Methodological proposal for evaluation of adhesion of root canal sealers to gutta-percha
Abstract
Aim: To compare the bond strength of an epoxy resin-based sealer and two calcium silicate-based sealers (CSS) to gutta-percha discs using a new method.
Methodology: Round discs of gutta-percha (n = 60), measuring 10 mm in diameter and 2 mm in thickness, were placed on a glass plate and a drop of each sealer (AH Plus, EndoSequence BC Sealer and EndoSeal MTA) was placed on their surface. Another identical disc was placed onto the first one and a standardized weight (0.0981 N) applied over them using a specially developed apparatus. Ten samples prepared for each sealer were submitted to a microshear bond strength test accomplished by a specially designed set-up coupled to a universal testing machine. The Kruskal–Wallis test followed by a post hoc procedure was used to compare groups considering the preliminary analysis of the raw data had indicated the nonadherence to a Gaussian distribution (Shapiro–Wilk, p < .05). Alpha error was set at 5%.
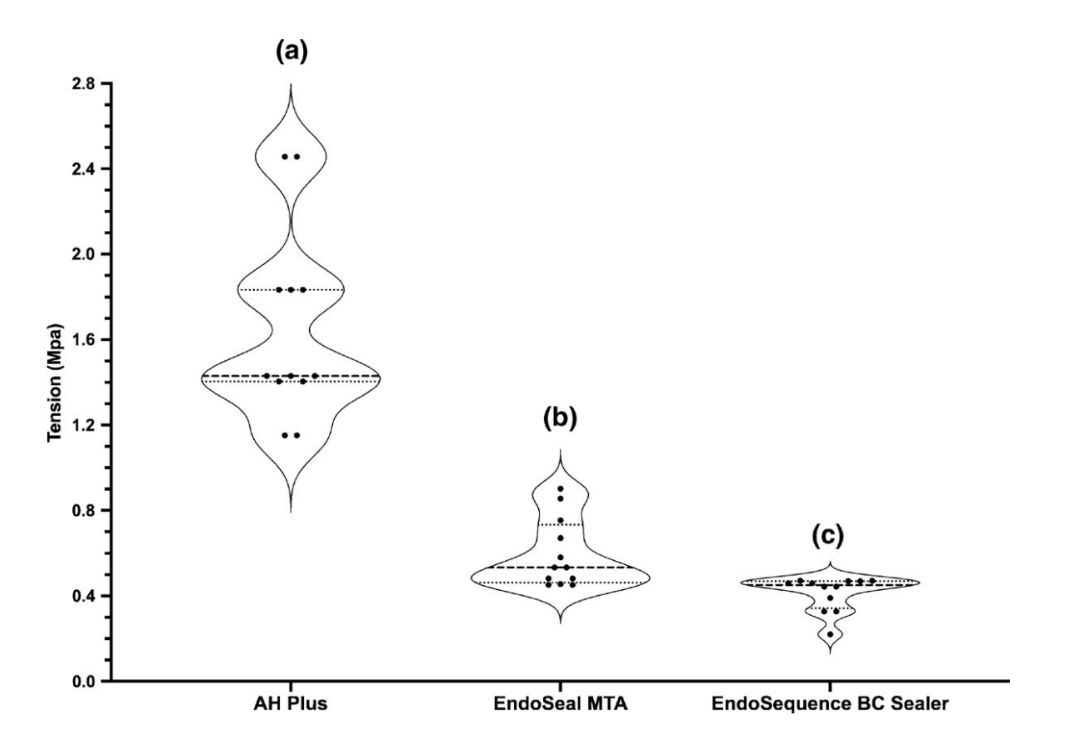
Results: Overall, no premature failure occurred. All sealers had some degree of adhesiveness to gutta-percha discs but with a significant difference amongst them (Kruskal– Wallis, p = .019). The epoxy resin-based sealer (AH Plus) had significantly higher median shear bond strength values (1.43 MPa; 1.40–1.83) compared to EndoSeal MTA (0.53 MPa; 0.46–0.73) (p = .021) and EndoSequence BC Sealer (0.45 MPa; 0.34–0.46) (p = .023), whilst the lowest median value was observed with EndoSequence BC Sealer (0.45 MPa; 0.34–0.46) (p < .05).
Conclusions: CSS sealers had weaker bonding to gutta-percha when compared to the epoxy resin-based AH Plus sealer. The proposed methodology is an innovative and reproducible method for testing the bond strength of root canal sealers to gutta-percha.
Introduction
The development of the first ready-to-use calcium silicate-based sealer in 2007 (iRoot SP; Innovative BioCeramix Inc.) attracted the attention of the endodontic community, and since then, several other calcium silicate-based sealers (CSS) have been launched. Preliminary positive perception on its use was based on the manufacturers’ claim that CSS were a successful version of MTA with handling and viscosity features optimized to fill the root canal space, considering their hydrophilic nature, bioactivity and good balance between physicochemical and biological properties (Almeida et al., 2020; Candeiro et al., 2012; Giacomino et al., 2019; Lv et al., 2017; Silva et al., 2016, 2017). In addition, most CSS are ready-to-use injectable pastes, which streamlines the filling procedures for dentists of all levels of skill and experience. As a consequence, CSS have gained large approval amongst clinicians over the last decade.
Originally, CSS were developed to fill the entire canal space without a solid core material, following the monoblock concept, an idea developed with methacrylate-based sealers (Tay & Pashley, 2007), which claims that the root canal space should be ideally filled with a single material, creating a single interface with the dentinal walls that, theoretically, would provide a better long-term fluid-tight seal (Tay & Pashley, 2007). Nonetheless, the use of CSS alone is not recommended since it would not be possible to penetrate into its mass after the final setting, in case root canal retreatment is necessary. Thus, the solution was to simply cement one master gutta-percha cone into the root canal space, the so-called single-cone technique, acting as a nucleus for the surrounding CSS. Additionally, the use of a single master cone would help not only on the distribution of the sealer within the canal space, but also provide better control of the apical limit of the root canal filling.
Regardless of the endodontic sealer used, its ability to adhere to both dentinal walls and gutta-percha is desired to avoid gaps at sealer/dentine and sealer/gutta-percha interfaces. A gap on either of these links will become an opportunity for microorganisms to invade and colonize the filled root canal. Although several methods were developed by international organizations to assess physical and biological properties of endodontic filling materials (ANSI/ADA, 2000; ISO, 2012), there is still no standard requirement for testing adhesion (Goracci et al., 2004). In a laboratory set-up, this property has been mostly evaluated by push-out bond strength resistance tests and contradictory findings have been reported because of the heterogeneity of the experimental protocols (Silva et al., 2019). For instance, whilst some studies reported higher bond strength for iRoot SP compared to epoxy resin-based sealers (Gokturk et al., 2017; Madhuri et al., 2016; Nagas et al., 2012), others reported lower bonding (Gade et al., 2015), or even no difference (Sagsen et al., 2011) between them. Nonetheless, the bond strength of CSS has been tested only to the dentinal walls, whilst there is still a lack of knowledge regarding their adhesion ability to core- filling materials, which is also important in terms of sealing ability and filling stability. In fact, this topic has been rarely explored in the literature (Hiraishi et al., 2005, 2006; Tagger et al., 2003a, 2003b; Teixeira et al., 2009), even though it has the same level of importance as adhesion to dentine. Indeed, this may help to explain the lack of proper and specifically designed laboratory methods to assess the bonding ability of a given sealer to gutta-percha core material.
Considering the lack of information on the adhesion of CSS to gutta-percha, the aim of this study was to propose a new method to quantify bond strength resistance to gutta-percha and to compare the bond strength of two CSS (EndoSequence BC Sealer; Brasseler; and EndoSeal MTA; Maruchi) to gutta-percha. An epoxy resin-based sealer (AH Plus; Dentsply De Trey) was used for comparison. The null hypothesis tested was that there would be no significant difference on the bond strength resistance of the sealers to gutta-percha.
Materials and methods
Sample size calculation
Based on the results of a pilot study, an effect size of 0.78 was estimated for the selection method. This value was input into a F family method (ANOVA: fixed effects, omnibus, one-way) at G × Power for Mac 3.1 (Heinrich Heine, Universität Düsseldorf, Düsseldorf, Germany), together with parameters alpha-type error of 5% and beta power of 95%. The software indicated a number of 10 samples per group to observe a significant effect.
Sample preparation
Sixty round discs of gutta-percha, measuring 10 mm of diameter and 2 mm of thickness, were produced from 1-mm-thick gutta-percha sheets using a proprietary technology (Dentsply Sirona Endodontics). The production of these gutta-percha discs embraced first the creation of gutta-percha sheets by plasticization in a laboratory dry-heating oven at 80°C, followed by a cooling process at ambient temperature, to obtain gutta-percha discs with 10 mm (∅) extracted from these sheets using an automatic metal punch. A standardized metallographic procedure was employed with coarse silicon carbide abrasive papers (180 to 600 grit) to produce gutta-percha discs with similar surface roughness in both faces. Subsequently, microhardness (MicroMet 5100 durometer; Buehler Ltd.), surface roughness and flatness (2D data) were evaluated in one of these discs with a bench-top optical profilometer (ZeGage Pro; Zygo Corporation) to assure the standardization of the discs.
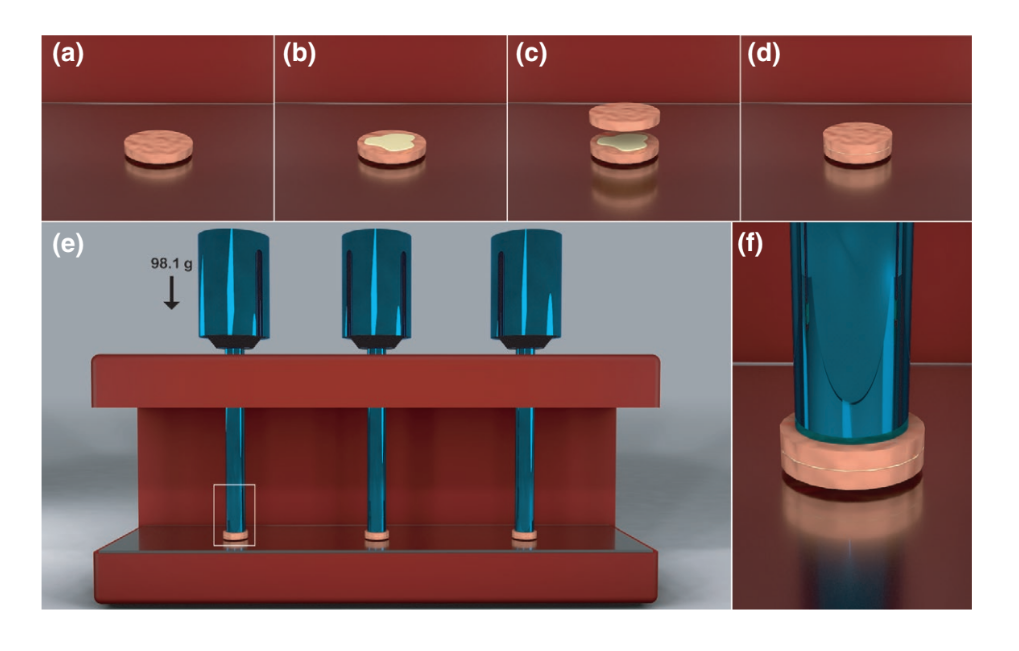
The discs were randomly distributed into 3 groups (n = 20) according to the sealers used: AH Plus, EndoSequence BC Sealer and EndoSeal MTA. Using a 0.5-ml automatic micropipette (Sigma-Aldrich Inc.), a 0.1 mL drop of each sealer, prepared according to the manufacturers’ specifications, was delivered onto the centre of a gutta-percha disc placed on a glass plate (Figure 1a,b). Then, another identical disc was aligned (Figure 1c) and placed over the first one (Figure 1d), and a weight (0.0981 N) applied over the discs for 200 s using a specially developed apparatus (Figure 1e,f) aiming to standardize the layer distribution and the thickness of the sealer. After removal of the material extruded onto the external surface of the discs using a dental microbrush applicator tip, the samples were stored at 37°C in contact with gauze moistened in phosphate-buffered saline solution (pH 7.2) for 7 days. After setting, the experimental samples were measured with a digital calliper to ensure a thickness of 4.1 ± 0.05 mm. Nonstandard samples were replaced. Ten samples per group were prepared and submitted to microshear bond test.
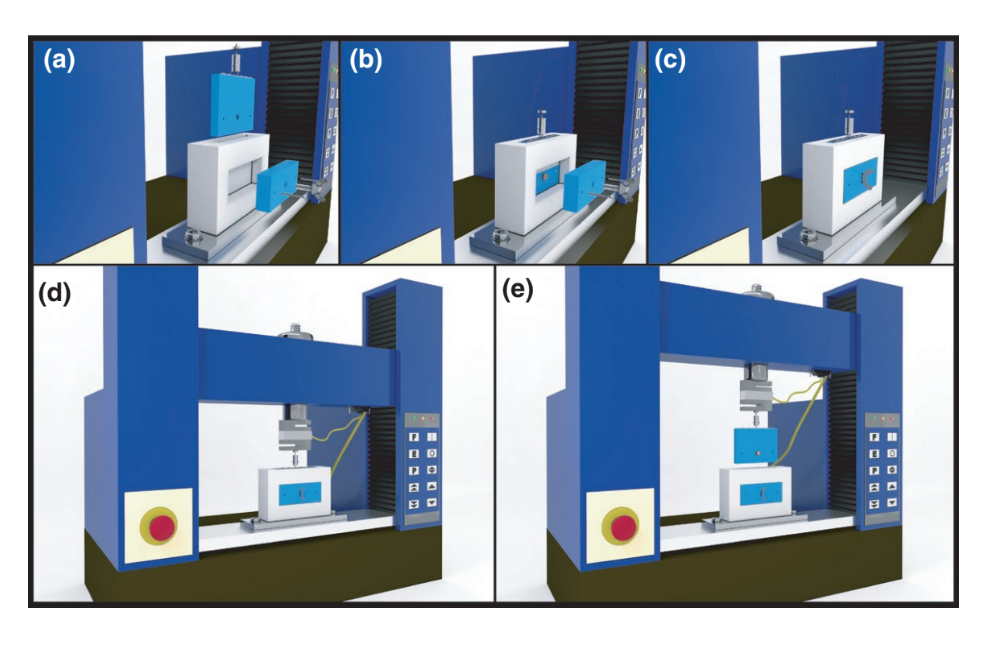
Microshear bond testing
The shear bond strength between gutta-percha discs and sealer was tested using a specially designed set-up coupled to a universal testing machine (Instron 4444; Instron Corporation) (Figure 2a). Each sample was then trapped in a container measuring 4.1 mm in thickness and 10.1 mm in diameter, composed of a static and a removable part (Figure 2b). After ensuring stabilization of the sample (Figure 2c), the moving part of the container was attached to the Instron machine (Figure 2d) and displaced vertically (longitudinally to the sealer film) (Figure 2e) with a constant speed of 0.5 mm/min to produce a shearing force that resulted in debonding of the disc–sealer interface. The microshear bond test was performed in a random order (i.e. load was applied randomly over the samples) by a blinded operator to the specific sealer under test. Bond strength was determined by using a real-time computer software program that plotted a load/time curve during the test. Bond failure load was registered when a sharp decline was observed on the graph and/or by the complete dislodgement of the material. The shear force required to separate the gutta-percha discs was recorded in Newtons (N) for each sample and then divided by their contact surface area, calculated as the area of a circle by the formula A = π.r², where π is the constant 3.14 and r is the radius of the disc. Shear bond strength results were expressed in Mega Pascals (MPa).
Statistical analysis
Preliminary analysis of the raw data indicated the nonadherence to a Gaussian distribution (Shapiro–Wilk, p = .036), and data were expressed as median and interquartile range. A Kruskal–Wallis test followed by a post hoc statistical procedure performed comparisons amongst the sealers using a standard alpha error set at 5% (SPSS v.24; SPSS Inc.).
Results
Overall, no premature failure occurred, which means that all sealers had adhesive properties to the gutta-percha discs, with no pre-test failure. Violin plots (Figure 3) show the median and interquartile range, as well as the distribution of the bond strength resistance data in each experimental group. A significant difference on the bond strength was observed amongst sealers (Kruskal–Wallis, p = .019). The epoxy resin-based sealer (AH Plus) had a significantly higher median bond strength values (1.43 MPa; 1.40–1.83) than EndoSeal MTA (0.53 MPa; 0.46–0.73) (p = .021) and EndoSequence BC Sealer (0.45 MPa; 0.34–0.46) (p = .023). The lowest median value was observed with EndoSequence BC Sealer (p < .05).
Discussion
Adhesion is a combination of physical and chemical mechanisms that allow the attachment of one material to another (Erickson, 1992). In Endodontics, adhesion represents the ability of a sealer to bond to dentine and to the core filling material (Ørstavik et al., 1983). The adhesion property of dental materials has been studied since the development of the experimental model proposed by Grossman (1976). Later, it was improved by using a universal testing machine to measure the load required to cause bond failure (Ørstavik et al., 1983). Since then, the bond strength of filling materials to dentine has been measured through tensile tests on external root dentine or on the root canal wall surface with pull-out or push-out methods (Goracci et al., 2004). Additionally, the qualitative analysis of the debonded surface of the filling materials (cohesive failure) or dentinal surface (adhesive failure) improved the understanding on the influence of various factors in intracanal adhesion (Saleh et al., 2003). However, whilst sealers can bond to dentine by their mechanical interlocking into the dentinal tubules and/or by chemical adhesion, the core material (gutta-percha) lacks adhesion to either dentine or sealer (Tay & Pashley, 2007).
Previous investigations have focused mostly on the adhesion quality of sealers to dentine, whilst only a few studies assessed the bond strength between gutta-percha and sealer (Hiraishi et al., 2005, 2006; Tagger et al., 2003a, 2003b; Teixeira et al., 2009), which is also essential to fulfil one of the basic requirements of root canal filling, that is to seal the root canal space (Grossman, 1976). In most of these studies, gutta-percha and/ or Resilon discs were in contact with a small amount of a sealer placed into a tube, whilst a wire loop was wrapped around the bonded assembly and a shearing force was applied (Hiraishi et al., 2005, 2006; Teixeira et al., 2009). In the present proposal, however, a large contact area between sealer and guttapercha discs was obtained, as well as the standardization of the sealer film thickness using a specific apparatus (Figure 1), thus avoiding premature failures. Moreover, other specific set-ups (Figure 2) allowed the shear-loading device to align closer to the adhesive interface. In this way, the internal validity of this experiment was improved by eliminating the bending moment created by the previous method, which could skew the real shear bond strength of materials.
The present results demonstrated that the adhesion of the epoxy resin-based sealer to gutta-percha outperformed the CSS, and therefore, the null hypothesis was rejected. Previous studies have already demonstrated some bond strength of epoxy resin-based sealers to gutta-percha (Tagger et al., 2003a, 2003b; Teixeira et al., 2009), but the present results confirmed that AH Plus had a superior bond to gutta-percha than CSS, which could be explained by two factors: (i) the possibility that CSS do not set under laboratory conditions (Silva et al., 2021) and (ii) the hydrophobic nature of gutta-percha (Hegde & Arora, 2015; Hegde & Murkey, 2017), which would decrease its interaction with CSS considering their hydrophilic nature. One may argue that the present results were a consequence of the improper use of CSS with gutta-percha instead of bioceramic pre-coated gutta-percha cones. However, so far, no manufacturer has disclosed that CSS should not be used with regular gutta-percha points. Actually, it has been reported that only 22.1% of CSS users have employed pre-coated gutta-percha in their root canal fillings (Guivarc'h et al., 2020), which endorses the purpose of this study. Moreover, EndoSeal MTA had greater adhesion to gutta-percha than EndoSequence BC Sealer and this may be a consequence of the different com- position of CSS. EndoSeal MTA is a pozzolan-based sealer. Pozzolans are a broad class of siliceous or siliceous and aluminous materials that, in themselves, possess little or no cementitious value but which will, in finely divided form and in the presence of water, react chemically with calcium hydroxide at ordinary temperature to form compounds possessing cementitious properties. The quantification of the capacity of a pozzolan to react with calcium hydroxide and water is given by measuring its pozzolanic activity. Pozzolana are naturally occurring pozzolans of volcanic origin (Singh, 2018). Overall, the pozzolanic reaction with calcium hydroxide and water optimizes the flow of a pre-mixed substrate assuring adequate working consistency and setting ability (Yoo et al., 2016). The incorporation of small particle pozzolan cement, which is a mineral aggregate with watery calcium silicate hydration, resulted in a fast-setting MTA without the addition of a chemical accelerator (Choi et al., 2013).
It is important to emphasize that commercially available gutta-percha may vary in its composition and physicochemical properties depending on the manufacturer. Therefore, it is likely that the results of shear bond strengths differ when different brands of gutta-percha are compared and this is a clear limitation of the current study. Moreover, specific coated gutta-percha cones have been recommended to be used with some CSS brands and their adhesion as well as their interfacial adaptation should be also evaluated in future studies. Unfortunately, the present methodology does not allow to be measured the bonding resistance of root canal sealers onto individual gutta-percha master cones and, therefore, does not intend to mimic the real-life clinical conditions. On the other hand, the present study presents an innovative and reproducible way for testing bonding between conventional or modified gutta-percha to various types of root canal sealers.
Conclusions
CSS had a weak bond to gutta-percha. The epoxy resin-based root canal sealer (AH Plus) had greater bonding values compared to the CSS, whilst EndoSeal MTA had greater adhesion to gutta-percha than EndoSequence BC Sealer. The present study introduces an innovative and reproducible method for testing the bond strength between conventional or modified gutta-percha to different types of root canal sealers.
Authors: Gustavo De-Deus, Diogo S. Oliveira, Daniele M. Cavalcante, Marco Simões-Carvalho, Felipe G. Belladonna, Leandro S. Antunes, Erick M. Souza, Emmanuel J. N. L. Silva, Marco A. Versiani
References:
- Almeida, M.M., Rodrigues, C.T., Mattos, A.A., Carvalho, K.-K.-T., Silva, E.-J.-N.-L., Duarte, M.-A.-H. et al. (2020) Analysis of the physiochemical propeties, cytotoxicity and volumetric changes of AH Plus, MTA Fillapex and TotalFill BC sealer. Journal of Clinical and Experimental Dentistry, 12, e1058–e1065.
- ANSI/ADA. (2000) Specification n° 57 endodontic sealing material. Chicago, IL: ANSI/ADA.
- Candeiro, G.T., Correira, F.C., Duarte, M.A., Ribeiro-Siqueira, D.C. & Gavini, G. (2012) Evaluation of radiopacity, pH, release of calcium ions, and flow of a bioceramic root canal sealer. Journal of Endodontics, 38, 842–845.
Choi, Y., Park, S.J., Lee, S.H., Hwang, Y.C., Yu, M.K. & Min, K.S. (2013) Biological effects and washout resistance of a newly developed fast-setting pozzolan cement. Journal of Endodontics, 39, 467–472.
Erickson, R.L. (1992) Surface interactions of dentin adhesive materials. Operative Dentistry, 5, 81–94.
Gade, V.J., Belsare, L.D., Patil, S., Bhede, R. & Gade, J.R. (2015) Evaluation of push-out bond strength of Endosequence BC sealer with lateral condensation and thermoplasticized technique: an in vitro study. Journal of Conservative Dentistry, 18, 124–127.
Giacomino, C.M., Wealleans, J.A., Kuhn, N. & Diogenes, A. (2019) Comparative biocompatibility and osteogenic potential of two bioceramic sealers. Journal of Endodontics, 45, 51–56.
Gokturk, H., Bayram, E., Bayram, H.M., Aslan, T. & Ustun, Y. (2017) Effect of double antibiotic and calcium hydroxide pastes on dislodgement resistance of an epoxy resin-based and two calcium silicate-based root canal sealers. Clinical Oral Investigations, 21, 1277–1282.
Goracci, C., Tavares, A.U., Fabianelli, A., Monticelli, F., Raffaelli, O., Cardoso, P.C. et al. (2004) The adhesion between fiber posts and root canal walls: comparison between microtensile and push-out bond strength measurements. European Journal of Oral Sciences, 112, 353–361.
Grossman, L.I. (1976) Physical properties of root canal cements. Journal of Endodontics, 2, 166–175.
Guivarc’h, M., Jeanneau, C., Giraud, T., Pommel, L., About, I., Azim, A.A. et al. (2020) An international survey on the use of calcium silicate-based sealers in non-surgical endodontic treatment. Clinical Oral Investigations, 24, 417–424.
- Hegde, V. & Arora, S. (2015) Fracture resistance of roots obturated with novel hydrophilic obturation systems. Journal of Conservative Dentistry, 18, 261–264.
- Hegde, V. & Murkey, L.S. (2017) Microgap evaluation of novel hydrophilic and hydrophobic obturating systems: a scanning electron microscope study. Journal of Clinical and Diagnostic Research, 11, 75–78.
- Hiraishi, N., Loushine, R.J., Vano, M., Chieffi, N., Weller, R.N., Ferrari, M. et al. (2006) Is an oxygen inhibited layer required for bonding of resin-coated gutta-percha to a methacrylate-based root canal sealer? Journal of Endodontics, 32, 429–433.
- Hiraishi, N., Papacchini, F., Loushine, R.J., Weller, R.N., Ferrari, M., Pashley, D.H. et al. (2005) Shear bond strength of Resilon to a methacrylate-based root canal sealer. International Endodontic Journal, 38, 753–763.
- ISO. (2012) International Standard ISO 6876:2012. Geneva: ISO.
- Lv, F., Zhu, L., Zhang, J., Yu, J., Cheng, X. & Peng, B. (2017) Evaluation of the in vitro biocompatibility of a new fast-setting ready-to-use root filling and repair material. International Endodontic Journal, 50, 540–548.
- Madhuri, G.V., Varri, S., Bolla, N., Mandava, P., Akkala, L.S. & Shaik, J. (2016) Comparison of bond strength of different endodontic sealers to root dentin: an in vitro push-out test. Journal of Conservative Dentistry, 19, 461–464.
- Nagas, E., Uyanik, M.O., Eymirli, A., Cehreli, Z.C., Vallittu, P.K., Lassila, L.V.J. et al. (2012) Dentin moisture conditions affect the adhesion of root canal sealers. Journal of Endodontics, 38, 240–244.
- Ørstavik, D., Eriksen, H.M. & Beyer-Olsen, E.M. (1983) Adhesive properties and leakage of root canal sealers in vitro. International Endodontic Journal, 16, 59–63.
- Sagsen, B., Ustün, Y., Demirbuga, S. & Pala, K. (2011) Push-out bond strength of two new calcium silicate-based endodontic sealers to root canal dentine. International Endodontic Journal, 44, 1088–1091.
- Saleh, I.M., Ruyter, I.E., Haapasalo, M.P. & Ørstavik, D. (2003) Adhesion of endodontic sealers: scanning electron microscopy and energy dispersive spectroscopy. Journal of Endodontics, 29, 595–601.
- Silva, E.J.N.L., Canabarro, A., Andrade, M.R.T.C., Cavalcante, D.M., Von Stetten, O., Fidalgo, T.K.D.S. et al. (2019) Dislodgment resistance of bioceramic and epoxy sealers: a systematic review and meta-analysis. The Journal of Evidence-Based Dental Practice, 19, 221–235.
- Silva, E.J.N.L., Carvalho, N.K., Prado, M.C., Zanon, M., Senna, P.M., Souza, E.M. et al. (2016) Push-out bond strength of injectable pozzolan-based root canal sealer. Journal of Endodontics, 42, 1656–1659.
- Silva, E.J.N.L., Ehrhardt, I.C., Sampaio, G.C., Cardoso, M.L., Oliveira, D.D.S., Uzeda, M.J. et al. (2021) Determining the setting of root canal sealers using an in vivo animal experimental model. Clinical Oral Investigations, 25, 1899–1906.
- Silva, E.J., Zaia, A.A. & Peters, A.O. (2017) Cytocompatibility of calcium silicate-based sealers in a three-dimensional cell culture model. Clinical Oral Investigations, 21, 1531–1536.
- Singh, M. (2018) Coal bottom ash. In: Siddique, R. & Cachim, P. (Eds.) Waste and supplementary cementitious materials in concrete. Characterisation, properties and applications, 1st edition. Duxford: Woodhead Publishing, pp. 3–50.
- Tagger, M., Greenberg, B. & Sela, G. (2003a) Interaction between sealers and gutta-percha cones. Journal of Endodontics, 29, 835–837. Tagger, M., Tagger, E., Tjan, A.H. & Bakland, L.K. (2003b) Shearing bond strength of endodontic sealers to gutta-percha. Journal of Endodontics, 29, 191–193.
- Tay, F.R. & Pashley, D.H. (2007) Monoblocks in root canals: a hypothetical or a tangible goal. Journal of Endodontics, 33, 391–398.
- Teixeira, C.S., Alfredo, E., Thomé, L.H.C., Gariba-Silva, R., Silva- Sousa, Y.T.C. & Sousa-Neto, M.D. (2009) Adhesion of an endodontic sealer to dentin and gutta-percha: shear and push-out bond strength measurements and SEM analysis. Journal of Applied Oral Science, 17, 129–135.
- Yoo, Y.-J., Baek, S.-H., Kum, K.-Y., Shon, W.-J., Woo, K.-M. & Lee, W.C. (2016) Dynamic intratubular biomineralization following root canal obturation with pozzolan-based mineral trioxide aggregate sealer cement. Scanning, 38, 50–56.
