Orthodontic repositioning of lateral incisors into central incisors
The clinical problem of how best to manage an anterior space resulting from a missing central incisor will only be encountered rarely. The goal should be to deliver treatment results that are indistinguishable from normal appearance. This article describes one treatment approach – orthodontic space closure with substitution of the maxillary central incisor by the lateral incisor. Treatment indications, orthodontic and restorative considerations, advantages and disadvantages, as well as the evidence base relating to this treatment modality will be presented and supported by two clinical case examples.
A central incisor may be missing following traumatic avulsion, developmental absence or an enforced extraction due to being malformed, grossly displaced, ankylosed, severely fractured or as a result of local pathology. The clinical management of the resultant anterior edentulous space, to produce both a functional and aesthetic result, can be a signifcant challenge. This is particularly the case for young patients, where there is a need to preserve alveolar bone and gingival architecture during the continuous growth of the dentofacial complex.
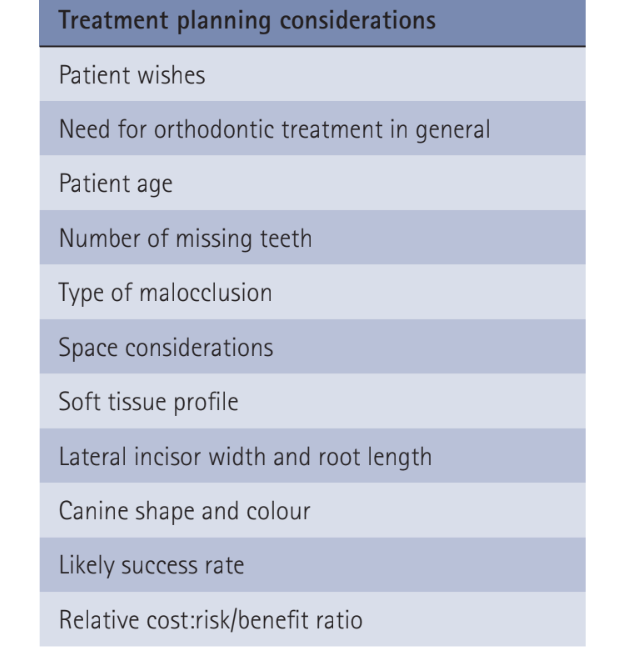
Essentially, there are three treatment approaches for a young person with a missing maxillary central incisor and concomitant malocclusion. The first involves reopening and/or maintaining the space throughout childhood allowing for a defnitive prosthetic replacement in adulthood. The second approach includes premolar autotransplantation followed by restorative modifcation to simulate a central incisor. The last treatment option consists of total orthodontic space closure with substitution of the lateral incisor for the central incisor in the final occlusal scheme. Each of these treatment approaches has its advantages and disadvantages, but the choice of the appropriate solution very much depends on the specifc characteristics of each individual situation. Important treatment planning considerations when deciding how best to manage a missing maxillary central incisor are listed in Table 1.
Total orthodontic space closure
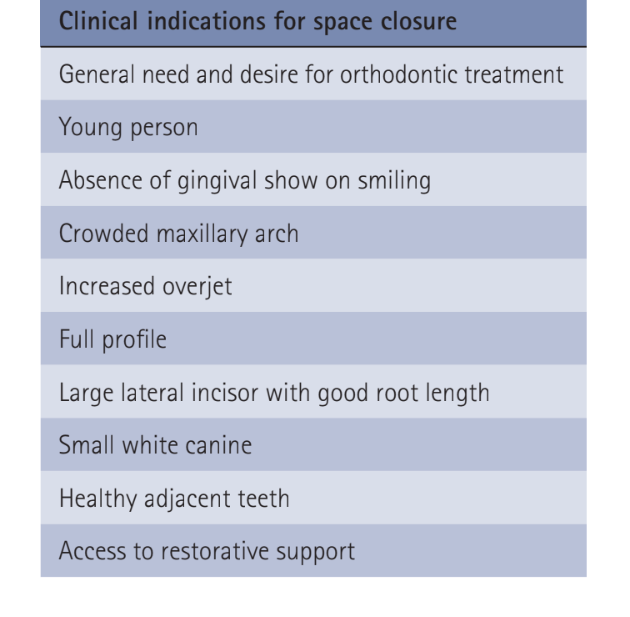
This article will specifically focus on orthodontic space closure with substitution of the maxillary central incisor by the lateral incisor. The clinical indications for choosing this treatment approach are listed in Table 2. This method is particularly favoured when there is concomitant dental crowding or an increased overjet, whereby the anterior edentulous space can be usefully utilised to correct the malocclusion avoiding the need to extract an additional tooth within the affected quadrant.
Undertaking orthodontic space closure in the management of a missing maxillary central incisor dictates that the lateral incisor takes over the aesthetic and functional role of the central incisor, the canine assumes the role of the lateral incisor and the first premolar the role of the canine.
Such positional alterations will necessitate specific orthodontic and restorative interventions to facilitate camouflaging the involved teeth. Camouflaging canines and premolars to resemble lateral incisors and canines respectively has widely been discussed in the literature. Therefore, we will concentrate on the orthodontic and restorative camouflage considerations relating to lateral incisors and their substitution for missing maxillary central incisors.
Orthodontic considerations
Diagnostic wax setup
A diagnostic wax setup of the proposed tooth movements and the necessary modifications to camouflage the teeth is a useful adjunct to facilitate treatment planning, patient consent and construction of a vacuformed matrix to aid restorative treatment.
Vertical tooth positioning
The orthodontist should disregard the incisal edge of the substituted lateral incisor as a guide for final tooth positioning and concentrate on correctly positioning the gingival margin. As such, the lateral incisor must be intruded significantly so that its gingival margin matches the adjacent central incisor and the ipsilateral first premolar, camouflaging as the canine.1 Intrusion also provides further intra-occlusal space to build up the tooth to the correct vertical height and contour to mimic a central incisor.
Mesio-distal tooth positioning
The cervical portion of the lateral incisor is narrower mesio-distally than the central. The mesial and distal margins must therefore be over contoured otherwise the restoration will be triangular in shape and not match the adjacent central incisor. In particular, the emergence profile of a maxillary central incisor is generally flat on the mesial surface. Therefore, in order to maximise aesthetics, the substituted lateral incisor should be moved as close to the midline so that the artificial crown can be made wider on the distal aspect rather than the mesial aspect. Movement of the lateral incisor close to the midline also facilitates creation of an adequate contact point with the adjacent central incisor, which in turn helps to provide adequate support for the interdental papilla.
Labio-palatal tooth positioning
The type of restoration to be placed on the lateral incisor will ultimately deter- mine its labio-palatal position. If a direct composite restoration or porcelain veneer is to be utilised the lateral incisor should be positioned palatally, close to contacting the mandibular incisors. If a porcelain crown is chosen the tooth should be positioned on the centre of the ridge, leaving 0.5-0.75 mm of overjet and allowing for minimal tooth preparation on the palatal aspect.8 It has also been proposed that the substituted lateral incisor should not actually contact the mandibular incisors, there- fore theoretically reducing the functional load on the tooth and avoiding unwanted jiggling forces.
Tooth angulation
The substituted lateral incisor should ideally be positioned more parallel than normal or even slightly upright. This will improve the mesial emergence profile and ensure that a favourable contact point can be created with the adjacent central incisor. Too much mesial crown angulation can result in a large gingival embrasure and a black negative space that compromises optimum aesthetics.
Appliance individualization
It is recommended that the central incisor bracket, in the pre-adjusted edgewise appliance, is placed on the substituted lateral incisor. The wide central incisor bracket will more efficiently maintain the desired mesio-distal angulation of the lateral incisor and will also ensure that the inclination of this tooth matches the adjacent central incisor.
Retention
There is a high risk of anterior space re- opening following this treatment approach and therefore long term, preferably fixed, orthodontic retention is necessary. If both central incisors are missing, consideration should be given to linking the restorations on the lateral incisors, either as linked integral restorations or by bonding a multi-strand orthodontic wire across their palatal surfaces. If full coverage porcelain crowns are to be used, it is recommended that they are constructed with a palatal grove of sufficient depth to accommodate the multi-strand wire.
Restorative considerations
Crown proportions
The substituted lateral incisor needs to be built up to the correct crown size and shape to mimic a central incisor. Guidance on the exact dimensions required can be gauged from the adjacent intact central incisor. However, if both central incisors are missing the use of the golden proportion, with a relative width ratio of 1.616:1.0:0.618 for the central incisor, lateral incisor and canine respectively, and the 80% rule, whereby the ideal maxillary central incisor should be approximately 80% width compared with height, can be helpful. However, many smiles exhibit disproportionality, so these measurements should not be taken as an absolute rule.
Type of restoration
Porcelain restorations, in particular ultra-thin enamel-bonded porcelain veneers, have proved to be both aesthetic and extremely durable restorations and represent the preferred treatment option for adults when camouflaging lateral incisors as centrals. An ultra-thin porcelain veneer can also be placed directly onto a lateral incisor of a young patient, as the risks of pulp perforation and exposure of gingival crown margins during tooth eruption are not contra-indications for a minimally invasive preparation with enamel-bonded porcelain. However, composite resin build-up of the substituted lateral incisor is still considered the treatment of choice in young patients; because it is reversible, non-destructive in nature, relatively inexpensive and allows for future incremental addition and removal of material as the patient continues to mature. In addition, the physical and optical characteristics of today’s resin materials combined with their improved handling properties and their ability to be polished to a natural luster enable the clinician to deliver a highly aesthetic and predictable restoration. The use of a vacuformed matrix when building up the lateral incisor is preferred to the ‘free hand’ intra-oral layering technique as it reduces chair time requirements and enhances accuracy.
Timing of restoration
It is often difficult to determine the exact space requirements for the final restoration during orthodontic treatment. This can be simplified if the lateral incisor is temporarily enlarged to the final dimensions necessary to mimic a central incisor before orthodontic treatment or before final space closure. Temporary enlargement can be achieved with the use of direct composite resin or the construction of a temporary crown using autopolymerizing acrylic resin.
Emergence profile
As previously alluded to, mesial and distal margins of the restoration on the lateral incisor must be over contoured for adequate central incisor appearance and to compensate for the narrower cervical width. If correctly constructed these over-hangs provide support and pressure to effectively sculpt the labial and interdental gingival tissues.
Functional occlusion
The root length of the substituted lateral incisor is shorter than a central incisor and therefore it has been postulated that it will not be able to tolerate protrusive forces as effectively. Consequently, it has been suggested that the artificial crown of the lateral incisor should be 0.5 mm shorter than the adjacent central incisor and that the canine in the true lateral incisor position should be slightly longer than the substituted lateral incisor, therefore allowing these neighbouring teeth to take the major load during mandibular excursions. If both central incisors are replaced then the substituted laterals and the canines should have equal crown heights. The use of linked restorations should also be considered to spread the occlusal loads over a greater combined root surface area.
Gingival margins
As previously highlighted, incorrect gingival margin height of the substituted lateral incisor to mimic the adjacent central incisor can adversely affect the appearance of the restoration. Periodontal surgical procedures, such as crown lengthening, in addition to orthodontic intrusion, may need to be considered. This would also facilitate retention of a large restoration on a smaller tooth.
Periodontal health
The over-contoured mesial and distal margins of the final restoration, although aesthetically necessary, may lead to plaque retention, poor food shedding and periodontal pathology. Strict adherence to oral hygiene instructions is therefore mandatory in order to maintain the health and the appearance of the treatment result.
Case examples
Case one
A 19-year-old male attended the orthodontic clinic following an internal referral from the restorative department. The patient had lost both maxillary central incisors following a traumatic injury aged 7 years. A previous course of orthodontic treatment had been undertaken but the patient failed to wear his retainers. Consequently, a space of 8 mm had reopened between the upper right and left lateral incisors (Fig. 1).

On examination there was a Class I skeletal pattern with a mild Class III incisor relationship. There was moderate crowding in the lower labial segment despite there being only three lower incisors (Figs 2a-d).

The anterior spacing was difficult to restore as the space was only sufficient for one tooth, which would give an unacceptable appearance. The options to close or open space were considered jointly by an orthodontic/restorative clinic. Opening the space would have required posterior extractions as well as long-term restorations with either implants or bridges to replace both missing central incisors. A treatment plan was therefore made to close the space, accepting the difficulties of restoring the lateral incisors. The loss of another lower incisor to relieve lower arch crowding and facilitate achievement of a Class I incisor relationship was also planned.
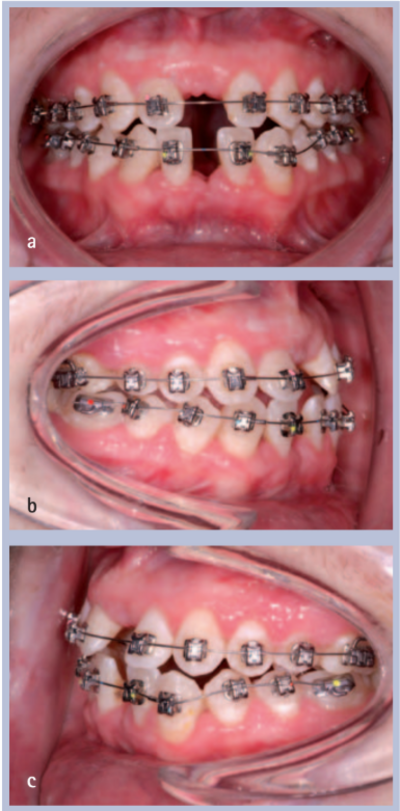
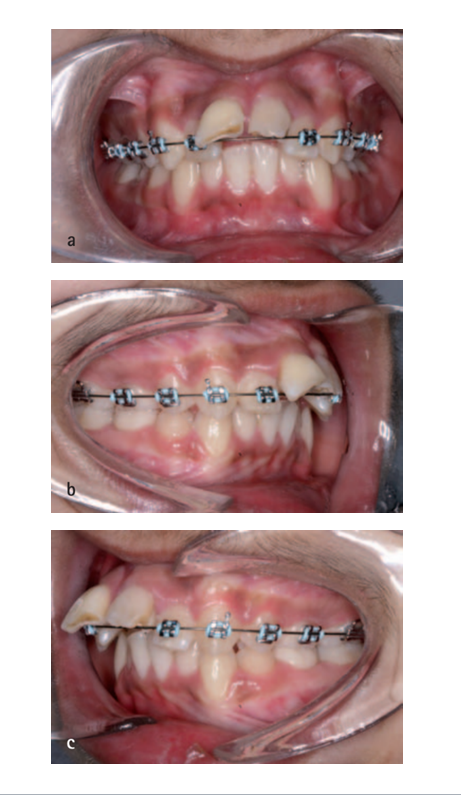
The orthodontic treatment was undertaken with upper and lower fixed self-ligating appliances (Damon, Ormco Ltd) and treatment progressed to close the anterior spacing (Figs 3a-c).
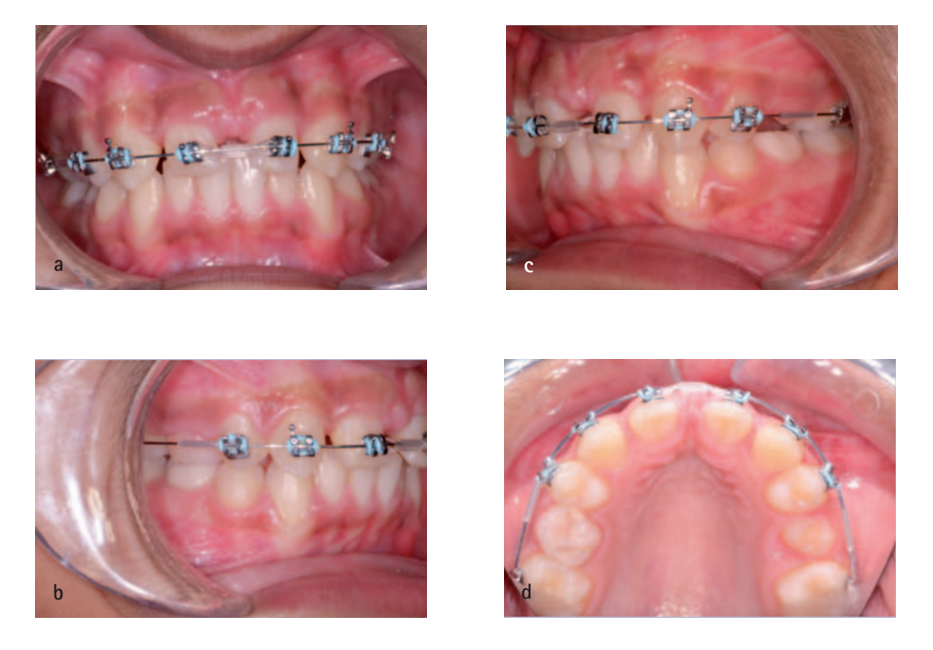
Towards the end of space closure the maxillary lateral incisors were built-up with composite resin to the desired dimensions to mimic central incisors and a vacuformed matrix was used (Fig. 4).

Periodontal surgery to lengthen the right maxillary lateral incisor crown and to match the lateral incisors’ gingival margins was also undertaken. Orthodontic brackets were then replaced and space closure completed to the correct space requirements (Fig. 5).

While the composite restorations were of reasonable appearance, the patient requested a more optimal aesthetic outcome. Therefore, following a risk-benefit discussion, on the day of appliance debond the lateral incisors were prepared for bonded porcelain crowns. The use of provisional composite restorations allowed for minimal tooth reduction. Nonetheless, tooth preparation did potentially jeopardise pulpal health, with the loss of vitality reported in up to 20% of crowned teeth. It is therefore important to highlight that crown preparation is not the first choice option in such cases and the use of more conservative adhesive techniques should always be attempted first. For this patient, the crowns were constructed with a palatal groove to accommodate a multi-strand orthodontic retainer wire, which was bonded in place on the same day as the crowns and aimed to prevent unwanted reopening of the midline space. The patient was notably pleased with the final treatment result (Figs 6a-f).

Case two
A 13-year-old boy was referred to the orthodontic department following treatment to his traumatised anterior teeth. One year ago the patient had fallen and traumatised both anterior teeth. The upper right central incisor (UR1) had been avulsed and the upper left central incisor (UL1) intruded. The UR1 had been re- implanted one hour post-trauma and the teeth were splinted together. Both teeth were subsequently accessed for pulp extirpation and a referral made to the orthodontic department.
Following a clinical and radiographic examination the patient presented with a Class II division 1 incisor relationship on a skeletal 2 base (Figs 7a and b).
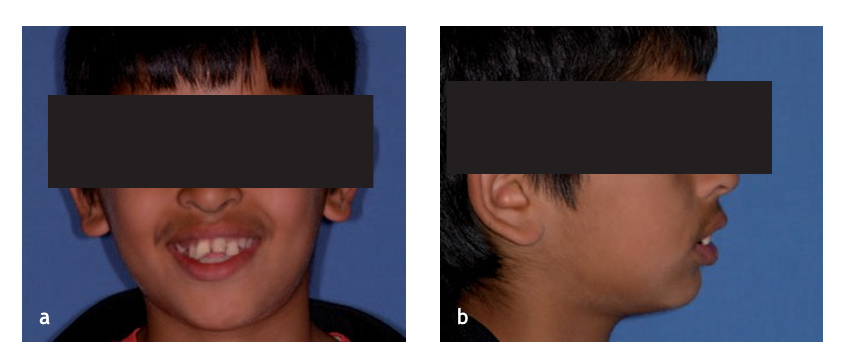
The overjet was increased at 11 mm and there was upper and lower dental crowding (Figs 8a-e). A treatment plan was formulated to remove the traumatised anterior teeth and disguise both maxillary lateral incisors as centrals.

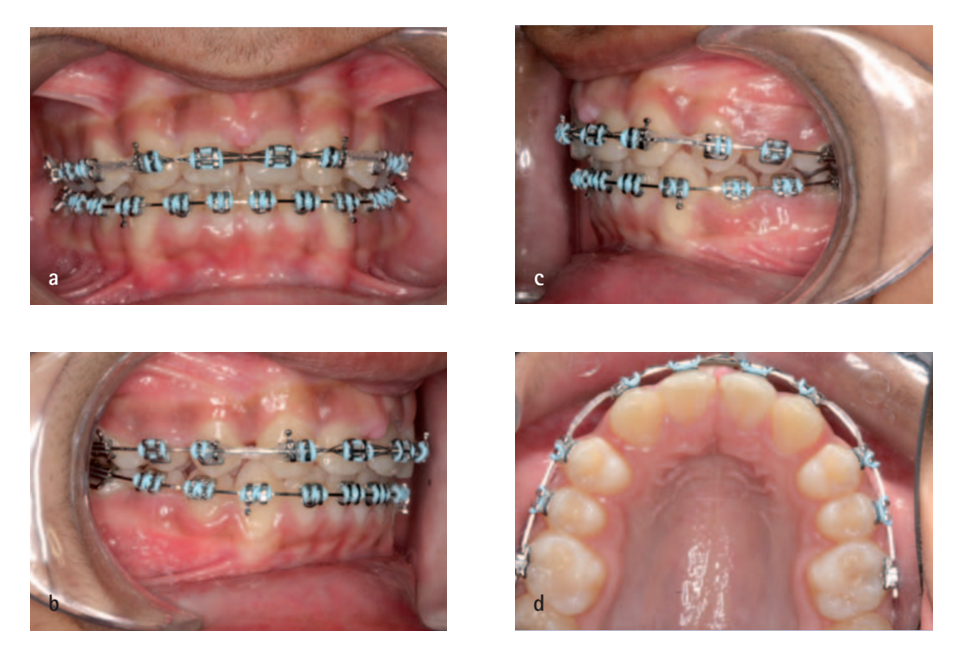
The orthodontic treatment was under- taken with upper and lower fixed appliances. Initially the maxillary central incisors were left in situ to maintain some form of aesthetics until the space closure stage when the extractions were undertaken (Figs 9a-c).
Once in rectangular stainless steel working archwires (Figs 10a-d) the maxillary lateral incisors were mesialised with a view to composite build-ups being placed after orthodontic treatment (Figs 11a-d).
Treatment progressed uneventfully (Figs 12a-e) and upper and lower removable retainers were fitted. Although treatment was offered to improve the appearance of the anterior teeth, in particular the positions of the gingival margins, the patient was extremely happy with the outcome and requested no further intervention (Figs 13a and b).


Discussion
This article describes one of the strategies for treating patients with one or two missing maxillary central incisors. Space closure and substitution of central incisors by lateral incisors is, however, sometimes questioned. Concern has been expressed that the treatment result might not look ‘natural’, particularly in patients with a unilateral missing central incisor. However, results which are almost indistinguishable from normal appearance can be produced, but indications for this selected approach (Table 2) must be present and attention to detail throughout treatment must be exercised. The recognised disadvantages of this treatment approach include: increased treatment complexity, requirement for integrated interdisciplinary management, increased functional load on the small lateral incisor root and a high risk of anterior space reopening. The latter is a particular problem and necessitates long-term orthodontic retention.
The main advantages of this treatment approach in young patients with a missing central incisor is the permanence and bio- logical compatibility of the treatment result, allowing for treatment to be completed in early adolescence soon after the fixed appliances are removed. Mesial movement of the lateral incisor into the central incisor space maintains alveolar bone height, along with attached gingiva and the interdental papilla, during the continuous growth of the dentofacial complex. Consequently the ‘red aesthetics’, the appearance of the soft tissue surrounding the tooth, can be maintained, which may be difficult to obtain with restorative rehabilitation and notably implants. The need for temporary prosthetic tooth replacements, such as removable prostheses or resin retained bridges until growth is complete and implants can be considered, is also eliminated along with their associated cost and maintenance implications.
It is important to adopt evidence- based clinical practice whenever possible. Unfortunately, with regards to the management of missing maxillary central incisors, there is an absence of research comparing the functional and aesthetic results of various treatment modalities. One study by Czochrowska et al. has, however, com- pared biological features and the clinical appearance of the substituted lateral incisor with the intact neighbouring central incisor in 20 patients consecutively treated with unilateral space closure. Essentially, they demonstrated that treatment was time consuming with a mean duration of 34 months; the lateral incisor root was capable of sup- porting a crown the size of a central incisor; periodontal health was not compromised and that all patients expressed satisfaction with the overall treatment result despite a professionally assessed, aesthetical match in only 50% of patients. Interestingly, these findings are similar to studies which compared autotransplanted premolars placed in the missing central incisor position with the intact neighbouring central incisor. Overall, this evidence would appear to support the clinical practice of orthodontic space closure and lateral incisor substitution in appropriate patients.
Conclusion
Orthodontic space closure with the substitution of a maxillary central incisor by a lateral incisor, although a clinical challenge, is a viable treatment approach to manage the rare clinical problem of a missing maxillary central incisor. Functional and aesthetically satisfactory results, which demonstrate permanence and good biological adaptation, are achievable as long as specific treatment indications are present, excellent restorative support is available and attention to detail is exercised throughout orthodontic treatment.
Authors: R. J. McDowall, R. Yar and D. T. Waring
Reference:
- Kokich V G, Crabill K E. Managing the patient with missing or malformed maxillary central incisors. Am J Orthod Dentofacial Orthop 2006; 129: S55–S63.
- Bowden D E, Patel H A. Autotransplantation of premolar teeth to replace missing maxillary central incisors. Br J Orthod 1990; 17: 21–28.
- Zachrisson B U. Improving orthodontic results in cases with maxillary incisors missing. Am J Orthod 1978; 73: 274–289.
- Zachrisson B U, Rosa M, Toreskog S. Congenitally missing maxillary lateral incisors: canine substitution. Am J Orthod Dentofacial Orthop 2011; 139: 434, 436, 438.
- Chaushu S, Becker A, Zalkind M. Prosthetic con- siderations in the restoration of orthodontically treated maxillary lateral incisors to replace missing central incisors: a clinical report. J Prosthet Dent 2001; 85: 335–341.
- Kokich V G, Nappen D L, Shapiro P A. Gingival contour and clinical crown length: their effect on the esthetic appearance of maxillary anterior teeth. Am J Orthod 1984; 86: 89–94.
- Newsome P R, Cooke M S. Modifying upper lateral incisors to mimic missing central incisors: new ways to overcome old problems? Restorative Dent 1987; 3: 91–95, 97, 99.
- Sabri R. Treatment of a class I crowded malocclu- sion with an ankylosed maxillary central incisor. Am J Orthod Dentofacial Orthop 2002; 122: 557–565.
- Schwaninger B, Shaye R. Management of cases with upper incisors missing. Am J Orthod 1977; 71: 396–405.
- Levin E I. Dental esthetics and the golden propor- tion. J Prosthet Dent 1978; 40: 244–252.
- Gürel G. The science and art of porcelain laminate veneers. London: Quintessence, 2003.
- Swift E J Jr, Friedman M J. Critical appraisal: porce- lain veneer outcomes, part II. J Esthet Restor Dent 2006; 18: 110–113.
- Asher C, Lewis D H. The integration of orthodontic and restorative procedures in cases with missing maxillary incisors. Br Dent J 1986; 160: 241–245.
- Czochrowska E M, Skaare A B, Stenvik A, Zachrisson B U. Outcome of orthodontic space closure with a missing maxillary central incisor. Am J Orthod Dentofacial Orthop 2003; 123: 597–603.
- Saunders W P, Saunders E M. Prevalence of periradicular periodontitis associated with crowned teeth in an adult Scottish subpopulation. Br Dent J 1998; 185: 137–140.
- Antosz M. Space closure for a missing central incisor. Am J Orthod Dentofacial Orthop 2003; 124: 18A.
- Hellekant M, Twetman S, Carlsson L. Treatment of a class II division 1 malocclusion with macrodontia of the maxillary central incisors. Am J Orthod Dentofacial Orthop 2001; 119: 654–659.
- Janson G, Valarelli D P, Valarelli F P, de Freitas M R, Pinzan A. Atypical extraction of maxillary central incisors. Am J Orthod Dentofacial Orthop 2010; 138: 510–517.
- Stenvik A, Zachrisson B U. Missing anterior teeth: orthodontic closure and transplantation as viable options to conventional replacements. Endod Topics 2006; 14: 41–50.
- Czochrowska E M, Stenvik A, Zachrisson B U. The esthetic outcome of autotransplanted premolars replacing maxillary incisors. Dent Traumatol 2002; 18: 237–245.
- Czochrowska E M, Stenvik A, Album B, Zachrisson B U. Autotransplantation of premolars to replace maxillary incisors: a comparison with natural incisors. Am J Orthod Dentofacial Orthop 2000; 118: 592–600.
