After access preparation, mesial and distal canals were prepared using Reciproc instruments and a new scan was taken. The volumes of pulp chamber and dental hard tissues in each specimen were measured before and after the experimental procedures, and the percentage volume reduction of hard tissues calculated for the entire tooth and for the crown separately. Teeth were then root filled, restored and subjected to fracture resistance tests in an universal testing machine. The force required to fracture was recorded in Newtons (N). The adherence of the variables to a Gaussian curve was verified using a Shapiro–Wilk test. Skewed data were analysed with nonparametric Wilcoxon signed rank or Spearman correlation tests, whilst the normally distributed data were analysed with a dependent samples Student t-test. Level of significance was set at 5%.
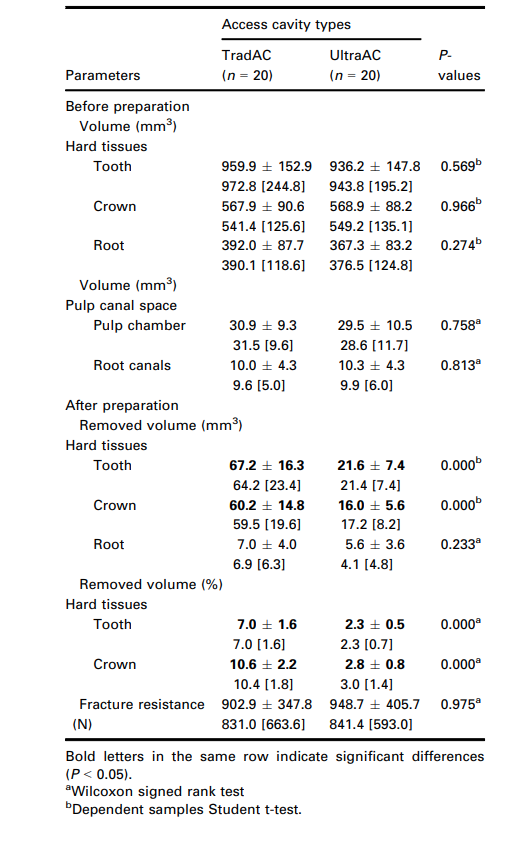
Results: Pre-operatively, no difference was observed between groups regarding the volume of pulp canal space or dental hard tissues (P > 0.05). After access preparation, volumes of the removed hard tissues from the entire tooth and from the crown were significantly greater in teeth prepared with TradAC than with UltraAC (P < 0.05). No significant difference was observed in the fracture resistance values between TradAC (902.9 ± 347.8 N) and UltraAC (948.7 ± 405.7 N) groups (P = 0.975). The Spearman test was unable to identify a correlation between fracture resistance and percentage volume of removed dental hard tissues in the entire root (P = 0.525, r = —0.084) or only in the crown (P = 0.152, r = —0.187).
Conclusion: The volume of hard dental tissues removed, although greater in teeth with TradAC compared to UltraAC, did not correlate with the fracture resistance results, indicating that a minimally invasive access cavity did not increase the resistance of restored mandibular first molars to fracture.
Introduction
The introduction of the minimal invasion concept in Endodontics, known as Minimally Invasive Endodontics (MIE), has been one of the most debated topics amongst enthusiastic professionals within the specialty in recent years. It is based on the hypothesis that preserving as much of the tooth crown structure as possible, including the pulp chamber roof and pericervical dentine, would be a basic requirement to prevent fracture of root filled teeth (Clark & Khademi 2010a,b). This initial proposal for conservative access preparations paved the way for the introduction of the so-called ultraconservative access cavity (UltraAC), commonly known as ‘ninja’ access (Plotino et al. 2017). UltraAC is an extreme example of the MIE concept and is designed for maximum preservation of dentine with minimal removal of the pulp chamber roof. As opposed to the traditional access cavity (TradAC), where the roof of the pulp chamber is removed completely and direct access up to the coronal third of root canals is created (Ingle 1985, Patel & Rhodes 2007), with the UltraAC the central fossa is accessed but with no further extensions, maintaining as much of the pulp chamber roof as possible as well as the pericervical dentine (Augusto et al. 2020, Silva et al. 2020a). The concept behind a positive association between the amount of dental structure preserved during access cavity preparation and fracture resistance seems to be logical, but up to now, it has not been validated scientifically (Silva et al. 2020b).
In the literature, most laboratory studies concluded that minimally invasive access cavities do not improve the fracture resistance of teeth (Moore et al. 2016, Chlup et al. 2017, Ivanoff et al. 2017, Rover et al. 2017, Corsertino et al. 2018, Sabeti et al. 2018, Augusto et al. 2020, Barbosa et al. 2020, Silva et al. 2020a). However, others reported greater tooth strength associated with UltraAC compared to TradAC (Krishan et al. 2014, Plotino et al. 2017, Abou-Elnaga et al. 2019, Zhang et al. 2019, Wang et al. 2020). As recently reported (Silva et al. 2020b), some methodological issues, mostly related to the lack of anatomical matching of tested specimens, storage conditions and sample preparation, have confounded the reliability of the results and partially explain these divergencies. In addition, although some studies suggested that there would be no correlation between the percentage of dentine removed by access cavities and the fracture resistance of teeth, in fact only a few accurately measured the volume of dental hard tissues removed after access preparation (Plotino et al. 2017, Isufi et al. 2020). In this context, the possibility to find a correlation between the fracture resistance and the volume of dentine and enamel removed after UltraAC and TradAC represents an unexplored line of investigation, essential to improve understanding of the impact of MIE on the preservation of tooth strength. The aim this study was based on the null hypothesis that no correlation exists between fracture resistance of root filled and restored mandibular first molars and the volume of dental hard tissues removed by the access cavity and root canal preparations.
Material and methods
Sample size calculation
The sample size was estimated based on an effect size of 1.90 calculated according to previous reported values on load at fracture of molar teeth prepared with TradAC or UltraAC (Plotino et al. 2017). The t-tests family at G*Power 3.1 software (Heinrich Heine University, Dusseldorf, Germany) were used to conduct the analysis (power level of 80%, a = 0.05) yielding a sample size of 18 teeth (n = 9 per group) as sufficient for detecting difference between groups. However, in order to increase certainty for the experiment, a total of 60 teeth (n = 30 per group) were included.
Sample selection and preparation
After approval of this research project by the local ethics committee (protocol 2.743.783), seventy recently extracted (no longer than six months) mandibular first molars with fully formed apices and intact crowns were selected from a tooth bank, cleaned and stored in distilled water until use. All teeth were scanned in a micro-CT device (SkyScan 1173; Bruker-micro-CT, Kontich, Belgium) within one week from this preliminary selection at 20 lm (pixel size), 70 kv, 114 mA, 360° rotation around the vertical axis, rotation step of 0.5°, frame averaging of 4 and camera exposure time of 272 ms. The X-ray beam was pre-filtered with a 0.5-mm-thick aluminium plate. Then, projection images were reconstructed into approximately 800–900 cross-sectional slices per tooth (NRecon software v.1.7.4.2; Bruker-micro-CT), using standardized parameters of beam hardening correction (20%), ring artefact correction (1) and smoothing (2). DataViewer software v.1.5.6 (Bruker-micro-CT) was used to evaluate the root canal configuration and exclude specimens with defects, craze lines, cracks, caries, resorption, cusp abrasion, cervical abrasion/erosion, fractures or incomplete root formation. Only teeth with one distal canal and a Vertucci’s type II canal configuration (Vertucci 1984) with isthmus type V (Hsu & Kim 1997) in the mesial root were selected. Then, ImageJ v.1.8.0_172 software (National Institutes of Health, Bethesda, MD, USA) was used to calculate the volumes of the root canal and the pulp chamber, as well as, of the dental hard tissues for the entire tooth, for the root and the crown itself. Considering that the crown is basically defined as the anatomical portion of teeth covered by enamel, the criteria adopted to determine its limit were the presence of enamel in at least one of the tooth surfaces (buccal, lingual, mesial or distal) of the cross-sectional images. Then, based on these morphometric parameters, sixty teeth were pair-matched and distributed into 2 experimental groups at random, according to the access cavity type:
Group 1 (n = 30)
A traditional access cavity (TradAC) was prepared using spherical (1012HL; KG Sorensen, Sa~o Paulo, Brazil) and Endo Z (Dentsply Sirona, Ballaigues, Switzerland) burs mounted on a high-speed handpiece with water cooling. In this group, the pulp chamber roof was completely removed and straight-line access to the root canal orifices was established with smoothly divergent axial walls (Ingle 1985, Patel & Rhodes 2007).
Group 2 (n = 30)
An ultraconservative access cavity (UltraAC) was prepared using the same burs as in Group 1. All teeth were accessed at the central fossa, but with no further extensions, maintaining as much of the pulp chamber roof and pericervical dentine as possible (Plotino et al. 2017, Augusto et al. 2020, Silva et al. 2020a).
After access cavity preparation, canal patency was achieved with a size 10 K-file (Dentsply Sirona) and working length established 1 mm short of the apical foramen, followed by glide path preparation with a size 15 K-file (Dentsply Sirona). Mesial and distal canals were prepared using Reciproc R25 (size 25, .08v taper) and R40 (size 40, .06v taper) instruments (VDW, Munich, Germany), respectively, powered by an electric motor (VDW Silver; VDW), according to the manufacturer’s directions. Each root canal was irrigated with a total of 6 mL of 2.5% sodium hypochlorite using a 30-gauge Endo-Eze needle (Ultradent Products Inc., South Jordan, UT, USA) inserted 2 mm up to the working length. Final irrigation was performed with 3 mL of 2.5% sodium hypochlorite followed by 3 mL of 17% ethylenediaminetetraacetic acid (3 min) and 3 mL of distilled water for 5 min. Then, root canals were dried with absorbent paper points and the specimens submitted to a new scan and reconstruction applying the afore-mentioned parameter settings. After scanning, specimens were kept at 100% relative humidity (37 °C) until the next experimental step. Post-operative images of each specimen were rendered (ImageJ v.1.8.0_172; National Institutes of Health) and coregistered with its respective preoperative datasets using the affine registration algorithm of the 3D Slicer software v. 4.5.0 (available from http://www.slicer.org). Then, the volume of hard tissues of each specimen was measured for the entire tooth, for the root, and for the crown, before (Vb) and after (Va) the experimental procedures (ImageJ v.1.8.0_172; National Institutes of Health; Table 1). Then, the percentage volume reduction of dental hard tissues for the entire tooth and separately for the crown was calculated using the formula: [(Vb – Va)*100]/Vb (De-Deus et al. 2020).
Root canal filling and restoration
After coating the canal walls with an epoxy resin-based sealer (AH Plus; Dentsply De Trey, Konstanz, Germany), the mesial and distal root canals were filled using the single-cone technique with R25 and R40 Reciproc gutta-percha cones (VDW), respectively. The master cones were sectioned at the orifice level and the pulp chamber completely cleaned with cotton pellets soaked in 70% alcohol. Subsequently, the pulp chamber and the access cavity walls were etched for 15 s with 37% phosphoric acid gel (Condac 37; FGM, Joinville, Brazil), rinsed with water-spray for 30 s and gently air-dried. After that, two layers of the bonding agent (Adper Single Bond 2; 3M ESPE, St Paul, MN, USA) were applied and light-cured for 20 s (Radii-cal; SDI, Bayswater, Australia). Then, a nano-particulate composite restoration (Vittra APS; FGM) was applied to the access cavity in 1.5-mm-thick increments (cured for 20 s), according to the manufacturer’s recommendation, followed by the storage of the specimens at 100% relative humidity (37 °C) for 1 week. No flowable composite was used considering that previous studies (Atalay et al. 2016, Isufi et al. 2016) did not report any influence of this type of material on the fracture resistance of endodontically treated molars. All endodontic and restorative procedures (access cavity preparation, root canal preparation, root canal filling and restoration) were accomplished by an experienced operator using an operating microscope over a period of 10 days.
Load at fracture
The root of each specimen was covered with a 0.3-mm-thick high fusion wax (Galileo; Talladium Inc., Valencia, CA, USA) to simulate the periodontal ligament (Krishan et al. 2014, Augusto et al. 2020, Bar- bosa et al. 2020) and embedded into acrylic resin (JET; Campo Limpo Paulista, SP, Brazil) to simulate the alveolar bone (Krishan et al. 2014, Augusto et al. 2020, Barbosa et al. 2020). Each acrylic block was positioned and stabilized on the lower plate of a universal testing machine (EMIC DL2000; EMIC, São José dos Pinhais, PR, Brazil) to allow the tip of a stainless-steel spherical tip (4 mm in diameter) to be positioned at the central fossa at 30° in relation to the long axis of the tooth (Rover et al. 2017). The load was applied at a cross-head speed of 1 mm min—1 until fracture occurred, represented by a sharp drop in the force detected by a dedicated software (Tesc EMIC). The force required to fracture was recorded in Newtons (N).
Statistical analysis
The adherence of the variables to a Gaussian curve was verified using a Shapiro–Wilk test, and those that were skewed were analysed with nonparametric the Wilcoxon signed rank test or the Spearman correlation test, whilst the normally distributed data were analysed with the parametric-dependent samples Student t-test. Firstly, the volumes of dental hard tissues (entire tooth, crown and root) and the canal space (pulp chamber and root canals) in the unprepared samples were compared between groups to validate their anatomical similarity. Then, the amount of dental hard tissues removed by the access preparation and root canal instrumentation as well as the results from the fracture resistance test were compared. Finally, a possible correlation between the fracture resistance results and the percentage volume reduction of hard tissues was verified. The Alpha-type error boundary limit for rejecting the null hypothesis was 5% (SPSS v.21.0; SPSS Inc., Chicago, IL, USA).
Results
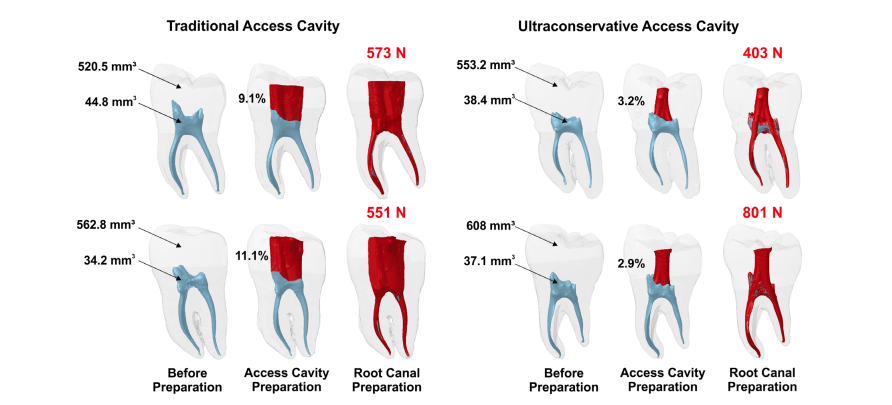
Table 1 summarizes the results of the tested variables obtained before and after preparation of mandibular molars with TradAC and UltraAC, whilst Figure 1 shows 3D models of representative specimens from each group. At baseline, the calculated volumes of dental hard tissues (entire tooth, crown and root) and canal space (pulp chamber and root canals) were similar between groups (P > 0.05), which validates sample selection and distribution. Similarly, after root canal instrumentation, no difference was observed in the amount of dental tissue removed from the roots (P = 0.233), indicating no biased influence of the instrumentation technique over the amount of tooth tissues removed by the access preparation itself. As it would be expected, the volumes of the hard tissues removed from the entire tooth, and from the crown separately, were significantly greater in teeth prepared with TradAC than with UltraAC (P < 0.001 and P < 0.001, respectively); however, no significant difference was observed in the fracture resistance results (P = 0.975; Table 1; Fig. 1). The Spearman test was unable to find any correlation between groups regarding the fracture resistance and the percentage of dental hard tissues removed in the entire root (P = 0.525, r = —0.084) or only in the crown (P = 0.152, r = —0.187).
Discussion
Fracture of root filled teeth has generally been assigned to an excessive loss of dentine resulted from the access cavity preparation (Kishen, 2006, Tzimpoulas et al. 2012). Thus, minimally invasive cavities were suggested in an attempt to maintain the fracture resistance of teeth by partially preserving the pulp chamber roof and pericervical dentine (Clark & Khademi 2010a). Although these pursuits are plausibility, so far, scientific findings are inconsistent and do not support the concept (Krishan et al. 2014, Moore et al. 2016, Chlup et al. 2017, Ivanoff et al. 2017, Plotino et al. 2017, Rover et al. 2017, Corsentino et al. 2018, Sabeti et al. 2018, Silva et al. 2018, 2020a, Abou-Elnaga et al. 2019, Zhang et al. 2019, Augusto et al. 2020, Barbosa et al. 2020, Wang et al. 2020). However, up to now, no study has correlated the amount of hard tissues removed by the access cavity preparation and the fracture resistance of teeth in order to obtain a better understanding of this phenomenon. Therefore, the present study aimed to evaluate this correlation in mandibular first molars prepared with UltraAC or TradAC using a robust and comprehensive model selection strategy. The Spearman test validated the hypothesis that the benefit in dental tissue preservation was not associated with the fracture resistance of root filled and restored teeth. However, this finding is in disagreement with a report that concluded greater fracture resistance strength of teeth with UltraAC compared to TradAC (Plotino et al. 2017), which may be explained by methodological differences. Plotino et al. (2017) based their anatomical sample selection and matching on a non-validated external measurement of the crown with a digital caliper, which differs substantially from the accurate 3D volumetric-based anatomical matching of hard tissues and pulp chamber volumes performed in the present study (Table 1). More recently, Isufi et al. (2020) proposed to categorise various access cavity formats based on the percentage of hard tissue removed after access preparation. According to the authors, for a given access cavity to be labelled as ‘traditional’ in mandibular molars, the percentage volume of dentine and enamel removed should be greater than 16% of the original volume of the crown. In the present study, however, although access preparations followed proper guidelines, several samples did not fit into the proposed classification with mean percentages of removed hard tissues being 10.6% and 2.8% in the TradAC and UltraAC groups, respectively. These findings clearly demonstrate that classifying cavities based only on the percentage of dental hard tissues removed lacks evidence as it may be influenced by the pulp chamber volume. For instance, a large pulp chamber may proportionally result in more preserved tissue when accessed by minimally invasive access cavities when compared to a small-sized chamber accessed using the same technique.
From a methodological perspective, sample preparation before a fracture test is a critical step that may affect the outcome of experimental procedures even after selecting teeth using strict criteria (Silva et al. 2020b). It must be taken into consideration that dentine removed by root canal preparation may affect the fracture resistance of teeth (Tang et al. 2010), but that the filling procedure and coronal restoration might contribute to the re-establishment of the fracture resistance of teeth by approximately 80% (Hamouda & Shehata 2011, Sandikci & Kaptan 2014). Consequently, these are important methodological steps to be performed in the selected specimens before the fracture test, notwithstanding some authors reported that these would introduce confounding variables to the test (Krishan et al. 2014, Moore et al. 2016, Ivanoff et al. 2017, Sabeti et al. 2018). In fact, performing canal filling and coronal restoration before the fracture test not only properly prepares the samples for the test, but also reproduces the technical procedures involved in every root filled tooth in a clinical setup. Therefore, in the present study, both groups were anatomically balanced according to the hard tissue and root canal space volumes before access cavity preparation (Table 1), and then, the canals were filled and the tooth restored, in an attempt to avoid anatomical and experimental bias that have been demonstrated to influence fracture resistance tests. Although previous studies reported shrinkage stress reduction through the use of a flowable resin in between the composite and the pulp chamber floor (De Gee et al. 1993, Oliveira et al. 2010, Aggarwal et al. 2014) and that restoration of molar teeth with UltraAC has been associated with a high incidence of voids (Silva et al. 2020c), a flowable composite was not used in this experiment considering that no difference was observed in the fracture resistance of teeth in which UltrAC and TradAC were restored using this material (Silva et al. 2020a). In this way, the present results suggest that fracture resistance of molars with UltrAC or TradAC restored only with composite, may not be affected. On the other hand, it is important to consider that only sound molars were used in this study and the influence of gaps and voids in compromised teeth restored with different materials is still unclear and needs additional research.
To properly validate and guarantee a sound correlation test between the removed dental tissues and the fracture resistance outcome, it is relevant confirm a statistically significant difference in the amount of tissue removed between the two groups after access cavity preparation, whilst keeping the other variables constant (Table 1). As discussed earlier, the presumption that UltraAC would amount to smaller percentages of removed tissue compared to TradAC is quite logical and thereby would imply a correlation with the fracture resistance results. Actually, logical reasoning dictates that for every unit loss in hard tissue volume, a correlative drop in the ability to resist compression forces would result. However, because teeth are different in terms of hard tissue volume, it is better to determine the percentage reduction in relation to the original tooth volume and correlate it to the fracture strength. In this study, the volumes of the dental hard tissues removed from the entire tooth, or only from the crown, were significantly greater in teeth prepared with TradAC than with UltraAC; on the other hand, no correlation was found between this percentage of reduction and fracture resistance (Table 1). This implies that the preserved hard tissues did not increase the resistance of restored mandibular molars. This finding rejects the alleged fracture resistance benefit of minimally invasive access cavities when the tooth is root filled and restored. Actually, minimally invasive access cavities have been reported to negatively affect the general outcome of root canal treatment by impairing root canal detection (Rover et al. 2017, Saygili et al. 2018), proper canal cleaning (Neelakantan et al. 2018) and the overall quality of canal shaping (Krishan et al. 2014, Barbosa et al. 2020), canal disinfection (Vieira et al. 2020) and canal filling (Barbosa et al. 2020, Silva et al. 2020a). Besides, previous studies described a significantly greater degree of root canal transportation after shaping through conservative endodontic access cavities (ConsAC) compared to traditional ones (Alovisi et al. 2018, Rover et al. 2017). This might be justified by the fact that minimal access cavities have considerable coronal interferences that may cause an excessive deflection of the active part of the instruments and, consequently, an irregular distribution of lateral forces within the root canal space which becomes overprepared on the internal surface of the canal (Eaton et al. 2015, Rover et al. 2017, Alovisi et al. 2018). Previous findings reported that root canal preparation in teeth with ConsAC using thermally treated instruments resulted in major deviation of the original anatomy at the apical level of the palatal canal of maxillary molars (Rover et al. 2017) and in the mesial canals of mandibular molars (Alovisi et al. 2018). The volume of hard tissues removed from the root portion after preparation is slightly lower in the UltraAC group (even if not statistically significant). Therefore, in contrast to the initial presumption, the evidence to date does not support the regular use of minimally invasive access cavities in routine clinical practice.
Although this experimental research attempted to overcome several methodological drawbacks that occurred in previous studies, it also has an important limitation: tooth age was not taken into consideration in sample selection. Various studies acknowledge that tooth age negatively impacts tooth toughness and ductility by reducing the endurance limit of dentine (Arola & Reprogel 2005, Kinney et al. 2005, Bajaj et al. 2006, Nazari et al. 2009, Ivancik et al. 2012). Consequently, further studies should be performed to evaluate the influence of tooth age on fracture resistance of root filled and restored teeth with various access cavity designs. Moreover, it is important to point out that there are two types of methods that can be used to test the fracture resistance of teeth: (i) the static test, used in the present setup, which consists of a single and continuous load applied to the occlusal surface of the teeth by an universal testing machine, and (ii) the dynamic test, in which teeth are subjected to multiple loading cycles with varying strengths and temperatures, simulating clinical conditions. This is another limitation of the present study considering that the statistic test does not replicate the dynamics of masticatory forces on teeth in function and in fact it measures the maximum load capacity of teeth. Therefore, further research using the dynamic method is recommended in order to test the fracture resistance of teeth with different access cavity preparations. Another issue that should be discussed is that, clinically, root canal treatment is mainly performed on molars affected by extensive caries destruction and loss of coronal tissue, which are usually considered a determinant for fracture resistance. Future studies should also consider an experimental setup with the absence of one or two proximal walls to test its relation to the fracture resistance of teeth with minimally invasive access cavities.
Conclusion
The volume of hard dental tissues removed was greater in teeth with TradAC than UltraAC, but this did not correlate with the fracture resistance results, indicating that the minimally invasive access cavity did not increase the resistance of root filled and restored mandibular first molars to fracture.
Authors: E. J. N. L. Silva, C. O. Lima, A. F. A. Barbosa, C. M. Augusto, E. M. Souza, R. T. Lopes, G. De-Deus, M. A. Versiani
References:
- Abou-Elnaga MY, Alkhawas MAM, Kim H, Refai AS (2019) Effect of truss access and artificial truss restoration on the fracture resistance of endodontically treated mandibular first molars. Journal of Endodontics 45, 813–7.
- Aggarwal V, Singla M, Yadav S, Yadav H (2014) Effect of flowable composite liner and glass ionomer liner on class II gingival marginal adaptation of direct composite restorations with different bonding strategies. Journal of Dentistry 42, 619–25.
- Alovisi M, Pasqualini D, Musso E et al. (2018) Influence of contracted endodontic access on root canal geometry: an in vitro study. Journal of Endodontics 44, 614–20.
- Arola D, Reprogel RK (2005) Effects of aging on the mechanical behavior of human dentin. Biomaterials 26, 4051–61.
- Atalay C, Yazici AR, Horuztepe A, Nagas E, Ertan A, Ozgunaltay G (2016) Fracture resistance of endodontically treated teeth restored with bulk fill, bulk fill flowable, fiber-reinforced, and conventional resin composite. Operative Dentistry 41, E131–E140.
- Augusto CM, Barbosa AFA, Lima CO et al. (2020) A laboratory study on the impact of ultraconservative access cavities and minimal root canal tapers on the ability to shape canals in extracted mandibular molars and their fracture resistance. International Endodontic Journal 53, 1516–29.
- Bajaj D, Sundaram N, Nazari A, Arola D (2006) Age, dehydration and fatigue crack growth in dentin. Biomaterials 27, 2507–17.
- Barbosa AFA, Silva EJNL, Coelho BP, Ferreira CMA, Lima CO, Sassone LM (2020) The influence of endodontic access cavity design on the efficacy of canal instrumentation, microbial reduction, root canal filling and fracture resistance in mandibular molars. International Endodontic Journal 53, 1666–79.
- Chlup Z, Zizka R, Kania J, Pribyl M (2017) Fracture behaviour of teeth with conventional and mini-invasive access cavity designs. Journal of the European Ceramic Society 37, 4423–9.
- Clark D, Khademi JA (2010a) Modern molar endodontic access and directed dentin conservation. Dental Clinics of North America 54, 249–73.
- Clark D, Khademi JA (2010b) Case studies in modern molar
- endodontic access and directed dentin conservation. Dental Clinics of North America 54, 275–89.
- Corsentino G, Pedullà E, Castelli L et al. (2018) Influence of
- access cavity preparation and remaining tooth substance on fracture strength of endodontically treated teeth. Journal of Endodontics 44, 1416–21.
- De Gee AF, Feilzer AJ, Davidson CL (1993) True linear polymerization shrinkage of unfilled resins and composites determined with a linometer. Dental Materials 9, 11–4.
- De-Deus G, Simões-Carvalho M, Belladonna FG et al. (2020) Arrowhead design ultrasonic tip as a supplementary tool for canal debridement. International Endodontic Journal 53, 410–20.
- Eaton JA, Clement DJ, Lloyd A, Marchesan MA (2015) Micro-computed tomographic evaluation of the influence of root canal system landmarks on access outline forms and canal curvatures in mandibular molars. Journal of Endodontics 41, 1888–91.
- Hamouda IM, Shehata SH (2011) Fracture resistance of posterior teeth restored with modern restorative materials. The Journal of Biomedical Research 25, 418–24.
- Hsu YY, Kim S (1997) The resected root surface. The issue of canal isthmi. Dental Clinics of North America 41, 529– 40.
- Ingle JI (1985) Endodontic cavity preparation. In: Ingle JI, Tamber J, eds. Endodontics, 3rd edn. Philadelphia, PA: Lea & Febiger, pp 102–67.
- Isufi A, Plotino G, Grande NM et al. (2016) Fracture resistance of endodontically treated teeth restored with abulkfill flowable material and a resin composite. Annali di Stomatologia (Roma) 7, 4–10.
- Isufi A, Plotino G, Grande NM, Testarelli L, Gambarini G (2020) Standardization of endodontic access cavities based on 3-dimensional quantitative analysis of dentin and enamel removed. Journal of Endodontics 46, 1495–500.
- Ivancik J, Majd H, Bajaj D, Romberg E, Arola D (2012) Contributions of aging to the fatigue crack growth resistance of human dentin. Acta Biomaterialia 8, 2737–46.
- Ivanoff CS, Marchesan MA, Andonov B et al. (2017) Fracture resistance of mandibular premolars with contracted or traditional endodontic access cavities and class II temporary composite restorations. Endodontic Practice Today 11, 7–14.
- Kinney JH, Nalla RK, Pople JA, Breunig TM, Ritchie RO (2005) Age-related transparent root dentin: mineral con- centration, crystallite size, and mechanical properties. Biomaterials 26, 3363–76.
- Kishen A (2006) Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endodontic Topics 13, 57–83.
- Krishan R, Paqué F, Ossareh A, Kishen A, Dao T, Friedman S (2014) Impacts of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors, premolars, and molars. Journal of Endodontics 40, 1160–6.
- Moore B, Verdelis K, Kishen A, Dao T, DipProstho FS (2016) Impacts of contracted endodontic cavities on instrumentation efficacy and biomechanical responses in maxillary molars. Journal of Endodontics 42, 1779–83.
- Nazari A, Bajaj D, Zhang D, Romberg E, Arola D (2009) Aging and the reduction in fracture toughness of human dentin. Journal of the Mechanical Behavior of Biomedical Materials 2, 550–9.
- Neelakantan P, Khan K, Hei GP, Yip CY, Zhang C, Pan Cheung GS (2018) Does the orifice-directed dentin conservation access design debride pulp chamber and mesial root canal systems of mandibular molars similar to a traditional access design? Journal of Endodontics 44, 274–9.
- Oliveira LC, Duarte S Jr, Araujo CA, Abrahaõ A (2010) Effect of low-elastic modulus liner and base as stress-absorbing layer in composite resin restorations. Dental Materials 26, 159–69.
- Patel S, Rhodes J (2007) A practical guide to endodontic access cavity preparation in molar teeth. British Dental Journal 203, 133–40.
- Plotino G, Grande NM, Isufi A et al. (2017) fracture strength of endodontically treated teeth with different access cavity designs. Journal of Endodontics 43, 995–1000.
- Rover G, Belladonna FG, Bortoluzzi EA, De-Deus G, Silva EJNL, Teixeira CS (2017) Influence of access cavity design on root canal detection, instrumentation efficacy, and fracture resistance assessed in maxillary molars. Journal of Endodontics 43, 1657–62.
- Sabeti M, Kazem M, Dianat O et al. (2018) Impact of access cavity design and root canal taper on fracture resistance of endodontically treated teeth: an ex vivo investigation. Journal of Endodontics. 44, 1402–6.
- Sandikci T, Kaptan RF (2014) Comparative evaluation of the fracture resistances of endodontically treated teeth filled using five different root canal filling systems. Nigerian Journal of Clinical Practice 17, 667–72.
- Saygili G, Uysal B, Omar B, Ertas ET, Ertas H (2018) Evaluation of relationship between endodontic access cavity types and secondary mesiobuccal canal detection. BMC Oral Health 18, 121.
- Silva AA, Belladonna FG, Rover G et al. (2020a) Does ultraconservative access affect the efficacy of root canal treatment and the fracture resistance of two-rooted maxillary premolars? International Endodontic Journal 53, 265–75.
- Silva EJNL, Oliveira VB, Silva AA et al. (2020c) Effect of access cavity design on gaps and void formation in resin composite restorations following root canal treatment on extracted teeth. International Endodontic Journal 53, 1540– 8.
- Silva EJNL, Pinto KP, Ferreira CM et al. (2020b) Current status on minimal access cavity preparations: a critical analysis and a proposal for a universal nomenclature. International Endodontic Journal 53, 1618–35.
- Silva EJNL, Rover G, Belladonna FG, De-Deus G, Teixeira CS, Fidalgo TKS (2018) Impact of contracted endodontic cavities on fracture resistance of endodontically treated teeth: a systematic review of in vitro studies. Clinical Oral Investi- gations 22, 109–18.
- Tang W, Wu Y, Smales RJ (2010) Identifying and reducing risks for potential fractures in endodontically treated teeth. Journal of Endodontics 36, 609–17.
- Tzimpoulas NE, Alisafis MG, Tzanetakis GN, Kontakiotis EG. (2012) A prospective study of the extraction and retention incidence of endodontically treated teeth with uncertain prognosis after endodontic referral. Journal of Endodontics 38, 1326–9.
- Vertucci FJ (1984) Root canal anatomy of the human permanent teeth. Oral Surgery Oral Medicine Oral Pathology 58, 589–99.
- Vieira GCS, Pérez AR, Alves FRF et al. (2020) Impact of contracted endodontic cavities on root canal disinfection and shaping. Journal of Endodontics 46, 655–61.
- Wang Q, Liu Y, Wang Z et al. (2020) Effect of access cavities and canal enlargement on biomechanics of endodontically treated teeth: a finite element analysis. Journal of Endodontics 46, 1501–7.
- Zhang Y, Liu Y, She Y, Liang Y, Xu F, Fang C (2019) The effect of endodontic access cavities on fracture resistance of first maxillary molar using the extended finite element method. Journal of Endodontics 45, 316–21.
