Digital workflows for the management of tooth wear
Abstract
For patients affected by tooth wear who require treatment to restore their dentition, the methods chosen can increasingly involve digital technology, with potentially less use of traditional, analogue treatment methods. Digital technology has transformed clinical photography and dental radiology, and is now available for most of the stages required for managing these patients. Continuous development of these digital technologies, both in the system capability and in the clinician interface, has brought the digital workflow within reach of more clinicians and therefore, for the treatment of more patients. While it is recognised that the comprehensive use of digital technologies is currently most likely to be used in clinical practice by specialist and private practitioners, it is expected that interest in and understanding of digital workflows will increase throughout the dental profession.
This paper provides a step-by-step overview of the digital workflow, for both simple and complex cases.
Introduction
The focus of this article is to present the digital workflow in managing tooth wear.
The necessary considerations for clinical treatment start with a comprehensive analysis and this is based on the three pillars of treatment planning:
- Desirability – understanding the patient’s true desires – are these aesthetic or functional requests?
2. Suitability – is the oral environment suitable for the outcome the patient wants? For example, the patient is not motivated to manage their oral hygiene yet desires porcelain veneers to improve the smile. This step involves:
- Medical and dental history
- Extraoral analysis – temporomandibular joint, muscles
- Aesthetic analysis (facial and dental)
- Intra-oral and dental assessment, including occlusion
- Periodontal assessment
- Radiographic assessment
- Functional analysis
- Phonetic analysis.
3. Affordability – finding a treatment option that suits the patient’s finances
There are also three main components to the digital workflow (Fig. 1):

- Data acquisition
- Data planning and digital design
- Data execution and delivery.
Data acquisition
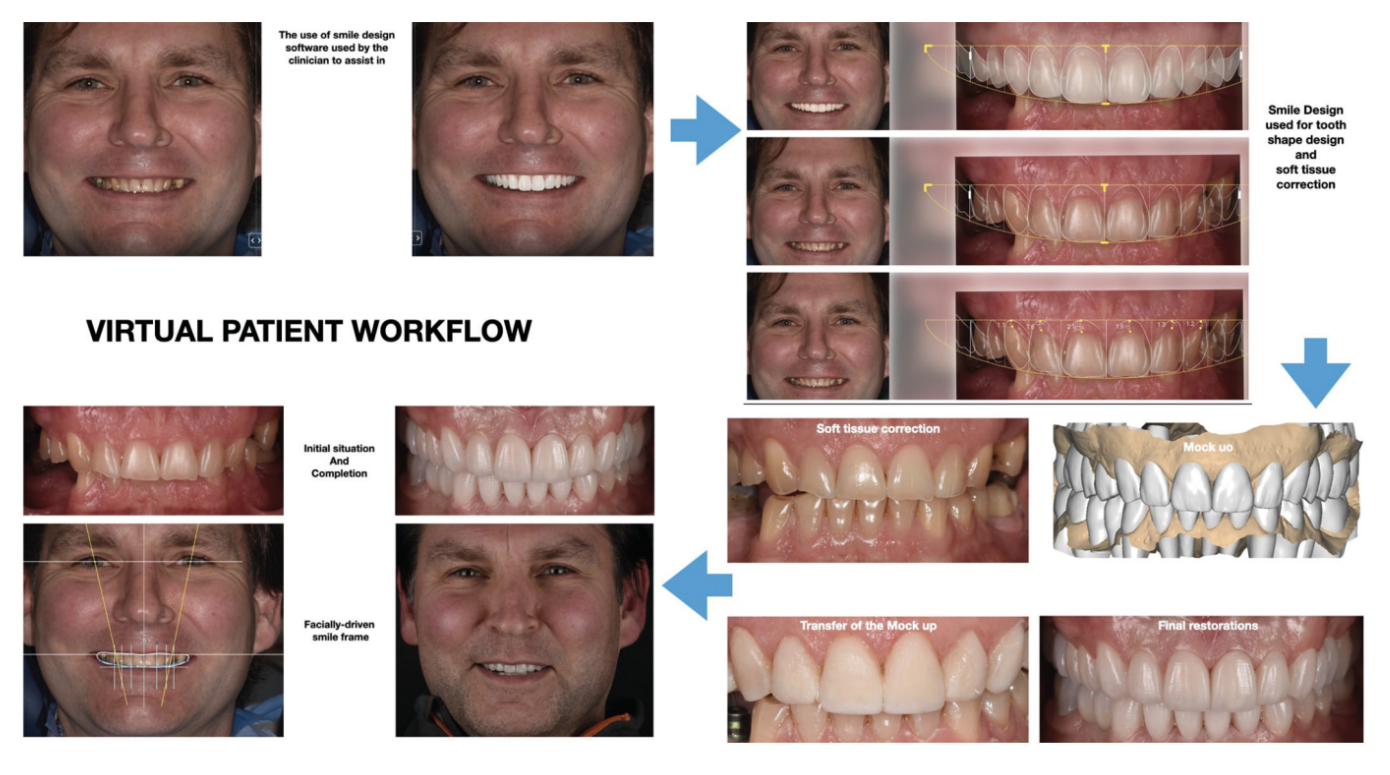
The objective of both analogue and digital workflows is a successful aesthetic and functional outcome, and data acquisition is the first step in ‘digitising’ the patient, which allows the clinician to plan treatment effectively. The combining of face scanners (FS), computed tomography and intra-oral scanning have created the virtual patient, and this is the starting point for 3D planning.
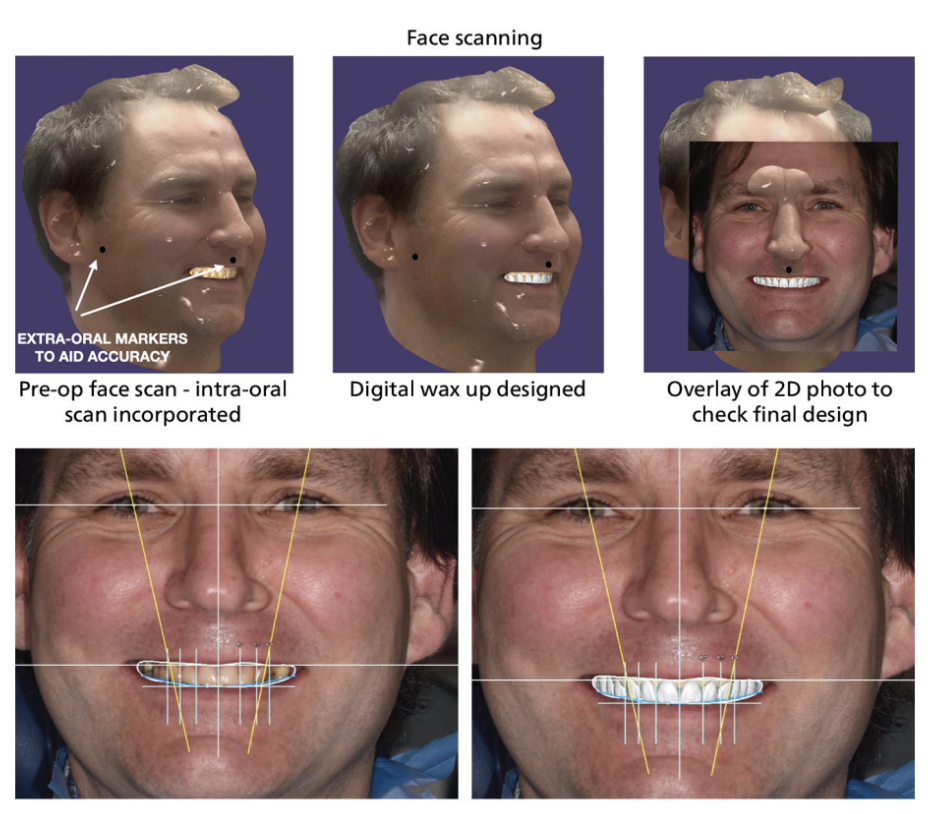
Facial scanning
The use of face scanning transfers the extra- oral features to aid the orientation of the facial vertical and horizontal lines in three dimensions and assists in matching with the dental vertical and horizontal lines. It improves the communication between the clinician, patient and dental technician, improving satisfaction and reducing the risk of an unacceptable outcome. The limitation is the scan quality detailing the teeth, hence the use of a picture to improve accuracy (Fig. 2).
Intra-oral scanning
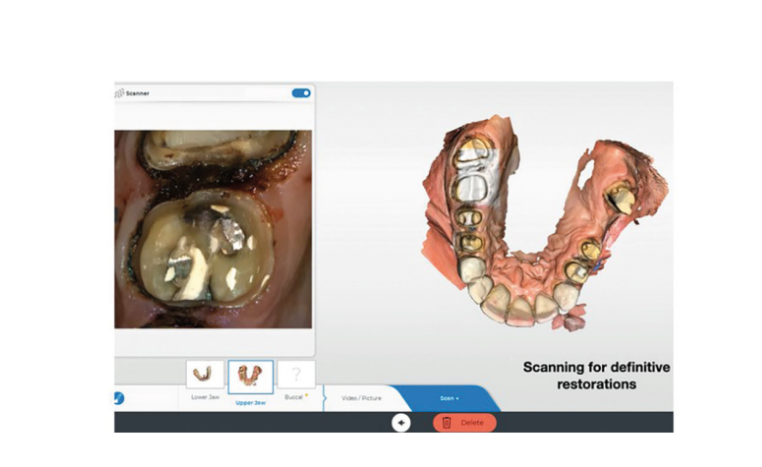
Intra-oral scanners take digital impressions and allow the transfer of the maxillary and mandibular arches, including bite registration. Alternatively, traditional analogue impressions can also be digitised at the laboratory using digital model scanners, highlighting the progression within the technical discipline (Fig. 3).

Recording the static occlusal position
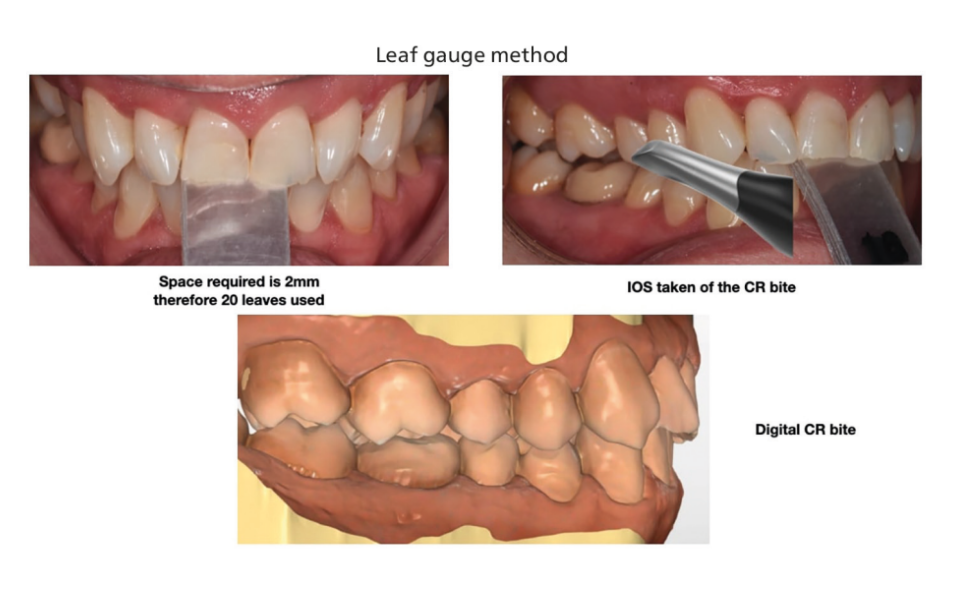
Whether conforming to the existing occlusion or re-organising the occlusion by restoration, it is necessary to accurately record an occlusal position. The joint reference position, centric relation (CR), is usually chosen, due to the variability in the centric occlusion position at maximum intercuspation. Several methods exist for determining the CR position and the author usually prefers a leaf gauge or an anterior stop device.
The leaf gauge or anterior stop device is placed anteriorly and the patient is asked to move the mandible forward (beyond the edge- edge position) and then backwards a few times until they are confident to do so. When the mandible reaches the most posterior position, the patient maintains contact with the leaf gauge and holds that position. This mandibular position is considered to be CR. An intra-oral scan of the left and right buccal segments then records the CR position (Fig. 4).
Articulation of digital impressions
The placement of the models within the digital articulator aims to position the maxilla to the craniofacial reference planes in a natural head position (NHP), which is reproducible but can be affected by several factors, such as airway patency and malocclusion type. Techniques available to use are:
- 3D face scan (in NHP) with 2D photograph
- A digital facebow
- Cone-beam computed tomography
- Stereophotogrammetry
- 4D virtual articulator – jaw motion analysis (Modjaw device)
- Kois facial reference glasses.
Recording dynamic occlusal movements
When using virtual digital articulators, the mandibular movements are estimated by simulation and the use of average values leads to restorations designed with shallow cusp angles/height and wider fossa shape. The 4D jaw motion analysis – Modjaw – can be used to digitally record and analyse dynamic lateral and protrusive mandibular movements (Fig. 5).
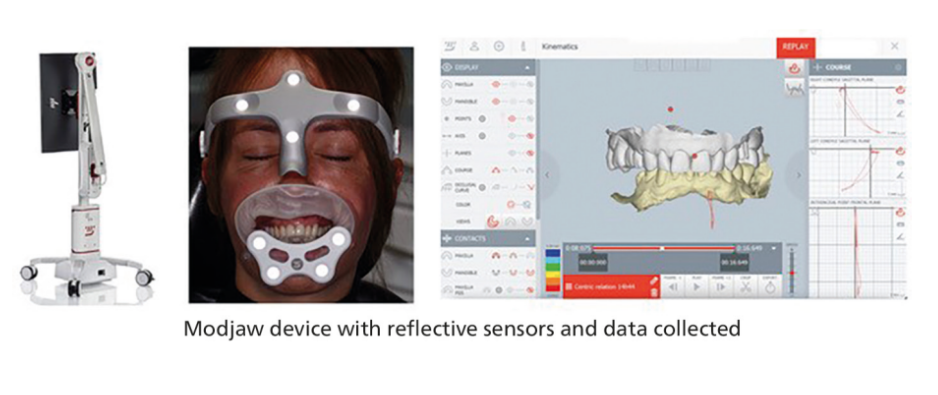
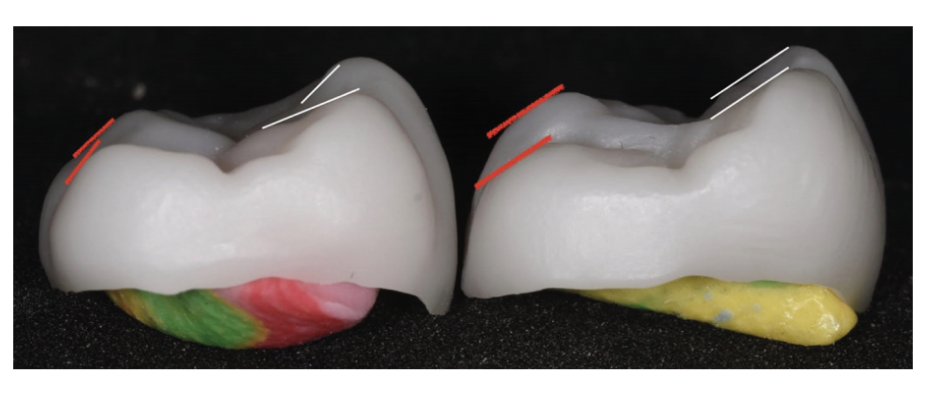
The accuracy of such devices is under scrutiny and a number of studies are now evaluating and comparing this to other methods. The use of this motion data results in more accurate restoration designs that are dictated by the motion of the mandible and the existing cuspal inclines of the teeth (see Figure 6).
Motion analysis also allows assessment of phonetics and, importantly, the space available when making sibilant sounds (based on the letter ‘s’), recognised as important when altering the occlusal vertical dimension.
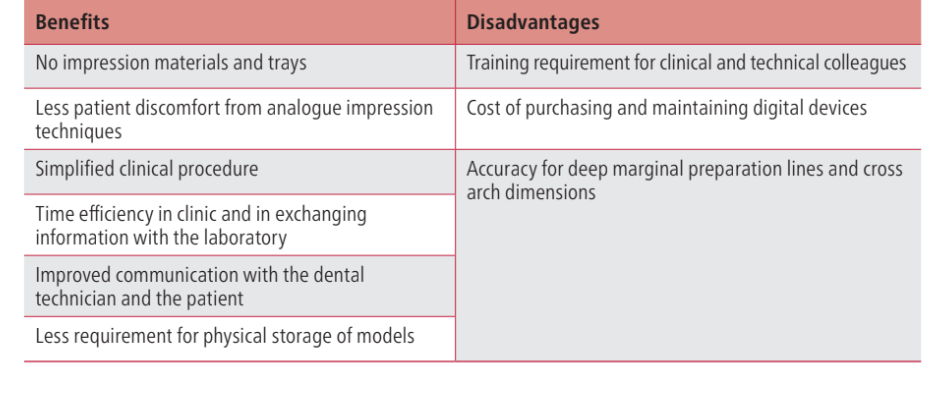
There are a benefits and disadvantages to using digital impression techniques (Table 1).
Data planning and digital design
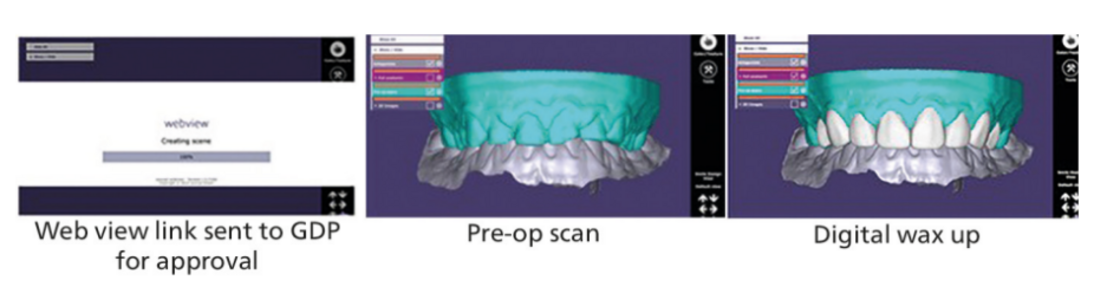
The scans are exported as an STL (Standard Tessellation Language) file format and imported into a computer-aided design and computer-aided manufacturing laboratory software programme, such as Exocad (Align Technology). The dental technician will require detailed instructions and can provide a digital smile preview (Fig. 7) or aesthetic and functional occlusal previews (Fig. 8) for approval by the clinician.
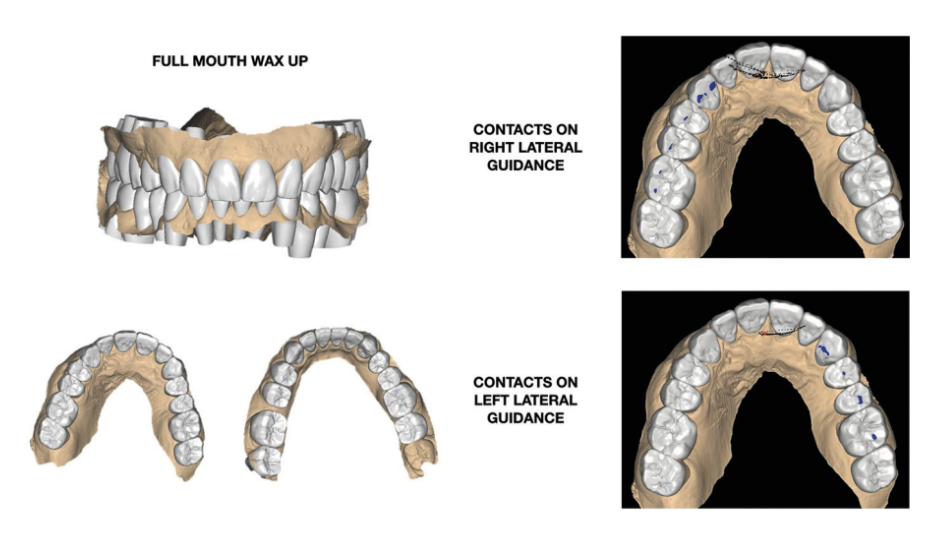
The design, once approved, will result in printed models of the final result and a silicone stent provided to transfer the result, allowing both the clinician and the patient to visualise the proposed outcome and assess occlusal contacts before finalising. This is necessary as part of the informed consent process, especially for complex treatments (Fig. 9).
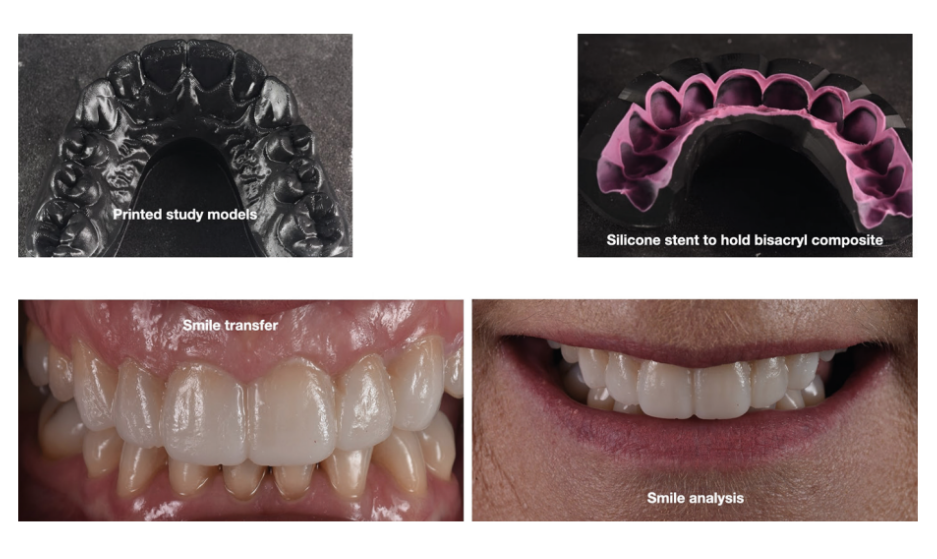
The intra-oral trial allows the clinician and patient to assess:
- Colour and shape of the teeth
- Incisal visibility at rest and when smiling
- Bulk of the material, especially palatally
- Function – occlusion and phonetics.
Any changes can be made at this stage and the altered trial restoration rescanned.
Data execution and delivery
The ongoing development, testing and use of digital technology had led to improved marginal fit and occlusal accuracy of restorations and understandably, many clinicians have probably been reluctant to move from accepted, traditional, analogue techniques until the digital workflow is proven.
Similar accuracies between analogue and digital techniques are now accepted, for up to four units. Full arch impressions continue to show conventional methods are superior, but it is expected that digital technology will equal and then surpass this as the software and hardware continue to develop.
Despite the ease of optical scanning (Fig. 10), the digital method does not compensate for inadequate tooth preparation and gingival retraction techniques. Meticulous care is required to deliver the best result possible.
Digital assessment of post-treatment occlusal contacts
In both analogue and digital workflows, at the restoration fit stage, the clinician will carefully examine the new occlusal contacts and if necessary, adjust. Ideally, the clinician would be able to compare initial and post-treatment occlusions.
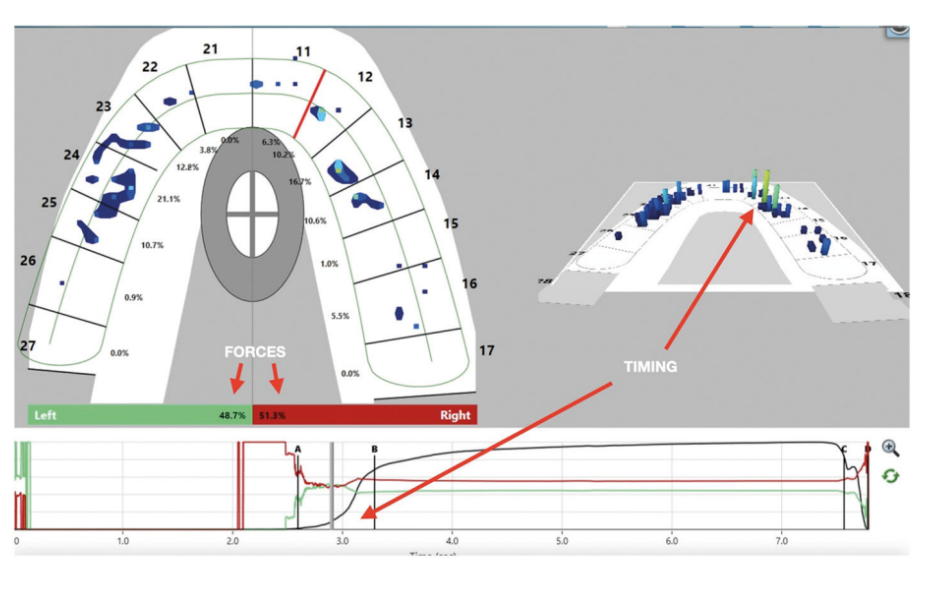
T-scan Novus (Tekscan Inc, USA) utilises a sensor pad, which allows measurement of force and timings of occlusal contacts (Fig. 11). The sensor is 100 microns in thickness with up to 1,370 pressure sensors. When force is applied, an electric current is generated, and the software interprets the data as high- resolution sensels. Articulating paper is still required to locate the mark, but the T-scan allows the correct interpretation of the force contact rather than interpreting colour.
Conclusion
Traditional, analogue dental methods have developed over decades and have resulted in good-quality treatment of patients globally. As in many other sectors for healthcare, and specifically in this case, dentistry is evolving as digital technology provides support for the clinical and technical team. The digital workflow (Fig. 12) is enhancing most stages of patient care and is improving communication, information collection, storage and processing, and the design and manufacture of accurate and reliable restorations. While current and future developments will enable further improvements, the digital dental workflow is moving beyond the domain of a few pioneer clinicians and into the practices of mainstream dental teams.
References:
- Coachman C, Paravina R D. Digitally Enhanced Esthetic Dentistry – From Treatment Planning to Quality Control. J Esthet Restor Dent 2016; DOI: 10.1111/ jerd.12205.
- Lee J D, Nguyen O, Lin Y-C et al. Facial Scanners in Dentistry: An Overview. Prosthesis 2022; 4: 664–678.
- McLaren E A, Garber D A, Figueira J. The Photoshop Smile Design technique (part 1): digital dental photography. Compend Contin Educ Dent 2013; 34: 772–776.
- Calamita M, Coachman C, Sesma N, Kois J. Occlusal vertical dimension: treatment planning decisions and management considerations. Int J Esthet Dent 2019; 14: 166–181.
- Radu M, Radu D, Abboud M. Digital recording of a conventionally determined centric relation: a technique using an intraoral scanner. J Prosthet Dent 2020; 123: 228–231
- Chiu C S, Clark R K. Reproducibility of natural head position. J Dent 1991; 19: 130–131.
- Amezua X, Iturrate M, Garikano X, Solaberrieta E. Analysis of the influence of the facial scanning method on the transfer accuracy of a maxillary digital scan to a 3D face scan for a virtual facebow technique: An in vitro study. J Prosthet Dent 2022; 128: 1024–1031.
- Lepidi L, Galli M, Mastrangelo F et al. Virtual Articulators and Virtual Mounting Procedures: Where Do We Stand? J Prosthodont 2021; 30: 24–35.
