Micro-CT assessment of gap-containing areas along the gutta-percha-sealer interface in oval-shaped canals
Abstract
Aim: To assess the interfacial adaptation (gap-containing areas) of two root canal sealers (EndoSequence BC Sealer and AH Plus) to a conventional gutta-percha (GP) cone (GP-sealer interface) in oval-shaped canals filled using the single cone technique.
Methodology: Sixteen teeth with oval-shaped canals were selected, scanned in a micro-computed tomographic device, and pair-matched according to the volume, aspect ratio and configuration of root canals. Root canals were then sequentially prepared with WaveOne Gold Primary and Large instruments, followed by filling with WaveOne Large GP points associated with either the premixed calcium-silicate EndoSequence BC Sealer or the epoxy resin-based AH Plus sealer (n = 8 per group) using the single cone technique. After 7 days stored in phosphate-buffered saline solution at 37°C, the specimens were rescanned and the reconstructed images segmented in order to differentiate the filling materials (sealer and GP cone) to the dentine. A total of 453 cross-sectional slices were assessed and categorized according to the presence or absence of gaps at the GP-sealer interface. Mann–Whitney U-test verified the differences between groups and were considered significant at alpha = 5%.
Results: Gaps were non-homogenously distributed in two-dimensional axial cross-section images and none of the specimens showed completely gap-free areas along the entire GP-sealer interface. Root canals filled with EndoSequence BC Sealer and AH Plus displayed 171 (37.75%) and 136 (30.02%) slices with gaps in the GP-sealer interface and these frequencies were statistically significant (p = .000).
Conclusions: Although none of the specimens had a gap-free area along the entire GP-sealer interface, oval canals filled with AH Plus showed less gaps than the ones filled with EndoSequence BC Sealer.
Introduction
Hydraulic cements, such as bioactive calcium phosphate ceramics, have been extensively used for bone regeneration due to their high biocompatibility, osteoinductive and osteoconductive properties, in both orthopaedics and dental fields (Daculsi et al., 1990; Demirkiran, 2012; LeGeros, 1988). In Endodontics, hydrophilic bioactive calcium silicate-based sealers (CSS) have earned considerable at- tention since the introduction of iRoot SP (Innovative BioCeramix Inc.) in 2007. This great interest was based upon the premise that CSS were developed as a derived version of the MTA cement, but with optimized handling, biological and viscosity properties (Candeiro et al., 2012; Silva et al., 2017; Silva-Almeida et al., 2017). This material is usually presented as a ready-to-use injectable paste stored in an airtight syringe that allows its application directly into the root canal space. The inherent features and clinical usefulness of CSS streamlined the root canal filling procedure to dentists of all skill levels. Therefore, it proved very popular amongst the endodontic community, even without the complete endorsement of science regarding some critical aspects of its in vitro properties (Elyassi et al., 2019; Silva et al., 2021; Tanomaru-Filho et al., 2017; Torres et al., 2020; Zordan-Bronzel et al., 2019), as well as the lack of long-term observational outcomes from ran- domized perspective clinical trials.
Originally, CSS, as a derived version of the MTA, were developed to fill the whole canal space following the ‘primary monoblock’ concept, which consists of the existence of only one interface extending circumferentially between the material and the root canal walls in order to improve the long-term fluid-tight seal (Tay & Pashley, 2007). Nonetheless, CSS are not appropriate to be used as a unique filler considering the possibility of not penetrating after final setting, precluding retreatment if necessary (Eymirli et al., 2019; Hess et al., 2011). The solution was to use another material—a master gutta- percha (GP) cone—to drive the sealer into the canal irregularities and to serve as a soft-core allowing root canal retreatment. Although this technique aimed to fill the root canal space by cementing a previously fitted GP master cone with CSS, it also introduces an additional interface to the filling mass. The idea of a root filling monoblock with two circumferential interfaces (GP-sealer and sealer-dentine) forming a single cohesive unit has gained attention with the advent of methacrylate-based sealers almost two decades ago. According to some authors, this type of sealer would be the ideal filling material to provide proper coronal seal and improve the fracture resistance of teeth (Shipper et al., 2004, 2005; Teixeira et al., 2004). Unfortunately, long-term clinical outcomes of endodontic treatments showed a high chance of failure in root canals filled with methacrylate-based sealers compared to conventional materials (Barborka et al., 2017; Strange et al., 2019), supporting the results of previous laboratorial studies (De-Deus et al., 2009, 2011; Hiraishi et al., 2007, 2008; Tay, Loushine, et al., 2005a; Tay Pashley, Williams, et al., 2005; Tay, Pashley, Yiu, et al., 2005; Tay et al., 2007).
The ability of the sealer to adhere to both dentinal walls and GP is a desired property since it is an important condition to attain a fluid-proof seal throughout the root canal system. The adhesion of CSS to root dentine was already addressed in several studies (Neelakantan et al., 2015; Oliveira et al., 2016; Sagsen et al., 2011; Silva et al., 2019). However, there is a paucity evidence on the quality of the interfacial adaptation between CSS and conventional GP (Gandolfi et al., 2013; Kim et al., 2017, 2018; Moinzadeh et al., 2015; Pedullà et al., 2020; Viapiana et al., 2016; Zare et al., 2021). Ideally, this is an important aspect once the sealer should bond simultaneously to both dentine and GP to improve the overall quality of the filling. Otherwise, a different interaction among them may result in the development of interfacial gaps, small empty areas usually impossible to be identified radiographically. Such interfacial failure can affect the stability of the GP cone and may function as a path for bacteria and their by-products, consequently compromising the long-term overall quality of root canal treatment.
The purpose of the present study was to assess the quality of the interfacial adaptation (gap-containing areas) between conventional GP cones and the premixed calcium-silicate EndoSequence BC Sealer (Brasseler USA) using micro-computed tomographic (micro-CT) imaging as an analytical tool. AH Plus sealer (Dentsply DeTrey GmbH) was used as reference for comparison. The null hypothesis tested was that the quality of the interface adaptation is not affected by the type of the sealer.
Material and methods
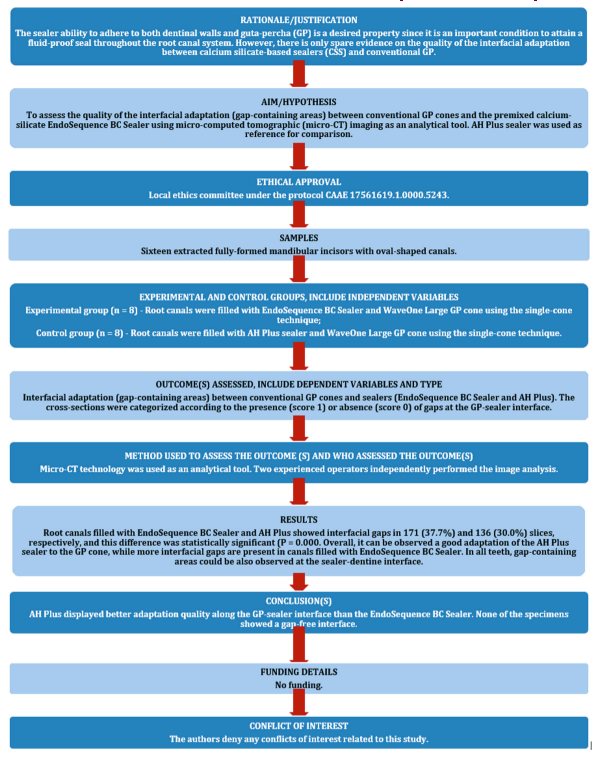
The manuscript of this laboratory study has been written according to Preferred Reporting Items for Laboratory studies in Endodontology (PRILE) 2021 guidelines (Nagendrababu et al., 2021). The steps in this study are depicted in the PRILE flowchart (Figure 1).
Sample size estimation
A score-based evaluation was used to assess the presence of gaps in the filling material per micro-CT cross-section. The number of slices required to verify significant differences between the groups was estimated based on the study of Eltair et al. (2018) in which an effect size of 0.43 was input together with an alpha-type error of 0.05 and power beta of 0.95 into an independent t-test family procedure (G*Power 3.1 for Macintosh; Heinrich Heine, Universität Düsseldorf). The output indicated a minimum of 139 slices per group. Considering the evaluation of 15–20 cross-sections per tooth (obtained at a 0.5-mm interval), a total of eight teeth per group was established for the present study.
Specimen selection and preparation
The local ethics committee approved this study (CAAE 17561619.1.0000.5243). A sample of 237 mandibular incisors obtained from a tooth bank were radiographed in both mesiodistal and buccolingual directions to exclude teeth with more than one root canal, incomplete root formation or fracture. From this initial sampling, 196 teeth were selected and scanned in a micro-CT device (SkyScan 1173; Bruker-microCT) at 70 kV, 114 mA, 19.79 μm (pixel size), 180° rotation around the vertical axis with steps of 0.7°, frame average of 5, using a 1.0-mm-thick aluminium filter. The projection images were reconstructed (NRecon v.1.7.16; Bruker-microCT) with similar parameters for ring artefact correction (4), contrast limits (0–0.05) and beam hardening correction (40%), resulting in 800–900 grayscale cross-sectional slices per tooth, extending from the cementoenamel junction to the apex. After exclusion of teeth with two or more canals or significant accessory anatomy, the cross- sectional images of 146 specimens were segmented using an automatic routine implemented in the ImageJ software (Fiji v.1.51n; Fiji) to create three-dimensional (3D) models of the specimens, as well as, to calculate the volume (in mm3) and the aspect ratio (AR) of the root canals (CTAn v.1.6.6.0; Bruker-microCT; De-Deus et al., 2020). The AR is the mathematical representation of the canal circularity and was measured by calculating the ratio between the major and minor axes of an ellipse fitted to the reconstructed canals in each cross-section using the shape descriptors plug-in of the ImageJ soft- ware. The AR of the root canals was calculated for each cross-section and plotted into a graph. Then, CTAn v.1.6.6.0 software (Bruker-microCT) was used to create 3D models of the root canals of teeth, while CTVol v.2.3.2.0 (Bruker-microCT) was employed to analyse qualitatively the root canal configuration (Figure 2).
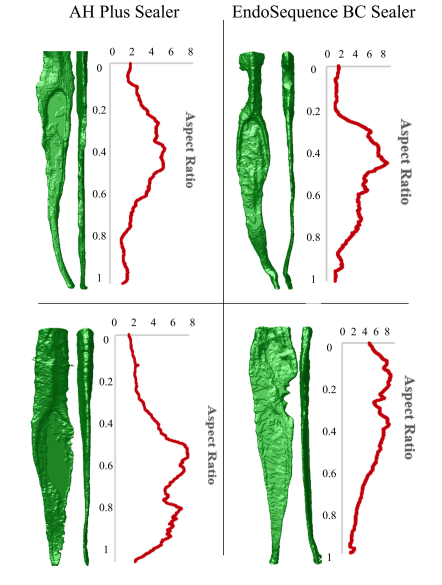
The pair-matching process was undertaken by firstly identifying root canals with similar volume (not higher than 2 mm3), similar AR graphic curves and similar canal configuration. A sample selection using these three parameters is an attempt to isolate the variables of interest, reducing the bias created by anatomic variation, which may be a confounding factor in a study of this nature. After these strict selection criteria, 16 teeth with oval canals (graphical curves of AR > 4) and maximum volume of 5 mm3 were paired (Figure 3), distributed into two experimental groups (n = 8), scanned and reconstructed using the aforementioned parameters, with the exception of pixel size (14.37 μm) and rotation (360°) with steps of 0.5°.
Root canal preparation
Each root was wrapped in Parafilm-M (Bemis NA) and embedded in polyvinyl siloxane (Speedex; Coltene) to simulate a closed-end system and to stabilize the specimens during the experimental procedures. Both the preparation and filling procedures of root canals were done by one specialist in endodontics with more than 8 years of experience.
After conventional access cavity, a size 10 K-file (Dentsply Sirona Endodontics) was used to confirm patency and to establish the working length 1.0 mm short of the apical foramen. Then, root canals were sequentially enlarged using WaveOne Gold Primary and Large instruments (Dentsply Tulsa Dental Specialties) operated with the VDW Silver motor (VDW) in the ‘WAVEONE ALL’ preset program. First, WaveOne Gold Primary was used up to the working length in a slow in-and-out pecking motion with 3 mm amplitude. After three pecking movements, the instrument was removed from the canal and cleaned with alcohol. The working length was achieved after three waves of instrumentation. Then, WaveOne Gold Large was used up to the working length in the same manner of the Primary instrument. Apical patency was confirmed with a size 15 K-file (Dentsply Sirona Endodontics) throughout the instrumentation procedures. After each preparation step with reciprocating instruments, root canals were irrigated with 3 ml of 2.5% sodium hypochlorite (NaOCl) using a 31-G NaviTip double side port needle (Ultradent Inc.) taken up to 1 mm short of the working length while, after patency, 1 ml of irrigant was dispensed. The removal of smear layer was performed using 3 ml of 17% EDTA (5 min) followed by a final flush with 2 ml of bidistilled water. Therefore, a total of 20 ml of irrigant solution was used in each root canal.
Root canal filling
The root canals were dried with paper points (Dentsply Sirona Endodontics) and filled using the single cone technique with WaveOne Large GP points (Dentsply Sirona Endodontics) associated with either EndoSequence BC Sealer (experimental group; n = 8) or AH Plus (control group, n = 8). The tested materials were prepared in separate glass slabs following the specific recommendations of each manufacturer. For the obturation procedure, 80 μl of sealer were obtained with a micropipette and delivered into each root canal with a size 25 K-file (Dentsply Sirona Endodontics) in a counter-clockwise rotation. Then, a WaveOne Large GP cone was gently inserted into the root canal space up to the working length. The excess of the GP cone was removed with a heat carrier (B&L Biotech) at the canal orifice level and the remaining material was vertically compacted with a compatible hand plugger (B&L Biotech). The quality of the root fillings was accessed by taken digital radiographs from buccolingual and mesiodistal directions and no specimen was discarded. Access cavities were then filled with Cavit G (3M ESPE) and the specimens stored at 37°C in phosphate-buffered saline solution for 7 days to allow the complete setting of the sealers. An experienced operator performed all procedures. After this period, all speci- mens were scanned again at 100 kV, 80 mA, 14.37 μm, 360° rotation at steps of 0.3° and frame average of 5, filtered by a 0.5-mm-thick aluminium foil.
Micro-CT analysis
After reconstruction of the projection images using contrast limits to enable the differentiation of sealer, GP cone and dentine, approximately 25 cross-sections in which was possible to observe the GP-cone interface were selected per tooth, in a total of 453 images. Two experienced operators independently performed the image analysis in order to categorize the cross sections according to the presence (score 1) or absence (score 0) of gaps at the GP-sealer in- terface. The final outcome was reached by an agreement between them.
Statistical analysis
The score used to categorize the occurrence of interfacial gap between GP cones and the tested sealers, per micro-CT cross-section, was considered as the unit for statistical analysis, and the Mann–Whitney U-test was applied to verify differences between groups at a significant level of 5% (SPSS 21.0; SPSS Inc.).
Results
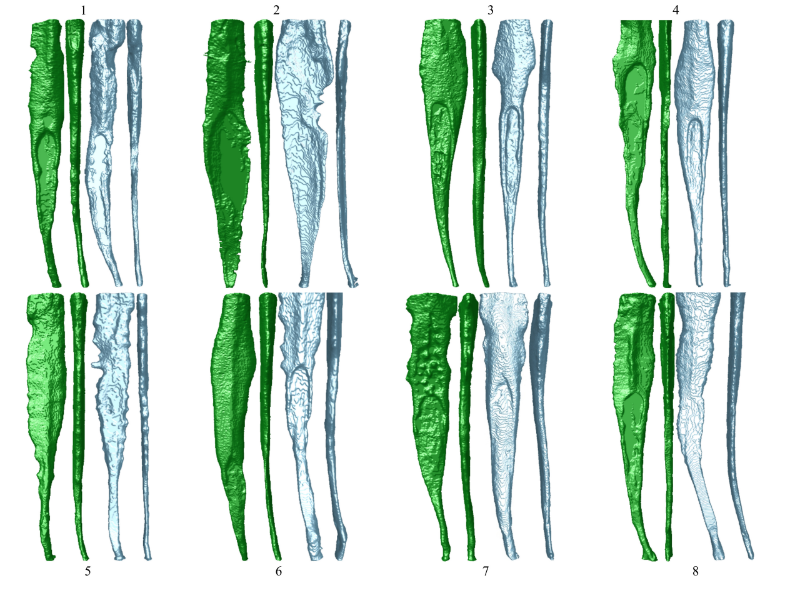
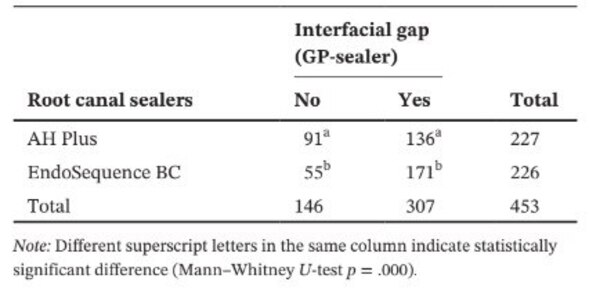
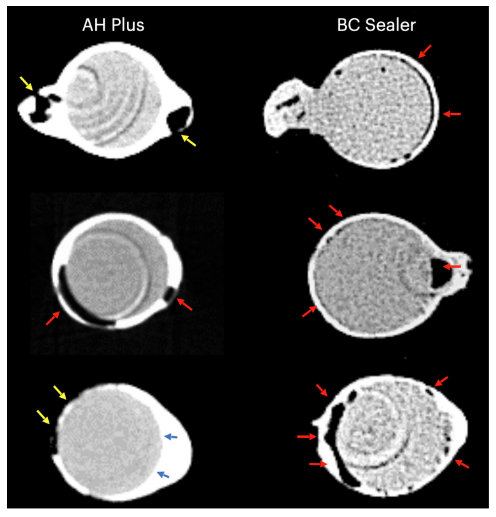
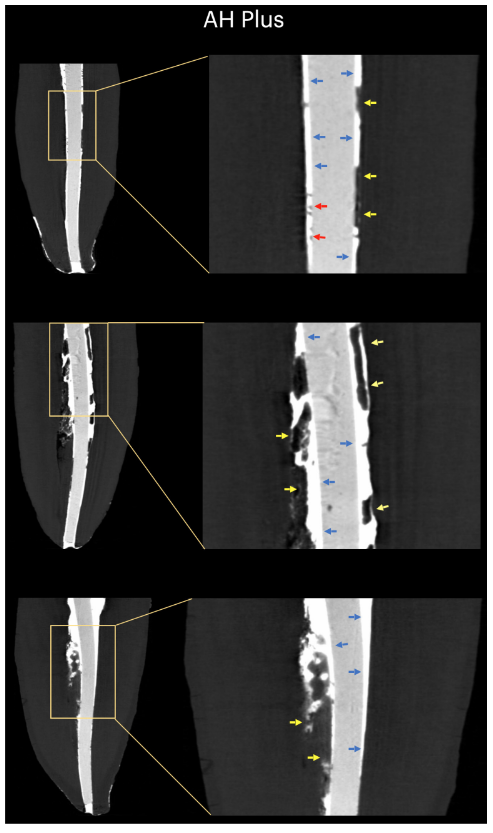
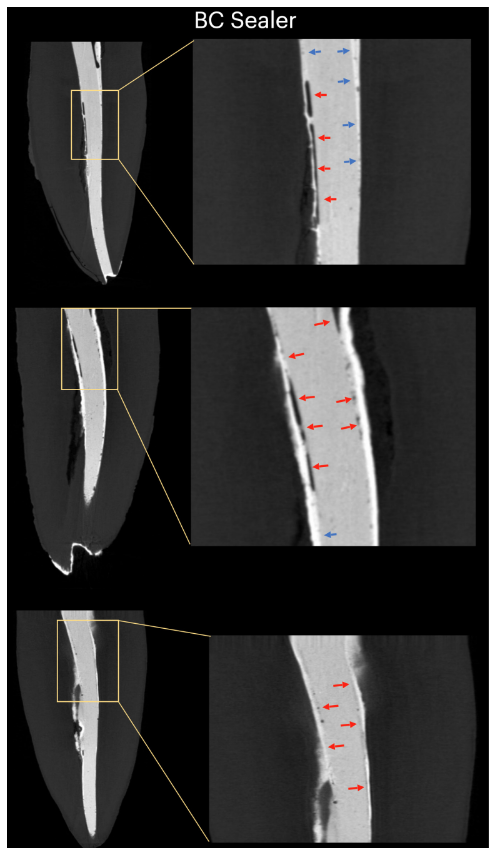
Table 1 presents the number of micro-CT cross-sections distributed according to the occurrence of interfacial gaps between the GP cone and the tested sealers. Gaps were non-homogenously distributed in the two-dimensional (2D) axial cross-section images and none of the specimens showed completely gap-free areas along the whole GP-sealer interface. Root canals filled with EndoSequence BC Sealer and AH Plus showed interfacial gaps in 171 (37.7%) and 136 (30.0%) slices, respectively, and this difference was statistically significant (p = .000). Figures 4–7 show representative transaxial and sagittal micro-CT images of root canals of mandibular incisors filled with single-cone technique using AH Plus and EndoSequence BC Sealer. Overall, it can be observed a good adaptation of the AH Plus sealer to the GP cone, while more interfacial gaps are present in canals filled with EndoSequence BC Sealer. In all teeth, gap-containing areas could be also observed at the sealer-dentine interface.

Discussion
The present study used a non-destructive analytical tool to evaluate the interfacial adaptation between conventional GP cones and different root canal sealers (AH Plus and EndoSequence BC Sealer), in anatomically matched oval-shaped canals of mandibular incisors filled using the single-cone technique. The results showed that teeth filled with EndoSequence BC Sealer had substantially higher frequency of cross-section images showing gaps in the GP-sealer interface than the ones filled with AH Plus, and the null hypothesis was rejected.
In the literature, several studies using different methods of analysis have reported contradictory results on the presence of gaps and voids in root canals filled with CSS (Gandolfi et al., 2013; Kim et al., 2017, 2018; Moinzadeh et al., 2015; Pedullà et al., 2020; Viapiana et al., 2016; Zare et al., 2021). Using the micro-CT technology, Yanpiset et al. (2018) reported minimal gaps and voids in teeth filled with the CSS TotalFill BC Sealer (FKG Dentaire, La Chaux-de-Fonds, Switzerland) and coated GP cones. Similarly, Eltair et al. (2018) did not demonstrate significant difference in the interfacial gaps between TotalFill BC Sealer and AH Plus, combined with coated or conventional GP cones, through a descriptive analysis with scanning electron microscopy. These results, however, contradict previous findings from Zhang et al. (2010) that demonstrated a better interfacial adaptation of iRoot SP sealer to GP when compared to AH Plus. Moreover, whilst Viapiana et al. (2016) showed that BioRoot RCS (Septodont) was associated with greater percentage of voids than AH Plus, Gandolfi et al. (2013), Kim et al. (2017) and Zare et al. (2021) did not report any differences among AH Plus and different brands of CSS. These inconsistencies might be mostly explained by methodological differences related to the micro-CT device (scanning and reconstruction parameters), sample selection, quality of root canal preparation, operators’ experience, filling technique and physicochemical proper- ties of the tested sealers. Thus, the rationale to interpret these dissimilarities when compared to the present results is based upon the fact that most of studies using micro-CT focused on the overall analysis of the percentage of voids calculated by assessing the volume of filling materials in relation to the prepared canal space (Gandolfi et al., 2013; Kim et al., 2017, 2018; Moinzadeh et al., 2015; Pedullà et al., 2020; Viapiana et al., 2016). This approach, however, fails to consider the specific interaction of the sealer and GP, as demonstrated in the present study, using a specific score-based parameter, which helps to understand the inconsistencies observed in relation to previous findings.
In this study, oval-shaped canals filled with conventional GP and EndoSequence BC Sealer using the single-cone technique had a higher number of slices presenting gaps in the GP-sealer interface than when using AH Plus (Table 1). Beyond some technical aspects of the root canal filling and differences in the physicochemical properties of the sealers, the present results can be also explained by variations in the chemical surface polarities between the tested sealers and the core material. Overall, GP points have only about 20% of the chemical composition to be GP, whereas the 60%–75% of the composition is zinc oxide filler. The remaining constituents are wax or resin to make the point more pliable and/or compactible and metal salts to lend radiopacity. On an organic versus inorganic basis, GP points are only 23.1% organic (GP and wax) and 76.4% inorganic fillers (zinc oxide and barium sulphate; Friedman et al., 1977). GP has a chemical structure based on the polymerization of a stereoisomer of isoprene, the monomer forming natural rubber, which leads to higher crystallinity having around 30%–40% hydrophobicity. In other words, GP’s hydrophobic properties are a consequence of its aliphatic chemical nature (Le Ferrand & Bacha, 2021). The other two main components of GP points are zinc oxide, wax and barium sulphate (inorganic fillers), which, in turn, also have hydrophobic features (Friedman et al., 1977; Moorer & Genet, 1982; Wilson et al., 1973; Wolfmeier et al., 2002). Therefore, it is possible that the hydrophobic nature of the GP cone has repelled more the CSS, a material that is well-known by its hydrophilicity (Hegde & Arora, 2015), than the AH Plus, an epoxy resin-based material that has a hydrophobic radical on its molecule (Lee et al., 2017), which partially explain the lowest number of gaps observed along its interface. Although the magnitude of the polarization forces between hydrophilic and hydrophobic endodontic materials is still to be determined, it is possible that these are weak forces. Consequently, it is unlikely that it could have a huge influence on their interaction, mostly when considering that these materials are enclosed within rigid dentinal walls. However, in an anatomical condition in which a large amount of sealer is needed to fill the root canal space, as when using the single-cone technique in oval-shaped canals, it may be hypothesized that the available space between the GP cone and the dentinal walls can provide enough space for the action of these forces. As shown in Figures 4 to 7, the GP-sealer interfacial gaps were mostly observed at the buccal and lingual aspects of the root canals, that is, the largest areas between the core and the dentinal walls in which the highest amount of sealer is located. One may argue that the present results were as a consequence of the improper use of CSS with conventional GP instead of calcium silicate-coated cones. However, so far, no manufacturer has disclosed that CSS could not be used with conventional GP points. Actually, a recent survey reported that only 22.1% of CSS users have employed pre-coated GP in their root canal fillings (Guivarc'h et al., 2020), evidence that endorses the main aim of the present study.
Although micro-CT technology allows non-destructive volumetric experiments, the high density of filling materials usually has a significant impact in the output quality of the reconstructed images, mainly at the edge regions, making the evaluation of interfaces a real challenge, especially when the density between sealer and GP cones are similar, directly affecting their contrasts (Sun et al., 2009; Zeiger et al., 2009). This means that even images acquired using adequate scanning and reconstructing parameters in appropriate micro-CT devices may often result in non-neglectable difficulties to identify and differentiate the boundaries between the root canal walls and filling components. This is a critical methodological aspect considering that the threshold determination for image segmentation is a subjective procedure that relies on the operator's experience and, consequently, may have a direct influence on the accuracy and reliability of the results. When dealing with non-homogenous structures, such as dentine, sealer and GP cones, this is quite a challenging task and still non-consensual aspect of the micro-CT assessment. Therefore, it is a misconception to believe that only the pixel size would determine the quality of the images obtained from a micro-CT scanning. In fact, it is the interplay between the contrast sensitivity and spatial resolution that defines what can be achieved with a CT scan (Stock 2009). While contrast resolution of a given image is a measure of how well a feature of interest can be distinguished from the neighbouring background, the spatial resolution describes how well small details can be imaged or small features can be located with respect to a reference point (Ketcham & Carlson, 2001). In the present study, although specimens were scanned using a pixel size of 14.37 μm, the overall contrast resolution of the acquired images was of medium quality and, therefore, no quantitative volumetric measurements of gaps were possible to be done, which may be considered a limitation of this study. However, the output quality was enough to identify and score the gap-containing areas along the GP-sealer interface using 2D transaxial images. Although some may argue that the pixel size used in this study is high, Pinto et al. (2021) demonstrated that visual and automatic segmentation can be applied to micro-CT images with voxel sizes from 5 to 20 µm to evaluate the filling of a sealer with radiopacity that complies with ISO 6876:2012 standard (ISO, 2012) such as the AH Plus (Silva et al., 2013) and EndoSequence BC Sealer (Candeiro et al., 2012).
As in this study, a recent micro-CT investigation also used 2D image slices to evaluate the GP-sealer interface in root canals of maxillary anterior teeth filled with the single-cone technique using conventional GP associated with AH Plus or EndoSequence BC sealers (Zare et al., 2021), but scanning was performed in a high-resolution device using a smaller pixel size (6 μm). In contrast with the present results, AH Plus group had a significantly lower GP-sealer interface (contact) ratio than the EndoSequence BC, and this dissimilarity can be explained by some methodological differences related to the root canal morphology (which was more round), the method of application of sealer (the ‘buttered’ cone technique) that favours materials with low viscosity such as CSS. Besides, in order to improve the overall quality of the analysis in the present study, two experienced operators performed the segmentation procedures and all analyses in separate, and the final outcome was reached by an agreement between them. A special care was also taken to ensure the comparability among the experimental groups by equalizing the anatomical factor. Well-balanced experimental groups were created by selecting anatomically matching root canals according to the AR, volume and 3D canal geometry after scanning 237 mandibular incisors (De-Deus et al., 2020). This approach allows a better control of the confounding effect that anatomical variances in root canal morphology may have on the results of laboratorial studies. Considering that minimising gaps in the GP-sealer and dentine-sealer interfaces is clinically relevant to prevent penetration of bacteria and/or their by-products (Yücel & Çiftçi, 2006), the present results should encourage the development of further studies to validate the filling ability of the single-cone technique with CSS not only in different canal morphologies, but also in teeth prepared with minimally invasive approaches.
Conclusions
Under the experimental framework of the current study, it may be concluded that AH Plus displayed better adaptation quality along the GP-sealer interface than the EndoSequence BC Sealer. None of the specimens showed a gap-free interface.
Authors: Gustavo De-Deus, Gustavo O. Santos, Iara Zamboni Monteiro, Daniele M. Cavalcante, Marco Simões-Carvalho, Felipe G. Belladonna, Emmanuel J. N. L. Silva, Erick M. Souza, Raphael Licha, Carla Zogheib, Marco A. Versiani
References
- Barborka, B.J., Woodmansey, K.F., Glickman, G.N., Schneiderman, E. & He, J. (2017) Long-term clinical outcome of teeth obturated with Resilon. Journal of Endodontics, 43, 556–560.
- Candeiro, G.T., Correia, F.C., Duarte, M.A., Ribeiro-Siqueira, D.C. & Gavini, G. (2012) Evaluation of radiopacity, pH, release of calcium ions, and flow of a bioceramic root canal sealer. Journal of Endodontics, 38, 842–845.
- Daculsi, G., Passuti, N., Martin, S., Deudon, C., Legeros, R.Z. & Raher, S. (1990) Macroporous calcium phosphate ceramic for long bone surgery in humans and dogs. Clinical and histological study. Journal of Biomedical Materials Research, 24, 379–396.
- De-Deus, G., Di Giorgi, K., Fidel, S., Fidel, R.A. & Paciornik, S. (2009) Push-out bond strength of Resilon/Epiphany and Resilon/ Epiphany self-etch to root dentin. Journal of Endodontics, 35, 1048–1050.
- De-Deus, G., Reis, C., Di Giorgi, K., Brandão, M.C., Audi, C. & Fidel, R.A. (2011) Interfacial adaptation of the Epiphany self-adhesive sealer to root dentin. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontics, 11, 381–386.
- De-Deus, G., Simões-Carvalho, M., Belladonna, F.G., Versiani, M.A., Silva, E.J.N.L., Cavalcante, D.M. et al. (2020) Creation of well-balanced experimental groups for comparative endodontic laboratory studies: a new proposal based on micro-CT and in silico methods. International Endodontic Journal, 53, 974–985.
- Demirkiran, H. (2012) Bioceramics for osteogenesis, molecular and cellular advances. In: Jandial, R. & Chen, M.Y. (Eds.) Regenerative biology of the spine and spinal cord. Advances in experimental medicine and biology. New York, NY: Springer, p. 760.
- Eltair, M., Pitchika, V., Hickel, R., Kühnisch, J. & Diegritz, C. (2018) Evaluation of the interface between gutta-percha and two types of sealers using scanning electron microscopy (SEM). Clinical Oral Investigations, 22, 1631–1639.
- Elyassi, Y., Moinzadeh, A.T. & Kleverlaan, C.J. (2019) Characterization of leachates from 6 root canal sealers. Journal of Endodontics, 45, 623–627.
- Eymirli, A., Sungur, D.D., Uyanik, O., Purali, N., Nagas, E. & Cehreli, Z.C. (2019) Dentinal tubule penetration and retreatability of a calcium silicate-based sealer tested in bulk or with different main core material. Journal of Endodontics, 45, 1036–1040.
- Friedman, C.E., Sandrik, J.L., Heuer, M.A. & Rapp, G.W. (1977) Composition and physical properties of gutta-percha endodontic filling materials. Journal of Endodontics, 3, 304–308.
- Gandolfi, M.G., Parrilli, A.P., Fini, M., Prati, C. & Dummer, P.M. (2013) 3D micro-CT analysis of the interface voids associated with Thermafil root fillings used with AH Plus or a flowable MTA sealer. International Endodontic Journal, 46, 253–263.
- Guivarc’h, M., Jeanneau, C., Giraud, T., Pommel, L., About, I., Azim, A.A. et al. (2020) An international survey on the use of calcium silicate-based sealers in non-surgical endodontic treatment. Clinical Oral Investigations, 1, 417–424.
- Hegde, V. & Arora, S. (2015) Sealing ability of a novel hydrophilic vs. conventional hydrophobic obturation systems: a bacterial leakage study. Journal of Conservative Dentistry, 18, 62–65.
- Hess, D., Solomon, E., Spears, R. & He, J. (2011) Retreatability of a bioceramic root canal sealing material. Journal of Endodontics, 37, 1547–1549.
- Hiraishi, N., Sadek, F.T., King, N.M., Ferrari, M., Pashley, D.H. & Tay, F.R. (2008) Susceptibility of a polycaprolactone-based root canal filling material to degradation using an agar-well diffusion assay. American Journal of Dentistry, 21, 119–123.
- Hiraishi, N., Yau, J.Y.Y., Loushine, R.J., Armstrong, S.R., Weller, R.N., King, N.M. et al. (2007) Susceptibility of a polycaprolactone-based root canal-filling material to degradation. III. turbidimetric evaluation of enzymatic hydrolysis. Journal of Endodontics, 33, 952–956.
- ISO. (2012) International Standard ISO 6876:2012: dental root canal sealing materials. Geneva: Switzerland.
- Ketcham, R.A. & Carlson, W.D. (2001) Acquisition, optimization and interpretation of X-ray computed tomographic imagery: applications to the geosciences. Computers and Geosciences, 27, 381–400.
- Kim, J.A., Hwang, Y.C., Rosa, V., Yu, M.K., Lee, K.W. & Min, K.S. (2018) Root canal filling quality of a premixed calcium silicate endodontic sealer applied using gutta-percha cone-mediated ultrasonic activation. Journal of Endodontics, 44, 133–138.
- Kim, S., Kim, S., Park, J.W., Jung, I.Y. & Shin, S.J. (2017) Comparison of the percentage of voids in the canal filling of a calcium silicate-based sealer and gutta-percha cones using two obturation techniques. Materials, 12(10), 1170.
- Le Ferrand, H. & Bacha, A. (2021) Discovery and rediscovery of gutta percha, a natural thermoplastic. MRS Bulletin, 46, 84–85.
- Lee, J.K., Kwak, S.W., Ha, J.H., Lee, W.C. & Kim, H.C. (2017) Physicochemical properties of epoxy resin-based and bioceramic-based root canal sealers. Bioinorganic Chemistry and Applications, 2017, 1–8.
- LeGeros, R.Z. (1988) Calcium phosphate materials in restorative dentistry: a review. Advances in Dental Research, 2, 164–180.
- Moinzadeh, A.T., Zerbst, W., Boutsioukis, C., Shemesh, H. & Zaslansky, P. (2015) Porosity distribution in root canals filled with gutta-percha and calcium silicate cement. Dental Materials, 31, 1100–1108.
- Moorer, W.R. & Genet, J.M. (1982) Antibacterial activity of gutta- percha cones attributed to the zinc oxide component. Oral Surgery, Oral Medicine, and Oral Pathology, 53, 508–517.
- Nagendrababu, V., Murray, P.E., Ordinola-Zapata, R., Peters, O.A., Rôças, I.N., Siqueira, J.F. Jr. et al. (2021) PRILE 2021 guide- lines for reporting laboratory studies in Endodontology: explanation and elaboration. International Endodontic Journal, 54, 1491–1515.
- Neelakantan, P., Nandagopal, M., Shemesh, H. & Wesselink, P. (2015) The effect of root dentin conditioning protocols on the push-out bond strength of three calcium silicate sealers. International Journal of Adhesion and Adhesives, 60, 104–108.
- Oliveira, D.S., Cardoso, M.L., Queiroz, T.F., Silva, E.J., Souza, E.M. & De-Deus, G. (2016) Suboptimal push-out bond strengths of calcium silicate-based sealers. International Endodontic Journal, 49, 796–801.
- Pedullà, E., Abiad, R.S., Conte, G., La Rosa, G.R.M., Rapisarda, E. & Neelakantan, P. (2020) Root fillings with a matched-taper single cone and two calcium silicate-based sealers: an analysis of voids using micro-computed tomography. Clinical Oral Investigations, 24, 4487–4492.
- Pinto, J.C., Torres, F.F.E., Lucas-Oliveira, E., Bonagamba, T.J., Guerreiro-Tanomaru, J.M. & Tanomaru-Filho, M. (2021) Evaluation of curved root canals filled with a new bioceramic sealer: a microcomputed tomographic study using images with different voxel sizes and segmentation methods. Microscopy Research and Technique, 84, 2960–2967.
- Sagsen, B., Ustun, Y., Demirbuga, S. & Pala, K. (2011) Push-out bond strength of two new calcium silicate-based endodontic sealers to root canal dentine. International Endodontic Journal, 44, 1088–1091.
- Shipper, G., Ørstavik, D., Teixeira, F.B. & Trope, M. (2004) An evaluation of microbial leakage in roots filled with a thermoplastic synthetic polymer-based root canal filling material (Resilon). Journal of Endodontics, 30, 342–347.
- Shipper, G., Teixeira, F.B., Arnold, R.R. & Trope, M. (2005) Periapical inflammation after coronal microbial inoculation of dog roots filled with gutta-percha or Resilon. Journal of Endodontics, 31, 91–96.
- Silva, E.J.N.L., Canabarro, A., Andrade, M.R.T.C., Cavalcante, D.M., Von Stetten, O., Fidalgo, T.K.D.S. et al. (2019) Dislodgment resistance of bioceramic and epoxy sealers: a systematic review and meta-analysis. Journal of Evidence-Based Dental Practice, 19, 221–235.
- Silva, E.J.N.L., Ehrhardt, I.C., Sampaio, G.C., Cardoso, M.L., Oliveira, D.D.S., Uzeda, M.J. et al. (2021) Determining the setting of root canal sealers using an in vivo animal experimental model. Clinical Oral Investigations, 25, 1899–1906.
- Silva, E.J., Rosa, T.P., Herrera, D.R., Jacinto, R.C., Gomes, B.P. & Zaia, A.A. (2013) Evaluation of cytotoxicity and physicochemical properties of calcium silicate-based endodontic sealer MTA Fillapex. Journal of Endodontics, 39, 274–277.
- Silva, E.J.N.L., Zaia, A.A. & Peters, O.A. (2017) Cytocompatibility of calcium silicate-based sealers in a three-dimensional cell cul- ture model. Clinical Oral Investigations, 21, 1531–1536.
- Silva-Almeida, L.H., Moraes, R.R., Morgental, R.D. & Pappen, F.G. (2017) Are premixed calcium silicate-based endodontic sealers comparable to conventional materials? A systematic review of in vitro studies. Journal of Endodontics, 43, 527–535.
- Strange, K.A., Tawil, P.Z., Phillips, C., Walia, H.D. & Fouad, A.F. (2019) Long-term outcomes of endodontic treatment performed with Resilon/Epiphany. Journal of Endodontics, 45, 507–512.
- Sun, J., Eidelman, N. & Lin-Gibson, S. (2009) 3D mapping of polymerization shrinkage using X-ray micro-computed tomography to predict microleakage. Dental Materials, 25, 314–320.
- Tanomaru-Filho, M., Torres, F.F.E., Chavez-Andrade, G.M., de Almeida, M., Navarro, L.G., Steier, L. et al. (2017) Physicochemical properties and volumetric change of silicone/ bioactive glass and calcium silicate-based endodontic sealers. Journal of Endodontics, 43, 2097–2101.
- Tay, F.R., Loushine, R.J., Lambrechts, P., Weller, R.N. & Pashley, D.H. (2005a) Geometric factors affecting dentin bonding in root canals: a theoretical modeling approach. Journal of Endodontics, 31, 584–589.
- Tay, F., Pashley, D., Williams, M., Raina, R., Loushine, R., Weller,
- R. et al. (2005b) Susceptibility of a polycaprolactone-based root canal filling material to degradation. I. Alkaline hydrolysis. Journal of Endodontics, 31, 593–598.
- Tay, F.R., Pashley, D.H., Yiu, C.K.Y., Yau, J.Y.Y., Yiu-fai, M., Loushine, R.J. et al. (2005c) Susceptibility of a polycaprolactone-based root canal filling material to degradation. II. Gravimetric evaluation of enzymatic hydrolysis. Journal of Endodontics, 31, 737–741.
- Tay, F.R. & Pashley, D.H. (2007) Monoblocks in root canals: a hypothetical or a tangible goal. Journal of Endodontics, 33, 391–398.
- Tay, F.R., Pashley, D.H., Loushine, R.J., Kuttler, S., García-Godoy, F., King, N.M. et al. (2007) Susceptibility of a polycaprolactone-based root canal filling material to degradation. Evidence of biodegradation from a simulated field test. American Journal of Dentistry, 20, 365–369.
- Teixeira, F.B., Teixeira, E.C., Thompson, J.Y. & Trope, M. (2004) Fracture resistance of roots endodontically treated with a new resin filling material. Journal of the American Dental Association, 135, 646–652.
- Torres, F.F.E., Zordan-Bronzel, C.L., Guerreiro-Tanomaru, J.M., Chavez-Andrade, G.M., Pinto, J.C. & Tanomaru-Filho, M. (2020) Effect of immersion in distilled water or phosphate-buffered saline on the solubility, volumetric change and presence of voids within new calcium silicate-based root canal sealers. International Endodontic Journal, 53, 385–391.
- Viapiana, R., Moinzadeh, A.T., Camilleri, L., Wesselink, P.R., Tanomaru Filho, M. & Camilleri, J. (2016) Porosity and sealing ability of root fillings with gutta-percha and BioRoot RCS or AH Plus sealers. Evaluation by three ex vivo methods. International Endodontic Journal, 49, 774–782.
- Wilson, A.D., Clinton, D.J. & Miller, R.P. (1973) Zinc oxide-eugenol cements: IV. Microstructure and hydrolysis. Journal of Dental Research, 52, 253–260.
- Wolfmeier, U., Schmidt, H., Heinrichs, F.L., Michalczyk, G., Payer, W., Dietsche, W. et al. (2002) Waxes. In: Ullmann's Encyclopedia of industrial chemistry. Vol 39. Weinheim: Wiley:112–172.
- Yanpiset, K., Banomyong, D., Chotvorrarak, K. & Srisatjaluk, R.L. (2018) Bacterial leakage and micro-computed tomography evaluation in round-shaped canals obturated with bioceramic cone and sealer using matched single cone technique. Restorative Dentistry & Endodontics, 43, e30.
- Yücel, A.C. & Çiftçi, A. (2006) Effects of different root canal obturation techniques on bacterial penetration. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontics, 102, e88–e92.
- Zare, S., Shen, I., Zhu, Q., Ahn, C., Primus, C. & Komabayashi, T. (2021) Micro-computed tomographic evaluation of single-cone obturation with three sealers. Restorative Dentistry & Endodontics, 46, e25.
- Zeiger, D.N., Sun, J., Schumacher, G.E. & Lin-Gibson, S. (2009) Evaluation of dental composite shrinkage and leakage in extracted teeth using X-ray microcomputed tomography. Dental Materials, 25, 1213–1220.
- Zhang, W., Li, Z. & Peng, B. (2010) Effects of iRoot SP on mineralization-related genes expression in MG63 cells. Journal of Endodontics, 36, 1978–1982.
- Zordan-Bronzel, C.L., Esteves Torres, F.F., Tanomaru-Filho, M., Chavez-Andrade, G.M., Bosso-Martelo, R. & Guerreiro-Tanomaru, J.M. (2019) Evaluation of physicochemical properties of a new calcium silicate-based sealer, Bio-C sealer. Journal of Endodontics, 45, 1248–1252.
