The Impact of TruNatomy and ProTaper Gold Instruments on the Preservation of the Periradicular Dentin and on the Enlargement of the Apical Canal of Mandibular Molars
Abstract
Introduction: This study aimed to evaluate the preservation of periradicular dentin and the enlargement of the apical canal of mandibular molars with TruNatomy (Dentsply Sirona, Ballaigues, Switzerland) and ProTaper Gold (Dentsply Sirona) instruments.
Methods: Twenty mandibular molars were scanned in a micro–computed tomographic device, anatomically paired, and distributed into 2 groups (n = 10). In the ProTaper Gold group, mesial and distal canals were prepared up to F2 (25/.08v) and F3 (30/.09v) instruments, whereas in the TruNatomy group, mesial and distal canals were enlarged up to the prime (26/.04v) and medium (36/.03v) instruments, respectively. After a new scan, the surface area, volume, unprepared areas, transportation, percentage of dentin removal, and dentin thickness parameters were calculated. Data were compared between groups using the Mann-Whitney test, the Student t test, and the nonmetric multidimensional scaling test with alpha set at 5%.
Results: No difference was found between groups regarding unprepared canal areas and the reduction of dentin thickness (P ˃ .05). Transportation was lower than 0.1 mm in all groups, and statistical differences were observed only at the apical third of the mesiobuccal canal with lower values in the TruNatomy group. ProTaper Gold removed more dentin than TruNatomy at the coronal level of mesial roots (1.8% and 1.0%, respectively) (P ˂ .05).
Conclusions: TruNatomy and ProTaper Gold were efficient for performing canal preparation in mandibular molars. The tested systems were similar in terms of untouched canal walls and remaining dentin thickness and slightly different in the apical transportation of mesial canals and the percentage of dentin removal at the coronal third but without clinically significant errors. (J Endod 2022;■:1–9.)
Since the inception of the mechanical enlargement of root canals using nickel-titanium (NiTi) instruments back in the 1990s, preparation techniques have been focused on creating tapered shapes to allow adequate cleaning, disinfection, and filling procedures. In 2009, Clark and Khademi suggested a new model of access opening and coronal preparation aiming to reduce the incidence of vertical root fractures in endodontically treated teeth. Their proposal was based on the preservation of the pulp chamber roof and the pericervical dentin, an area located 4 mm above and 4 mm below the crestal bone. Later, studies using finite element analysis confirmed that this area has an important function in transferring occlusal forces through the root, potentially reducing the stress in the coronal area and, consequently, helping in the maintenance of the resistance strength of teeth. Throughout the years, this seminal idea of dentin conservation evolved to include other aspects of the root canal treatment. This is currently known as minimally invasive endodontics, a concept that includes the preservation of sound tooth structure not only related to the access cavity opening but also to root canal preparation. However, if on one hand the preservation of sound dentin tissue is desirable, on the other hand, conservative canal preparation may compromise the removal of pulp tissue remnants and pathogenic microorganisms from within the root canal space.
The minimally invasive concept applied to root canal preparation aims to preserve more dentin at the pericervical region and includes the use of low tapered instruments for shaping. In the last years, several companies have developed new NiTi systems with small dimensions (tip and taper) to fulfill this goal. For instance, the TruNatomy rotary system (Dentsply Sirona, Ballaigues, Switzerland) is a set of instruments made of a maximum fluted diameter of 0.8-mm NiTi wire with a proprietary heat treatment. Instruments present a variable taper and an off-centered parallelogram cross-sectional design to preserve the radicular dentin during mechanical preparation. Previous studies on this system reported a high cyclic fatigue resistance and a great ability to maintain the original canal anatomy. Although the TruNatomy system was developed to preserve more dentin during canal preparation, little is known regarding this specific feature.
Therefore, this study aimed to evaluate canal transportation, dentin thickness, and the percentage of removed dentin and unprepared canal areas at the coronal and apical thirds of mesial and distal canals of mandibular molars prepared with TruNatomy and ProTaper Gold (Dentsply Sirona) systems. The null hypotheses tested were that there would be no differences between the tested systems on the investigated parameters.
Materials and methods
Sample Size Calculation
Sample size calculation was based on data from a previous study. Power calculation was performed using G*Power 3.1 software for Windows (Henrick Heine-Universität, Düsseldorf, Germany) with α = 0.05, power of 95%, and an effect size of 1.64 input into the t test family. A total of 18 samples (9 per group) were indicated as the ideal number of specimens required to observe significant differences between groups. Ten samples were used per group to compensate for possible sample loss during experimental procedures.
Specimen Selection and Groups This study was approved by the local ethics committee (protocol 4.667.320). Twenty mandibular molars with a single distal canal and moderately curved type II and IV mesial canals (˂20˚) and isthmus types II and V were selected from a pool of teeth extracted for reasons not related to this study. The specimens were scanned in a micro– computed tomographic device (SkyScan 1173; Bruker-microCT, Kontich, Belgium) at 70 kV, 114 mA, 20 mm (pixel size), 360˚ rotation around the vertical axis, and a 0.5 rotation step using a 0.5-mm-thick aluminum filter. Images were reconstructed (NRecon v.1.6.1.0, Bruker-microCT) using beam hardening correction of 20%, ring artifact correction of 1, and smoothing of 2, resulting in the acquisition of 600–700 axial cross sections per sample. The acquired data sets were evaluated regarding canal configuration (CTVol v.3.3.1, Bruker-microCT) and 3-dimensional morphometric parameters (volume and surface area) of the mesiobuccal (MB), mesiolingual (ML), and distal canals (CTAn v.1.6.6.0, Bruker-microCT). The selected teeth were kept stored in distilled water until the experimental procedures when they were anatomically matched and distributed into 2 experimental groups (n = 10) according to the rotary preparation protocol: TruNatomy and ProTaper Gold.
Root Canal Preparation
After conventional access cavity preparation, root canals were accessed, and apical patency was confirmed with a size 10 K-file (Dentsply Sirona). When the tip of the instrument was visible through the main foramen, 1.0 mm was subtracted to determine the working length (WL). No coronal flaring was performed, and a glide path was achieved to the WL with a size 15 K-file (Dentsply Sirona). Before shaping procedures, each root was covered with a layer of a light-cured resin (Whitegold Protector Blue, Dentsply Sirona) to simulate a closed system, and teeth were mounted on a dental mannequin in a mandibular jaw under rubber dam isolation to reproduce the clinical conditions. All procedures were performed using an operating microscope at X12.5 magnification (OPMI pico; ZEISS, Jena, Germany), and preparation protocols were performed as follows:
- TruNatomy system: after the enlargement of the coronal third with the orifice modifier instrument (size 20, .08v taper), patency was confirmed with size 10 and 15 K-files. In all canals, the glider (size 17, .02v taper) and the prime (size 26, .04v taper) instruments were taken up to the WL. Distal canals were further enlarged with the medium instrument (size 36, .03v taper). All instruments were used at 500 rpm and 1.5 Ncm.
- ProTaper Gold system: S1 (size 18, .02v taper) and S2 (size 20, .04v taper) instruments were used to enlarge the coronal and middle thirds of the canals. In all canals, after apical patency using size 10 and 15 K-files, S1, S2, F1 (size 20, .07v taper), and F2 (size 25, .08v taper) instruments were used up to the WL. Distal canals were further enlarged with the F3 instrument (size 30, .09v taper). All instruments were used at 300 rpm with torque set at 5.2 Ncm (S1), 1.5N cm (S2), and 3.1 Ncm (F1, F2, and F3).
Instruments were activated using the X- Smart Plus motor (Dentsply Sirona) set with torque and rotation speed as recommended by the manufacturers with 3 in-and-out movements and an amplitude of 3–5 mm. Each instrument was used on a single tooth and discarded. An operator with more than 10 years of experience using rotary systems performed all preparation protocols. Root canal irrigation was performed using a 30-G NaviTip double-side port needle (Ultradent Inc, South Jordan, UT) taken up to 2 mm short of the WL. Each canal was irrigated with 2 mL 2.5% sodium hypochlorite (NaOCl) after access preparation and glide path procedures, respectively; 2 mL 2.5% NaOCl after each instrument; and 1 mL 2.5% NaOCl after recapitulation with a patency file. Final irrigation was performed with 3 mL 2.5% NaOCl followed by 3 mL 17% EDTA (1 minute) and 3 mL 2.5% NaOCl (1 minute). After slightly drying the root canals with ProTaper Gold and TruNatomy paper points (Dentsply Sirona), samples were imaged again using the same parameters of the initial scan.
Micro–computed Tomographic Analysis
After the coregistration of pre- and postoperative data sets (3D Slicer v.4.4.0; available at www.slicer.org), the coronal (from the furcation level up to 4 mm in the apical direction) and apical (from the main foramen up to 3 mm in the coronal direction) areas of the mesial and distal root canals were analyzed regarding untouched canal walls, volume of dentin removal, transportation, and dentin thickness using ImageJ v.1.50 d (National Institutes of Health, Bethesda, MD) and CTAn v.1.6.6.0 software.
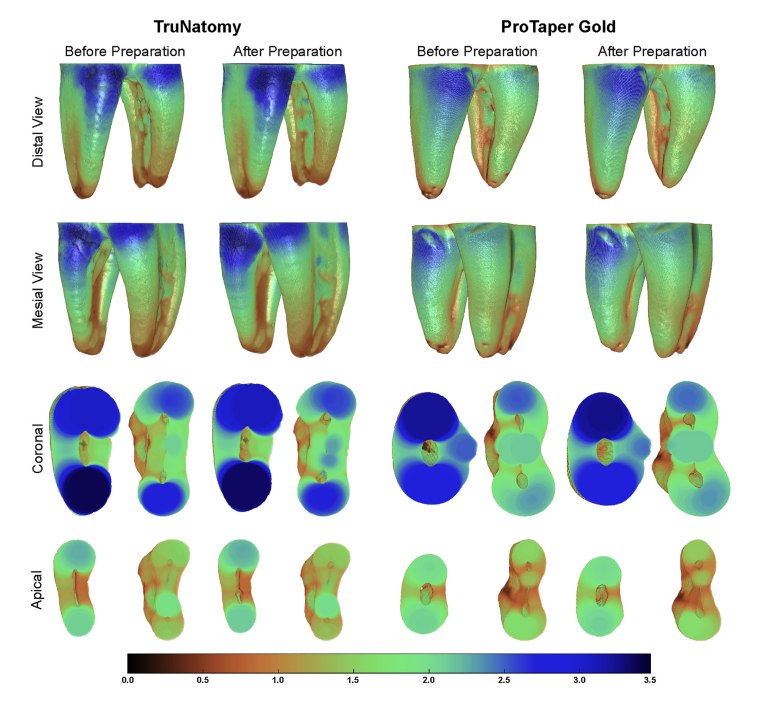
The percentage of unprepared areas (untouched canal walls) was calculated by the number of static voxels (voxels present at the same position on the canal surface before and after preparation) divided by the total number of voxels present on the root canal surface according to the following formula: (number of static voxels*100)/number of surface voxels. The percentage volume of dentin removal was calculated within the volume of interest (coronal and apical areas) as follows: (DVB - DVA)/(DVB X 100), where DVB and DVA is the dentin volume (in mm3) before and after preparation, respectively. Canal transportation was assessed by calculating the center of gravity of the root canal in each slice and connecting them along the z-axis with a fitted line using XLSTAT-3DPlot for Windows (Addinsoft, New York, NY). Then, mean transportation (in mm) was calculated in each canal by comparing the centers of gravity before and after preparation at the coronal (n = 200 slices) and apical (n = 150 slices) areas. For the analysis of dentin thickness, 3-dimensional mapping was created and saved for structure thickness (CTAn v.1.6.6.0). Then, color-coded cross sections of the roots were used to identify and measure the smallest dentin thickness (in mm) and the percentage thickness reduction of dentin at 1.0-mm intervals of the coronal and apical areas of each canal in both mesial and distal aspects of the roots. Qualitative comparisons of dentin thickness before and after preparation procedures were also performed using 3-dimensional color-coded models of the matched roots (CTVox v.3.3.1, Bruker-microCT).
Statistical Analysis
At first, data were tested for normality (Shapiro-Wilk test) and homoscedasticity (Levene test). The analysis of variance test with permutations was used to confirm the degree of homogeneity (baseline) of the groups regarding volume and surface area of the MB, ML, and distal canals. Then, depending on data distribution, statistical comparisons between groups regarding the tested parameters were performed using the Mann- Whitney (non-parametric data) or Student t test (parametric data). A multivariate analysis using nonmetric multidimensional scaling was applied to explore the similarities among teeth regarding the percentage reduction of dentin thickness measured at the coronal and apical levels in both the distal and mesial aspects of the roots. The tests were performed with a significance level of 5% using BioStat v. 5.0.1 (AnalystSoft, Walnut, CA) and R 3.6.0 (The R Foundation, Vienna, Austria; available at https://www.R-project.org) software.
Results
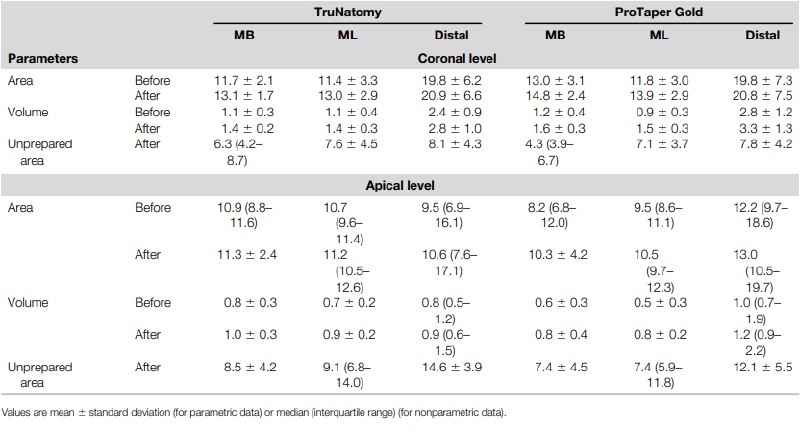
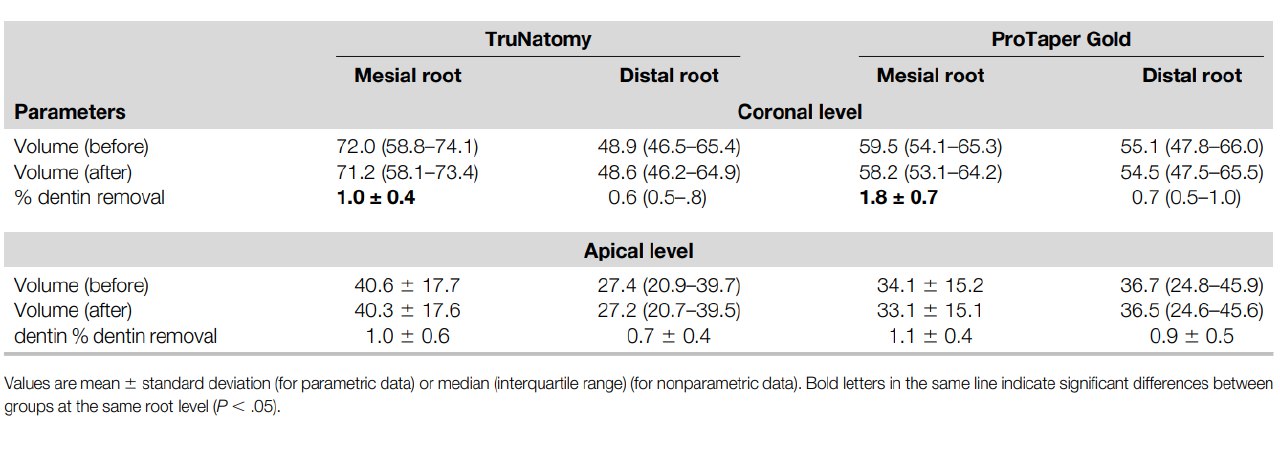
Results were depicted using the mean (standard deviation) or median (interquartile range) depending on data distribution. Table 1 exhibits the results of volume, surface area, and the unprepared area, whereas transportation and the percentage of dentin removed are displayed in Tables 2 and 3, respectively. The degree of homogeneity between groups regarding volume and surface area of root canals at baseline (before preparation) was confirmed (P ˃ .05), and no difference was observed in the percentage of untouched canal areas at the coronal or apical levels of all roots (P ˃ .05) (Table 1, Fig. 1).
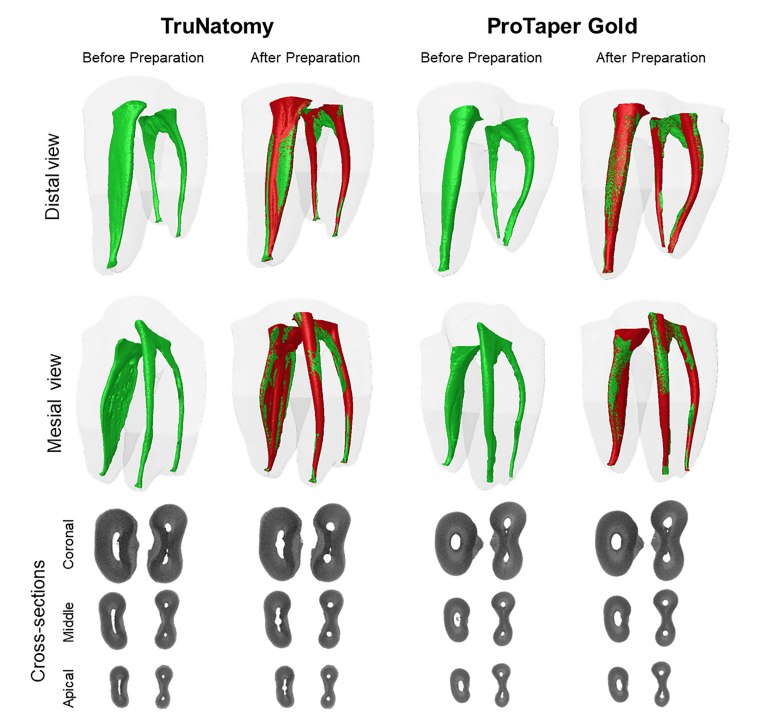
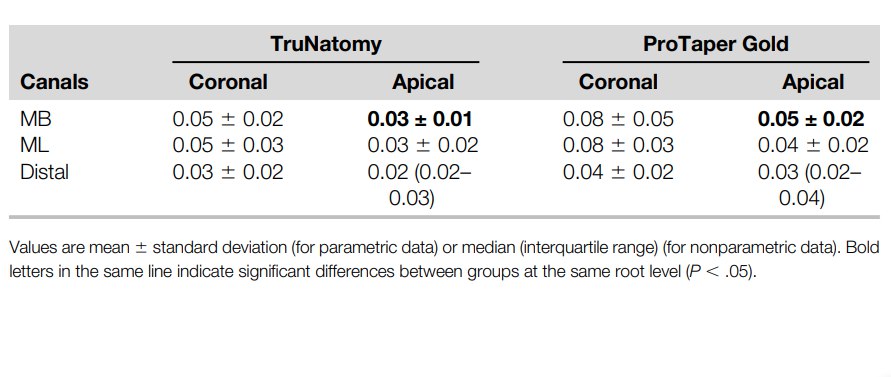
Transportation was lower than 0.1 mm in all groups and only at the apical level of the MB canal did preparation with TruNatomy instruments result in significantly less transportation (0.03 mm) than with ProTaper Gold (0.05 mm) (P ˂ .05) (Table 2, Fig. 2).
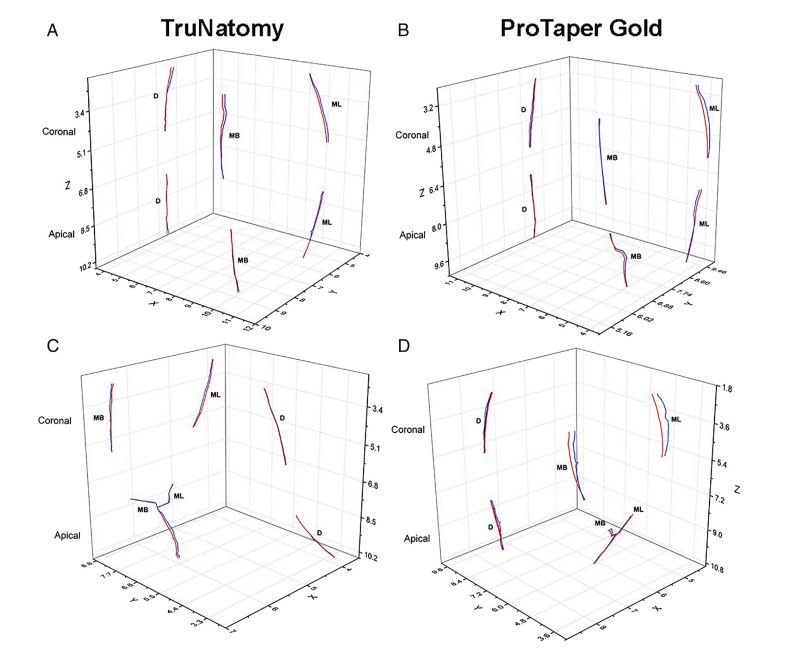
No difference was observed in the percentage of dentin removed at the apical level of both roots and at the coronal level of the distal root; however, a higher mean percentage removal of dentin was observed at the coronal level of mesial roots prepared with ProTaper Gold (1.8%) compared with TruNatomy (1%) instruments (P ˂ .05) (Table 3). No difference was found between the TruNatomy and ProTaper Gold groups regarding the percentage reduction of dentin thickness at the coronal and apical levels in both the distal and mesial aspects of all roots (P ˃ .05) (Fig. 3; Supplemental Fig. S1 is available online at www.jendodon.com).
Discussion
Clinical strategies and ideal shaping procedures are still being changed as new NiTi rotary instruments are constantly launched on the market. In the last years, protocols on root canal preparation have been directed toward the concept of minimally invasive endodontics in order to preserve dentin in both the coronal and radicular portions of teeth. Following this trend, manufacturers are developing instruments with small dimensions aiming to fulfill this goal. This study compared 1 of these new systems (ie, TruNatomy) with the well-studied ProTaper Gold regarding canal transportation, dentin thickness, dentin removal, and unprepared canal areas at the coronal and apical thirds of the mesial and distal canals of mandibular molars. The null hypothesis tested that there would be no difference in the performance of the 2 systems was confirmed for untouched canal walls and dentin thickness parameters but not for transportation and dentin removal.
In necrotic teeth, noninstrumented areas of the root canal system may potentially harbor remnants of bacterial biofilms which ultimately can affect the likelihood of treatment failure. Therefore, the main concern of minimal canal enlargement is its potential impact on the mechanical preparation of the root canal walls, mostly in infected cases. In the present study, the mean percentage of unprepared areas after canal preparation varied from 4.3%–14.6% (Table 1), which is in agreement with a previous study (6%–13%) that used similar methodology to evaluate the ProTaper Gold system. As stressed in other studies using micro–computed tomographic technology as an analytical tool, no shaping protocol was able to prepare the whole canal walls, an aspect that can be explained by the anatomic complexities of the mesial and distal canals of mandibular molars. Interestingly, despite differences in the geometry of the ProTaper Gold and TruNatomy instruments, no difference was observed between them in either the apical or coronal third regarding the percentage of untouched walls after preparation. In another study, TruNatomy also performed similarly to Reciproc Blue R25 (VDW, Munich, Germany), an instrument with similar dimensions (size 25, .08v taper) as the ProTaper Gold F216. This finding may be explained by the off-centered cross-sectional design of the TruNatomy system, which, unlike the conventional concentric design in the ProTaper Gold system, creates a snakelike motion that allows the instrument to touch more canal walls even though it has smaller dimensions. This snakelike motion has been associated with an increase in the space for the removal of pulp remnants and debris.
Apical transportation may compromise disinfection and the appropriate seal of the root canal system. In the literature, rotary NiTi instruments have been shown to properly maintain the original canal curvature, even in extremely curved canals. In the current study, the movement of the centers of gravity were metrically evaluated in absolute numbers (mm), slice by slice, as canal transportation. This method allows the precise evaluation of transportation of the whole volume of interest in 3 dimensions (Fig. 2), unlike some studies in which this parameter is measured using an outdated method based on a few 2-dimensional slices. Overall, it was observed that transportation was lower than 0.1 mm in both groups, a result that can be explained by the high flexibility of the tested instruments and the low degree of curvature of the selected roots. This finding is in agreement with studies demonstrating the ability of heat-treated instruments to prepare curved canals with low transportation values. However, the apical third of mesial canals prepared with TruNatomy showed lower mean transportation (0.03 mm) compared with the ProTaper Gold system (0.05 mm). Although this difference may be explained by dissimilarities in the tip size and NiTi alloy treatment of the tested systems, the values are so small that they can be considered irrelevant from a clinical perspective. In fact, transportations up to 0.15 mm are considered acceptable and only values higher than 0.3 mm have been deemed to negatively impact the prognosis of treatment.
The evaluation of dentin thickness is important because excessive removal of dentin could predispose teeth to root fracture. When instruments remain centered in the canal, it is expected that more dentin is maintained. Therefore, it is possible that because TruNatomy and ProTaper Gold systems performed quite similar in terms of canal preparation (volume and surface area) (Table 1), untouched canal walls (Table 1), and transportation (Table 2), no difference was also observed between them regarding the percentage reduction of dentin thickness in all evaluated levels (coronal and apical) and aspects (mesial and distal) of both roots (Fig. 3; Supplemental Fig. S1 is available online at www.jendodon.com). However, at the coronal level of the mesial roots, ProTaper Gold showed a higher mean percentage of removed dentin (1.8%) than TruNatomy (1%). Although this result can be easily explained due to differences in the taper of the master apical instruments used in this root (ProTaper Gold 25/.08v and TruNatomy 26/.04), these percentage volumes of removed dentin are so low that they can also be considered nonsignificant from a clinical standpoint. On the other hand, no difference was observed in the distal canal or at the apical level of both roots. These findings can be explained because the mesiodistal and buccolingual diameters of the coronal part of the distal canals are usually larger than the tested instruments. Moreover, at the apical level, the smaller tip size of the final instrument of the ProTaper Gold system (size 30, .09 taper) compared with the TruNatomy group (size 36, .03 taper) is compensated by its larger taper. The fact that the TruNatomy group promoted better dentin preservation at the coronal portion of the mesial roots but similar dentin thickness reduction compared with the ProTaper Gold group can be explained by the method of analysis. Although dentin removal was calculated in a 3-dimensional way (dentin volume), dentin thickness was measured in root slices obtained at specific levels of the root from the furcation and the apical foramen.
In the present study, a great effort was made to ensure the homogeneity of the specimens regarding configuration, volume, and surface area of the root canals in both the coronal and apical thirds based on preoperative scans. Proper pairing of samples increases the validity of the study, substantially reducing the anatomic bias, which could lead to inaccurate results. In addition, canal preparations were performed using a dental mannequin at an ergonomic working position under rubber dam isolation and magnification with an operating microscope to simulate the clinical environment. The coronal third was evaluated because excessive removal of the pericervical dentin has been related to root weakening and strip perforation, whereas the enlargement of the apical portion has been associated with treatment outcome. The middle third was excluded from the analysis because the independent assessment of the root canals was not possible due to the presence of isthmuses. Although some results could be explained based on differences in the overall dimensions of the master instruments used in each group, this was in fact the limitation of the present research because the ProTaper Gold system has no similar instruments to TruNatomy in terms of tip and taper.
Although the TruNatomy system has been claimed to provide a slim shaping instrumentation because of its geometry, regressive tapers, and slim design, the present results do not corroborate this statement. In fact, preparation protocols of the tested systems had similar results for the root canal area and volume as well as untouched canal walls and remaining dentin thickness after preparation. The only statistical differences were noted in the apical canal transportation of mesial roots and the percentage of dentin removal at the coronal third. However, these differences must be critically evaluated in terms of clinical relevance because they were minimal. It is likely that these differences could be more evident if this study had been conducted using narrow canals, but in the regular canal anatomy of mandibular molars, in which both buccolingual and mesiodistal dimensions of the root canal are preserved, it may be said that the tested systems were safe, effective, and performed quite similarly in terms of canal shaping.
In the last years, many practitioners have advocated the idea of minimal canal preparation to preserve the strength and function of endodontically treated teeth. At first glance, this proposal seems logical and justifiable, but it may hide a problem because undershaped, undercleaned, and/or underfilled root canals may increase the odds of failure, especially in the presence ofinfection. For clinicians, it is important to comprehend that although the concept of minimally invasive dentistry is founded on “a systematic respect for the original tissue”, it does not mean that respecting the original tissue is more important than preventing or treating the pulp/periapical disease. This is a common misunderstanding and despite the passionate way that some clinicians defend one side versus the other, usually ignoring experts’ opinions for the sake of commercial informative reports, the positive effect of minimally invasive preparation is still not demonstrated, and, therefore, the uncertainty about this approach remains.
Within the limitations of this study, it was concluded that TruNatomy and ProTaper Gold systems were efficient for performing the preparation of mesial and distal root canals of mandibular molars. The tested systems were similar in terms of untouched canal walls and remaining dentin thickness and slightly different in the apical transportation of mesial canals and the percentage of dentin removal at the coronal third but without clinically significant errors.
Authors: Emmanuel J. N. L. Silva, Carolina Oliveira de Lima, Ana Flavia Almeida Barbosa, Ricardo Tadeu Lopes, Luciana Moura Sassone, and Marco Aurelio Versiani
References:
- Clark D, Khademi J. Modern endodontic access and dentin conservation, part I. Dent Today 2009;28. 86, 88, 90.
- Clark D, Khademi J. Modern endodontic access and dentin conservation, part 2. Dent Today 2009;28. 86, 88, 90.
- Jiang Q, Huang Y, Tu X, et al. Biomechanical properties of first maxillary molars with different endodontic cavities: a finite element analysis. J Endod 2018;44:1283–8.
- Yuan K, Niu C, Xie Q, et al. Comparative evaluation of the impact of minimally invasive preparation vs. conventional straight-line preparation on tooth biomechanics: a finite element analysis. Eur J Oral Sci 2016;124:591–6.
- Zhang Y, Liu Y, She Y, et al. The Effect of endodontic access cavities on fracture resistance of first maxillary molar using the extended finite element method. J Endod 2019;45:316–21.
- Gutmann JL. Minimally invasive dentistry (endodontics). J Conserv Dent 2013;16:282–3.
- Bóveda C, Kishen A. Contracted endodontic cavities: the foundation for less invasive alternatives in the management of apical periodontitis. Endod Topics 2015;3:169–86.
- Bürklein S, Schäfer E. Minimally invasive endodontics. Quintessence Int 2015;46:119–24.
- Paraskevopoulou MT, Khabbaz MG. Influence of taper of root canal shape on the intracanal bacterial reduction. Open Dent J 2016;10:568–74.
- Plotino G, Özyürek T, Grande NM, et al. Influence of size and taper of basic root canal preparation on root canal cleanliness: a scanning electron microscopy study. Int Endod J 2019;52:343–51.
- Barbosa AF, Silva EJ, Coelho BP, et al. The influence of endodontic access cavity design on the efficacy of canal instrumentation, microbial reduction, root canal filling and fracture resistance in mandibular molars. Int Endod J 2020;53:1666–79.
- Sabeti M, Kazem M, Dianat O, et al. Impact of access cavity design and root canal taper on fracture resistance of endodontically treated teeth: an ex vivo investigation. J Endod 2018;44:1402–6.
- Mustafa R, Al Omari T, Al-Nasrawi S, et al. Evaluating in vitro performance of novel nickel-titanium rotary system (TruNatomy) based on debris extrusion and preparation time from severely curved canals. J Endod 2021;47:976–81.
- Peters OA, Arias A, Choi A. Mechanical properties of a novel nickel-titanium root canal instrument: stationary and dynamic tests. J Endod 2020;46:994–1001.
- Kabil E, Katić M, Anić I, et al. Micro-computed evaluation of canal transportation and centering ability of 5 rotary and reciprocating systems with different metallurgical properties and surface treatments in curved root canals. J Endod 2021;47:477–84.
- Pérez Morales ML, González Sánchez AO, Olivieri JG, et al. Micro-computed tomographic assessment and comparative study of the shaping ability of 6 nickel-titanium files: an in vitro study. J Endod 2021;47:812–9.
- Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol 1984;58:589–99.
- Hsu YY, Kim S. The resected root surface. The issue of canal isthmuses. Dent Clin North Am 1997;41:529–40.
- Siqueira JF Jr, Pérez AR, Marceliano-Alves MF, et al. What happens to unprepared root canal walls: a correlative analysis using micro-computed tomography and histology/scanning electron microscopy. Int Endod J 2018;51:501–8.
- Lima CO, Barbosa AF, Ferreira CM, et al. The impact of minimally invasive root canal preparation strategies on the ability to shape root canals of mandibular molars. Int Endod J 2020;53:1680–8.
- Gagliardi J, Versiani MA, de Sousa-Neto MD, et al. Evaluation of the shaping characteristics of ProTaper Gold, ProTaper NEXT, and ProTaper Universal in curved canals. J Endod 2015;41:1718–24.
- Brasil SC, Marceliano-Alves MF, Marques ML, et al. Canal transportation, unprepared areas, and dentin removal after preparation with BT-RaCe and ProTaper Next systems. J Endod 2017;43:1683–7.
- Arias A, Singh R, Peters OA. Torque and force induced by ProTaper universal and ProTaper next during shaping of large and small root canals in extracted teeth. J Endod 2014;40:973–6.
- Pasqualini D, Alovisi M, Cemenasco A, et al. Micro-computed tomography evaluation of Protaper Next and BioRace shaping outcomes in maxillary first molar curved canals. J Endod 2015;41:1706–10.
- Wu MK, Fan B, Wesselink PR. Leakage along apical root fillings in curved root canals. Part I: effects of apical transportation on seal of root fillings. J Endod 2000;26:210–6.
- Bürklein S, Jäger PG, Schäfer E. Apical transportation and canal straightening with different continuously tapered rotary file systems in severely curved root canals: F6 SkyTaper and OneShape versus Mtwo. Int Endod J 2017;50:983–90.
- Veltri M, Mollo A, Mantovani L, et al. A comparative study of Endoflare-Hero Shaper and Mtwo NiTi instruments in the preparation of curved root canals. Int Endod J 2005;38:610–6.
- Gambill JM, Alder M, del Rio CE. Comparison of nickel-titanium and stainless steel hand-file instrumentation using computed tomography. J Endod 1996;22:369–75.
- Silva EJ, Pacheco PT, Pires F, et al. Microcomputed tomographic evaluation of canal transportation and centring ability of ProTaper next and twisted file adaptive systems. Int Endod J 2017;50:694–9.
- Peters OA. Current challenges and concepts in the preparation of root canal systems: a review. J Endod 2004;30:559–67.
- Lim SS, Stock CJ. The risk of perforation in the curved canal: anticurvature filing compared with the stepback technique. Int Endod J 1987;20:33–9.
- Hülsmann M, Peters OA, Dummer P. Mechanical preparation of root canals: shaping goals, techniques and means. Endod Topics 2005;10:30–76.
- Zelic K, Vukicevic A, Jovicic G, et al. Mechanical weakening of devitalized teeth: three-dimensional finite element analysis and prediction of tooth fracture. Int Endod J 2015;48:850–63.
- Fatima S, Kumar A, Andrabi SM, et al. Effect of apical third enlargement to different preparation sizes and tapers on postoperative pain and outcome of primary endodontic treatment: a prospective randomized clinical trial. J Endod 2021;47:1345–51.
- Ericson D. What is minimally invasive dentistry? Oral Health Prev Dent 2004;2(Suppl 1):287–92.

/public-service/media/default/145/GbhGY_65311921a3b65.jpg)
/public-service/media/default/147/bjsSM_65311952dfadf.jpg)
/public-service/media/default/158/GMj69_65311b2333f75.jpg)
/public-service/media/default/148/ix2WY_6531196adc6ec.jpg)